Abstract
We conducted an epidemiologic study to understand temporal and spatial patterns of hemorrhagic fever with renal syndrome (HFRS) in the Republic of Korea (ROK). We estimated the incidence among civilians in endemic areas through the active surveillance system during the major epidemic periods, from September to December, between 1996 and 1998. We also estimated the prevalence among Korean military personnel from 1995 to 1998. In addition, we assessed seroprevalence, subclinical infection rate, and vaccination rates in both civilians and military personnel. The incidence in civilians ranged from 2.1 to 6.6 per 100,000 person-months. The annual prevalence in the military personnel was 40-64 per 100,000 military populations, and remained generally constant throughout the study period with seasonal variation. This is the prospective epidemiologic data set on HFRS in the ROK since the inactivated Hantaan virus vaccine was licensed for use in the late 1990s. These results will be invaluable in establishing a national immunization program against HFRS.
Keywords: Hemorrhagic Fever with Renal Syndrome, Hantaan virus, Epidemiology, Incidence, Prevalence, Korea
INTRODUCTION
Hemorrhagic fever with renal syndrome (HFRS), caused by Hantaviruses (family Bunyaviridae, genus Hantavirus), is a rodent-borne zoonosis widely distributed over Europe and Asia. More than 20 strains of Hantaviruses are known worldwide, but not all strains are associated with human disease. Among Hantaviruses, the major causative agents are Hantaan, Seoul, and Puumala viruses (1-3). In the Republic of Korea (ROK), both Hantaan and Seoul viruses are known as the etiologic agents of HFRS. These viruses establish chronic infections in certain species of rodents and are transmitted to man primarily via aerosols or fomites from feces, urine, and saliva of infected mice (2-4). Hantaan virus, carried by Apodemus agrarius and Apodemus peninsulae, causes a severe form of HFRS and is mostly distributed in rural areas, whereas Seoul virus, carried by domestic (Rattus norvegicus and Rattus rattus) and laboratory rats, causes urban and laboratory-acquired cases respectively and may cause a milder clinical syndrome (5,6).
HFRS is characterized by a triad of fever, hemorrhagic manifestations including petechiae, and renal impairment, but there are marked variations in the severity, duration, and degree of each organ involvement. In general, patients complain of abrupt fever, eye symptoms, gastrointestinal symptoms, and other nonspecific constitutional symptoms. Therefore, diagnosis must be confirmed by serologic tests (3,7-9).
HFRS is one of the important acute febrile infections during autumn and a major public health problem in the ROK. It was recognized for the first time in Korea in 1951 among soldiers of the United Nations (10). The causative pathogen 'Hantaan virus' was discovered by Lee et al. in 1976 (5,11) and named after the Hantaan River crossing the endemic areas near the demilitarized zone (DMZ) between North and South Korea.
There are two epidemic periods of HFRS each year, the major (October-December) and minor epidemic periods (May-July). The majority of cases (more than 75% of patients) occur during the major epidemic period. Seoul virus infection is less seasonal in occurrence. There are two high-risk groups of HFRS; residents in the northern part of the country, who are mostly farmers, and Korean soldiers stationed in the field (9,12-14).
More than 500 HFRS cases were serologically confirmed and hospitalized annually in the 1980s (9). However, the number of the reported cases has gradually decreased to approximately 300-400 cases per year since it was legally designated as a communicable disease in 2000 (15). Nevertheless, the associated factors have not been defined. The inactivated Hantavirus vaccine (Hantavax®, Korean Green Cross, Korea) has been commercially available since October 1990. Since its adoption into the national immunization program in 1992, it has been widely distributed to public health centers and the Korean army. Because the vaccine has not been evaluated for efficacy in a controlled trial, the protective effect of the vaccine is still under debate (16-19). Moreover, there are only a few published data on the incidence or prevalence of HFRS (20).
In this study, we conducted an epidemiologic suwey of HFRS in the ROK. We estimated the incidence, prevalence, subclinical infection, vaccination rate, and seroprevalence in high-risk groups--civilians in the endemic areas and Korean military personnel.
MATERIALS AND METHODS
Study areas
Civilians
We developed a HFRS surveillance system in two neighboring endemic areas, Yeoncheon and Paju, with a population of approximately 55,000 and 178,000, respectively, where many cases of HFRS have been reported for the past years. These areas are typical farm villages, located in mountainous districts of the northernmost of Gyeonggi province. The Hantaan River flows through the southeast part of Yeoncheon (Fig. 1). Each village is served by a public health clinic that provides centralized support for the village-run immunization program and health care.
Fig. 1.
Study areas, Yeoncheon and Paju, which are located in the northernmost part of Gyeonggi province, Republic of Korea. ADL, armistice demarcation line (—); DMZ, demilitarized zone (---).
Military personnel
We collected and analyzed HFRS cases in Korean military troops throughout the country.
Study design
The research team included infectious disease specialists of Korea University Medical Center, two epidemiologists, a virologist, and a medical officer. Cases of HFRS were identified through active surveillance systems, described below. Seroepidemiologic surveys were carried before and after the major or minor epidemic period to assess subclinical infection rate and seroprevalence. Vaccination rates were also assessed in both study groups.
Definition
A confirmed case of HFRS was defined as a patient with symptoms and signs comparable to acute stage of HFRS and positive indirect immunofluorescent antibody test (IFA) for Hantaan virus: four-fold rising antibody titers or seroconversion in the paired sera. A case of subclinical infection was defined as a person who showed the positive IFA criteria without any history of febrile illness or vaccination. Seroprevalence at a point in time was represented as percentage of cases showing ≥1:32 with IFA in the unvaccinated population for the past three years.
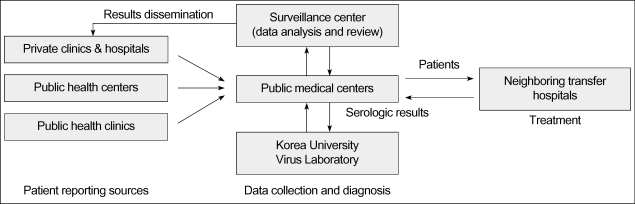
Active surveillance system
An active surveillance system was established in the Yeoncheon Medical Center from 1996 to 1998 and another was established in the Paju Public Health Center in 1998. The study period for each year was from September to December (Fig. 2). The system actively searched for acute febrile patients whose clinical features were compatible with HFRS. Reporting sources included the public health center and public health clinics, private clinics, and hospitals in each area. The study team regularly contacted reporting institutes once a week to elicit reports, including negative reports. Paired sera (acute and convalescent phases) were collected from all reporting patients for serologic tests. The study team also reviewed medical records of HFRS from six hospitals in adjacent areas to discover cases who might have escaped the surveillance system.
Fig. 2.
Active surveillance system for HFRS established in endemic areas.
As for the Korean military personnel, we used the HFRS surveillance system from January 1995 to December 1998, which had already been established in the Armed Forces Capital Hospital (AFCH); all HFRS cases, including suspected cases, in the military troops were to be sent to the AFCH. We reviewed medical records of the reported cases.
Seroepidemiologic surveys
Surveys in civilians were conducted in both Yeoncheon and Paju areas during the major epidemic periods from 1997 to 1998. Paired sera were obtained in August and the following February of each year. Written questionnaires were given to each subject. The questionnaire included past history of HFRS, HFRS vaccination for the past three years, and any febrile illness experienced during the study periods.
As for the military personnel, paired sera were obtained from the unvaccinated, healthy volunteers in March and in August 1995 for the minor epidemic period and in August 1996 and in February 1997 for the major epidemic period. Subclinical infection rates were calculated per epidemic period.
Vaccination records
Since vaccination for HFRS has been done exclusively at public health centers and public health clinics, we reviewed HFRS vaccination records of civilians (≥20 yr-old) from the public health centers in Yeoncheon (1996 to 1998) and Paju (1997 to 1998). As for the military personnel, we reviewed vaccination records of four divisions in which more than 10 cases of HFRS per year have been reported during the past five years.
Serologic test
Indirect immunofluorescent antibody assay for Hantaan virus was performed by an expert at the Institute of Viral Diseases, Korea University, Seoul, ROK (21). Serum samples with titers ≥1:32 were considered positive, but paired sera were required to assess current or subclinical infection.
Data analysis
Incidence in civilians of Yeoncheon was calculated for the major epidemic periods from 1996 to 1998 by taking the number of new HFRS cases reported during the study period and dividing by the four-month Yeoncheon population; represented as 100,000 person-months. Incidence in those of Paju was calculated similarly. The annual prevalence in the military personnel was calculated from 1995 to 1998 by taking all the HFRS cases reported each year and dividing by the 100,000 military populations. 95% confidence intervals of each estimate (incidence or prevalence) were calculated using the standard errors in each year in a region.
Incidence = Number of new HFRS case during September to December in a year / Population at Risk in a region during the same period [person-months]
Prevalence in military personnel = Number of total cases among the military personnel / Total number of military personnel
RESULTS
Surveillance
Civilians
In Yeoncheon, the active surveillance system identified 43 acute febrile patients in 1996; 29 cases were followed up and 5 cases were verified as HFRS. In 1997, 104 acute febrile patients were initially reported; 45 cases were followed up and 7 were confirmed as HFRS. In 1998, 99 acute febrile patients were initially enrolled; 33 cases were followed up and 5 patients were finally diagnosed as HFRS. An additional 9 HFRS cases were found by reviewing medical records of neighboring hospitals.
In Paju, 39 acute febrile patients were enrolled in 1998 and 5 of them were confirmed as HFRS. An additional 10 patients were found by reviewing medical records. More than 70% of the patients with HFRS were male (male:female=29:12), with the average age being forty-four years (range, 15 to 93). Annual population estimates were obtained from the provincial health department. The population size of Yeoncheon during the study period was approximately 55,000. The number of inhabitants in Paju was approximately 178,000 in 1998.
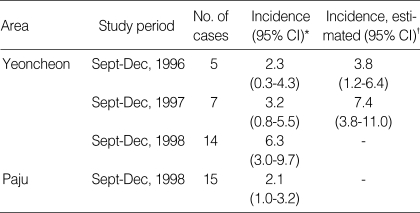
The incidence in Yeoncheon, from 1996 to 1998, ranged from 2.3 to 6.6 per 100,000 person-months. The incidence in Paju in 1998 was 2.1 per 100,000 person-months. The incidence was highest in 1998; there also were several cases admitted to neighboring hospitals. In order to take follow-up loss cases into account, we calculated the estimated incidence. The estimated incidence rates in Yeoncheon in 1996 and 1997 were 3.9 and 7.6 per 100,000 person-months, respectively (Table 1). Since a large number of cases were detected outside the active surveillance system in 1998, we could not assess the estimated incidence. Among the HFRS cases, none of them had history of vaccination against HFRS and only 1 patient died of the disease.
Table 1.
Incidence of HFRS in civilians from endemic areas during the study periods (1996-1998)
*Incidence rate is presented as 100,000 person-months. †Estimated incidence rate of HFRS cases when follow-up loss cases are taken into account.
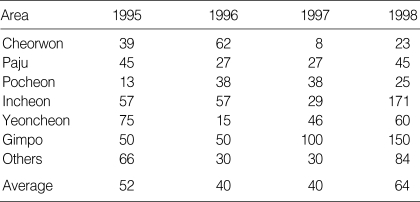
Military personnel
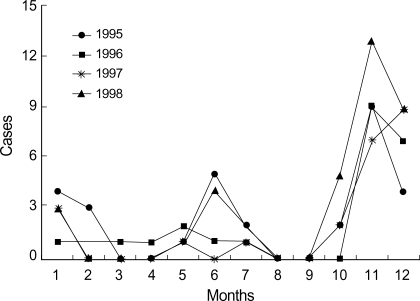
We assessed the annual prevalence of HFRS in Korean military personnel from 1995 to 1998 by analyzing the data obtained from the preexisting HFRS surveillance system in the AFCH. The annual prevalence varied from 40 to 64 per 100,000 military populations during the study years (Table 2). The highest prevalence was observed in 1998. The cases occurred predominantly during November and December each year. Noticeably, minor peaks were also observed in 1995 and 1998 (Fig. 3).
Table 2.
Annual prevalence of HFRS in Korean military personnel (1995-1998) (cases per 100,000)
Fig. 3.
Monthly distribution of HFRS cases among Korean military personnel (1995-1998).
Subclinical infection of Hantaan virus infection and its seroprevalence
Civilians
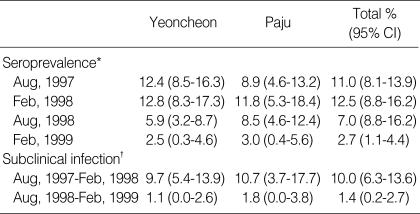
Seroepidemiologic surveys were performed among civilians in the endemic areas in 1997 and 1998. Serum samples and questionnaires were collected from volunteers in August and the following February each year. Seroprevalence of Hantaan virus antibodies before and after the major epidemic period were 11.0% (49/444) and 12.5% (38/304) in 1997, and 7.0% (34/486) and 2.7% (10/369) in 1998, respectively. There were no significant differences between the study areas (Table 3).
Table 3.
Seroprevalence and subclinical infection rate (%; 95% CI) of HFRS among civilians living in two endemic areas before and after the major epidemic period (1997-1998)
*% of civilians with positive serologic tests, but had no HFRS vaccination for the previous three years. †% of civilians with seroconversion or four-fold rising antibody titer in paired sera, but had no vaccination and clinical symptoms and signs for HFRS.
The subclinical infection rates during the major epidemic periods varied from 10.0% (26/261) in 1997 to 1.4% (5/348) in 1998 (Table 3). All subclinical cases showed seroconversion with reciprocal antibody titers ranging from 64 to 1,024. Three exceptional cases in which more than a four-fold rise in antibody titer were observed.
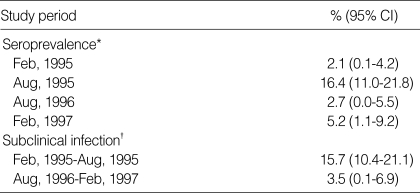
Military personnel
To investigate seroprevalence and subclinical infection, a total of 200 unvaccinated healthy personnel were recruited in the beginning of the study. Serum samples were collected in February and August 1995 for the minor epidemic period, and in August 1996 and February 1997 for the major epidemic period. Seroprevalence after the minor epidemic period in 1995 increased markedly from 2.1% (4/187) in February to 16.4% (30/183) in August. As for the major epidemic period in 1996, the seroprevalence rose from 2.7% (3/115) to 5.2% (6/116).
The subclinical infection rate for the minor epidemic period in 1995 was 15.7% whereas the rate for the major epidemic period in 1996 was 3.5% (Table 4). The higher seroprevalence and subclinical infection rate after the minor epidemic period in 1995 suggest an increase in disease activity during this interval.
Table 4.
Seroprevalence and subclinical infection rates of HFRS in Korean military personnel (1995-1996)
*% of military personnel with a positive serologic test. †% of military personnel with seroconversion or four-fold rising antibody titer in paired sera.
Vaccination rate
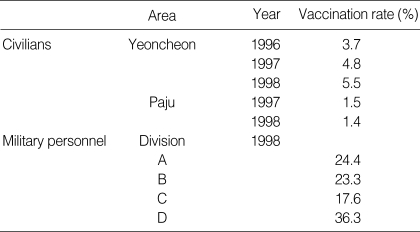
Civilians
The annual vaccination rate among civilians in Yeoncheon ranged from 3.7 to 5.5% between 1996 and 1998; in Paju, it ranged from 1.4 to 1.5% between 1997 and 1998 (Table 5). The vaccination rate was highest in subjects aged between 60 and 70 yr, especially in men.
Table 5.
Vaccination rates in civilians*and military personnel
*≥20 yr of age.
Military personnel
Since accessibility to vaccination records of military was limited, we were only able to assess vaccination rates of four divisions stationed in endemic areas. The vaccination rate ranged from 17.6% to 36.3% which was much higher than that of the civilian population (Table 5).
DISCUSSION
This is the prospective study that describes the epidemiology of HFRS in the ROK. This study determines the incidence, prevalence, seroprevalence, and subclinical infection rate in two high-risk groups, civilians in endemic areas and military personnel, during the epidemic months of the year. We identified HFRS cases through the active surveillance systems established in the endemic areas and the Korean troops. The incidence in the civilian group ranged from 2.1 to 6.6 per 100,000 person-months during the major epidemic period from 1996 to 1998. The estimated incidence rates rose to 3.9-7.6 per 100,000 person-months in Yeoncheon, when the follow-up loss cases were taken into account. Considering higher male to female ratio in the follow-up loss cases, the incidence might have been even higher since HFRS was more common among males, predominantly between 20 to 60 yr old (7).
During the 3-yr study period, HFRS showed the peak incidence in 1998. Although the surveillance system was expected to find all HFRS cases within the study area, a significant numbers of cases were detected outside the active surveillance system. Severe cases showing typical clinical features of HFRS are likely to escape the surveillance system, because many of them are directly admitted to university hospitals by their family members who are well aware of the clinical manifestations of the disease. Accordingly, it was important to review the medical records of neighboring hospitals to detect additional HFRS cases. On the other hand, the active surveillance system is important in detecting the mild to moderate HFRS cases, which are more likely to go undetected without the serologic confirmation.
We estimated the prevalence of HFRS instead of incidence in Korean military personnel because there were limitations in access to the vaccination records. The annual prevalence from 1995 to 1998 was 40-64 per 100,000 military personnel, based on detection of the hospitalized cases. The hospital-based surveillance system for HFRS has been maintained in the AFCH since the 1980s; any symptomatic patients suspected to have HFRS are to be transferred and admitted to the AFCH. Review of the surveillance data from the ROK Army showed that the reported cases have distinctly decreased over the past years: from 166 to 73 cases (average, 130 cases) per year between 1981 and 1990, and from 59 to 23 cases per year (average, 37 cases) between 1991 and 1998. HFRS has been categorized as a reportable disease since 1997. Although incidence or prevalence studies have not been performed previously, it has been reported that more than 500 cases of HFRS were serologically confirmed annually among civilians and Korean military personnel in the 1980s (9). There was some confusion or misunderstanding in the cited data for hospitalized civilian cases, rising to approximately 1,000 HFRS cases during the early 1990s; serologic tests were performed at several institutes with the samples from the same patient and each of the results were counted separately and then erroneously summed.
The reasons for the recent decrease in HFRS in the ROK have not been evaluated in depth. Possible related factors are improvement in the standard of living and housing in rural areas, ecological changes in rodent populations or other natural factors, and/or the effect of vaccination. The annual vaccination rates in civilians older than 20 yr old in the endemic areas were 1.4-5.5% during the study period. The vaccination rate in the military personnel from the 4 divisions of the Army in 1998 was much higher than civilians, ranging from 17.6 to 30%. Interestingly, the declining trend in the reported HFRS cases in the ROK Army in recent years is coincident with the start of vaccination in 1991. However, the effectiveness of HFRS vaccine should be evaluated in clinical trials.
There were mild fluctuations in HFRS incidence during the study period possibly related to the size of infected rodent population, climate, outdoor activities, and exploitation of fields and mountains. A seroepizootiologic study has reported annual fluctuating rodents' population in recent years (22). The number of rodents trapped in 29 widely separated areas, including Apodemus agrarius and Apodemus peninsulae, was larger in 1997 and 1998, compared with those in 1996. The overall Hantavirus seroprevalence in trapped rodents was 13.1 to 13.6%.
Seasonal variation of HFRS is clearly observed in the military personnel, with the major peak occurring between October and December and the minor peak between May and July, which is consistent with previous reports. HFRS occurs throughout the year, but more than 85% of cases occurred during the major and minor epidemic periods (3,7,9).
In our seroepidemiologic study, seroprevalence and subclinical infection rates among civilians and military personnel varied every year. The incidence of HFRS was high during the 1998 epidemic period and this seems to be due to low seroprevalence (7.0%) in the civilians before the epidemic. Relatively low incidence of HFRS during the 1997 epidemic can be related to relatively higher seroprevalence of 11%, which might have conferred immunity to HFRS. Song reported previously that relatively high subclinical infection rates after big outbreaks played a significant role in decreasing the incidence of HFRS (23). As shown in our data, seroprevalence or subclinical infection rates in the civilian population were higher than those of the military personnel population. This might be due to perennial exposure of the civilian population to the high-risk environments compared to the military personnel who are exposed to the environment for, at most, three years during their enlistment. Interestingly, the highest subclinical infection rate of 15.7% and relatively high reported cases found in the military personnel during the minor epidemic period in 1995 could be due to possible mass exposure to a common source of infection. Seroprevalences of HFRS in the neighboring countries were comparable: 12% in rural China (24) and 6.2% in Taiwan (25).
According to the Korean CDMR (Communicable Disease Monthly Report), the reported cases of HFRS have slightly increased since 1999. 392 cases were reported in 2003 and, contrary to previous reports, many of them occurred in the southwestern area of the country (15). However, the CDMR also included suspected cases in its analysis. Therefore, close observation is required in the following years.
A limitation of this study is that the analysis of the civilian population included data from only a 4 month period, from September to December. This limitation is difficult to overcome because long-term surveillance of rural civilian populations is technically challenging. Therefore, to get around this problem, we determined the exact incidence during the major epidemic periods when more than 75% of cases occur. Because of the limitation of this study design, we represented the incidences in civilians as person-months. However, the active surveillance system for the military personnel was in place year-round, making it possible to assess annual prevalence in military personnel.
Our data indicate that the incidence of HFRS in civilian populations in endemic areas varies every year, depending on the local seroprevalences and subclinical infection rates. Since rodents are major reservoirs for transmissions of Hantaan virus, the seroprevalence of the rodent population should be determined. Furthermore, the annual population cycle should also be determined to see how it is linked to annual incidence of HFRS. As for the military personnel, the prevalence remained generally the same throughout the study period with seasonal variations. Since the military personnel are a high risk group and the vaccination rate is about 30%, this population could be a good candidate for field trials. Our epidemiologic data on HFRS will be invaluable for establishing immunization strategies, immunization program policy, and vaccine efficacy studies.
Footnotes
This work was supported by grants from Korea Green Cross Corporation (KGCC).
References
- 1.Schmaljohn CS, Hasty SE, Dalrymple JM, LeDuc JW, Lee HW. Antigenic and genetic properties of viruses linked to hemorrhagic fever with renal syndrome. Science. 1985;227:1041–1044. doi: 10.1126/science.2858126. [DOI] [PubMed] [Google Scholar]
- 2.LeDuc JW. Epidemiology of Hantaan and related viruses. Lab Anim Sci. 1987;37:413–418. [PubMed] [Google Scholar]
- 3.Lee HW, van der Groen G. Hemorrhagic fever with renal syndrome. Prog Med Virol. 1989;36:62–102. [PubMed] [Google Scholar]
- 4.Tsai TF. Hemorrhagic fever with renal syndrome: mode of transmission to humans. Lab Anim Sci. 1987;37:428–430. [PubMed] [Google Scholar]
- 5.Lee HW, Lee PW, Johnson KM. Isolation of the etiologic agent of Korean hemorrhagic fever. 1978. J Infect Dis. 2004;190:1711–1721. doi: 10.1093/infdis/190.9.1711. [DOI] [PubMed] [Google Scholar]
- 6.Lee HW, Johnson KM. Laboratory-acquired infections with Hantaan virus, the etiologic agent of Korean hemorrhagic fever. J Infect Dis. 1982;146:645–651. doi: 10.1093/infdis/146.5.645. [DOI] [PubMed] [Google Scholar]
- 7.Lee JS. Clinical feature of hemorrhagic fever with renal syndrome in Korea. Kidney Int. 1991;40(Suppl 35):88–93. [PubMed] [Google Scholar]
- 8.Lee JS. Clinical manifestations and treatment of HFRS and HPS. In: Lee HW, Calisher C, Schmaljohn CS, editors. Manual of hemorrhagic fever with renal syndrome and hantavirus pulmonary syndrome. Seoul: WHO Collaborating Center for Virus Reference and Research (Hantaviruses) Asan Institute for Life Science; 1999. pp. 18–27. [Google Scholar]
- 9.Lee HW. Hemorrhagic fever with renal syndrome in Korea. Rev Infect Dis. 1989;11(Suppl 4):864–876. [PubMed] [Google Scholar]
- 10.Smadel JE. Epidemic hemorrhagic fever. Am J Public Health. 1953;43:1327–1330. doi: 10.2105/ajph.43.10.1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee HW, Lee PW. Korean hemorrhagic fever 1, demonstration of causative antigen and antibodies. Korean J Intern Med. 1976;19:371–383. [Google Scholar]
- 12.Hwang YJ, Park JH, Yeh MH, Dixon KE. A case-control study of risk factors for hemorrhagic fever with renal syndrome. Korean J Epidemiol. 1994;16:41–53. [Google Scholar]
- 13.Yang CW, Jang DH, Cho YH. Epidemiologic study of hemorrhagic fever with renal syndrome in Korean military: 1985-1990. Korean J Intern Med. 1987;42:802–808. [Google Scholar]
- 14.Lee M. Hemorrhagic fever with renal syndrome (Korean hemorrhagic fever) Rinsho Ketsueki. 1987;28:496–504. [PubMed] [Google Scholar]
- 15.Korea Center for Disease Control and Prevention (KCDC) Recent trends in notifiable disease occurrence based on the data of 2003. Communicable Disease Monthly Report, Korea. 2004;15:130–151. [Google Scholar]
- 16.Lee HW, Kwon EH, Park SC, Cheong HJ, Kim WJ, Jeong EK. Policy on vaccine and vaccination in Korea. J Nat Academy Science. 1999;38:1–75. [Google Scholar]
- 17.Sohn YM, Rho HO, Park MS, Kim JS, Summers PL. Primary humoral immune responses to formalin inactivated hemorrhagic fever with renal syndrome vaccine (Hantavax): consideration of active immunization in South Korea. Yonsei Med J. 2001;42:278–284. doi: 10.3349/ymj.2001.42.3.278. [DOI] [PubMed] [Google Scholar]
- 18.Park KH, Kim CS, Moon KT. Protective effectiveness of hantavirus vaccine. Emerg Infect Dis. 2004;10:2218–2220. doi: 10.3201/eid1012.040684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cho HW, Howard CR, Lee HW. Review of an inactivated vaccine against hantaviruses. Intervirology. 2002;45:328–333. doi: 10.1159/000067925. [DOI] [PubMed] [Google Scholar]
- 20.Lee M. Epidemiology. In: Lee M, editor. Korean hemorrhagic fever (Hemorrhagic fever with renal syndrome) Seoul: Seoul National University Press; 1986. pp. 27–48. [Google Scholar]
- 21.Niklasson B. Virus detection and identification with serological test. In: Lee HW, Calisher C, Schmaljohn CS, editors. Manual of hemorrhagic fever with renal syndrome and hantavirus pulmonary syndrome. Seoul: WHO Collaborating Center for Virus Reference and Research (Hantaviruses) Asan Institute for Life Science; 1999. pp. 80–121. [Google Scholar]
- 22.Baek LJ, Song JW, Song KJ. Seroepizoonotiology of Hantavirus infection in indigenous rodents in Korea, during 1995-2000. J Microbiol Biotechnol. 2002;12:53–58. [Google Scholar]
- 23.Song G. Epidemiological progresses of hemorrhagic fever with renal syndrome in China. Chin Med J. 1999;112:472–477. [PubMed] [Google Scholar]
- 24.Ruo SL, Li YL, Tong Z, Ma QR, Liu ZL, Tang YW, Ye KL, McCormick JB, Fisher-Hoch SP, Xu ZY. Retrospective and prospective studies of hemorrhagic fever with renal syndrome in rural China. J Infect Dis. 1994;170:527–534. doi: 10.1093/infdis/170.3.527. [DOI] [PubMed] [Google Scholar]
- 25.Kao CL, Chen CJ, Yen TS, Lien JC, Yang CS. Seroepidemiology of Hantaan virus infection in Taiwan. J Med Virol. 1996;50:309–313. doi: 10.1002/(SICI)1096-9071(199612)50:4<309::AID-JMV5>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]