Abstract
Background
There is a need for biomarkers insuring identification of septic patients at high-risk for death. We performed a prospective, multicenter, observational study to investigate the time-course of lipopolysaccharide binding protein (LBP) serum levels in patients with severe sepsis and examined whether serial serum levels of LBP could be used as a marker of outcome.
Methodology/Principal Findings
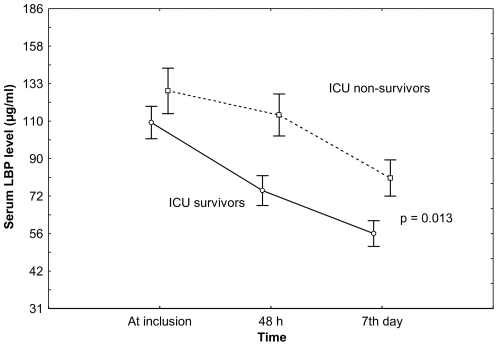
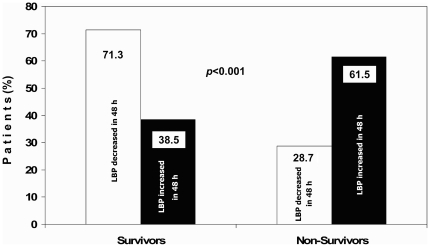
LBP serum levels at study entry, at 48 hours and at day-7 were measured in 180 patients with severe sepsis. Data regarding the nature of infections, disease severity, development of acute lung injury (ALI) and acute respiratory distress syndrome (ARDS), and intensive care unit (ICU) outcome were recorded. LBP serum levels were similar in survivors and non-survivors at study entry (117.4±75.7 µg/mL vs. 129.8±71.3 µg/mL, P = 0.249) but there were significant differences at 48 hours (77.2±57.0 vs. 121.2±73.4 µg/mL, P<0.0001) and at day-7 (64.7±45.8 vs. 89.7±61.1 µg/ml, p = 0.017). At 48 hours, LBP levels were significantly higher in ARDS patients than in ALI patients (112.5±71.8 µg/ml vs. 76.6±55.9 µg/ml, P = 0.0001). An increase of LBP levels at 48 hours was associated with higher mortality (odds ratio 3.97; 95%CI: 1.84–8.56; P<0.001).
Conclusions/Significance
Serial LBP serum measurements may offer a clinically useful biomarker for identification of patients with severe sepsis having the worst outcomes and the highest probability of developing sepsis-induced ARDS.
Introduction
Sepsis remains a major challenge in critical care medicine. It is the leading cause of death and its mortality has not decreased substantially in the past decade [1], [2]. An explosion of information regarding the inflammatory response to sepsis has prompted a search for biomarkers that help elucidate molecular pathways that are important in the pathogenesis of the septic process and acute lung injury, that predict outcome, and that may serve as surrogate indicators of potential benefits of therapies [3]–[8]. However, there is not convincing evidence to support the clinical use of any specific marker. Lipopolysaccharide binding protein (LBP), a key participant in the inflammatory response to infection, may be a useful marker for diagnosis and prognosis of patients with bacterial infections [9]. LBP is a type I acute phase response protein that is produced by hepatocytes, respiratory epithelial cells and a myriad of other cell types [10], and enhances the recognition of endotoxin and pathogens by the immune system [11]. LBP binds to Gram-negative bacteria via the lipid A part of the lipopolysaccharide (LPS) which mediates its binding to the CD14 cellular receptor molecule presented by monocytes and macrophages [12], [13]. Binding of LPS activates monocyte/macrophage system cells via Toll-like receptors [14], resulting in the production of pro-inflammatory cytokines that aggravate the clinical presentation of sepsis. In humans, LBP is constitutively present at a mean serum concentration of 5–20 µg/mL [15], [16], reaching peak levels higher than 200 µg/mL during the acute-phase reaction [5], [13], [17]. LBP also mediates the immune response to diverse pathogens including Gram-positive bacteria [18]. Thus, several studies have reported increased LBP serum levels in adult patients with sepsis caused by bacterial and fungal infections [13], [16]–[22]. However, some of those studies have shown conflicting results and others failed to show any correlation between blood levels and disease severity, most likely due to the limited number of patients with severe sepsis [13], [6]–[22] and/or the absence of follow-up LBP measurements [16], [17], [19]–[21].
In this study, using a large, multicenter cohort of patients meeting the international criteria for severe sepsis, we hypothesized that the pattern of LBP serum levels during the first week of severe sepsis development is a marker of severity and prognosis. The goals of this study were to determine: (i) whether there is a different pattern of LBP serum levels between survivors and non-survivors; (ii) the utility of monitoring LBP serum changes within the first 7 days of severe sepsis as a predictor of outcome, and (iii) whether LBP serum levels differ between patients who developed different degrees of lung injury.
Materials and Methods
Objectives
We analyzed the time-course of LBP serum levels in patients with severe sepsis to investigate the hypothesis that serial serum levels of LBP could be used as a marker of severity and outcome in patients with severe sepsis.
Ethics
The study was approved by the Ethics Committees for Clinical Research of the Hospital Universitario NS de Candelaria in Tenerife, Spain, and of the Hospital Universitario Río Hortega in Valladolid, Spain. Written informed consent was obtained from each patient or an appropriate proxy.
Participants
This multicenter, prospective, observational study included consecutive patients older than 18 years old fulfilling the International Sepsis Criteria for severe sepsis [23] admitted between April 2003 and March 2006 into a network of Spanish intensive care units (ICUs) (see appendix for a list of participating centers). We chose to study only patients with severe sepsis to guarantee severity of illness and a high risk for death. All patients were screened for severe sepsis on ICU admission and daily thereafter. Severe sepsis was defined as sepsis complicated by organ dysfunction [23]. We considered sepsis as a clinical syndrome defined by the presence of both infection and a systemic inflammatory response [23], [24]. Sepsis was microbiologically documented or clinically suspected as a result of the presence of white blood cells in a normally sterile body fluid, a perforated viscus, chest X-ray consistent with pneumonia and associated with purulent tracheal secretion, or other clinical syndromes associated with a high probability of infection. Clinically documented infection was defined by the presence of gross pus or an abscess, but no microbiological confirmation because of ongoing antibiotic therapy. Patients were enrolled into this study within the first 24 hours of meeting criteria for severe sepsis. Patients in whom decisions to withhold or withdraw life sustaining treatment were established within the first 24 hours of ICU admission, were excluded. All patients were screened on a daily basis for the presence of clinical and analytical signs of sepsis and, when indicated, cultures, biopsy or aspiration of the potentially infected sites were obtained. Patients were followed until ICU discharge or death.
As a general approach, and for the purpose of this prospective, observational, multicenter, cohort study, all participating physicians were urged to administer broad-spectrum antimicrobial agents in a timely manner, ensure early identification of causative microorganism, intravenous antibiotics as soon as sepsis was suspected or recognized, and to optimize antibiotic selection and timely administration on the basis of the antibiogram. For the ventilatory management, a tidal volume of 5–9 mL/kg predicted body weight at a ventilatory rate to maintain adequate PaCO2, and with PEEP and FiO2 combinations to maintain PaO2>60 mmHg or SpO2>90% were recommended. Fluid resuscitation and vasopressor administration were individualized. The goal was to maintain a systolic blood pressure ≥90 mmHg or a mean arterial pressure of ≥65 mmHg. It was recommended to maintain hemoglobin between 7–10 g/dl [25]. None of the patients in this cohort received activated protein C or low doses of corticosteroids as an adjunctive treatment.
Data collection
All data were collected on standardized forms by the clinicians responsible for the study in each ICU. Data collection included demographics, diagnoses, comorbidities, source of sepsis and isolated pathogens. Clinical and laboratory data needed to calculate the Acute Physiology and Chronic Health Evaluation (APACHE) II score were collected within the first 24 hours after ICU admission [26]. All patients enrolled in the present study were followed prospectively for the development of acute lung injury (ALI) and acute respiratory distress syndrome (ARDS), as defined by the American-European Consensus Conference [27]. In addition, number of organ failures included in the Sequential Organ Failure Assessment (SOFA) scale [28], date and time of inclusion into the study (fulfilled the criteria for severe sepsis), ICU and hospital length of stay, and ICU, hospital and 28-day mortality were recorded.
Blood sampling and laboratory analyses
Blood samples (5 mL) were collected within 24 hours of meeting severe sepsis criteria (baseline). Additional blood samples were obtained at 48 hours and at 7 days after study entry, only if the patient remained hospitalized into the ICU. Samples were centrifuged at 4°C for 10 min at 3200 rpm within 35 min after sampling. Three aliquots of serum were collected in cryovials and frozen and stored at −80°C. Participating centers shipped the tubes on dry ice to the research laboratory of the coordinating center. Serum LBP was assayed using a commercially available chemoluminescence fully automated immunoassay in an Immulite 1000 analyzer (Diagnostics Products Corporation, Siemens Medical Solutions, Germany). As stated by the manufacturer, the lower assay limit for the LBP assay was 0.2 µg/ml, and the calibration ranged was up to 200 µg/ml, having a 103 linear dynamic range. The described manufacturer within-run intra-sample coefficient of variation ranged from uppermost values of 5,8% for mean concentrations of 14 µg/ml to 3.3% for a concentration of 43 µg/ml. A dilution series was performed for those samples with initial values above the range limit. Single LBP serum measurements in each patient were determined by the same investigator (MM) who was blinded to the clinical parameters and outcome of patients.
We chose to test several markers within the inflammatory cascade in a subset of 107 patients in whom adequate serum was available. We measured four biomarkers that have pathogenetic basis in sepsis and ALI/ARDS [interleukin (IL)-6, IL-1-beta, IL-10, and C-reactive protein (CRP)] at study entry, at 48 h and at 7 days. Biomarkers levels were measured in duplicate using a commercial kit according to manufacturer's instructions: IL-6, IL-1-beta, and IL-10 (Siemens Medical Solutions Diagnostics, Caernarfon, UK) in an Immulite analyzer, and CRP (Roche Diagnostic, Basilea, Switzerland) in a Hitachi 917 analyzer.
Statistical analysis
Continuous variables are described as either a mean±standard deviation (SD), or as a median with interquartile range (IQR). Serum levels among different groups were compared by ANOVA or Student t-test. Categorical variables were compared using the Pearson's chi-square test. A logistic regression model with backwards elimination was used to predict disease outcomes by the variation of LBP levels at 48 hours (transformed into a simple 2 status categorical variable: increase or no-increase), adjusting for age, gender, number of organ failures, ARDS and APACHE II score. To compare the evolution of LBP and IL-6, IL-1-beta, IL-10, and RCP levels during the first week, a longitudinal analysis using a general linear model (GLIM) for repeated measures was used to test the variation of markers levels over time within and between groups. A Kaplan-Meier survival analysis was used to compare 28-day survival between patients with and without LBP increase at 48 hours of study enrollment. Finally, to validate and compare the LBP serum levels as a possible biomarker, receiver operator characteristic (ROC) curves and the area under the curves (AUC) were computed to determine the sensitivity/specificity pairs corresponding to particular LBP levels and APACHE II scores for the discrimination between survivors and non-survivors. Data were analyzed by using SPSS 15.0 for windows (SPSS Inc, Chicago, IL). A two-tailed P value<0.05 was considered significant.
Results
We enrolled 180 patients with severe sepsis. Main characteristics of the cohort are presented in Table 1. Mean age was 63.3±15 years and mean APACHE II score was 23.2±6.8. Patients had been hospitalized a median of 1 day (IQR: 0–7 days) prior to ICU admission and 54.4% had severe sepsis on ICU admission. Peritonitis was the leading cause of severe sepsis followed by pneumonia. Blood cultures were negative in 49.5% of cases. Most commonly isolated microorganisms were Gram-negative bacteria. Fifty-five percent developed ARDS and 31.1% developed ALI during hospitalization. Overall ICU mortality was 41.1% (Table 1).
Table 1. Main characteristics of 180 patients with severe sepsis.
| Variable | Patients (N = 180) | |
| Gender, male/female (%) | 59/41 | |
| Age (mean±SD) | 63±15 | |
| Severity (mean±SD) | ||
| APACHE II score | 23.2±6.8 | |
| SOFA score | 9.7±3.3 | |
| Number of organ failures | 2.3±1.3 | |
| White blood cells at study entry, 103 cells/mL | 16,8±9,6 | |
| ICU admission | ||
| Days between hospital and ICU admission, median (p25, p75) | 1 (0–7) | |
| Days between ICU admission and severe sepsis criteria, mean±SD | 1.6±3.1 | |
| Median ICU stay, days (p25, p75) | 7 (3–17) | |
| Identified Pathogen (%) | ||
| Positive blood cultures | 50.5 | |
| Gram-negative only | 25.0 | |
| Gram-positive only | 15.0 | |
| Fungi only | 2.8 | |
| Polymicrobial | 7.8 | |
| Source of infection (%) | ||
| Gastro-intestinal tract | 47.8 | |
| Respiratory tract | 36.1 | |
| Bone and soft tissue | 8.9 | |
| Genitourinary tract | 4.4 | |
| Catheter related | 2.8 | |
| Comorbid conditions (%) | ||
| Insulin-dependent diabetes | 7.8 | |
| Immunosuppression | 10.0 | |
| Lung injury (%) | ||
| ARDS | 55 | |
| ALI | 31 | |
| Outcome (%) | ||
| 28-day mortality | 40.5 | |
| ICU mortality | 41.1 | |
| Hospital mortality | 46.7 | |
APACHE: Acute Physiology and Chronic Health Evaluation; SOFA: sequential organ failure assessment; ICU: intensive care unit; ARDS: acute respiratory distress syndrome; ALI: acute lung injury.
The mean baseline LBP serum level was 122.5±74 µg/mL (range 26.9–334.0 µg/mL) without significant differences between age, gender, APACHE II score or source of infection. There were no statistical differences of LBP levels in relation to the causative pathogens at study entry: gram-negative infections (136.1±82.8), gram-positive infections (126.4±72.0 µg/ml), fungal infections (96.5±53.7 µg/ml), polymicrobial infections (135.2±73.0 µg/ml) (p = 0.385); at 48 hours: gram-negative infections (91.8±66.3 µg/ml), gram-positive infections (81.7±61.5 µg/ml), fungal infections (62.9±26.3 µg/ml), polymicrobial infections (105.5±63.2 µg/ml) (p = 0.714); and at 7 days: gram-negative infections (76.9±45.8 µg/ml), gram-positive infections (72.7±68.2 µg/ml), fungal infections (40.4±27.9 µg/ml), polymicrobial infections (69.6±49.2 µg/ml) (p = 0.865).Mean LBP levels decreased at 48 hours (93.7±66.8 µg/mL) and at day-7 (73.0±52.4 µg/mL). This decrease was significantly larger in patients who survived and in those who did not develop ARDS. The largest differences in LBP levels were found at 48 hours between patients who developed ARDS and ALI, and between survivors and non-survivors (P<0.0001, for both comparisons) (Table 2). Patients developing ARDS had the highest values of LBP.
Table 2. LBP serum levels among patients with different degrees of lung injury and in ICU survivors and non-survivors.
| Condition | Outcome | Baseline (N = 180) | 48 h (N = 147) | 7th Day (N = 100) |
| Lung Injury | ARDS (N = 99) | 132.5±76.5 | 112.5±71.8 | 79.3±56.1 |
| ALI (N = 56) | 116.4±72.2 | 76.6±55.9 | 68.8±46.9 | |
| non ALI/ARDS (N = 25) | 96.7±61.9 | 51.9±30.5 | 43.0±26.4 | |
| P-value* | 0.106 | <0.0001 | 0.076 | |
| ICU Survival | Survivors (N = 106) | 117.4±75.7 | 77.2±57.0 | 64.7±45.8 |
| Non-survivors (N = 74) | 129.8±71.3 | 121.2±73.4 | 89.7±61.1 | |
| P-value‡ | 0.249 | <0.0001 | 0.017 |
Values are expressed as mean±SD in µg/mL. LBP: lipopolysaccharide binding protein; ARDS: acute respiratory distress syndrome; ALI: acute lung injury; ICU: intensive care unit.
P- value from one way ANOVA.
P- value from t-test.
The GLIM test for repeated measures showed that LBP levels during the first week of severe sepsis clearly separated survivors from non-survivors (P<0.013) (Figure 1). The initial sample size of 180 patients at study entry was subsequently reduced to 147 patients at 48 hours and to 100 patients after one week due to either ICU death (16 patients at 48 h, 22 patients at day-7), ICU discharge alive (10 patients at 48 h, 26 patients at day-7) and/or non-available samples (7 patients at 48 h, 1 patients at day-7). We noted that patients with an ICU stay less than 48 hours had a higher mortality rate (57.6%, 19 out of 33) than the remaining patients in the study (37.4%, 55 out of 147) (p = 0.033). However, when patients with <48 hours ICU stay were compared to those with ≥48 hours ICU stay, there were no significant differences with regard to age (P = 0.457), gender (P = 0.205), lung injury (P = 0.248), source of infection (P = 0.446), or LBP serum levels at study entry (P = 0.792).
Figure 1. LBP serum levels in 180 patients with severe sepsis during the first week in the ICU.
Data are reported as mean (±SE). LPB: lipopolysaccharide-binding protein; ICU: intensive care unit. P-value was obtained using a general linear model.
IL-6, IL-1-beta, IL-10, and CRP levels in survivors and non survivors are summarized in Figure S1 (see supporting material). Using the same analyses that we used for LBP, none of those 4 biomarkers showed statistically significant differences among survivors and non-survivors across days examined. Furthermore, since the sample size of the subset of patients in whom we measured these additional markers was smaller (107 vs. 180 for LBP), for each of these markers we generated a simulated 180 patient dataset increasing artificially their sample size by adding measures from 73 randomly selected cases by resampling. Despite this correction, no statistical significant differences were found between survivors and non-survivors. For IL-6 (the marker with best significance level), the significance levels were p = 0.281 at study entry, p = 0.347 at 48 hours, and p = 0.082 at 7 days.
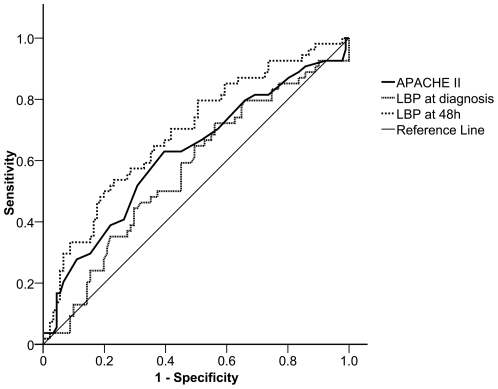
ROC curves and AUC (Figure 2) showed that LBP serum levels at 48 hours were a better predictor of outcome than the APACHE II score calculated within the first 24 h after ICU admission. The significance for APACHE II was P = 0.016 (AUC: 0.62; 95% CI: 0.52–0.71), for LBP at study entry was P = 0.173 (AUC: 0.57; 95% CI: 0.47–0.66) and for LBP at 48 hours was P<0.0001 (AUC: 0.71; 95%CI: 0.61–0.80).
Figure 2. Receiver operator characteristic (ROC) curves for discriminating survivors from non-survivors.
Curves were obtained according to lipopolysaccharide-binding protein (LBP) serum levels at study entry and at 48 h. ROC results using APACHE II scores on the day of ICU admission are also plotted for comparison. APACHE: Acute Physiology and Chronic Health Evaluation; ICU: intensive care unit.
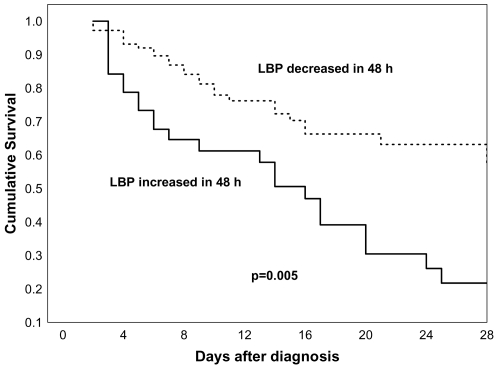
We noted that in 39 patients, LBP serum levels increased at 48 hours compared to baseline (mean increase 49.7 µg/mL) and their mortality was significantly higher than in the 108 patients in whom LBP decreased (mean decrease −52.9 µg/ml) [mortality 61.5% vs. 28.7%, respectively; odds ratio (OR) 3.97; 95% CI: 1.85–8.57, P<0.001] (Figure 3). Even after adjusting for age, gender, number of failing organs, and APACHE II score, an increase of LBP at 48 hours continued to predict a higher mortality risk (adjusted OR: 2.76; 95% CI: 1.16–6.54, P = 0.018).Kaplan-Meier 28-day survival curves showed strong significant differences between patients with or without increases in LBP levels at 48 hours (log rank test, P = 0.0001) (Figure 4).
Figure 3. Percentage of survivors and non-survivors patients with severe sepsis according to changes in LBP levels after 48 h of enrolment.
LPB: lipopolysaccharide-binding protein. P-value was obtained using chi-square test.
Figure 4. Kaplan-Meier curves for 28-day survival analysis of patients with severe sepsis.
In continuous line, patients in which lipopolysaccharide-binding protein (LBP) serum levels increased at 48 h; in discontinuous line, patients in which LBP did not increase at 48 h.
Discussion
The main finding of this study is that changes in LBP serum levels at 48 hours after the onset of severe sepsis were associated with disease severity and outcome. Our findings indicate that serial LBP serum measurements may offer a clinically useful biomarker for identification of patients, with severe sepsis, having the worst outcomes and the highest probability of developing sepsis-induced ARDS. In our study, as well as in previous studies [13], [22], serum LBP levels did not differ among patients with gram-negative, gram-positive or fungal infections. The mean LBP serum levels in our series are within the same range as in previous reports [13], [19], [22], [29]–[31].
Blairon et al [20] measured LBP serum levels daily until day 5 or death in a small sample of 24 patients with severe sepsis, but they were unable to demonstrate any correlation between LBP levels and severity, as defined by APACHE II, lung injury and multiple organ dysfunction scores. Prucha et al [13] assessed LBP levels at study entry and at 3- to 5-day intervals for 30 days or until death in a mixed population of 68 patients with systemic inflammatory response, sepsis or septic shock. However, they did not find significant differences in LBP levels between patients with systemic inflammatory response and sepsis or between survivors and non-survivors, since only 9 patients had severe sepsis and/or septic shock. Sakr et al [22] measured the time course of LBP levels in a mixed sample of 327 critically ill patients in which only 55 patients had severe sepsis. As in other previous studies with limited number of patients [13], [16], [30], they found that during the first two days of the disease process LBP concentrations were higher in patients with severe sepsis than in those without sepsis, although no further differences between these groups of patients were observed after the second day. Additionally, Sakr et al [22] concluded that the maximum LBP serum concentration during the first 3 days in the ICU discriminated between survivors and non-survivors, but they were unable to determine if such levels could discriminate between survivors and non survivors among patients with severe sepsis because of the limited sample size (n = 55).
The study by Opal et al [17] is the only published report with a sample size comparable to our study. They measured LBP plasma levels in 253 patients with severe sepsis and/or septic shock and reported mean LBP levels in the lower range of those not only in our series but also in other recent reports [13], [22], [29]. They found that LBP levels were less elevated in non-survivors than survivors. Although the mean APACHE II score in their series was similar to our series, the mortality of their cohort was lower (32.4%) than in our series or that reported in recent epidemiological studies [2], [32]–[35]. Several differences could explain the discrepancies between the two studies. First, the study by Opal et al was a secondary analysis of a population of septic patients selected from the placebo arm of a phase III randomized controlled trial to define the safety and efficacy of recombinant human interleukin 1 receptor antagonist in patients with sepsis [36]. Second, it is plausible that a selection bias occurred since the strict inclusion and exclusion criteria would select patients who were more likely to benefit by the drug under investigation. The observational and non-therapeutic nature of our study design allowed the inclusion of all consecutive patients meeting the criteria for severe sepsis with virtually no exclusion criteria, and therefore, we believe that our patients more closely represent those patients with severe sepsis managed in a routine ICU [35]. The later would explain why our patient population was sicker than the Opal et al. Third, the placebo (control) group in the parent paper by Fisher et al [36] consisted of 302 patients, from which (according to Table 4 in their paper) only 187 patients (62%) had dysfunction of one or more organs, a necessary criteria for being diagnosed as having severe sepsis. However, Opal et al included 253 patients out of those 302 (84%) as having severe sepsis. Forth, although the mean APACHE II score in the Opal et al study was apparently similar to our cohort (26 vs. 23), the magnitude of the standard deviations in both studies (13.6 vs. 6.8, respectively) showed more heterogeneity in their patient population than in our cohort (p = 0.005). Fifth, we do not have much information regarding the prevalence of acute respiratory failure and the use of mechanical ventilation in the Opal study. They reported that 27% of patients had ARDS whereas in our patient population, all patients were mechanically ventilated and 55% had ARDS. We are not surprised by the high prevalence of acute lung dysfunction in our series of severe sepsis since sepsis is the most common clinical condition associated with the development of ARDS and this relationship increases with sepsis severity. In addition, it has been reported that in more than half of patients with severe sepsis without ARDS there is an increased extravascular lung water content, representing subclinical and clinical lung injury [37]. Lastly, there is no enough information on how LBP assays were performed in the Opal et al paper to allow a comparison with our study. Since the data and blood sample collection in the two studies are separated by 15 years, we should acknowledge that differences in patient care, ICU admission policies, the nature of the patient mix, the use of retrospective analysis of data, methods of blood collection and shipping and the technology for LBP assays could explain discrepancies in the reported LBP values.
Our study is the first to report an association between LBP levels and severity of respiratory dysfunction and between LBP levels and outcome in patients with sepsis-induced ARDS. Only 19 ARDS patients were diagnosed during the first 48-hour of study entry; the rest were diagnosed later during ICU hospitalization. Thus, in most cases, the worsening of pulmonary dysfunction followed LBP increase. Martin et al [31] measured LBP concentrations in the bronchoalveolar lavage fluid (BAL) of 82 patients with ARDS. Although they found that LBP increased markedly in the BAL, LBP values were similar in all subgroups of patients and were not related to survival. Cunningham et al [38] assessed time-dependent changes in LBP serum concentrations in 121 trauma patients on hospital admission and at 24 h. In this very low-mortality group (16.3%), a significant increase in LBP concentration was observed at 24 h (28.0±25.3 vs.72.3±45.7 µg/mL). However, although baseline LBP levels were significantly greater in non-survivors than in survivors, after controlling for age and disease severity, LBP concentration did not predict survival. The major difference between those studies [31], [38] and ours is that they measured LBP levels within the first 24 h of admission to the ICU in a heterogeneous population of patients, whereas we performed serial measurements in a population of patients with the same clinical condition (severe sepsis).
In general, our findings and those from other previous reports [13], [16], [17], [19]–[22], [29], [30], [38] support the important role that LBP plays in host-defense during sepsis. In the current study, the variation of LBP concentrations at 48 h predicted worsening acute lung injury and death. We postulate that changes in biomarker levels during the course of severe sepsis may enable physicians to identify those patients who are most at risk for deterioration and who are in greatest need of early intervention. A close examination of changes in LBP serum levels at 48 h and their correlation with outcome enabled us to identify a subgroup of 39 patients (21.7%) in which significantly worse outcomes were observed. In those patients, rather than decreasing LBP levels at 48 h, as expected, the serum concentrations were higher than at onset [Note that these increments were not small (median: 49.7 µg/mL; IQR: 15.1–63.3 µg/mL)]. We cannot explain this finding but can speculate why these patients progressed toward a fatal outcome. During sepsis, LBP levels are modified by polymorphic genetic variation of the LBP gene [3], [39]–[41], predisposing these patients to excessive inflammation during an infection and contributing to a poor outcome. Chien et al [41] have recently reported that the presence of a common variant in the 5′ flanking region of the LBP gene was correlated with basal LBP serum levels in healthy controls and mortality in patients after allogeneic hematopoietic cell transplantation.
In our study, the changes in the systemic levels of IL-6, IL-1-beta, IL-10, and CRP were unable to discriminate survivors from non survivors during the first week of severe sepsis. In addition, LBP levels at 48 h performed better than APACHE II in predicting ICU outcome. The ROC curve showed that LBP at 48 h dominates APACHE II for any given sensitivity or specificity threshold. The APACHE II requires collection of data regarding numerous variables over a period of time (during the first 24 hours of ICU admission) taking into account the most abnormal values, relies on laboratory data that may be not uniformly collected, and its use is limited by significant inter- and intraobserver variability [42]. It has been reported that several factors influence the performance of severity of illness scoring system: lead time bias [43], case mix, pre-ICU or ICU management, sampling rate of laboratory and hemodynamic data [44], and novel advances in ICU care and therapy since scoring systems were described [26]. On the other hand, it is important to emphasize that the APACHE II score was developed to predict mortality in general ICU population using data during the first 24 hours of ICU stay. On average, patients from our study met severe sepsis criteria almost 2 days after ICU admission and we did not calculate APACHE II at the time patients met criteria for severe sepsis since it is unknown whether the use of APACHE scores generated at the time of patient enrolment result in under or over performance of APACHE II. We speculate that the main reason behind APACHE II not being a good predictor in severe sepsis could be due to APACHE II is a general purpose severity of disease classification system while LBP serum levels might have a more specific association with severe sepsis. Since APACHE II includes many physiological measurements that are not related with sepsis, it is plausible that it does not perform as well on a cohort of patients with severe sepsis in whom the main cause of death (multiple organ dysfunction) is attributed mainly to one factor (severe infection).
It is unlikely that the multifaceted nature of severe sepsis or ARDS would be only monitored with the use of a single biomarker. Microarray-based genome-wide gene expression analysis have shown in animal models that the induction of systemic inflammation by sepsis can cause synergistic effects with acute lung injury in the setting of mechanical ventilation, suggesting that molecules related to the innate immune pathway recognizing the endotoxin might be regulated as well in the presence of lung injury in the absence of infection [45]–[47]. In a recent metaanalysis, Wurfel [48] has indicated that across the different experiments, the most clearly overrepresented theme was “responses to pathogens”, noting that the selected genes for the final analyses were identified as differentially regulated in the presence of injury by mechanical ventilation alone. Given this evidence, and since our study have not been designed to answer the question of whether the LBP response is specific or typical of many acute phase proteins, we suggest that the response is, most likely, non-specific.
There are some limitations to our study. First, confirmatory studies with large sample sizes are required to validate this study. Second, despite the fact that changes in mean LBP levels discriminated survivors from non-survivors, our findings cannot define a cut-off point to clearly identify septic patients at 48 h who will survive from those who will not survive, nor clearly identify septic patients who will develop ARDS from those who will not develop it. Third, a drop off in the number of patients at 48 h (from 180 to 147) could affect the overall significance. However, we do not think that this event would have a major effect on the utility of LBP levels as a prognostic biomarker. It is plausible that those who died within the first 48 h had higher levels of serum LBP in the hours that preceded death, making the overall significance even greater if those values were considered at 48 h. Forth, different therapeutic regimes could influence the LBP values and their associated outcome. However, since it was beyond the scope of this study, we do not know whether treatment-dependent variables may influence the performance of our model under different practice patterns. None of the patients in this cohort received activated protein C or low doses of corticosteroids as an adjunctive treatment. As Kalil et al have recently evaluated [49], the strength of statistical and clinical evidence is weak for most clinical trials on therapies that have been recommended in recent guidelines for treating patients with severe sepsis, particularly for low dose steroids, recombinant human activated protein C, and early goal-directed therapy. Those authors have stated that it is essential to replicate those trials in confirmatory studies before guidelines can be fully adopted by clinicians. In fact, a new PROWESS trial is currently underway to test (and validate) the effects of activated protein C in a high risk septic population.
Our findings add additional justification for evaluating LBP in various high-risk populations during clinical trials. As Minter et al [50] have recently suggested, biomarkers may ultimately serve as targets for future therapeutic trials in severe sepsis whereas it seems essential to choose a biomarker defining appropriate high-risk populations in whom the initial immune inflammatory response is amplified beyond the threshold that is tolerated by the host. Serial monitoring of LBP serum levels may be an appropriate biomarker for subgroup selection and guiding of therapy. We also anticipate that pharmacologic modulation of LBP activation may represent a novel target for future therapeutic trials in the setting of severe sepsis.
In summary, the current study constitutes a step forward over previous published studies investigating the potential use of LBP as a biomarker in sepsis. We have found that a distinct pattern of elevated serum levels of LBP in patients with severe sepsis is strongly associated with increased mortality and the development of ARDS. Additional study is necessary, however, before this or any biomarker can be used to predict outcome in severe sepsis.
Supporting Information
Comparison of serum levels of IL-6, IL-1-beta, IL-10, and CRP in 107 patients with severe sepsis during the first week in ICU. Data are reported as mean (±SE). IL: interleukin; CRP: C-reactive protein; ICU: intensive care unit. P-value was obtained using GLIM.
(0.49 MB TIF)
Acknowledgments
GEN-SEP investigators are:
Villar J,a,b Espinosa E,c Sangüesa R,c Muros M,b,d Pérez-Méndez L,b,e Maca-Meyer N,e Tejera P,e Flores Cb,e, Blanch L,b,f Artigas A.b,f
aMultidisciplinary Organ Dysfunction Evaluation Research Network, Hospital Universitario Dr. Negrin, Las Palmas de Gran Canaria; bCIBER de Enfermedades Respiratorias, Spain; cDept. of Anesthesia, dDept. of Clinical Biochemistry, eUnidad de Investigación, Hospital Universitario N.S. de Candelaria, Santa Cruz de Tenerife, fCritical Care Center, Corporació Parc Taulí, Sabadell, Barcelona, Spain.
GRECIA investigators are:
Blanco J,a,b Muriel A,a Sagredo V,c Ballesteros JC,d Taboada F,d Muñiz G,d Gandía F,e Bobillo F,e Tamayo L,f Labattut AG,g Collado J,h Valledor M,i Antuña MT,i López MJ,j Cortina JJ,j Saldaña T,k Caballero A,k Álvarez T,k De Frutos M,l Guerra J,m Álvarez B,n Sandoval J.n
aMedicina Intensiva, Hospital Universitario Rio Hortega, Valladolid; bCIBER de Enfermedades Respiratorias, Spain; cMedicina Intensiva Hospital Clínico Universitario, Salamanca; dMedicina Intensiva, Hospital Central de Asturias, Oviedo; eMedicina Intensiva, Hospital Clinico Universitario, Valladolid; fMedicina Intensiva, Hospital Universitario Río Carrión, Palencia; gMedicina Intensiva, Hospital General de Soria, Soria; hMedicina Intensiva, Complejo Hospitalario de León, León; iMedicina Intensiva, Hospital San Agustín, Aviles; jMedicina Intensiva, Hospital General de Segovia, Segovia; kMedicina Intensiva, Hospital Virgen de la Concha, Zamora; lMedicina Intensiva, Hospital General Yagüe, Burgos; mMedicina Intensiva, Hospital de Cabueñes, Gijón; nMedicina Intensiva, Hospital del Bierzo, Ponferrada.
Footnotes
Competing Interests: Authors do not have any conflict of interest to declare in relation to this manuscript.
Funding: Supported by grants from FUNCIS (37/02) and Ministerio de Ciencia of Spain (SAF 2004-6833). CF was supported by an agreement between Instituto de Salud Carlos III and FUNCIS (EMER07/001) under ENCYT 2015 framework. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Friedman G, Silva E, Vincent JL. Has the mortality of septic shock changed with time? Crit Care Med. 1998;26:2078–2086. doi: 10.1097/00003246-199812000-00045. [DOI] [PubMed] [Google Scholar]
- 2.Engel C, Brukhorst FM, Bone HG, Brunkhorst R, Gerlach H, et al. Epidemiology of sepsis in Germany: results from a national prospective multicenter study. Intensive Care Med. 2007;33:606–618. doi: 10.1007/s00134-006-0517-7. [DOI] [PubMed] [Google Scholar]
- 3.Villar J, Maca-Meyer N, Pérez-Méndez L, Flores C. Understanding genetic predisposition to sepsis. Crit Care. 2004;8:180–189. doi: 10.1186/cc2863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McClintock D, Zhuo H, Wickersham N, Matthay MA, Ware LB. Biomarkers of inflammation, coagulation and fibrinolysis predict mortality in acute lung injury. Crit Care. 2008;12:R41. doi: 10.1186/cc6846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Salluh JIF, Bozza PT. Biomarkers of sepsis: lost in translation? Crit Care Med. 2008;36:2192–2194. doi: 10.1097/CCM.0b013e31817c0cd8. [DOI] [PubMed] [Google Scholar]
- 6.Lee PS, Patel SR, Christiani DC, Bajwa E, Stossel T, et al. Plasma gelsolin depletion and circulating actin in sepsis – A pilot study. PLoS ONE. 2008;3:e3712. doi: 10.1371/journal.pone.0003712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang Z, Chen F, Zhai R, Zhang L, Su L, et al. Plasma neutrophil elastase and elafin imbalance is associated with acute respiratory distress syndrome (ARDS) development. PLoS ONE. 2009;4:e4380. doi: 10.1371/journal.pone.0004380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shapiro NI, Trzeciak S, Hollander JE, Birkhahn R, Otero R, et al. A prospective, multicenter derivation of a biomarker panel to assess risk or organ dysfunction, shock, and death in emergency department patients with suspected sepsis. Crit Care Med. 2009;37:96–104. doi: 10.1097/CCM.0b013e318192fd9d. [DOI] [PubMed] [Google Scholar]
- 9.Schumann RR, Leong SR, Flaggs DW, Gray PW, Wright SD, et al. Structure and function of lipopolysaccharide binding protein. Science. 1990;249:1429–1431. doi: 10.1126/science.2402637. [DOI] [PubMed] [Google Scholar]
- 10.Dentener MA, Vreugdenhil ACE, Hoet PHM, Vernooy JHJ, Nieman FHM, et al. Production of the acute-phase protein lipopolysaccharide binding protein by respiratory type II epitelial cells. Implications for local defense to bacterial endotoxins. Am J Respir Cell Mol Biol. 2000;23:146–1453. doi: 10.1165/ajrcmb.23.2.3855. [DOI] [PubMed] [Google Scholar]
- 11.Vreugdenhil ACE, Dentener MA, Snoek AMP, Greve JWM, Buurman WA. Lipopolysaccharide binding protein and serum amyloid A sby human intestinal epithelial cells during the acute phase response1. J Immunol. 1999;163:2792–2798. [PubMed] [Google Scholar]
- 12.Grunwald U, Fan X, Jack RS, Workalemahu G, Kallies A, et al. Monocytes can phagocytose gram-negative bacteria by a CD-14 dependent mechanism. J Immunol. 1996;157:4119–4121. [PubMed] [Google Scholar]
- 13.Prucha M, Herold I, Zazula R, Dubska L, Dostal M, et al. Significance of lipopolysaccharide binding protein (an acute phase protein) in monitoring critically ill patients. Crit Care. 2003;7:R154–159. doi: 10.1186/cc2386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cohen J. The immunopathogenesis of sepsis. Nature. 2002;420:885–891. doi: 10.1038/nature01326. [DOI] [PubMed] [Google Scholar]
- 15.Gallay P, Barras C, Tobias PS, Calandra T, Glauser MP, et al. Lipopolysaccharide (LPS)-binding protein in human serum determines the tumor necrosis factor response of monocytes to LPS. J Infect Dis. 1994;170:1319–1322. doi: 10.1093/infdis/170.5.1319. [DOI] [PubMed] [Google Scholar]
- 16.Gaïni S, Koldkjaer OG, Pedersen C, Pedersen SS. Procalcitonin, lipopolysaccharide binding protein, interleukin-6 and C-reactive protein in community-acquired infections and sepsis: a prospective study. Crit Care. 2006;10:R53. doi: 10.1186/cc4866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Opal SM, Scannon PJ, Vincent JL, White M, Carroll SF, et al. Relationship between plasma levels of lipopolysaccharide (LPS) and LPS-binding protein in patients with severe sepsis and septic shock. J Infect Dis. 1999;180:1584–1591. doi: 10.1086/315093. [DOI] [PubMed] [Google Scholar]
- 18.Schröder NWJ, Morath S, Alexander C, Hamann L, Hartung T, et al. Lipoteichoic acid (LTA) of Streptococcus pneumoniae and Staphylococcus aureus cctivates immune cells via Toll-like receptor (TLR)-2, lipopolysaccharide-binding protein (LBP), and CD14, whereas TLR-4 and MD-2 are not involved. J Biol Chem. 2003;278:15587–15594. doi: 10.1074/jbc.M212829200. [DOI] [PubMed] [Google Scholar]
- 19.Sablotzki A, Borgermann J, Baulig W, Friedrich I, Spillner J, et al. Lipopolysaccharide binding protein (LBP) and markers of acute-phase response in patients with multiple organ dysfunction syndrome (MODS) following open heart surgery. Thorac Cardiovasc Surg. 2001;49:273–278. doi: 10.1055/s-2001-17803. [DOI] [PubMed] [Google Scholar]
- 20.Blairon L, Wittebole X, Laterre PF. Lipopolysaccharide binding protein serum levels in patients with severe sepsis due to gram-positive and fungal infections. J Infect Dis. 2003;187:287–291. doi: 10.1086/346046. [DOI] [PubMed] [Google Scholar]
- 21.Gaïni S, Pedersen SS, Koldkjær OG, Pedersen C, Moestrup SK, et al. New immunological serum markers in bacteraemia: anti-inflammatory soluble CD163, but not proinflammatory high mobility group-box 1 protein, is related to prognosis. Clin Exp Immunol. 2008;151:423–431. doi: 10.1111/j.1365-2249.2007.03586.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sakr Y, Burgett U, Nacul FE, Reinhart K, Brunkhorst F. Lipopolysaccharide binding protein in a surgical intensive care unit: a marker of sepsis? Crit Care Med. 2008;36:2014–2022. doi: 10.1097/CCM.0b013e31817b86e3. [DOI] [PubMed] [Google Scholar]
- 23.Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, et al. 2001 SCCC/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003;31:1250–1256. doi: 10.1097/01.CCM.0000050454.01978.3B. [DOI] [PubMed] [Google Scholar]
- 24.Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections. Am J Infect Control. 1988;16:128–140. doi: 10.1016/0196-6553(88)90053-3. [DOI] [PubMed] [Google Scholar]
- 25.Hebert PC, Wells G, Blajchman MA, Marshall J, Martin C, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med. 1999;340:409–417. doi: 10.1056/NEJM199902113400601. [DOI] [PubMed] [Google Scholar]
- 26.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: A severity of disease classification system. Crit Care Med. 1985;13:818–829. [PubMed] [Google Scholar]
- 27.Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, et al. The American-European Consensus Conference on ARDS: Definitions, mechanisms, relevant outcomes and clinical trial coordination. Am J Respir Crit Care Med. 1994;149:818–824. doi: 10.1164/ajrccm.149.3.7509706. [DOI] [PubMed] [Google Scholar]
- 28.Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med. 1998;26:1793–1800. doi: 10.1097/00003246-199811000-00016. [DOI] [PubMed] [Google Scholar]
- 29.Zweigner J, Gramm HJ, Singer OC, Wegscheider K, Schumann RR. High concentrations of lipopolysaccharide binding protein in serum of patients with severe sepsis or septic shock inhibit the lipopolysaccharide response in human monocytes. Blood. 2001;98:3800–3808. doi: 10.1182/blood.v98.13.3800. [DOI] [PubMed] [Google Scholar]
- 30.Gaïni S, Koldkjær OG, Møller HO, Pedersen C, Pedersen SS. A comparison of high-mobility group-box 1 protein, lipopolysaccharide-binding protein and procalcitonin in severe community-acquired infections and bacteraemia: a prospective study. Crit Care. 2007;11:R76. doi: 10.1186/cc5967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Martin TR, Rubenfeld GD, Ruzinski JT, Goodman RB, Steinberg KP, et al. Relationship between soluble CD14, lipopolysaccharide binding protein, and alveolar inflammatory response in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 1997;155:937–944. doi: 10.1164/ajrccm.155.3.9117029. [DOI] [PubMed] [Google Scholar]
- 32.Padkin A, Goldfrad C, Brady AR, Young D, Black N, Rowan K. Epidemiology of severe sepsis occurring in the first 24 hrs in intensive care units in England, Wales, and Northern Ireland. Crit Care Med. 2003;31:2332–2338. doi: 10.1097/01.CCM.0000085141.75513.2B. [DOI] [PubMed] [Google Scholar]
- 33.Brun-Buisson C, Meshaka P, Pinton P, Vallet B EPISEPSIS Study Group. EPISEPSIS: a reappraisal of the epidemiology and outcome of severe sepsis in French intensive care units. Intensive Care Med. 2004;30:580–588. doi: 10.1007/s00134-003-2121-4. [DOI] [PubMed] [Google Scholar]
- 34.Ferrer R, Artigas A, Levy MM, Blanco J, González-Díaz G, et al. Improvement in process of care and outcome after a multicenter severe sepsis educational program in Spain. JAMA. 2008;299:2294–2303. doi: 10.1001/jama.299.19.2294. [DOI] [PubMed] [Google Scholar]
- 35.Blanco J, Muriel-Bombín A, Sagredo V, Taboada F, Gandía F, et al. Incidence, organ dysfunction and mortality in severe sepsis: a Spanish multicentre study. Crit Care. 2008;12:R158. doi: 10.1186/cc7157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fisher CJ, Dhainaut J-F, Opal SM, Pribble JP, Balk RA, et al. Recombinant human interleukin-1 receptor antagonist reduces mortality of patients with sepsis syndrome as a function of severity: a randomized, double-blind, placebo-controlled trial. JAMA. 1994;271:1836–1843. [PubMed] [Google Scholar]
- 37.Martin GS, Eaton S, Mealer M, Moss M. Extravascular lung water in patients with severe sepsis: a prospective cohort study. Crit Care. 2005;9:R74–82. doi: 10.1186/cc3025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cunningham SC, Malone DL, Bochicchio GV, Genuit T, Keledjian K, et al. Serum lipopolysaccharide-binding protein concentrations in trauma victims. Surg Infect. 2006;7:251–261. doi: 10.1089/sur.2006.7.251. [DOI] [PubMed] [Google Scholar]
- 39.Hubacek JA, Stüber F, Fröhlich D, Book M, Wetegrove S, et al. Gene variants of the bacterial/permeability increasing protein and lipopolysaccharide binding protein in sepsis patients: Gender-specific genetic predisposition to sepsis. Crit Care Med. 2001;29:557–561. doi: 10.1097/00003246-200103000-00015. [DOI] [PubMed] [Google Scholar]
- 40.Chien JW, Boeckh MJ, Hansen JA, Clark JG. Lipopolysaccharide binding protein promoter variants influence the risk for Gram-negative bacteremia and mortality after allogeneic hematopoietic cell transplantation. Blood. 2008;111:2462–2469. doi: 10.1182/blood-2007-09-101709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Flores C, Pino-Yanes MM, Villar J. A quality assessment of genetic association studies supporting susceptibility and outcome in acute lung injury. Crit Care. 2008;12:R130. doi: 10.1186/cc7098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Polderman KH, Thijs LG, Girbes AR. Interobserver variability in the use of APACHE II scores. Lancet. 1999;353:380. doi: 10.1016/S0140-6736(05)74953-9. [DOI] [PubMed] [Google Scholar]
- 43.Tunnell RD, Millar BW, Smith GB. The effect of lead time bias on severity of illness scoring, mortality prediction and standardized mortality ratio in intensive care-a pilot study. Anaesthesia. 1998;53:1045–1053. doi: 10.1046/j.1365-2044.1998.00566.x. [DOI] [PubMed] [Google Scholar]
- 44.Suistomaa M, Kari A, Ruokonen E, Takala J. Sampling rate causes bias in APACHE II and SAPS II scores. Intensive Care Med. 2000;26:1727–1729. doi: 10.1007/s001340000677. [DOI] [PubMed] [Google Scholar]
- 45.Herrera MT, Toledo C, Valladares F, Muros M, Díaz-Flores L, et al. Positive end-expiratory pressure modulates local and systemic inflammatory responses in a sepsis-induced lung injury model. Intensive Care Med. 2003;29:1345–1353. doi: 10.1007/s00134-003-1756-5. [DOI] [PubMed] [Google Scholar]
- 46.Brégeon F, Delpierre S, Chetaille B, Kajikawa O, Martin TR, et al. Mechanical ventilation affects lung function and cytokine production in an experimental model of endotoxemia. Anesthesiology. 2005;102:331–339. doi: 10.1097/00000542-200502000-00015. [DOI] [PubMed] [Google Scholar]
- 47.Gharib SA, Liles WC, Matute-Bello G, Glenny RW, Martin TR, et al. Computational identification of key biological modules and transcription factors in acute lung injury. Am J Respir Crit Care Med. 2006;173:653–658. doi: 10.1164/rccm.200509-1473OC. [DOI] [PubMed] [Google Scholar]
- 48.Wurfel MM. Microarray-based analysis of ventilator-induced lung injury. Proc Am Thorac Soc. 2007;4:77–84. doi: 10.1513/pats.200608-149JG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kalil AC, Sun J. Why are clinicians not embracing the results from pivotal clinical trials in severe sepsis? A Bayesian analysis. PLoS ONE. 2008;3:e2291. doi: 10.1371/journal.pone.0002291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Minter RM, Bi X, Ben-Josef G, Wang T, Hu B, et al. LPS-binding protein mediates LPS-induced liver injury and mortality in the setting of biliary obstruction. Am J Physiol Gastrointest Liver Physiol. 2009;296:G45–54. doi: 10.1152/ajpgi.00041.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Comparison of serum levels of IL-6, IL-1-beta, IL-10, and CRP in 107 patients with severe sepsis during the first week in ICU. Data are reported as mean (±SE). IL: interleukin; CRP: C-reactive protein; ICU: intensive care unit. P-value was obtained using GLIM.
(0.49 MB TIF)