Abstract
Previously published analyses showed that inequalities in mortality rates between residents of poor and wealthy neighborhoods in New York City (NYC) narrowed between 1990 and 2000, but these trends may have been influenced by population in-migration and gentrification. The NYC public housing population has been less subject to these population shifts than those in other NYC neighborhoods. We compared changes in mortality rates (MRs) from 1989–1991 to 1999–2001 among residents of NYC census blocks consisting entirely of public housing residences with residents of nonpublic housing low-income and higher-income blocks. Public housing and nonpublic housing low-income blocks were those in census block groups with ≥50% of residents living at <1.5 times the federal poverty level (FPL); nonpublic housing higher-income blocks were those in census block groups with <50% of residents living at <1.5 times the FPL. Information on deaths was obtained from NYC’s vital registry, and US Census data were used for denominators. Age-standardized all-cause MRs in public housing, low-income, and higher-income residents decreased between the decades by 16%, 28%, and 22%, respectively. While mortality rate ratios between low-income and higher-income residents narrowed by 8%, the relative disparity between public housing and low-income residents widened by 21%. Diseases amenable to prevention including malignancies, diabetes, and chronic lung disease contributed to the increased overall mortality disparity between public housing and lower-income residents. These findings temper previous findings that inequalities in the health of poor and wealthier NYC neighborhood residents have narrowed. NYC public housing residents should be a high-priority population for efforts to reduce health disparities.
Keywords: Health status disparities; New York City; Housing, Public; Immigrants and emigrants
Introduction
Goals for improving population health include the reduction of health disparities. Neighborhood-level poverty has been shown to be a powerful indicator of negative health outcomes, and area-based socioeconomic position (SEP) measures have been used to both target interventions and track changes in health disparities over time.1–3 When area-based SEP measures are used to track and interpret health disparities, the compositional and contextual factors influencing health within neighborhoods and secular changes in these factors must be considered.4–14 If these changes are not reflected in the relative or absolute value of poverty concentration at the neighborhood level, measured trends in area-based health disparities may not be accurate.
In New York City (NYC), all-cause mortality decreased by 25% between 1990 and 2000, the greatest decrease in the past six decades.15 The poorest neighborhoods had greater decreases in mortality than the wealthiest neighborhoods, leading to a reduction in mortality disparities.16 These analyses defined NYC neighborhoods using large geographic areas known as community districts (median population = 125,000), which comprise dozens of census tracts (median number of tracts = 36, range 15–105).16 Although this definition of neighborhood allows for relatively stable mortality estimates and may have “real-life” meaning, it also allows for substantial heterogeneity of compositional and contextual neighborhood effects to influence the mortality estimates.16,17
Over a decade, the demographics of an urban neighborhood can change substantially, as a result of in- or out-migration. A 9.6% increase in NYC’s population from 1990–2000 (7,322,564 to 8,008,278) suggests in- and out-migration during the 1990s that could influence trends in health measured at the neighborhood level.18 For example, in-migrants to low-income neighborhoods may be healthier than the average individual residing in neighborhoods to which they in-migrate, due to social, behavioral, or selection factors related to the physical and psychological demands of relocation.19–21 Out-migration of healthier populations from impoverished neighborhoods could also occur. Secular changes in poverty concentration could occur as a result from any combination of individual, structural, social, and economic trends in the neighborhood. “Gentrification” is often used to describe a decrease in neighborhood poverty concentration, and “digression” is used to describe an increase in neighborhood poverty concentration. Gentrification is often characterized by in-migration of populations with higher SEP than existing residents, which may or may not be accompanied by displacement among the lower-SEP residents.22 Although gentrification has inspired debate with minimal agreement on definition and operationalization, the impact of gentrification on health has been demonstrated in many populations.23–27 Therefore, health improvements measured among residents of low-income neighborhoods undergoing gentrification may not reflect improvements in the health of low-income individuals residing in the areas prior to the gentrification.
In contrast to the general NYC population—which has been characterized by rapid growth, net in-migration, and gentrification—residents of public housing in NYC are relatively socioeconomically homogeneous and less subject to these demographic shifts compared to other low-income communities. Public housing tenants make up nearly 5% of New Yorkers and must be legal US residents and meet low-income criteria for entry into a public housing residence.
The influence of migration and gentrification could result in a spurious narrowing of health disparities by SEP.24 If area-based socioeconomic measures are to be used to track secular changes in health disparities for populations (as opposed to geographic areas), then epidemiologic analyses should seek to minimize the potential impacts of migration and changes in poverty concentration. Our objective was to examine mortality trends in residents of low-income neighborhoods compared to more affluent neighborhoods while reducing the potential influence of secular compositional and contextual changes in the neighborhoods due to migration and changing poverty concentration. Trends in mortality rates in NYC from 1990 to 2000 among three populations identified by the type of neighborhood in which the residents live—public housing residents, residents of low-income neighborhoods without public housing, and residents of higher-income neighborhoods without public housing—were examined.
Methods
Mortality Data
Mortality data for NYC residents who died in NYC during 1989–1991 and 1999–2001 were obtained from the Office of Vital Statistics, New York City Department of Health and Mental Hygiene. The number of deaths was summed over the 3-year periods (1989–1991 and 1991–2001) to bracket the decennial census years and allow for computing average MRs using census-based denominators. Cause of death was determined from the underlying cause of death reported on death certificates using the International Classifications of Disease (ICD) revision 9 for deaths reported in 1989–1991 and 1999, and revision 10 for 2000–2001. The numbers of all-cause deaths and cause-specific deaths for the 12 leading causes of death from 1999–2001 were compiled, using categories consistent with a prior study of mortality disparities in residents of NYC neighborhoods.16 Each of the top 12 causes of death contributed at least 1% of all deaths in each time period (1989–1991 and 1999–2000). These causes, their corresponding ICD-9 and ICD-10 codes, and comparability ratios1 are: major cardiovascular diseases including heart disease and stroke (390–434, 436–448; I00–I78; 0.9981); malignancies (140–208; C00–C97; 1.0068); HIV/AIDS (42–44; B20–B24; 1.0637); diabetes (250; E10–E14; 1.0082); pneumonia and influenza (480–487; J10–J18; 0.6982); chronic lower respiratory diseases (490–494, 496; J40–J47; 1.0478); drug-related (304, E850–E852, E854–E855, E858; F11–F16, F18–F19, X40–X42, X44; n/a); homicide (E906–E969; X85–Y09, Y87.1; 0.9983); liver disease (571; K70, K73–K74; 1.0367); external causes (e.g., accidents, injuries, and poisonings, but excluding drug overdose; E800.0–849.9, E853.0–E853.9, E856.0–E857.9, E859–E869, E880–E929; V01–X39, X43, X45–X59, Y85–Y86; n/a); renal disease (580–589; N00–N07, N17–N19, N25–27; 1.2320); and septicemia (38; A40–A41; 1.1949). The comparability ratios for the leading causes of death are small in comparison to the changes we observed in mortality rates over time. Therefore, the mortality rates presented are not adjusted for the change in the coding system.
Restriction and Classification of Neighborhoods
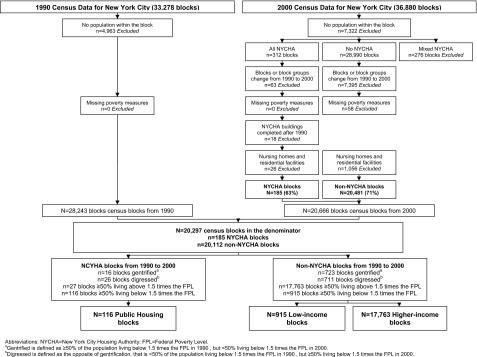
Three types of neighborhoods were identified by restricting and classifying NYC census blocks for use in our analysis as described below and depicted in Figure 1. To minimize heterogeneity within the types of neighborhoods, poverty concentration (classified at the census block group level) and public housing (classified at the census block level) were used to describe and classify each census block as belonging to one of the three specified neighborhood types. This classification was possible because many NYC census blocks are occupied entirely by public housing residences, thereby allowing for the use of census-based denominators to estimate mortality rates.
FIGURE 1.
The restriction and classification of New York City census blocks into one of three categories (public housing, low-income, higher-income), 1990 and 2000.
Public housing neighborhood census blocks were defined as census blocks in which all housing units are owned by the New York City Housing Authority (NYCHA), based on Map Pluto data provided by the New York City Department of City Planning. Geographic information systems data provided by NYCHA was used to identify census blocks corresponding to public housing developments opened after 1990, which were excluded from our analysis due to lack of data for those developments in 1990. To facilitate comparison with nonpublic housing low-income census blocks, public housing census blocks were further restricted to those located in census block groups in which ≥50% of the residents live in households with income <1.5 times the federal poverty level (FPL).28 Because the FPL does not adjust for geographic differences in the cost-of-living, and the cost-of-living is higher in NYC than many other geographical locations in the USA, a poverty income ratio of 1.5 was chosen to better reflect household poverty. This area-based measure of economic deprivation is a robust predictor of inequalities in population health.29–31
Low-income neighborhood census blocks were defined as census blocks with no housing units owned by NYCHA and which are located in census block groups in which ≥50% of the residents live below 1.5 times the FPL.
Higher-income neighborhood census blocks were defined as census blocks with no housing units owned by NYCHA and located in census block groups in which <50% of the residents live below 1.5 times the FPL.
To minimize misclassification of census blocks, any block that included a mixture of public housing and private residential units was excluded. To ensure consistency in census block classification over time, the blocks were further restricted to blocks and block groups with no change in geographic boundaries between 1990 and 2000. Acknowledging controversy in operationalizing gentrification, we defined gentrification as a decrease from ≥50% to <50% living below 1.5 times the FPL from 1990 to 2000. Similarly, digression was operationalized as an increase from <50% to ≥50% living below 1.5 times the FPL. Only census blocks located in census block groups with stable poverty concentration (i.e., ≥50% living below 1.5 times the FPL in both the 1990 and 2000 census for public housing and low-income blocks and <50% living below 1.5 times the FPL in both the 1990 and 2000 census for higher income blocks) were included. After applying these exclusions, sex- and age-specific population counts were summed across blocks within each of three neighborhood types (public housing, low-income, and higher-income) to use as denominators for estimation of MRs. Population counts stratified by age and race or ethnicity are not available at the block level, removing the possibility of directly calculating age and race or ethnicity adjusted MRs.
Linkage of Mortality Data to Census Blocks
There were 376,835 deaths of NYC residents occurring in NYC from 1989–1991 and 1999–2001; 118,673 out of 202,144 (58.7%) deaths from 1989–1991 and 96,511 out of 169,002 (57.1%) deaths from 1999–2001 were included as these deaths were of residents of census blocks included in the study.
Analysis
Age-adjusted, all-cause, and cause-specific MRs and rate ratios (MRRs) were calculated for residents of public housing, low-income, and higher-income neighborhoods. All MRs were age-standardized to the year 2000 standard US population. The gamma distribution was used to estimate the variance and 95% confidence intervals for the overall and cause-specific age-standardized MRs.32 Age-specific MRs were also calculated, and the Poisson distribution was used for the calculation of the 95% confidence intervals. MRRs were calculated with 95% confidence intervals estimated using the variance from the rates. Finally, to assess the cause-specific contributions to overall mortality disparities, age-standardized mortality rate differences (MRDs) were calculated for each category of cause of death and statistical significance was determined by non-overlapping 95% confidence intervals. All analyses were performed using SAS 9.1.
Results
Characteristics of Census Blocks Included and Excluded
The distribution of census blocks excluded because of gentrification (operationalized as a census block within in a block group in which ≥50% of residents were living below 1.5 times the FPL in 1990, but in which <50% of residents were living below 1.5 times the FPL in 2000) was consistent with our hypothesis that the public housing populations have been less subject to the influence of neighborhood gentrification than the low-income populations in NYC (Figure 1). Of the 132 public housing blocks with unchanged census geography and in block groups in which ≥50% of residents were living below 1.5 times the FPL in 1990, 16 blocks (12%) were in block groups that gentrified by 2000. In contrast, gentrification occurred in 723 (44%) of the 1,638 nonpublic housing census blocks in which ≥50% of residents were living below 1.5 times the FPL. The 29,558 populated 2000 census blocks and the 28,315 populated 1990 census blocks were restricted to 116 public housing blocks, 915 low-income blocks, and 17,763 higher-income blocks.
The population in public housing census blocks declined by 13% while populations of low- and higher-income blocks grew by 9% and 11%, respectively (Table 1). The public housing population had the highest proportion of residents reporting living in their homes for at least 5 years in 2000. Consistent with more in-migration, the low- and higher-income populations saw a decline in the proportion of long-term residents from 1990 to 2000. Population change varied by age and group; both the public housing and low-income populations had a decrease in the proportion of the population <45 years old, while the higher-income population had an increase in this age group. Despite these trends, the public housing and low-income populations were still much younger compared to the higher-income population in 2000.
Table 1.
Demographic characteristics of the public housing, low-income, and higher-income populations, New York City, 1990 and 2000
| Public housing N = 116 census blocks | Low-income N = 915 census blocks | Higher-income N = 17,763 census blocks | ||||
|---|---|---|---|---|---|---|
| 1990 | 2000 | 1990 | 2000 | 1990 | 2000 | |
| Total population | 135,139 | 116,947 | 346,799 | 376,627 | 4,261,845 | 4,714,595 |
| Households living in residence for 5 or more years (%)a | 66 | 67 | 57 | 55 | 63 | 58 |
| Age (%)b | ||||||
| 0–24 years | 48 | 47 | 48 | 47 | 30 | 32 |
| 25–44 years | 26 | 25 | 30 | 29 | 35 | 34 |
| 45–64 years | 17 | 19 | 14 | 16 | 20 | 22 |
| 65+ years | 8 | 9 | 7 | 7 | 14 | 12 |
| Percentage living below 1.5 times the federal poverty line (%)a | 63 | 64 | 66 | 63 | 19 | 23 |
| Race/ethnicity (%)b | ||||||
| Non-Hispanic White | 3 | 2 | 10 | 10 | 56 | 44 |
| Non-Hispanic Black | 51 | 46 | 32 | 30 | 21 | 23 |
| Hispanic | 45 | 48 | 55 | 55 | 15 | 18 |
| Foreign Bornb | 12 | 17 | 23 | 29 | 30 | 38 |
aMean percentage measured at the census block group level
bMean percentage measured at the census block level
Poverty concentration, by design, remained high and was comparable in both the public housing and low-income neighborhoods, though poverty concentration decreased by 3% in the latter (Table 1). There was a decrease in the proportion of non-Hispanic Black residents and an increase in Hispanic residents of public housing census blocks. The proportions of non-Hispanic White and Hispanic low-income residents were somewhat higher compared to public housing residents, but these proportions were stable from 1990 to 2000. The proportion of non-Hispanic White higher-income residents fell 12% from 1990 to 2000, as the proportion of foreign born higher-income residents increased by 8%. Although the proportion of foreign-born residents rose in all three groups, it was substantially lower in the public housing residents in 1990 and 2000.
All-Cause and Cause-Specific Mortality Rates and Ratios
All-cause MRs decreased from 1989–1991 to 1999–2001 by 16%, 28%, and 22% in the public housing, low-income, and higher-income populations, respectively (Table 2). From 1989–1991 to 1999–2001, the all-cause MRR comparing residents of public housing with residents of low-income and with higher-income neighborhoods increased by 21% and 14%, respectively; the all-cause MRR in the low-income population compared to the higher-income population decreased by 8%.
Table 2.
Age-adjusted mortality rates and mortality rate ratios in the public housing, low-income, and higher-income populations in New York City, 1989–1991 and 1999–2001
| Causea | MRsb in the public housing census blocks | MRsb in the low-income census blocks | MRsb in the higher-income census blocks | MRRsc of public housing/higher-income | MRRsc of low-income/higher-income | MRRsc of public housing/low-income | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1989–1991 | 1999–2001 | 1989–1991 | 1999–2001 | 1989–1991 | 1999–2001 | 1989–1991 | 1999–2001 | 1989–1991 | 1999–2001 | 1989–1991 | 1999–2001 | |
| All | 1,468 | 1,234 | 1,211 | 870 | 826 | 643 | 1.78 | 1.92 | 1.47 | 1.35 | 1.21 | 1.42 |
| Cardiovascular disease | 522 | 458 | 477 | 349 | 381 | 307 | 1.37 | 1.49 | 1.25 | 1.14 | 1.09 | 1.31 |
| Malignancies | 251 | 271 | 209 | 183 | 180 | 158 | 1.39 | 1.72 | 1.16 | 1.16 | 1.20 | 1.48 |
| Breastd | 39 | 41 | 26 | 26 | 32 | 25 | 1.22c | 1.64 | 0.81 | 1.04c | 1.50 | 1.58 |
| Colon | 25 | 33 | 29 | 20 | 23 | 19 | 1.08c | 1.74 | 1.26 | 1.05c | 0.86c | 1.65 |
| Lung | 53 | 64 | 45 | 42 | 42 | 36 | 1.26 | 1.78 | 1.07c | 1.17 | 1.18c | 1.52 |
| Prostated | 45 | 70 | 32 | 36 | 30 | 26 | 1.50 | 2.69 | 1.07c | 1.38 | 1.41c | 1.94 |
| HIV/AIDS | 142 | 83 | 89 | 52 | 46 | 13 | 3.09 | 6.38 | 1.93 | 4.00 | 1.60 | 1.60 |
| Diabetes | 29 | 56 | 23 | 36 | 10 | 17 | 2.90 | 3.29 | 2.30 | 2.12 | 1.26c | 1.56 |
| Influenza and pneumonia | 73 | 47 | 56 | 31 | 34 | 24 | 2.15 | 1.96 | 1.65 | 1.29 | 1.30 | 1.52 |
| Chronic lower respiratory disease | 35 | 43 | 24 | 26 | 18 | 18 | 1.94 | 2.39 | 1.33 | 1.44 | 1.46 | 1.65 |
| Drug-related | 35 | 29 | 22 | 20 | 6 | 7 | 5.83 | 4.14 | 3.67 | 2.86 | 1.59 | 1.45 |
| Homicide | 59 | 23 | 56 | 15 | 16 | 5 | 3.69 | 4.60 | 3.50 | 3.00 | 1.05c | 1.53 |
| Liver disease | 31 | 21 | 29 | 16 | 10 | 5 | 3.10 | 4.20 | 2.90 | 3.20 | 1.07c | 1.31c |
| External causes | 26 | 19 | 26 | 18 | 18 | 12 | 1.44 | 1.58 | 1.44 | 1.50 | 1.00c | 1.06c |
| Renal disease | 22 | 20 | 10 | 16 | 8 | 9 | 2.75 | 2.22 | 1.25c | 1.78 | 2.20 | 1.25c |
| Septicemia | 28 | 18 | 17 | 11 | 7 | 6 | 4.00 | 3.00 | 2.43 | 1.83 | 1.65 | 1.64 |
| Other | 215 | 145 | 173 | 97 | 92 | 62 | 2.34 | 2.34 | 1.88 | 1.56 | 1.24 | 1.49 |
aCauses are ranked by the 1999–2001 MRs in the public housing population
bAll MRs are per 100,000 persons and rounded to the nearest whole number
cMRR is not statistically significantly from 1.00; all other MRRs are significantly different from 1
dMRs and MRRs are sex-specific
Time trends in cause-specific MRs were more variable (Table 2), with the following cause-specific MRs increasing from 1989–1991 to 1999–2001: malignancies, diabetes, and chronic lung disease in the public housing population; diabetes, chronic lung disease, and renal disease in the low-income population; and diabetes, drug-related and renal disease in the higher-income population. Consistent with citywide and national trends, diabetes mortality was the only cause of death to increase in all three populations. Notably, the diabetes MR in the public housing population increased by 93%, and the gap in diabetes mortality between the public housing population and the low- and higher-income populations increased in relative and absolute terms. At the same time, age-adjusted MRs from HIV/AIDS decreased dramatically in all three populations. Although the absolute improvement in the HIV/AIDS MRs was greatest in the public housing population, the proportionate mortality reduction was greatest in the higher-income population, producing a larger relative disparity comparing the higher-income to public housing populations in 1999–2001. Age-adjusted MRs for cardiovascular disease and homicide also decreased substantially in all three populations from 1989–1991 to 1999–2001.
Malignancy MRs increased only in the public housing population, resulting in the proportion of the all-cause MR due to malignancies increasing from 17% in 1989–1991 to 22% in 1999–2001 (Table 2). In the public housing population, mortality from breast, colon, lung, and prostate cancer increased from 1989–1991 to 1999–2001 accounting for much of a widening gap in cancer mortality compared with the other groups (Table 2). All four of these site-specific cancer MRs decreased in the higher-income population from 1989–1991 to 1999–2001, while in the low-income population, breast cancer mortality was unchanged, prostate cancer mortality increased slightly, and lung and colon cancer decreased.
All Cause and Cause-Specific Mortality Rate Differences
The overall MRD between the low- and higher-income populations narrowed, with substantial reductions in MRDs for cardiovascular disease, pneumonia, and influenza, and homicide contributing to the narrowing disparity (Table 3). By contrast, the overall MRD comparing the public housing population to the higher-income population declined only slightly, while the difference between the public housing and lower-income populations increased. Notably, MRDs between public housing populations and the other populations increased for cardiovascular disease, cancer, diabetes, and chronic lower respiratory diseases. These increased differences in cause-specific mortality in the public housing population compared to the other populations were somewhat offset by a decrease in the HIV/AIDS MRDs and a decrease in homicide MRDs in the public housing population compared to the higher-income population (Table 3). As a consequence of these trends, the proportion of the overall MRD in the public housing compared to the low-income population accounted for by cardiovascular disease, cancer, diabetes, and chronic lower respiratory diseases increased from 40% in 1989–1991 to 64% in 1999–2001. Similarly, comparing the public housing to the higher-income population, the overall MDR accounted for by these chronic diseases increased from 39% in 1989–1991 to 56% in 1999–2001.
Table 3.
Age-adjusted mortality rate differences in the public housing, low-income, and higher-income populations in New York City, 1989–1991 and 1999–2001
| Causea | MRDb public housing–higher-Income | MRDb lower-income–higher-income | MRDb public housing–low-income | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 1989–1991 | 1999–2001 | % Change | 1989–1991 | 1999–2001 | % Change | 1989–1991 | 1999–2001 | % Change | |
| All | 642 | 590 | −8 | 385 | 227 | −41 | 257 | 363 | 41 |
| Cardiovascular disease | 141 | 151 | 7 | 96 | 42 | −56 | 45 | 109 | 142 |
| Malignancies | 71 | 113 | 59 | 29 | 25 | −14 | 42 | 88 | 110 |
| HIV/AIDS | 96 | 70 | −27 | 43 | 39 | −9 | 53 | 31 | −42 |
| Diabetes | 19 | 39 | 105 | 13 | 19 | 46 | 6c | 20 | 233 |
| Influenza and pneumonia | 39 | 23 | −41 | 22 | 7 | −68 | 17 | 16 | −6 |
| Chronic lower respiratory disease | 17 | 25 | 47 | 6 | 8 | 33 | 11 | 17 | 55 |
| Drug-related | 29 | 22 | −24 | 16 | 13 | −19 | 13 | 9 | −31 |
| Homicide | 43 | 18 | −58 | 40 | 10 | −75 | 3c | 8 | 167 |
| Liver disease | 21 | 16 | −24 | 19 | 11 | −42 | 2c | 5c | 150 |
| External causes | 8 | 7 | −13 | 8 | 6 | −25 | 0c | 1c | – |
| Renal disease | 14 | 11 | −21 | 2c | 7 | 250 | 12 | 4c | −67 |
| Septicaemia | 21 | 12 | −43 | 10 | 5 | −50 | 11 | 7 | −36 |
| Other | 123 | 83 | −33 | 81 | 35 | −57 | 42 | 48 | 14 |
aCauses are ranked by the 1999–2001 MRs in the public housing population.
bAll MRDS are per 100,000 and rounded to the nearest whole number
cMRD is not statistically significantly from 0; all other MRDs are significantly different from 0
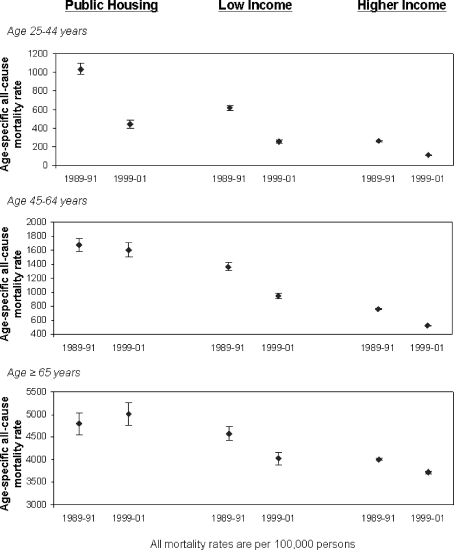
Age-Specific All-Cause Mortality Rates
MRs among 25–44-year-olds fell substantially and significantly from 1989–1991 to 1999–2001 among public housing, low-income, and higher-income populations (Figure 2). In contrast, in middle-aged (45–64 years) and older (≥65 years) adults, MRs declined significantly in low-income and higher-income populations, while no substantial or statistically significant decrease occurred in either of these age groups in the public housing population. To ensure that these trends in age-specific mortality rates were not caused by changing population age distributions, a sensitivity analysis was conducted with age adjustment (using 5-year strata) within each of the three age categories, showing no differences in the results (not shown). In each time period, the higher-income population had consistently lower age-specific all-cause MRs compared to the low-income population, which had consistently lower age-specific all-cause MRs compared to the public housing population.
FIGURE 2.
Age-specific, all-cause mortality rates for the public housing, low-income, and higher-income populations in New York City, 1989–1991 and 1999–2001.
Discussion
Age-adjusted, all-cause mortality in NYC neighborhoods decreased from 1989–1991 to 1999–2001, with the greatest decrease in residents of low-income neighborhoods (28%) and the smallest decrease in residents of public housing (16%). In addition to the decrease in mortality, we found a narrowing mortality disparity between nongentrifying low-income and higher-income neighborhoods, consistent with a prior study comparing community districts.16 In contrast, the public housing population appears to have lagged behind NYC’s overall mortality improvements of the 1990s and by the end of that decade had an age-adjusted all-cause mortality rate nearly twice that of those living in higher-income neighborhoods. Deaths among those age ≥45 years from cardiovascular diseases and cancers amenable to prevention contributed substantially to this growing mortality gap. While our study does not provide definitive explanations for the disparity between public housing communities and other low-income communities or for its increase during the 1990s, our analysis suggests that selection factors and trends in population composition contributed. Whatever the explanation, the findings indicate that public housing residents should be a high priority for programs to reduce health disparities. In addition, our results illustrate the need for caution when using area-based measures to track population health disparities over time, especially for larger and more diverse neighborhoods.
The decrease in mortality in all three New York City population groups from 1989–1991 and 1999–2001 was greater than that observed nationally during the 1990s when age-adjusted mortality rates declined 7% overall.33 Mortality decreases during the 1990s that were especially relevant to urban populations include a decrease in homicides and in deaths due to HIV/AIDS with the introduction of highly active antiretroviral therapy in 1996.34 In addition, declines in these causes of death, cardiovascular, influenza, and pneumonia death rates also contributed to falling all-cause mortality in all three New York City populations tracked in our analysis.
We followed the recommendation of Krieger, et al. to use small areas (block groups in our case) to define SEP.1 By further stratifying census blocks in low-income areas into public housing and nonpublic housing subsets, two low-income populations were created with somewhat different demographic composition and population change over time, and with markedly different MRs and trends. Why should mortality be higher and improving more slowly in public housing residents?
Public housing provides apartments at affordable rents to hundreds of thousands of low-income New Yorkers. This subsidy should relieve the budgetary and psychological stress of high-housing costs, and this benefit could indirectly promote better health than would otherwise be the case. Our study did not, and could not, examine the health of public housing residents relative to what it would be without access to subsidized housing. Rather, for reasons discussed below, our findings suggest that at least part of the mortality disadvantage among public housing residents is due to the fact that in an increasingly expensive city, public housing serves as a stable and affordable refuge for the most disadvantaged and perhaps less healthy New Yorkers.
While nonpublic housing low-income census blocks had a substantially higher mean proportion of foreign-born residents than public housing census blocks, the foreign-born population increased by a larger proportion in public housing from 1990 to 2000. Recent immigrants may be healthier than the populations they join, especially those of later middle age.35 Health status could also differ among those who migrate domestically and those who do not. The public housing population had the highest percentage of households living in their residence for 5 years or more, and this percentage increased from 1990 to 2000. Because public housing households can transfer to another public housing unit or development for reasons such as household growth, this measure likely understates the relative stability of the public housing population in NYC. The declining population in public housing while nonpublic housing low-income neighborhoods grew is also consistent with public housing experiencing less in-migration. Relative to the rest of the city, there was a reduction from 1990 to 2000 in the number of residents aged 15–34 years in the public housing population and great stability in the population older than aged 35 years (Table 1). This pattern could reflect the “aging-in-place” of public housing residents who remain in public housing as their children move away and waiting lists that can last years, leaving few vacancies for younger families. Thus, the higher mortality in the relatively stable, public housing population, and its slower improvement compared to the other low-income populations in the city suggests that a time-varying compositional effect caused by in-migration of healthier populations may account for some of the decreased MR in nonpublic housing low-income populations.
The proportion of public housing census blocks that gentrified from 1990 to 2000 was less than the proportion of nonpublic housing low-income census blocks that gentrified (12% vs. 44%). However, this difference cannot account for the greater improvement in mortality in residents of nonpublic housing low-income census blocks because we excluded census block groups that experienced a substantial decrease in poverty concentration during that decade from our nonpublic housing low-income blocks. Even with this restriction, it is possible that there were unmeasured differences in gentrification between the public housing and nonpublic housing blocks. This could have happened if, for example, nonpublic housing low-income blocks had a larger influx of younger, upwardly mobile adults but still with low enough incomes to remain below the threshold we used for poverty.
Thus, our analyses suggest that the compositional and contextual components that characterize public housing neighborhoods may account for their mortality disadvantage in both time periods relative to other low-income neighborhoods and that their relatively stable composition over time may account for the slower improvement in mortality during the 1990s.4,36–38 There may be, of course, a variety of other compositional and contextual characteristics not examined in this study that could also contribute—aspects of the built and social environment of public housing, for example. But, whatever the underlying cause of the mortality differences, their magnitude calls for a public health response. Understanding the mediating factors linking social disadvantage to poor health in the public housing population is a prerequisite to informed intervention.39 A full exploration of such factors is beyond the scope of our data, but examining causes of death provides some clues. An increase in cancer mortality among public housing residents accounts for a growing proportion of mortality disparities in that population. Especially notable are substantial increases in potentially preventable deaths from prostate, lung, colon, and breast cancer. This finding is consistent with the proposition that disparities widen most for diseases amenable to prevention measures and suggests that gaps in access and/or use of cancer screening and smoking cessation services in the public housing population may have widened during the 1990s.40 With successes in increasing smoking cessation and access to colonoscopy in NYC since 2002, surveys of the public housing population should be considered to assess how well they have been reached by these efforts. More generally, an assessment of health risks, behaviors, and access in the public housing population might identify other opportunities for intervention to address preventable causes of premature death in this population.41
As the SEP of the residents was defined using area-based measures instead of individual-level information, the study is an ecological study and the usual limitations to interpreting findings from such a design apply. Caution should be used when generalizing findings to other urban areas due to the differences in the public housing sector. Also, the accuracy of census data could differ by neighborhood income or public housing status. In particular, underreporting of household size may be more common among public housing respondents, due to concerns around eligibility and program regulations. Evidence that this phenomenon was not particularly pronounced is that the mortality differences were greatest in the older age groups, though younger residents would be more likely to be underreported. Census block level assignment to public housing and nonpublic housing groups precluded individual-level race information in the MR denominator data because denominators jointly stratified by age and race are not available at the census block level. We do not think these limitations can account for the large mortality disparities we observed or for the relative lack of improvement in mortality over time in the public housing population. Race and ethnicity compositions in the neighborhood populations are fairly stable in 1990 and 2000, suggesting it is more than race and ethnicity driving the widening of the mortality disparity over this time period.
This analysis refines the previous mortality findings from an area-based investigation in NYC between 1989–1991 and 1999–200116 and tempers the encouraging observation that disparities in the health of poor and wealthy New Yorkers have narrowed. Eliminating health disparities is at the center of contemporary US public health policy, and these findings highlight a population in particular need of increased attention.42
Acknowledgment
This work was funded by the Josiah H. Macy Foundation and the Fund for Public Health in New York, Inc.
Conflicts of interest None
Footnotes
 |
References
- 1.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter?: the Public Health Disparities Geocoding Project. Am J Epidemiol. 2002; 156(5): 471–482 doi:10.1093/aje/kwf068. [DOI] [PubMed]
- 2.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures—the public health disparities geocoding project. Am J Public Health. 2003; 93(10): 1655–1671 doi:10.2105/AJPH.93.10.1655. [DOI] [PMC free article] [PubMed]
- 3.Murray CJ, Kulkarni SC, Michaud C, et al. Eight Americas: investigating mortality disparities across races, counties, and race-counties in the United States. PLoS Med. 2006; 3(9): e260 doi:10.1371/journal.pmed.0030260. [DOI] [PMC free article] [PubMed]
- 4.Macintyre S. What are spatial effects and how can we measure them? In: Dale A, ed. Exploiting national survey data: the role of locality and spatial effects. Manchester: Faculty of Economic and Social Studies, University of Manchester; 1997: 1–17.
- 5.Macintyre S, Maclver S, Sooman A. Area, class and health: should we be focusing on places or people? J Soc Policy. 1993; 22: 213–234 doi:10.1017/S0047279400019310. [DOI]
- 6.Duncan C, Jones K, Moon G. Context, composition and heterogeneity: using multilevel models in health research. Soc Sci Med. 1998; 46(1): 97–117 doi:10.1016/S0277-9536(97)00148-2. [DOI] [PubMed]
- 7.Duncan C, Jones K, Moon G. Health-related behaviour in context: a multilevel modeling approach. Soc Sci Med. 1996; 42(6): 817–830 doi:10.1016/0277-9536(95)00181-6. [DOI] [PubMed]
- 8.Diez-Roux AV, Link BG, Northridge ME. A multilevel analysis of income inequality and cardiovascular disease risk factors. Soc Sci Med. 2000; 50(5): 673–687 doi:10.1016/S0277-9536(99)00320-2. [DOI] [PubMed]
- 9.Diez-Roux AV. Multilevel analysis in public health research. Annu Rev Public Health. 2000; 21: 171–192 doi:10.1146/annurev.publhealth.21.1.171. [DOI] [PubMed]
- 10.Blalock HM. Contextual-effects models: theoretical and methodologic issues. Annu Rev Sociol. 1984; 10: 353–372 doi:10.1146/annurev.so.10.080184.002033. [DOI]
- 11.Ellaway A, Macintyre S. Does where you live predict health related behaviours?: a case study in Glasgow. Health Bull (Edinb). 1996; 54(6): 443–446. [PubMed]
- 12.Macintyre S, Ellaway A. Social and local variations in the use of urban neighbourhoods: a case study in Glasgow. Health Place. 1998; 4(1): 91–94 doi:10.1016/S1353-8292(97)00030-0. [DOI] [PubMed]
- 13.Sooman A, Macintyre S. Health and perceptions of local environment in socially contrasting neighbourhoods in Glasgow. Health Place. 1995; 1(1): 15–26 doi:10.1016/1353-8292(95)00003-5. [DOI]
- 14.Cheadle A, Wagner E, Koepsell T, Kristal A, Patrick D. Environmental indicators: a tool for evaluating community-based health-promotion programs. Am J Prev Med. 1992; 8(6): 345–350. [PubMed]
- 15.Office of Vital Statistics. Summary of vital statistics 2006: The city of New York. New York: NYC DOHMH; 2006.
- 16.Karpati AM, Bassett MT, McCord C. Neighbourhood mortality inequalities in New York City, 1989–1991 and 1999–2001. J Epidemiol Community Health. 2006; 60(12): 1060–1064 doi:10.1136/jech.2006.047100. [DOI] [PMC free article] [PubMed]
- 17.Elliott P, Wartenberg D. Spatial epidemiology: current approaches and future challenges. Environ Health Perspect. 2004; 112(9): 998–1006. [DOI] [PMC free article] [PubMed]
- 18.Bureau of the Census. FactFinder: Population Finder: New York city, New York. Bureau of the Census, US Department of Commerce 2007; Available at: http://factfinder.census.gov. Accessed on: May 23, 2007.
- 19.Gushulak B. Healthier on arrival? Further insight into the “healthy immigrant effect”. CMAJ. 2007; 176(10): 1439–1440 doi:10.1503/cmaj.070395. [DOI] [PMC free article] [PubMed]
- 20.McDonald JT, Kennedy S. Insights into the “healthy immigrant effect”: health status and health service use of immigrants to Canada. Soc Sci Med. 2004; 59(8): 1613–1627 doi:10.1016/j.socscimed.2004.02.004. [DOI] [PubMed]
- 21.Singh GK, Miller BA. Health, life expectancy, and mortality patterns among immigrant populations in the United States. Can J Public Health. 2004; 95(3): I14–21. [DOI] [PMC free article] [PubMed]
- 22.Freeman L, Branconi F. Gentrification and displacement: New York City in the 1990s. J Am Plann Assoc. 2004; 70(1): 39–52 doi:10.1080/01944360408976337. [DOI]
- 23.Congdon P. An analysis of population and social change in London wards in the 1980s. Trans Inst Br Geogr. 1989; 14(4): 478–491 doi:10.2307/623013. [DOI] [PubMed]
- 24.Morenoff JD, House JS, Hansen BB, Williams DR, Kaplan GA, Hunte HE. Understanding social disparities in hypertension prevalence, awareness, treatment and control: the role of neighborhood context. Soc Sci Med. 2007; 65(9): 1853–1866. [DOI] [PMC free article] [PubMed]
- 25.Harpham T, Stephens C. Policy directions in urban health in developing countries—the slum improvement approach. Soc Sci Med. 1992; 35(2): 111–120 doi:10.1016/0277-9536(92)90158-M. [DOI] [PubMed]
- 26.Swerdlow M. “Chronicity,” “nervios” and community care: a case study of Puerto Rican psychiatric patients in New York City. Cult Med Psychiatry. 1992; 16(2): 217–235 doi:10.1007/BF00117019. [DOI] [PubMed]
- 27.Bondi L. Geography and gender. Geogr Rev. 1989; 2(5): 2–6. [PubMed]
- 28.Fisher GM. The development and history of the poverty thresholds. Soc Secur Bull. 1992; 55(4): 3–14. [PubMed]
- 29.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Painting a truer picture of US socioeconomic and racial/ethnic health inequalities: the Public Health Disparities Geocoding Project. Am J Public Health. 2005; 95(2): 312–323 doi:10.2105/AJPH.2003.032482. [DOI] [PMC free article] [PubMed]
- 30.Krieger N, Waterman PD, Chen JT, Soobader MJ, Subramanian SV. Monitoring socioeconomic inequalities in sexually transmitted infections, tuberculosis, and violence: geocoding and choice of area-based socioeconomic measures—the public health disparities geocoding project (US). Public Health Rep. 2003; 118(3): 240–260. [DOI] [PMC free article] [PubMed]
- 31.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Choosing area based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: the Public Health Disparities Geocoding Project (US). J Epidemiol Community Health. 2003; 57(3): 186–199 doi:10.1136/jech.57.3.186. [DOI] [PMC free article] [PubMed]
- 32.Fay MP, Feuer EJ. Confidence intervals for directly standardized rates: a method based on the gamma distribution. Stat Med. 1997; 16: 791–801 doi:10.1002/(SICI)1097-0258(19970415)16:7<791::AID-SIM500>3.0.CO;2-#. [DOI] [PubMed]
- 33.Kung HC, Hoyert DL, Xu J, Murphy SL. Deaths: final data for 2005. National Vital Statistics Report; vol 56 no 10. Hyattsville: National Center for Health Statistics; 2008. [PubMed]
- 34.Palella FJ Jr, Delaney KM, Moorman AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998; 338(13): 853–860 doi:10.1056/NEJM199803263381301. [DOI] [PubMed]
- 35.Gee EM, Kobayashi KM, Prus SG. Examining the healthy immigrant effect in mid- to later life: findings from the Canadian Community Health Survey. Can J Aging. 2004; 23(Suppl 1): S61–S69. [PubMed]
- 36.Jenks C, Mayer SE. The social consequences of growing up in a poor neighborhood. In: McGeary M, ed. Inner-city poverty in the United States. Washington, D.C.: National Academy Press; 1990: 111–186.
- 37.Mayer SE, Jencks C. Growing up in poor neighborhoods: how much does it matter? Science. 1989; 243(4897): 1441–1445 doi:10.1126/science.243.4897.1441. [DOI] [PubMed]
- 38.Susser M, Susser E. Choosing a future for epidemiology: II. From black box to Chinese boxes and eco-epidemiology. Am J Public Health. 1996; 86(5): 674–677 doi:10.2105/AJPH.86.5.674. [DOI] [PMC free article] [PubMed]
- 39.Oakes JM. The (mis)estimation of neighborhood effects: causal inference for a practicable social epidemiology. Soc Sci Med. 2004; 58(10): 1929–1952 doi:10.1016/j.socscimed.2003.08.004. [DOI] [PubMed]
- 40.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;Spec No.:80–94 doi:10.2307/2626958. [DOI] [PubMed]
- 41.Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Soc Sci Med. 2002; 55(1): 125–139 doi:10.1016/S0277-9536(01)00214-3. [DOI] [PubMed]
- 42.US Department of Health and Human Services. Healthy People 2010: understanding and improving health. 2nd edn. Washington, D.C.: Government Printing Office, US Department of Health and Human Services; 2007.