Abstract
Information on history of suicidal thoughts and behaviors is critical in risk assessment, and multi-informant assessment has been recommended. Despite this, relatively little is known about parent-adolescent agreement regarding adolescent suicidality. To examine the extent and predictors of such agreement, 448 psychiatrically hospitalized adolescents and their parents were administered structured interviews assessing suicidal thoughts, plans, and attempts and completed measures of youth internalizing and externalizing behaviors, perceived family social support, and parental distress and psychopathology. Adolescents reported significantly more suicidal ideation, plans, and attempts than parents. Parental history of depression and adolescent perceived family support were associated with significantly greater agreement about suicidality. History of multiple suicide attempts was associated with greater disagreement about suicidality.
Rates of suicide increase during adolescence, making it the third leading cause of death in this age group (Hamilton et al., 2007). Primary risk factors for suicide attempts and suicide include a previous suicide attempt, suicidal ideation, affective disorders, alcohol/substance abuse, conduct disordered or aggressive-impulsive behavior, and availability of the means (Gould, Greenberg, Velting, & Shaffer, 2003). Moreover, male gender, older age, and availability of the means have been associated with death by suicide (Gould et al., 2003). Essential components of risk assessment in children and adolescents include assessment of previous suicidal acts and current suicide plans (Pfeffer, 2001). Moreover, practice guidelines recommend gathering and integrating information from multiple informants (American Academy of Child and Adolescent Psychiatry, 2001).
Evidence-based assessment of child psychopathology generally involves collecting information from multiple informants using multiple methods, such as interviews and self-report questionnaires, to appreciate the range and depth of a child's symptoms (Mash & Hunsley, 2005). However, this approach brings in the unique interpretations of informants and variation inherent in different observational settings (Achenbach, McConaughy, & Howell, 1987). When informants report differing information, professionals are faced with the challenge of integrating this information for diagnosis and treatment planning.
INFORMANT AGREEMENT ABOUT CHILD PSYCHOPATHOLOGY
Agreement among informants regarding child and adolescent emotional and behavioral problems has been found to be low to moderate across different population samples and with various assessment strategies (e.g., Achenbach et al., 1987; Herjanic & Reich, 1997). Through an extensive meta-analysis including studies of youth ages 2.5 to 19 years, Achenbach et al. (1987) showed modest parent-child agreement (r = .25). Yeh and Weisz (2001) examined agreement between parents and children ages 7 to 18 years with reference to a presenting problem that brought them to an outpatient clinic. Among 381 pairs of children and their parents, 63% failed to agree on even one presenting problem. In addition to the implications for diagnosis and treatment planning, informant disagreement has been shown to predict future difficulties. For example, in a study in which adolescents ages 15 to 18 years were reassessed at 19 to 22 years, greater discrepancy between parents and adolescents regarding internalizing and externalizing problems predicted adverse outcomes 4 years later. Drug and tobacco use, legal problems, expulsion from school/job, unwanted pregnancy, deliberate self-harm, and referral to mental health services were all associated with informant disagreement 4 years earlier (Ferdinand, van der Ende, & Verhulst, 2004). Given the frequency of disagreement and the poor prognosis associated with such disagreement, it is important to consider the factors that influence agreement.
Factors Influencing Agreement
Investigators have examined various factors that affect agreement between parents and children including (a) type of child or adolescent problem, (b) age and gender, (c) aspects of family life and associated stressors, and (d) parental psychopathology. We use the word child or children to indicate individuals younger than 18 years of age unless referring to a study that exclusively focused on adolescents.
There is greater correspondence between parent and child ratings of externalizing compared to internalizing symptoms (Achenbach et al., 1987; Edelbrock, Costello, Dulcan, Conover, & Kala, 1986; Kolko & Kazdin, 1993). In a sample of children, Herjanic and Reich (1997) showed a low to moderate level of agreement on responses to structured diagnostic interview questions. The highest level of agreement was found for “concrete, observable, severe and unambiguous symptoms,” such as suspension from school and a history of trouble with the police (p. 30). In addition, it has generally been found that children report more symptoms, both internalizing and externalizing, than do parent informants (Sourander, Helstela, & Helenius, 1999; Stanger & Lewis, 1993). With regard to depressive disorders, parents have been found to be less aware of episodic or severe episodes but more aware of chronic, low-level depression in adolescents (Cantwell, Lewinsohn, Rohde, & Seeley, 1997). However, one study found that parents reported more depressive symptoms in inpatient adolescents than did the adolescents themselves (King, Katz, et al., 1997), such that findings vary across samples with different symptom severity levels.
Various studies have analyzed the effect of age and gender on agreement between parents and children, with mixed findings. Results are often difficult to interpret, given the many factors and interactions included in the analyses. Many studies showed greater agreement between parents and preadolescents versus adolescents (Achenbach et al., 1987; Tarullo, Richardson, Radke- Yarrow, & Martinez, 1995), whereas others showed agreement increasing with child age (Edelbrock et al., 1986; Grills & Ollendick, 2003). Conversely, some studies showed no effect based on the child's age (Seiffge-Krenke & Kollmar, 1998; Yeh & Weisz, 2001). Overall, there is no consensus regarding the effect of age on parent-child agreement.
Many researchers have failed to find any effect of child gender on parent-child agreement (e.g., Achenbach et al., 1987; Stanger & Lewis, 1993; Tarullo et al., 1995). Studies that do find gender effects generally find greater discrepancy in parent-adolescent reports for girls than boys; these differences are strongest for internalizing symptoms (Sourander et al., 1999; Verhulst & Van der Ende, 1992). Although the literature does not clearly identify gender effects on parent-child agreement, there are some indications that male children are more likely to agree with their parents.
Family communication, recent stressors, and children's perceptions of family support and warmth have been studied in relation to parent-child agreement about symptoms. Discrepancies in parent-child ratings of symptoms have been related to low parental warmth and acceptance (Kolko & Kazdin, 1993; Treutler & Epkins, 2003). Family conflict and stressors have also been associated with greater discrepancy in parent-child agreement about psychopathology when compared to families with less conflict and stressors (Grills & Ollendick, 2003; Kolko & Kazdin, 1993). Family communication has been found to impact parental identification of adolescent daughters' depression (Logan & King, 2002). Overall, there is converging evidence that family support, warmth, and communication improve parent-child agreement regarding psychopathology.
Findings regarding parental psychopathology and its effect on parent-child agreement are variable (Jensen, Traylor, Xenakis, & Davis, 1988; Kolko & Kazdin, 1993; Treutler & Epkins, 2003). Investigating the “depression bias,” or the effect of maternal dysphoria on report of child behaviors and emotional state, Youngstrom, Izard, and Ackerman (1999) reported evidence that maternal dysphoria corresponded to higher maternal reports of negative behaviors and emotions in 5-year-old children than those of control judges who observed the same children completing tasks. A parental depression bias has also been found to exist with adolescent children (Youngstrom, Loeber, & Stouthamer-Loeber, 2000). Tarullo and colleagues (1995), however, reported that mothers with affective illness did not overreport child and adolescent problems and that mother-child agreement was greater for families in which the mother had affective illness. Taken together, there is mixed evidence on the effect of parental depression in child assessment. Parental depression may bias parents to perceive more negative emotions and behaviors in their child or may make parents more sensitive to noticing their child's emotional distress. In a review of the literature on maternal depression bias, Richters (1992) examined evidence for actual distortion in reports of children's symptoms by mothers with depression. He systematically evaluated studies using predetermined standards for determining distortion (e.g., comparison to reports of independent raters of child behaviors in situations comparable to that in which maternal reports were obtained). Richters reported that none of the studies met the minimum criteria for the presence of distortion.
Overall, children and adolescents tend to report more symptoms of psychopathology than do parents, and agreement is higher for observable behavioral symptoms than for internalizing symptoms. Agreement between parent and child reports appears to be mediated by the nature of the child's psychopathology, psychological symptoms of the parent, and aspects of family functioning. Mental health clinicians must rely heavily on patient and informant reports, and must integrate varying perspectives into their patient assessments for accurate diagnosis and treatment planning.
AGREEMENT ABOUT SUICIDAL IDEATION AND ATTEMPTS
Although there is limited research specifically addressing agreement about child/adolescent suicidality, several studies suggest that informant disagreement is common. Community-based studies suggest that adolescents report significantly more suicidal thoughts and behaviors than are reported by their parents. In large community samples, parents were unaware of 50 to 90% of adolescent reported suicidal ideation (Breton, Tousignant, Bergeron, & Berthiaume, 2002; Kashani, Goddard, & Reid, 1989; Sourander et al., 1999; Velez & Cohen, 1988). Further, studies have found that parents were unaware of 60 to 95% of adolescent-reported suicide attempts (Breton et al., 2002; Sourander et al., 1999; Velez & Cohen, 1988; Walker, Moreau, & Weissman, 1990).
Similar to the level of agreement in community samples, parent-adolescent agreement about suicide attempt history is low to moderate in clinical samples of adolescent suicide attempters. Zimmerman and Asnis (1991) reported on a sample of 50 adolescent suicide attempters in which 60% of parents were unaware of adolescents' reported suicide attempts. The authors found that the majority of adolescents had not told anybody they were going to make an attempt, suggesting that some of this lack of awareness is related to limited adolescent disclosure.
Less information is available regarding factors that may be associated with parent-child agreement about suicide attempts. In a preliminary report of 13 suicide attempters from a community sample of youth and young adults, ages 6 to 23 years, Walker et al. (1990) found differences between families in which children reported suicide attempts that were not identified by their mothers and those families in which attempts were identified by parents. Families in which parents did not identify child suicide attempts were characterized by more attempts by the child, more serious suicidal intent, parental separation or divorce, and a higher rate of maternal substance abuse. Parents with depression have also been found to identify fewer cases of adolescent- reported suicidality than parents without psychopathology (Klimes-Dougan, 1998).
THIS STUDY
Parental awareness of suicidality is necessary to obtain appropriate treatment for the adolescent, monitor for safety, and restrict access to means for self-harm. Although previous research suggests that adolescents report significantly more suicidal ideation and attempts than their parents, relatively little is known about parent, child, and family factors that affect agreement. Although research suggests that adolescents generally report more suicidal behavior than their parents, disagreement can also occur when parents report suicidality that was not reported by the adolescent. These different types of disagreement may be influenced by different factors and may predict different outcomes (Ferdinand et al., 2004). This study's goal is to investigate parent-child agreement regarding suicidal thoughts and behaviors to inform evidence-based risk assessment and treatment planning for suicidal youth.
This study examined the extent of parent-adolescent agreement about current and past suicidal thoughts and behaviors in a sample of suicidal, psychiatrically hospitalized adolescents. We hypothesized that there would be low to moderate agreement between parents and adolescents about suicidal thoughts and behaviors. Agreement was hypothesized to be higher for (a) past month rather than past year suicidality, and (b) suicidal behavior in comparison to ideation, as parent-adolescent agreement has been shown to be higher for behaviors than internal experiences. This study also examined parent, child, and family characteristics that might differentiate (a) parent-only reported suicidality versus parent-adolescent agreement about suicidality and (b) adolescent-only reported suicidality versus parent- adolescent agreement. Based on previous studies, we hypothesized that greater agreement would be associated with male gender, presence of externalizing or observable symptoms, and perceived family support. Exploratory analyses investigated the potential associations of child age, history of multiple attempts, parental psychopathology, and family structure with parent- adolescent agreement. The influence of attempt method on parent-adolescent agreement has not been investigated in previous studies and was also considered in exploratory analyses.
METHOD
Participants
The data for this study are part of a larger study inves- tigating the efficacy of the Youth-Nominated Support Team-II intervention with suicidal adolescents (King, Merchant, Ewell-Foster, Kerr, & Hanna, 2007). A total of 448 adolescents, ages 13 to 17 years, were recruited from two psychiatric hospitals. For inclusion in the study, a parent and/or child report of serious suicidal ideation or recent suicide attempt on the Diagnostic Interview Schedule for Children (DISC-IV; Shaffer, Fisher, Lucas, & NIMH DISC Editorial Board, 1998) was required. Forty-three percent of study-eligible adolescents agreed to participate. There were no significant differences by consent status in age, gender, or race, the only variables for which information was available about nonparticipants. Additional details regarding participant recruitment and sample characteristics are reported in King et al. (2007). The data presented are from the baseline assessments completed during the adolescents' hospitalizations.
Measures
DISC-IV
The DISC-IV is a structured diagnostic interview administered to parents and adolescents (Shaffer et al., 1998). It is a widely used interview with demonstrated test-retest reliability and criterion validity with clinician ratings (Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000). Only the DISC-IV suicidal ideation questions were used, which assessed past-month and past-year serious thoughts of suicide, presence of suicide plan, and suicide attempt (yes, no, don't know). These specific items have demonstrated good test-retest reliability (κ = .72-.88). Additional questions assessed method of attempts. Parent and adolescent reported suicide attempt methods were grouped into the following three broad categories for analyses: ingestion of prescription or nonprescription medications, cutting, and other highly lethal means (shooting, hanging, drowning, etc.).
Schedule for Affective Disorders and Schizophrenia for School-Age Children: Present and Lifetime Version (K-SADS-PL)
The K-SADS-PL is a semistructured interview for children ages 6 to 18 which provides Diagnostic and Statistical Manual of Mental Disorders (4th ed.) diagnostic data (Kaufman et al., 1997). The full K-SADS was administered to adolescents and selected sections were also administered to parents (i.e., affective disorders, psychosis, substance use, oppositional defiant disorder, and conduct disorder). The K-SADS was used to assess baseline diagnoses in this study. It has demonstrated strong test-retest reliability, concurrent validity, and interrater reliability (Kaufman et al., 1997). Interviewers were trained mental health professionals who completed 20 hours of K-SADS-PL training and established interrater reliability with a senior diagnostician on four consecutive interviews prior to study onset. The mean agreement on presence/absence of mood, anxiety, or behavior disorder diagnoses was 82%. Mean agreement on specific type of mood disorder was 100% with 98% agreement regarding age of onset of depressive disorders.
Suicidal Ideation Questionnaire-junior (SIQ- JR)
The SIQ-JR was used to assess the frequency of adolescents' suicidal thoughts. It is a 15-item self-report questionnaire with excellent, well-documented psychometric properties (Reynolds, 1988, 1992). SIQ-JR total scores of psychiatrically hospitalized adolescents have been found to be significant predictors of suicidal thoughts and attempts 6-months posthospitalization (King, Hovey, Brand, & Ghaziuddin, 1997). The SIQ- JR had excellent internal consistency in this sample (α= .92).
Youth Self-Report (YSR)
The YSR is an adolescent completed 119-item questionnaire assessing a variety of emotional and behavioral problems in youth (Achenbach, 1991). The broadband internalizing and externalizing scales are used in this study and have strong psychometric properties, including internal consistency, test-retest reliability, and criterion validity (Achenbach, 1991). Internal consistency in this sample was .89 for internalizing and .86 for externalizing symptoms.
Brief Symptom Inventory (BSI)
The BSI is a 53- item self-report questionnaire completed by parents to measure current levels of their own emotional distress (Derogatis & Melisaratos, 1983). Items are rated on a 0(not bothered by symptom) to 4 (extremely bothered by symptom) scale for the past week. There is evidence for the scale's convergent, discriminant, and predictive validity (Derogatis & Melisaratos, 1983). Subscales were strongly intercorrelated in this sample and factor analysis suggested that a single summary score, the Global Severity Index, best represented these items. Possible scores range from 0 to 4. Internal consistency was .71 in this sample.
Perceived Social Support from Family (PSS-Fa)
The PSS-Fa is a 20-item self-report questionnaire assessing adolescents' perceptions of social support received from family members (Procidano & Heller, 1983). The PSS-Fa has demonstrated concurrent validity with other measures of perceived family support (Cumsille & Epstein, 1994). Internal consistency was .72 in this sample.
Family History Screen (FHS)
The FHS is a brief screening measure of 15 psychiatric disorders in biological parents (Weissman et al., 2000). For this study, the items identifying maternal or paternal history of depression were used. A summary variable was calculated to indicate the presence or absence of depression in either parent. The validity of the FHS has been demonstrated in comparison to interview-based diagnoses and the greatest sensitivity was found for the depression items (Weissman et al., 2000).
Procedures
Institutional Review Board approval was obtained for all procedures used in this study. Parents or guardians of eligible adolescents were approached and provided with information about this study during the adolescent's hospitalization, and a member of the research team was available to answer questions. Parents or guardians provided informed consent and assent was obtained from adolescents.
Data Analytic Plan
The extent of agreement between parents and adolescents about suicidal thoughts and behaviors was assessed for the past month and past year. Cohen's kappa values were calculated to show the magnitude of chance-corrected agreement. Positive kappa values signify agreement greater than would be expected by chance, with 1.0 reflecting perfect agreement. McNemar tests were calculated to evaluate differences in response rates. Significant McNemar tests suggest that one informant is significantly more likely to give a particular response.
For past-month suicidal thoughts, plans, and attempts, parent-adolescent dyads who agreed were compared using logistic regression analyses to (a) dyads in which only the adolescent reported suicidality and (b) dyads in which only the parent reported suicidality. Variables that did not differentiate groups in univariate analyses (e.g., race, mother vs. father informant, family structure, family income, and severity of substance use) were not included in the regression analyses. Sex, age, perceived family support, youth reports of multiple past suicide attempts, parent BSI scores, parental history of depression, and both internalizing and externalizing YSR variables were included in logistic regression analyses. Assumptions for the use of logistic regression were considered. The dyads in this sample were independent and the dependent variable was binary. Whereas the dependent variable was not evenly distributed between agreement and disagreement in several analyses, this was consistent with what would be expected, with no reason to believe that it reflected sampling bias. Therefore, weighting of the dependent variable was not used. Chi-square analyses then examined differences in level of agreement about suicide attempts by attempt method.
RESULTS
Baseline demographic and clinical characteristics of the sample are shown in Table 1. The adolescents' mean age was 15.6 (SD = 1.3). These adolescents were experiencing significant suicidal ideation, as evidenced by a mean percentile score on the SIQ-JR of 90 (SD = 11.8). The descriptive statistics for primary study variables are presented in Table 2.
TABLE 1.
Sample Characteristics
| n | % | |
|---|---|---|
| Gender | ||
| Female | 319 | 71 |
| Male | 129 | 29 |
| Race | ||
| White | 375 | 84 |
| African American | 29 | 7 |
| Hispanic | 8 | 2 |
| Other | 24 | 5 |
| Youth-Reported No. Lifetime | ||
| Suicide Attempts | ||
| None | 114 | 25 |
| One | 147 | 33 |
| Multiple | 171 | 38 |
| Parent Informant | ||
| Mother | 373 | 83 |
| Father | 45 | 10 |
| Grandmother | 12 | 3 |
| Other Family Member/Guardian | 10 | 3 |
| Diagnoses | ||
| Major Depressive Disorder | 387 | 86 |
| Attention Deficit Hyperactivity | 76 | 17 |
| Disorder | ||
| Conduct Disorder | 64 | 14 |
| Oppositional Defiant Disorder | 88 | 20 |
| Anxiety Disorder | 161 | 36 |
| Alcohol/Substance Abuse | 84 | 19 |
Note. Diagnoses do not total 100% because of comorbidity.
TABLE 2.
Descriptive Statistics for Predictor Variables
| Measure | Minimum | Maximum | M | SD |
|---|---|---|---|---|
| Perceived Family Support | 0 | 20.00 | 8.80 | 5.60 |
| Brief Symptom Inventory Global Severity Index | 0 | 3.38 | 0.64 | 0.59 |
| Youth Self Report-Internalizing | 4 | 58.00 | 28.40 | 10.80 |
| Youth Self Report-Externalizing | 0 | 54.00 | 21.50 | 9.50 |
Extent of Agreement
The extent of agreement between parents and adolescents about suicidal thoughts and behaviors is shown in Table 3 for the past year and Table 4 for the past month. In this sample of psychiatrically hospitalized, suicidal adolescents, agreement between parents and adolescents about adolescents' history of serious thoughts of suicide was no greater than chance. Agreement about the adolescent's history of creating a serious plan for suicide was greater than chance, but the magnitude of this agreement was low (past-year κ = .162, past-month κ = .150). There was greater informant agreement about adolescents' history of suicide attempts, with agreement being higher for more recent attempts (past-month κ = .735, 95% confidence interval = .669-.801; past-year κ = .560, 95% confidence interval = .478-.642). Results show that, overall, adolescents are significantly more likely than parents to report their own suicidal thoughts, plans, and attempts.
TABLE 3.
Parent-Adolescent Agreement Regarding Suicidal Thoughts and Behaviors in Past Year
| A-Yes | A-No/DK | κ | McNemar χ2 | ||
|---|---|---|---|---|---|
| P-Yes | 317 | 11 | |||
| Thoughts | -.022 | 81.301** | |||
| P-No/DK | 112 | 2 | |||
| P-Yes | 113 | 24 | |||
| Plan | .162** | 118.712** | |||
| P-No/DK | 181 | 114 | |||
| P-Yes | 202 | 13 | |||
| Attempt | .560** | 36.890** | |||
| P-No/DK | 69 | 105 |
Note. A = adolescent; P = parent; DK = do not know.
p≤.01.
TABLE 4.
Parent-adolescent Agreement Regarding Suicidal Thoughts and Behaviors in past Month
| A-Yes | A-No/DK | κ | McNemar χ2 | ||
|---|---|---|---|---|---|
| P-Yes | 248 | 23 | |||
| Thoughts | .009 | 88.994** | |||
| P-No/DK | 147 | 15 | |||
| P-Yes | 101 | 44 | |||
| Plan | .150** | 51.358** | |||
| P-No/DK | 143 | 131 | |||
| P-Yes | 188 | 17 | |||
| Attempt | .735** | 6.685** | |||
| P-No/DK | 37 | 166 |
Note. A = adolescent; P = parent; DK = do not know.
p≤.01.
Factors Influencing Agreement
Parent-reported suicidality not identified by adolescent
Table 5 presents logistic regression analyses identifying predictors of parent-only reported suicidal thoughts, plans, and attempts compared to parent- adolescent agreement. Parent-adolescent agreement about suicidal thoughts (n = 263) was compared to parent-only reported thoughts (n = 23), agreement about suicide plans (n = 232) was compared to parent-only reported plans (n = 44), and agreement about attempts (n = 354) was compared to parent-only reported attempts (n = 17). Adolescents who reported higher levels of externalizing symptoms were less likely to be in the parent-only reported suicidal ideation group. For each 1-point increase in externalizing symptoms (range = 0-54), adolescents were 7.5% less likely to be in this group (p<.05).
TABLE 5.
Logistic Regression for Agreement Versus Parent-Only Reported Suicidal Thoughts and Behavior
| β | SE of β | Wald Stat. | Odds Ratio | |
|---|---|---|---|---|
| Thoughts | ||||
| Sex | .578 | .641 | .811 | 1.782 |
| Age | -.164 | .236 | .473 | .849 |
| Perceived Family | -.062 | .059 | 1117 | .940 |
| Support | ||||
| BSI Total | .568 | .421 | 1.824 | 1.765 |
| Parental History of Depression | .361 | .624 | .334 | 1.435 |
| YSR-Internalizing | -.051 | .030 | 2.862 | .950 |
| YSR-Externalizing | -.078 | .039 | 4.008* | .925 |
| Multiple Attempt History | -.439 | .641 | .469 | .645 |
| Plan | ||||
| Sex | .096 | .450 | .045 | 1.100 |
| Age | -.023 | .148 | .023 | .978 |
| Perceived Family Support | -.001 | .034 | .001 | .999 |
| BSI Total | .073 | .297 | .061 | 1.076 |
| Parental History of Depression | .495 | .408 | 1.472 | 1.641 |
| YSR-Internalizing | .008 | .020 | .170 | 1.008 |
| YSR-Externalizing | -.016 | .022 | .483 | .985 |
| Multiple Attempt History | .526 | .386 | 1.856 | 1.691 |
| Attempts | ||||
| Sex | -1.095 | .810 | 1.828 | .335 |
| Age | .150 | .236 | .406 | 1.162 |
| Perceived Family Support | -.006 | .053 | .012 | .994 |
| BSI Total | -.150 | .550 | .074 | .861 |
| Parental History of Depression | .050 | .608 | .007 | 1.052 |
| YSR-Internalizing | -.016 | .030 | .286 | .984 |
| YSR-Externalizing | .045 | .034 | 1.740 | 1.046 |
| Multiple Attempt History | -.637 | .647 | .968 | .529 |
Note. The total sample size for each regression varied: thoughts n = 254; plan n = 244; attempt n = 344. Higher levels of YSR externalizing symptoms were associated with less disagreement about suicidal thoughts. BSI = Brief Symptom Inventory; YSR = Youth Self Report.
p ≤ .05.
The parent-reported attempt method was compared for adolescents who agreed with their parent regarding the presence of an attempt (n=188) and those adolescents who denied an attempt reported by parents (n=17) during the past month. The proportions of each attempt method for both groups are depicted in Figure 1. In parent-adolescent dyads who disagreed, parents reported a greater proportion of cutting than ingestion as the attempt method (χ2=8.569, p<.01). There was no significant difference in the proportion of other highly lethal means in comparison to ingestion or cutting. The small sample size in the disagreement group did not permit analyses of predictors of disagreement separately by attempt method.
FIGURE 1.
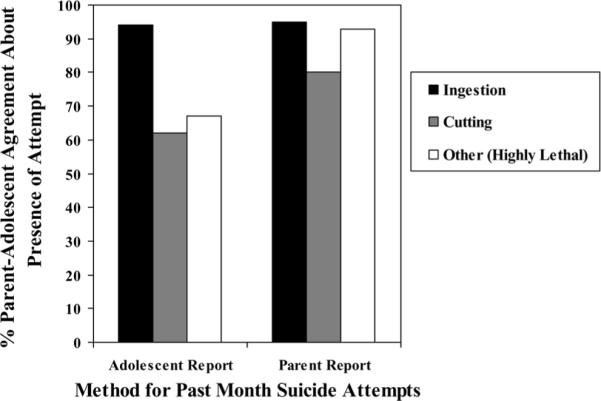
Percentage of agreement by attempt method. Note: adolescent-reported attempts, n = 225 (agree n = 188, adolescent-only report n = 37). Parent-reported attempts, n = 205 (agree n = 188, parent-only report n = 17).
Adolescent-reported suicidality not identified by parent
Table 6 presents logistic regression analyses identifying predictors of adolescent-only reported suicidal thoughts, plans, and attempts compared to parent-adolescent agreement. Parent-adolescent agreement about suicidal thoughts (n=263) was compared to adolescent-only reported thoughts (n=147), agreement about suicide plans (n=232) was compared to adolescent-only reported plans (n=143), and agreement about attempts (n=354) was compared to adolescent-only reported attempts (n=37). Adolescents who reported higher levels of internalizing symptoms and had parents with a history of mental illness were less likely to be in the adolescent-only reported suicidal ideation group. For each 1-point increase in youth reported internalizing symptoms (range=4-58), adolescents were 3.3% less likely to be in this group (p<.05). A history of depression in either parent decreased the likelihood of being in the adolescent-only reported suicidal ideation group by 50.5% (p<.05).
TABLE 6.
Logistic Regression for Agreement Versus Adolescent-Only Reported Suicidal Thoughts and Behavior
| β | SE of β | Wald Stat. | Odds Ratio | |
|---|---|---|---|---|
| Thoughts | ||||
| Sex | .270 | .261 | 1.071 | 1.310 |
| Age | .106 | .093 | 1.313 | 1.112 |
| Perceived Family Support | -.028 | .022 | 1.508 | .973 |
| BSI Total | -.120 | .218 | .306 | .887 |
| Parental History of | -.703 | .244 | 8.312** | .495 |
| Depression | ||||
| YSR-Internalizing | -.034 | .013 | 7.060** | .967 |
| YSR-Externalizing | .018 | .014 | 1.566 | 1.018 |
| Multiple Attempt History | -.053 | .244 | .048 | .948 |
| Plan | ||||
| Sex | .466 | .273 | 2.914 | 1.593 |
| Age | .025 | .095 | .067 | 1.025 |
| Perceived Family Support | -.055 | .023 | 5.697* | .946 |
| BSI Total | -.369 | .231 | 2.537 | .692 |
| Parental History of Depression | -.227 | .253 | .804 | .797 |
| YSR-Iinternalizing | .020 | .013 | 2.449 | 1.020 |
| YSR-Externalizing | -.007 | .014 | .280 | .993 |
| Multiple Attempt History | .530 | .249 | 4.521* | 1.699 |
| Attempts | ||||
| Sex | -.147 | .439 | .112 | .864 |
| Age | -.356 | .154 | 5.369* | .700 |
| Perceived Family Support | -.080 | .040 | 4.086* | .923 |
| BSI Total | .497 | .304 | 2.671 | 1.644 |
| Parental History of Depression | -.322 | .402 | .640 | .725 |
| YSR-Internalizing | -.011 | .020 | .330 | .989 |
| YSR-Externalizing | -.002 | .022 | .006 | .998 |
| Multiple Attempt History | .916 | .394 | 5.414* | 2.500 |
Note. The total sample size for each regression varied: thoughts n = 370; plan n = 336; attempt n = 354. Higher levels of YSR internalizing symptoms and parental history of depression were associated with less disagreement about suicidal thoughts. Higher levels of family support were associated with less disagreement about suicide plans. A history of multiple suicide attempts was associated with greater disagreement about suicide plans. Older age and higher levels of family support were associated with less disagreement about suicide attempts. Multiple attempt history was associated with greater disagreement about past month suicide attempt. BSI = Brief Symptom Inventory; YSR = Youth Self Report.
p≤.05.
p≤.01.
Adolescents who perceived less family support were more likely to report a serious suicide plan that was not identified by their parents. For each 1-point increase in perceived family social support (range=0-20), adolescents were 5.4% less likely to be in the adolescent-only reported suicide plan group (p<.05). Furthermore, adolescents who reported a history of multiple suicide attempts were 69.9% more likely to report a suicide plan not identified by parents (p<.05).
Younger adolescents, those who perceived less family support, and those with a history of multiple suicide attempts were more likely to report a suicide attempt that was not identified by parents. For each 1-point increase in perceived family support scores, adolescents were 7.7% less likely to be in the adolescent-only reported suicide attempt group (p<.05). Older adolescents showed greater agreement with parents about suicide attempts, such that for each one year increase in age, adolescents were 30% less likely to report an attempt not identified by parents (p<.05). Finally, a history of multiple suicide attempts was associated with a 250% increase in likelihood of being in the adolescent-only reported suicide attempt group (p<.05).
For adolescents who reported a suicide attempt in the past month, the adolescent-reported attempt method was compared for parent-adolescent dyads who agreed regarding the presence of an attempt (n=188) and those dyads who did not agree (n=37). The proportions of each attempt method reported for both groups are shown in Figure 1. Adolescents whose parents did not also identify a suicide attempt reported a greater proportion of cutting than ingestion (χ2=30.113, p<.01) and a greater proportion of other highly lethal attempt methods than ingestion compared to parent-adolescent dyads in agreement (χ2=18.086, p<.01). There was no significant difference in the proportion of other highly lethal means in comparison to cutting. There was a large enough sample size with adolescent-only reported attempts to explore predictors of agreement by type of attempt. Girls (odds ratio=1.5, p<.05) and those with higher levels of parental distress on the BSI (odds ratio=12.738, p<.01) were more likely to report an attempt by cutting that was not identified by parents. That is, gender (female) and parental distress predicted parent-adolescent disagreement in the subgroup of adolescents who reported the suicide attempt method of cutting. No significant predictors were found for other attempt methods.
DISCUSSION
In this large-scale study of suicidal adolescents, parent-adolescent agreement about suicidal ideation (serious thoughts and plans) was low. Despite the fact that these adolescents were hospitalized, 37% of parents were unaware of adolescent-reported suicidal thoughts and 59% were unaware of adolescent-reported suicide plans. These levels of disagreement are on the low end of the ranges found in community samples, where 50 to 90% of parents have been found to be unaware of suicidal ideation (Breton et al., 2002; Kashani et al., 1989; Sourander et al., 1999; Velez & Cohen, 1988). As hypothesized, agreement was highest concerning recent suicide attempts among these psychiatrically hospitalized adolescents and was higher for behaviors (attempts) than for ideation. As in community studies, adolescents reported significantly higher levels of suicidal thoughts, plans, and behaviors than their parents, indicating that adolescent involvement in the assessment of suicidality is absolutely critical. Possible explanations for the apparent underreporting by parents are lack of awareness, parental denial, or differing interpretation of events (Zimmerman & Asnis, 1991).
Predictors of Disagreement
Perceived family support was found to play an important role in parental awareness of adolescent-reported suicide plans and attempts. This finding is consistent with studies of other forms of psychopathology showing greater discrepancies in parent and child reports of symptoms in the context of low parental warmth and acceptance (Kolko & Kazdin, 1993; Treutler & Epkins, 2003). Low levels of family support have also been associated with higher rates of suicidal behavior in adolescents (King, Segal, Naylor, & Evans, 1993; Perkins & Hartless, 2002). The combination of low family support and decreased parental awareness about suicidal behavior is particularly concerning and may place the adolescent at even higher risk for future suicidality. Family-based intervention strategies aimed at improving family support and communication may be particularly important for families with discrepant reports about suicidality and low perceived family support.
Adolescents with a self-reported history of multiple suicide attempts were more likely than those with one or no attempts to report suicidal plans and attempts that were not identified by parents. A history of attempts increases the adolescent's risk for future death by suicide (Brent, Baugher, Bridge, Chen, & Chiappetta, 1999), and it is very concerning when parents are not aware of serious suicidality in this context. Family-based interventions designed to improve communication and support may also be particularly important for the families of multiple attempters.
Parents were more likely to be aware of adolescent-reported suicidal ideation if either parent had a history of depression. This finding is consistent with the Tarullo et al. (1995) study suggesting that parental experience of mental illness makes them more sensitive to and aware of their child's experience of distress but inconsistent with studies suggesting that parental depression has a distorting role in their perceptions of the adolescent's experience (e.g., Youngstrom et al., 1999; Youngstrom et al., 2000). Notably, a critical review by Richters (1992) failed to find support for the presence of a maternal depression bias. Several studies finding greater disagreement in the context of parental psychopathology have been conducted with community samples (Jensen et al., 1988; Youngstrom et al., 2000). In a severely impaired sample that is psychiatrically hospitalized, such as in this study, parental experience with depression may be associated with greater sensitivity to and awareness of the adolescent's thoughts and behavior.
In comparing attempt method for parents and adolescents who agreed and disagreed, we found that cutting was the attempt method most likely to be reported by only parents or only adolescents. The classification of cutting behavior in adolescents appears to be more ambiguous than other attempt methods. Nonsuicidal self-injury is relatively common among adolescents (Lloyd-Richardson, Perrine, Dierker, & Kelley, 2007) and may be confused with behavior involving suicidal intent by both parents and adolescents. Moreover, suicidal intent is difficult to ascertain in adolescents and stated intent may vary with the adolescent's emotional state and with when the adolescent is queried (King, 1997). It is also possible that parents are more likely to be unaware of low-lethality attempts by cutting, which may occur frequently and be hidden by clothing, compared to other methods, such as ingestion, which may require emergency treatment. Preliminary analyses suggest that adolescent girls and those with parents who were experiencing greater emotional distress were more likely to disagree about suicide attempts by cutting.
The study hypothesis that intact family structure would be associated with greater agreement was not supported. In this sample the family structure (i.e., intact biological family, single parent, or stepfamily) did not significantly impact the extent of agreement between parents and adolescents about suicidality.
Study Limitations
The large sample of psychiatrically hospitalized adolescents in this study provides valuable information about parent-adolescent agreement in acutely suicidal populations; however, the findings may not generalize to outpatient or community populations. This sample was also predominately Caucasian, which limits its generalizability to other ethnic groups. Additional research with ethnic minorities and outpatient or community samples is recommended. The majority of parent informants in the study were mothers, and these findings may not generalize to fathers or other caretakers. As this study was a preliminary investigation of predictors of parent-adolescent agreement about suicidality and made use of secondary analyses, some predictor measures were brief and completed by only one informant. In future studies, it will be important to include more detailed and multi-informant measures of family functioning and family mental health history. Finally, despite a large sample size, the total sample size for certain comparisons (e.g., parent-only reported suicidal thoughts and attempts) was relatively small.
Implications for Research, Policy, and Practice
Within the context of these limitations, our findings have implications for the clinical assessment of suicide risk and the treatment of adolescents at high risk, rein-forcing the well-known guideline that adolescent involvement in the assessment of suicidality is essential. In families where the adolescent perceives low family support, has a history of multiple suicide attempts, and parents have less direct experience with psychopathology, parents may be unaware of the nature and extent of their child's suicidality. In these cases, it is especially important to involve parents in the adolescent's short- and long-term safety planning and treatment to increase parental awareness and help them provide a safe home environment for the adolescent. It may also be useful to educate all parents in clinical settings about the significant levels of disagreement between parents and adoles- cents about these life-threatening thoughts and behaviors. These data suggest that clinicians should not dismiss parental depression as distorting perceptions of their adolescent's suicidality, as such a history of depression may enhance parental awareness of the adolescent's suicidal thoughts and plans. Given the high levels of disagreement between parents and adolescents, a conservative approach would take seriously and address either parent or child report of suicidality. In this manner, these findings inform clinical practice.
When cutting is reported by either parent or adolescent, it is especially important to understand each informant's interpretation of the intent of the behavior. One treatment goal may be to increase parental awareness of suicidal thoughts and behaviors so that they may better monitor their adolescents. Improved family support and communication may help foster such awareness of suicidality and help families to better support adolescents in the treatment and recovery process.
These findings also have implications for research on the assessment, treatment, and case management of adolescent suicidality. For example, the effect of parent-adolescent disagreement about suicidality on treatment adherence and outcomes remains to be investigated. Future studies combining qualitative and quantitative strategies may also be useful in improving our understanding of why this disagreement exists, what would encourage adolescents to share this important information with parents, and how to make parents more aware of the experience of suicidality in their adolescents. Further investigation into the assessment and treatment of suicide attempts by cutting is also important.
Acknowledgments
We also thank the study independent evaluators, especially Cheryl McManus, Tracy Laichalk, Kristin Chadha, Elisa Berger, and Jeff Ammons; the research managers, Barbara Hanna, Alissa Huth-Bocks, and Louis Weisse; and the statistical consultant, Joe Kazemi.
REFERENCES
- Achenbach TM. Manual for the Youth Self-Report and 1991 Profile. Department of Psychiatry, University of Vermont; Burlington: 1991. [Google Scholar]
- Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychological Bulletin. 1987;101:213–232. [PubMed] [Google Scholar]
- American Academy of Child and Adolescent Psychiatry Practice parameter for the assessment and treatment of children and adolescents with suicidal behavior. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:24S–51S. doi: 10.1097/00004583-200107001-00003. [DOI] [PubMed] [Google Scholar]
- Brent DA, Baugher M, Bridge J, Chen T, Chiappetta L. Age- and sex-related risk factors for adolescent suicide. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:1497–1505. doi: 10.1097/00004583-199912000-00010. [DOI] [PubMed] [Google Scholar]
- Breton J, Tousignant M, Bergeron L, Berthiaume C. Informant-specific correlates of suicidal behavior in a community survey of 12- to 14-year-olds. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:723–730. doi: 10.1097/00004583-200206000-00012. [DOI] [PubMed] [Google Scholar]
- Cantwell DP, Lewinsohn PM, Rohde P, Seeley JR. Correspondence between adolescent report and parent report of psychiatric diagnostic data. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:610–619. doi: 10.1097/00004583-199705000-00011. [DOI] [PubMed] [Google Scholar]
- Cumsille PE, Epstein N. Family cohesion, family adaptability, social support, and adolescent depressive symptoms in out-patient clinic families. Journal of Family Psychology. 1994;8:202–214. [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: An introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- Edelbrock CS, Costello AJ, Dulcan MK, Conover NC, Kala R. Parent-child agreement on child psychiatric symptoms assessed via structured interview. Journal of Child Psychology and Psychiatry. 1986;27:181–190. [PubMed] [Google Scholar]
- Ferdinand RF, van der Ende J, Verhulst FC. Parent-adolescent disagreement regarding psychopathology in adolescents from the general population as a risk factor for adverse outcome. Journal of Abnormal Psychology. 2004;113:198–206. doi: 10.1037/0021-843X.113.2.198. [DOI] [PubMed] [Google Scholar]
- Gould MS, Greenberg T, Velting DM, Shaffer D. Youth suicide risk and preventive interventions: A review of the past 10 years. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42:386–405. doi: 10.1097/01.CHI.0000046821.95464.CF. [DOI] [PubMed] [Google Scholar]
- Grills AE, Ollendick TH. Multiple informant agreement and the Anxiety Disorders Interview Schedule for Parents and Children. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42:30–40. doi: 10.1097/00004583-200301000-00008. [DOI] [PubMed] [Google Scholar]
- Hamilton BE, Minino AM, Martin JA, Kochanek KD, Strobino DM, Guyer B. Annual summary of vital statistics: 2005. Pediatrics. 2007;119:345–360. doi: 10.1542/peds.2006-3226. [DOI] [PubMed] [Google Scholar]
- Herjanic B, Reich W. Development of a structured psychiatric interview for children: Agreement between child and parent on individual symptoms. Journal of Abnormal Child Psychology. 1997;25:21–31. doi: 10.1023/a:1025703323438. [DOI] [PubMed] [Google Scholar]
- Jensen PS, Traylor J, Xenakis SN, Davis H. Child psychopathology rating scales and interrater agreement: I. Parents' gender and psychiatric symptoms. Journal of the American Academy of Child & Adolescent Psychiatry. 1988;27:442–450. doi: 10.1097/00004583-198807000-00012. [DOI] [PubMed] [Google Scholar]
- Kashani JH, Goddard P, Reid JC. Correlates of suicidal ideation in a community sample of children and adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1989;28:912–917. doi: 10.1097/00004583-198911000-00016. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- King CA. Suicidal behavior in adolescence. In: Maris R, Silverman M, Canetto S, editors. Review of suicidology, 1997. Guilford; New York: 1997. pp. 61–95. [Google Scholar]
- King CA, Hovey JD, Brand E, Ghaziuddin N. Prediction of positive outcomes for adolescent psychiatric inpatients. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:1434–1442. doi: 10.1097/00004583-199710000-00026. [DOI] [PubMed] [Google Scholar]
- King CA, Katz SH, Ghaziuddin N, Brand E, Hill EM, McGovern L. Diagnosis and assessment of depression and suicidality using the NIMH Diagnostic Interview Schedule for Children (DISC-2.3) Journal of Abnormal Child Psychology. 1997;25:173–181. doi: 10.1023/a:1025739730823. [DOI] [PubMed] [Google Scholar]
- King CA, Merchant C, Ewell-Foster C, Kerr DCR, Hanna B. Acutely suicidal adolescents with histories of multiple attempts: A highly impaired subgroup of males and females. 2007. Manuscript submitted for publication. [Google Scholar]
- King C, Segal H, Naylor M, Evans T. Family functioning and suicidal behavior in adolescent inpatients with mood disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32:1198–1206. doi: 10.1097/00004583-199311000-00013. [DOI] [PubMed] [Google Scholar]
- Klimes-Dougan B. Screening for suicidal ideation in children and adolescents: Methodological considerations. Journal of Adolescence. 1998;21:435–444. doi: 10.1006/jado.1998.0166. [DOI] [PubMed] [Google Scholar]
- Kolko DJ, Kazdin AE. Emotional/behavioral problems in clinic and nonclinic children: Correspondence among child, parent and teacher reports. Journal of Child Psychology and Psychiatry. 1993;34:991–1006. doi: 10.1111/j.1469-7610.1993.tb01103.x. [DOI] [PubMed] [Google Scholar]
- Lloyd-Richardson EE, Perrine N, Dierker L, Kelley ML. Characteristic and functions on non-suicidal self-injury in a community sample of adolescents. Psychological Medicine. 2007;37:1183–1192. doi: 10.1017/S003329170700027X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan DE, King CA. Parental identification of depression and mental health service use among depressed adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:296–304. doi: 10.1097/00004583-200203000-00009. [DOI] [PubMed] [Google Scholar]
- Mash EJ, Hunsley J. Evidence-based assessment of child and adolescent disorders: Issues and challenges. Journal of Clinical Child and Adolescent Psychology. 2005;34:362–379. doi: 10.1207/s15374424jccp3403_1. [DOI] [PubMed] [Google Scholar]
- Perkins DF, Hartless G. An ecological risk-factor examination of suicide ideation and behavior of adolescents. Journal of Adolescent Research. 2002;17:3–26. [Google Scholar]
- Pfeffer CR. Diagnosis of childhood and adolescent suicidal behavior: Unmet needs for suicide prevention. Biological Psychiatry. 2001;49:1055–1061. doi: 10.1016/s0006-3223(01)01141-6. [DOI] [PubMed] [Google Scholar]
- Procidano ME, Heller K. Measures of perceived social support from friends and from family: Three validation studies. American Journal of Community Psychology. 1983;11:1–24. doi: 10.1007/BF00898416. [DOI] [PubMed] [Google Scholar]
- Reynolds WM. Suicidal Ideation Questionnaire: Professional manual. Psychological Assessment Resources; Odessa, FL: 1988. [Google Scholar]
- Reynolds WM. Measurement of suicidal ideation in adolescents. Paper presented at the annual meeting of the American Association of Suicidology; Chicago. Apr, 1992. [Google Scholar]
- Richters JE. Depressed mothers as informants about their children: A critical review of the evidence for distortion. Psychological Bulletin. 1992;112:485–499. doi: 10.1037/0033-2909.112.3.485. [DOI] [PubMed] [Google Scholar]
- Seiffge-Krenke I, Kollmar F. Discrepancies between mothers' and fathers' perceptions of sons' and daughters' problem behaviour: A longitudinal analysis of parent-adolescent agreement on internalising and externalising problem behaviour. Journal of Child Psychology and Psychiatry. 1998;39:687–697. [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas C, NIMH DISC Editorial Board, editors. DISC-IV. Diagnostic Interview Schedule for Children (Youth informant and parent informant interviews): Epidemiologic version. Joy and William Ruane Center to Identify and Treat Mood Disorders, Division of Child Psychiatry, Columbia University; New York: 1998. [Google Scholar]
- Sourander A, Helstela L, Helenius H. Parent-adolescent agreement on emotional and behavioral problems. Social Psychiatry and Psychiatric Epidemiology. 1999;34:657–663. doi: 10.1007/s001270050189. [DOI] [PubMed] [Google Scholar]
- Stanger C, Lewis M. Agreement among parents, teachers, and children on internalizing and externalizing behavior problems. Journal of Clinical Child Psychology. 1993;22:107–115. [Google Scholar]
- Tarullo LB, Richardson DT, Radke-Yarrow M, Martinez PE. Multiple sources in child diagnosis: Parent-child concordance in affectively ill and well families. Journal of Clinical Child Psychology. 1995;24:173–183. [Google Scholar]
- Treutler CM, Epkins CC. Are discrepancies among child, mother, and father reports on children's behavior related to parents' psychological symptoms and aspects of parent-child relationships? Journal of Abnormal Child Psychology. 2003;31:13–27. doi: 10.1023/a:1021765114434. [DOI] [PubMed] [Google Scholar]
- Velez CN, Cohen P. Suicidal behavior and ideation in a community sample of children: Maternal and youth reports. Journal of the American Academy of Child & Adolescent Psychiatry. 1988;27:349–356. doi: 10.1097/00004583-198805000-00014. [DOI] [PubMed] [Google Scholar]
- Verhulst FC, Van der Ende J. Agreement between parents' reports and adolescents' self-reports of problem behavior. Journal of Child Psychology and Psychiatry. 1992;33:1011–1023. doi: 10.1111/j.1469-7610.1992.tb00922.x. [DOI] [PubMed] [Google Scholar]
- Walker M, Moreau D, Weissman MM. Parents' awareness of children's suicide attempts. American Journal of Psychiatry. 1990;147:1364–1366. doi: 10.1176/ajp.147.10.1364. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Adams P, Wolk S, Verdeli H, Olfson M. Brief screening for family psychiatric history: The Family History Screen. Archives of General Psychiatry. 2000;57:675–682. doi: 10.1001/archpsyc.57.7.675. [DOI] [PubMed] [Google Scholar]
- Yeh M, Weisz JR. Why are we here at the clinic? Parent-child (dis)agreement on referral problems at outpatient treatment entry. Journal of Consulting and Clinical Psychology. 2001;69:1018–1025. doi: 10.1037//0022-006x.69.6.1018. [DOI] [PubMed] [Google Scholar]
- Youngstrom E, Izard C, Ackerman B. Dysphoria-related bias in maternal ratings of children. Journal of Consulting and Clinical Psychology. 1999;67:905–916. doi: 10.1037//0022-006x.67.6.905. [DOI] [PubMed] [Google Scholar]
- Youngstrom E, Loeber R, Stouthamer-Loeber M. Patterns and correlates of agreement between parent, teacher, and male adolescent ratings of externalizing and internalizing problems. Journal of Consulting and Clinical Psychology. 2000;68:1038–1050. doi: 10.1037//0022-006x.68.6.1038. [DOI] [PubMed] [Google Scholar]
- Zimmerman JK, Asnis GM. Parents' knowledge of children's suicide attempts. American Journal of Psychiatry. 1991;148:1091–1092. doi: 10.1176/ajp.148.8.aj14881091. [DOI] [PubMed] [Google Scholar]


