Abstract
SYNOPSIS
There is a growing body of literature associating abnormal scapular positions and motions, and, to a lesser degree, clavicular kinematics with a variety of shoulder pathologies. The purpose of this manuscript is to (1) review the normal kinematics of the scapula and clavicle during arm elevation, (2) review the evidence for abnormal scapular and clavicular kinematics in glenohumeral joint pathologies, (3) review potential biomechanical implications and mechanisms of these kinematic alterations, and (4) relate these biomechanical factors to considerations in the patient management process for these disorders. There is evidence of scapular kinematic alterations associated with shoulder impingement, rotator cuff tendinopathy, rotator cuff tears, glenohumeral instability, adhesive capsulitis, and stiff shoulders. There is also evidence for altered muscle activation in these patient populations, particularly, reduced serratus anterior and increased upper trapezius activation. Scapular kinematic alterations similar to those found in patient populations have been identified in subjects with a short rest length of the pectoralis minor, tight soft-tissue structures in the posterior shoulder region, excessive thoracic kyphosis, or with flexed thoracic postures. This suggests that attention to these factors is warranted in the clinical evaluation and treatment of these patients. The available evidence in clinical trials supports the use of therapeutic exercise in rehabilitating these patients, while further gains in effectiveness should continue to be pursued.
Keywords: acromioclavicular joint, biomechanics, rotator cuff, scapula, shoulder
Shoulder pain and associated glenohumeral joint movement dysfunctions are common and debilitating conditions.12,84,117 The most frequently occurring problems include shoulder impingement and associated rotator cuff disease or tendinopathy, which can progress to rotator cuff tears,24,84 as well as glenohumeral joint instability and adhesive capsulitis. With the exception of adhesive capsulitis, the majority of these shoulder complaints are related to occupational or athletic activities that involve frequent use of the arm at, or above, shoulder level. The point prevalence of shoulder pain in certain sports or occupations can reach 40% or higher.31,41,68
Shoulder impingement has been defined as compression, entrapment, or mechanical irritation of the rotator cuff structures and/or long head of the biceps tendon either beneath the coracoacromial arch (subacromial) or between the undersurface of the rotator cuff and the glenoid or glenoid labrum (internal). Repetitive impingement is one of multiple proposed mechanisms for the development of rotator cuff disease, as well as progression to partial or full-thickness rotator cuff tearing.87,106
The pathogenesis of rotator cuff tendinopathy is not precisely known and is somewhat controversial; however, a multifactorial etiology is likely.81,106 Proposed mechanisms include (1) anatomic reductions in the available space beneath the coracoacromial arch or within the supraspinatus outlet area leading to subacromial impingement,129 (2) intrinsic tendon degeneration from eccentric overload, ischemia, aging, or inferior tissue properties,106 and (3) scapular or humeral movement alterations compromising the rotator cuff tissues through subacromial or internal impingement.84 There is evidence in an animal model for eccentric overuse, or eccentric overuse combined with reduced available subacromial space (subacromial impingement), as a factor resulting in the development of rotator cuff tendinopathy.106 Such factors are likely of greatest interest to physical therapists, as rehabilitation programs are often directed at correction of posture or movement deviations believed to reduce the subacromial space, or directed at improvement of tissue properties through stretching and strengthening. Regardless of initial etiology, movement deviations that further compromise the subacromial space or contribute to internal impingement are presumed undesirable in the presence of a rotator cuff or long head of the biceps tendinopathy. The majority of rotator cuff tears are believed to be a progression of cumulative trauma from shoulder impingement or progressive rotator cuff disease, rather than a consequence of acute trauma.87
Glenohumeral joint instability is generally classified as traumatic or atraumatic in origin, as well as by direction of the instability (anterior, posterior, inferior, or multidirectional). Instability can also occur from repetitive microtrauma, particularly in overhead athletes. Primary complaints may relate to dysfunction or pain, with underlying instability often contributing to the development of secondary impingement or rotator cuff tendinopathy. Adhesive capsulitis, which is often idiopathic in origin, can also contribute to secondary impingement or rotator cuff disease.
There is a growing body of literature associating abnormal scapulothoracic kinematics, and, to a lesser degree, clavicular kinematics, with a variety of shoulder pathologies. Abnormal scapular or clavicular kinematics have been identified in populations with shoulder impingement,25,44,58,64,71,73,77,123 rotator cuff tendinopathy,64,82 rotator cuff tears,20,82,92 shoulder instability,46,90,91,92,119,123 and adhesive capsulitis.28,65,99,118 The purpose of this manuscript is to (1) review the normal kinematics of the scapula and clavicle during arm elevation, (2) review the evidence for abnormal scapular and clavicular kinematics in the above identified glenohumeral joint pathologies, (3) review potential biomechanical implications and mechanisms of these kinematic alterations, and (4) relate these biomechanical factors to considerations in the clinical evaluation and treatment of these disorders.
SCAPULAR KINEMATICS DURING ARM ELEVATION
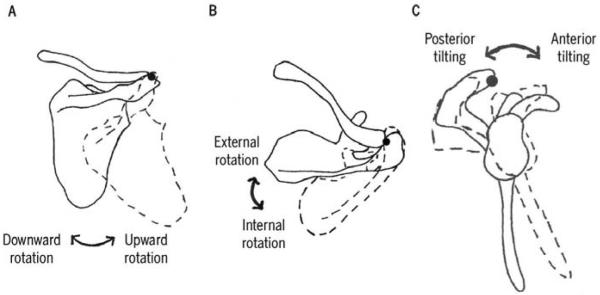
Scapular position on the thorax and control during motion is a critical component of normal shoulder function. During elevation of the arm overhead, the scapula should upwardly rotate and posteriorly tilt on the thorax (FIGURE).78 Upward rotation is the predominant scapulothoracic motion. The motion of the scapula with regard to changes in scapular internal rotation angle shows more variability across subjects, investigations, planes of elevation, and point in the range of motion of elevation.4,78 Slight increases in scapular internal rotation may be normal early in the range of arm elevation in scapular plane abduction and flexion. It is generally accepted that end range elevation in healthy subjects involves some scapulothoracic external rotation, although limited data are available.78
FIGURE.
Scapular motions from (A) posterior (upward/downward rotation), (B) superior (internal/external rotation), and (C) lateral (anterior/posterior tilting) views. Axes of rotation are indicated as black dots. Reprinted with permission from Borich et al.2
Scapulothoracic kinematics involve combined sternoclavicular (SC) and acromioclavicular (AC) joint motions.69,78,110 Substantive 3-dimensional motions occur at both the SC and AC joints during arm elevation in healthy subjects.69,78,110 The clavicle demonstrates a pattern of slight elevation and increasing retraction as arm elevation progresses overhead.69,78 Simultaneously, the scapula is upwardly rotating, internally rotating, and posteriorly tilting relative to the clavicle at the AC joint.110 Scapulothoracic “translations” of elevation/depression and abduction/adduction have also traditionally been described.73,110 These motions actually derive from clavicular motions at the SC joint. Scapulothoracic elevation is a result of SC elevation, and abduction/adduction is a result of SC protraction/retraction.110
Scapular Kinematic Alterations in Shoulder Impingement or Rotator Cuff Disease
The largest number of studies investigating scapular kinematic alterations have been completed in the area of shoulder impingement or rotator cuff disease.25,38,44,58,64,71,73,77,82,107,123 Substantial variations are present across studies with regard to subject demographics, clinical presentation, measurement methodologies, arm movements tested, scapular kinematic descriptions, and portions of the range of motion where deviations were described. However, identified deviations can be generally summarized as presence or absence of significant alterations in scapular upward rotation, posterior tilt, internal rotation, clavicular elevation or retraction, scapular symmetry and topography, or scapulohumeral rhythm (TABLE 1).
TABLE 1.
Investigations of Abnormal Scapular Kinematics During Humeral Elevation in Subjects With Shoulder Impingement or Rotator Cuff Tendinopathy
| Investigation | General Methods | Sample | Position Alteration Investigated | Significant Deviation Identified |
|---|---|---|---|---|
| Warner et al123 | Moiré topographic analysis | 22 controls, 7 with impingement, 17-47 years old, both genders | • Scapular asymmetry, increased topography or winging | • Increased asymmetry and topography in impingement group |
| Lukasiewicz et al73 | Static digitizing, comparisons between groups and sides | 20 nonimpaired, 17 with impingement, 25-66 years old, both genders | • Upward rotation | • No significant differences |
| • Posterior tilt | • Decreased in the impingement group and side of impingement | |||
| • Internal rotation | • No significant differences | |||
| • Elevation | • Increased in the impingement group | |||
| Ludewig and Cook71 | Electromagnetic surface sensors | 26 controls, 26 with impingement, 20-71 years old, males only, overhead construction workers | • Upward rotation | • Decreased in the impingement group |
| • Posterior tilt | • Decreased in the impingement group | |||
| • Internal rotation | • Increased in the impingement group | |||
| Graichen et al38 | Supine static MRI, comparisons between groups and sides | 14 controls, 14 with unilateral impingement, no full-thickness tear, 22-62 years old, both genders | • Upward rotation | • No significant differences |
| Endo et al26 | Static radiographs, comparisons between sides | 27 with unilateral impingement, 41-73 years old, both genders | • Upward rotation | • Decreased on the side of impingement |
| • Posterior tilt | • Decreased on the side of impingement | |||
| • Internal rotation | • No significant differences | |||
| Hebert et al44 | Optical surface sensors, comparisons between groups and sides | 10 healthy, 41 with impingement, 30-60 years old, both genders | • Upward rotation | • No significant differences |
| • Posterior tilt | • No significant differences | |||
| • Internal rotation | • Increased on the side of impingement | |||
| Su et al107 | Static digital inclinometer, comparisons between groups and before and after swim practice | 20 healthy, 20 with impingement, 18-35 years old, both genders, swimmers | • Upward rotation | • Decreased after practice in the impingement group |
| Mell et al82 | Electromagnetic surface sensors | 15 healthy, 13 with rotator cuff tendi-nopathy, no full-thickness tears, 30-74 years old, both genders | • Scapulohumeral rhythm | • No significant differences |
| McClure et al77 | Electromagnetic surface sensors | 45 controls, 45 with impingement, 24-74 years old, both genders | • Upward rotation | • Increased in the impingement group |
| • Posterior tilt | • Increased in the impingement group | |||
| • Internal rotation | • No significant differences | |||
| • Elevation | • Increased in the impingement group | |||
| • Retraction | • Increased in the impingement group | |||
| Lin et al64 | Electromagnetic surface sensors | 25 controls, 21 with shoulder dysfunction, 27-82 years old, males only | • Upward rotation | • Decreased in the shoulder dysfunction group |
| • Posterior tilt | • Decreased in the shoulder dysfunction group | |||
| • Internal rotation | • No significant differences | |||
| • Elevation | • Increased in the shoulder dysfunction group | |||
| Laudner et al58 | Electromagnetic surface sensors | 11 controls, 11 with internal impingement, 18-30 years old, males only, throwers | • Upward rotation | • No significant differences |
| • Posterior tilt | • Increased in the internal impingement group | |||
| • Internal rotation | • No significant differences | |||
| • Elevation | • Increased at higher angles in the internal impingement group | |||
| • Retraction | • No significant differences |
Overall, the evidence for scapular kinematic alterations in patients with impingement or rotator cuff symptoms is substantial, with 9 of 11 cited studies identifying a significant group difference in at least 1 variable (TABLE 1).25,38,44,58,64,71,73,77,82,107,123 However, there are discrepancies regarding the consistency of findings and direction of deviations noted. Of the studies specifically investigating scapular upward rotation during arm elevation, 4 of 9 found decreased upward rotation,25,64,71,107 1 increased upward rotation,77 and 4 no differences38,44,58,73 in symptomatic subjects, when compared to asymptomatic individuals. Somewhat greater consistency in findings is present for measurements of scapular posterior tilt during arm elevation, with 4 of 7 studies finding decreased posterior tilt in symptomatic subjects,25,64,71,73 2 increased posterior tilt,58,77 and 1 no significant difference.44 For scapular internal rotation, only 2 of 7 studies found an increase in internal rotation in symptomatic subjects,44,71 and the remaining 5 found no significant differences between symptomatic and asymptomatic individuals.25,58,64,73,77 Findings for alteration in clavicular or scapular elevation were most consistent across studies with elevation being significantly increased in symptomatic subjects in all 4 of the studies investigating this variable.58,64,73,77 Clavicular retraction in subjects with impingement was found to be increased in 1 study77 and not significantly altered in the other.58
The inability to detect significant differences between groups for all variables consistently across investigations is not fully surprising. Investigations are often undertaken with small sample sizes, resulting in limited statistical power for some comparisons, given the large variation in movement patterns of healthy subjects.71,78 The 2 investigations noted above as finding no group differences38,82 had only 14 and 13 subjects with impingement or tendinopathy, respectively. Investigators have tested various planes of shoulder elevation, with and without external loading or other factors, such as fatigue. The most common measurement method uses surface motion sensors whose precision is impacted by skin motion artifact.52 More precise imaging methods, such as 3-dimensional magnetic resonance imaging, have, to date, been primarily limited to static imaging in supine positions without normal gravitational loading.38
Lack of significant differences between groups also likely relates to the presumed multifactorial etiology of impingement and the limitations of clinical diagnosis. Even if one assumes that scapular kinematic alterations are one of the definite causative mechanisms of impingement and rotator cuff tendinopathy, not all subjects in a particular sample are likely to have scapular position or motion deviations. Furthermore, different scapular kinematic alterations may be present in different subgroups of subjects. These subgroup deviations may not be detected in group averages.38 Currently, the presence, absence, or type of specific scapular kinematic deviation is not well distinguished in the clinical diagnostic process inherent to the inclusion criteria of most investigations. In particular, individuals with internal impingement may have very different scapular kinematic alterations as compared to those with subacromial impingement. Only 1 group of investigators to date has compared a small sample of 11 subjects with internal impingement to a control group of throwers,58 and this is 1 of the 2 investigations with disparate findings regarding scapular posterior tilt. Other investigators have predominately presumed that their subject sample's impingement is subacromial but have not identified criteria to distinguish or exclude internal impingement. Additionally, the impact of factors such as age, arm dominance, gender, and upper extremity “exposure” to occupational or athletic activities on scapular kinematics are not well understood and vary substantially across investigations. Finally, progression of tendinopathy to partial- or full-thickness rotator cuff tearing is considered a continuum of the disease process.87 Although most studies attempt to exclude full-thickness tearing based on clinical examination, only 2 investigations used imaging methods to exclude subjects with full-thickness rotator cuff tears from their tested samples.38,82 No investigations used diagnostic methods able to exclude partial-thickness cuff tears.
The effect of rotator cuff tears on scapular kinematics may be of particular interest with regard to the discussion of disparate results between studies. Five investigations to date have compared the scapular kinematics of small subject samples (6 to 20 individuals with cuff tear) with known full-thickness tears to controls during arm elevation.20,38,82,92,128 All of those studies noted tendencies toward increased scapular upward rotation during arm elevation, although only 2 investigations measured differences showing statistically significant alterations in scapulohumeral rhythm.20,82 All authors suggested that these alterations were compensatory to maximize arm elevation in the absence of intact rotator cuff function. Interestingly, in 1 investigation, surgical cuff repair appeared to “normalize” the presumed compensation.92 Further support for a theory of compensatory scapular upward rotation in the absence of an intact rotator cuff is provided by an investigation of healthy subjects before and after a suprascapular nerve block to produce experimental dysfunction of the supraspinatus and infraspinatus muscles.79 Following nerve block, subjects demonstrated significant increases in scapular upward rotation and external rotation during arm elevation.79 Consideration of these findings suggests that increased scapular upward rotation may be a positive compensation in the presence of rotator cuff dysfunction. Variations in scapular upward rotation findings during arm elevation across investigations of subjects with shoulder impingement might relate to the limited clinical knowledge of status or severity of involvement of the rotator cuff, particularly with regard to full- or partial-thickness tearing. Increased use of ultrasound imaging in the diagnosis of cuff integrity may be helpful in future work to clarify disparate findings.112
Theorized Effects of Scapular Kinematic Alterations
Without the ability to follow human subjects longitudinally, it is difficult to fully discern if alterations found in scapular kinematics are compensatory or contributory to an impingement mechanism of rotator cuff disease. Further insight may be gained, however, through investigations linking kinematic alterations to reductions in the subacromial space, or proximity of structures such as the glenoid and cuff undersurface in internal impingement. Based on anatomical relationships, it is generally believed that reductions in scapular upward rotation and posterior tilt during arm elevation could reduce the available subacromial space, thus contributing to development or progression of impingement as well as a poorer environment for tissue healing.84 How scapular internal rotation might impact the subacromial space is less clear, as increased scapular internal rotation without altering humeral position should result in greater glenohumeral joint external rotation. Humeral external rotation is presumed beneficial to the subacromial space, allowing improved clearance for the greater tuberosity.30 However, a relative increase in glenohumeral joint external rotation via increased scapular internal rotation might increase the risk for posterior cuff internal impingement.93 The potential impact of clavicular motion alterations on subacromial space or internal impingement is even less well understood. Increased clavicular elevation may improve the available subacromial space through superior movement of the acromioclavicular joint. Alternatively, increased elevation may couple with increased anterior tilt of the scapula, thus possibly compromising the available subacromial space.110
Through magnetic resonance imaging, significant movement-related reductions in the acromiohumeral distance in the symptomatic shoulder of individuals with impingement have been found.37,43 However, these reductions were not linked to specific motion deviations of the scapula or humerus. Only 2 investigations were located to date that have attempted to directly link alterations in scapular kinematics to reductions in the subacromial space.51,105 In a very small investigation of 4 healthy subjects, supine magnetic resonance images were obtained with sandbags holding the scapulae into “protracted” (scapular abduction) or “retracted” (scapular adduction) positions.105 Subsequently, subacromial width and angle were measured in both positions. Significant reductions in the subacromial parameters were identified in the protracted position.105 Review of these sagittal plane changes, however, appears consistent with what would occur with increased anterior tilt of the scapula, rather than scapular protraction.105 Using a cadaver model of subacromial clearance (superior humeral translation prior to significant subacromial contact force), Karduna and colleagues51 investigated the impact of imposed scapular positions of upward rotation, internal rotation, and posterior tilt on the available superior humeral translation. No significant differences were found with changes in scapular internal rotation and posterior tilt.51 Contrary to expectations, increased scapular upward rotation reduced rather than increased the magnitude of available superior humeral translation.51 Although the MR investigation provides support for common presumptions of subacromial space reduction, this cadaver study challenges the common presumptions of how scapular alterations might impact the subacromial space.51,105 Additional investigations linking scapular kinematic alterations to the magnitude of available subacromial space and proximity of potential impinging structures are needed to further ascertain the clinical and biomechanical importance of the kinematic alterations identified in patient populations.
Scapular kinematic Alterations Assiciated with Glenohumeral Joint Instability
The available literature investigating scapular kinematic abnormalities associated with glenohumeral joint instability is also increasing. There are again wide variations in study samples and methodologies, but more consistency in results reported. Five investigations have compared subjects with multidirectional instability to control subjects during elevation of the arm.46,90,91,119,123 Four of these investigations assessed scapular upward rotation either directly, or indirectly by assessing scapulohumeral rhythm.46,90,91,119 All 4 identified significantly less scapular upward rotation or a significantly greater scapulohumeral rhythm ratio (indicative of a lesser scapular upward rotation component) in the subjects with instability.46,90,91,119 Two of these studies also assessed scapular internal rotation and both found significantly greater scapular internal rotation in the subjects with instability.90,119 In their Moiré topographic analysis, Warner and colleagues123 also assessed subjects with instability and reported significantly more scapular “winging” in these subjects. This winging is defined as greater prominence of the scapular medial border consistent with increased internal rotation.123 In the single study found that compared subjects with anterior glenohumeral joint instability to controls, significant differences in scapulohumeral rhythm were observed between groups.92 Early in the range of motion (0°-90°), subjects with instability had a lesser scapular upward rotation contribution to arm elevation, whereas later in the arm elevation range of motion, the scapular contribution was significantly greater.92
Similar to comparisons between subjects with impingement and controls, the cross-sectional nature of these investigations does not provide definitive evidence for either a causative or compensatory mechanism of kinematic alterations. Mechanically, however, reduced scapular upward rotation is believed to be detrimental to maintaining inferior stability at the glenohumeral joint.47 This suggests that these reductions in scapular upward rotation in individuals with multidirectional instability do not represent a positive compensation but likely contribute to inferior glenohumeral joint instability.47 Increased scapular internal rotation is believed to mechanically reduce anterior bony stability; however, a cadaver investigation reported increased glenohumeral joint capsular tension with scapular protraction, which may contribute to overall stability.125 Interestingly, in healthy subjects, glenohumeral elevation and internal and external rotation strength is decreased during isometric testing in scapular protracted positions, which incorporate clavicular protraction and scapulothoracic internal rotation.103,104 Likewise, when overhead athletes with and without impingement symptoms were manually repositioned into increased scapular retraction and posterior tilting, there were significant increases in shoulder elevation strength.109 Further investigation is also needed in subjects with glenohumeral joint instability to better understand the compensatory or causative nature and biomechanical consequences of their scapular kinematic alterations.
Scapular kinematic Alterations Associated With Adhesive Capsulitis or Shoulder Stiffness
Only recently have investigators started to study scapular kinematics during humeral elevation in subjects with adhesive capsulitis or shoulder stiffness.28,65,99,118 Three studies identified significant increases in scapular upward rotation on the affected side of subjects with adhesive capsulitis as compared to their nonaffected side.28,99,118 Vermeulen et al118 were also able to show a change toward a more “normalized” scapular upward rotation after physical therapy intervention, supporting the premise that the increased scapular upward rotation was compensatory to maximize overall range of motion overhead in the presence of reduced mobility at the glenohumeral joint.
Lin and colleagues65 separated “stiff shoulders” into anterior and posterior stiffness at the glenohumeral joint. They found those with anterior glenohumeral joint tightness demonstrated greater scapular upward rotation and less posterior tilt as compared to the individuals in the group with posterior tightness.65 However, they did not compare the scapular kinematics to a control group or to the unaffected arm. In addition, their subjects' range-of-motion deficits were predominately in humeral internal/external rotation rather than humeral elevations.65 As such, these subjects were not identified as representing a group with adhesive capsulitis but described as having anterior or posterior stiffness.65
In summary, scapular or clavicular motion or position alterations are present in persons with a variety of shoulder disorders (TABLE 2). But the causative or compensatory nature of these kinematic alterations and their associated biomechanical implications regarding rotator cuff function remain speculative. Regardless of this compensatory or causative nature, however, it is of interest to understand the biomechanical mechanisms contributing to these alterations. Factors contributing to alterations presumed detrimental might be the focus of rehabilitation. Alternatively, patients might be taught how to produce a compensatory deviation deemed beneficial to reducing pain or improving function or stability.
TABLE 2.
Summary of Scapular Kinematics During Arm Elevation in Healthy and Pathologic States
| Group | Healthy | Impingement or Rotator Cuff Disease | Glenohumeral Joint Instability | Adhesive Capsulitis |
|---|---|---|---|---|
| Primary scapular motion | Upward rotation | Lesser upward rotation | Lesser upward rotation | Greater upward rotation |
| Secondary scapular motion | Posterior tilting | Lesser posterior tilting | No consistent evidence for alteration | No consistent evidence for alteration |
| Accessory scapular motion | Variable internal/external rotation | Greater internal rotation | Greater internal rotation | No consistent evidence for alteration |
| Presumed implications | Maximize shoulder range of motion and available sub-acromial space | Presumed contributory to subacromial or internal impingement | Presumed contributory to lesser inferior and anterior joint stability | Presumed compensatory to minimize functional shoulder range-of-motion loss |
Pontential Biomechanical Mechanisms Contributing To Alterations in Scapular Kinematics
Potential contributing mechanisms to abnormal scapular kinematics include pain, soft tissue tightness, muscle activation or strength imbalances, muscle fatigue, and thoracic posture.84 Muscle activation in patient populations is the most common factor investigated; but these muscle activity alterations are not typically directly linked to scapular kinematic alterations. In subjects with impingement or shoulder dysfunction, significantly less serratus anterior muscle activation and greater upper trapezius activation were found in the same subjects with less scapular upward rotation and posterior tilt,64,71 as well as greater scapular elevation.64 Considering these findings with an understanding of these muscles' ability to produce or control scapular rotations,29,48 the lesser serratus activations may be critical in contributing to the lesser posterior tilt and upward rotation observed. The greater upper trapezius activation is likely contributing to the greater elevation of the scapula through greater clavicular elevation.29,48 It should be kept in mind, however, that this is an interpretation of the results of these studies, as relationships between muscle activation and scapular kinematics were not direct findings of these investigations. Several other investigations provide support for the premise of lesser serratus activation and/or greater upper trapezius activation in a variety of patient populations across a variety of tasks, including swimmers with shoulder pain,100 persons with frozen shoulder,66 throwers with anterior glenohumeral instability,35 overhead athletes with impingement syndrome,14 or persons with various glenohumeral joint pathologies.95 Significantly less protraction force has also been identified in overhead athletes with shoulder impingement as compared to their noninvolved side or a control group.17 None of these latter investigations, however, simultaneously measured scapular kinematics.
Timing of scapulothoracic muscle activation has also been investigated. The temporal recruitment pattern of the upper and lower trapezius and serratus anterior displayed significantly greater variability in competitive freestyle swimmers with shoulder impingement as compared to a control group of competitive swimmers.120 Significantly delayed middle and lower trapezius activation has been demonstrated in overhead athletes with shoulder impingement, as compared to a control group, in response to an unexpected drop of the arm from an abducted position.16 Similar to kinematic findings, although it is generally believed that these altered muscle activations contribute to abnormal scapular kinematics and shoulder pathology, a causative or compensatory motor control mechanism cannot currently be ascertained.
The influence of pain on muscle activation patterns is also poorly understood. Interestingly, experimentally induced pain produced through injection of hypertonic saline directly into the upper, middle, and lower divisions of the trapezius in otherwise healthy subjects, resulted in decreased upper trapezius and increased lower trapezius activation on the painful side and increased trapezius activation on the contralateral side during repetitive bilateral flexion.27 Further investigation of the influence of induction or removal of pain and the relationships between pain state, muscle activation, and scapular kinematics is needed.
Another model to relate muscle activation patterns to alterations in scapular kinematics is the experimental induction of muscle fatigue. However, none of the investigations of shoulder fatigue identified to date have attempted to specifically fatigue isolated scapulothoracic muscles, and the inability to specifically fatigue a single muscle or muscle group complicates interpretation of the findings.23,113 In response to a resisted humeral external rotation fatigue protocol, one investigation demonstrated significant reductions in scapular upward rotation, posterior tilt, and external rotation postfatigue.113 However, another investigation also inducing shoulder fatigue via resisted humeral external rotation found significant increases rather than decreases in scapular upward rotation.23 Findings were similar in direction between the 2 investigations for reduced posterior tilt post fatigue.23,113 When fatiguing the shoulder through repetitive overhead activities22 or resisted elevation,80 significant increases in scapular upward and external rotation, as well as increases in clavicular retraction22 or decreases in scapulohumeral rhythm ratio, consistent with increased scapular upward rotation,80 were found postfatigue. Based on electromyographic analysis of median power frequency in these investigations,22,80 fatigue was present in the deltoid muscles, as well as the scapulothoracic muscles. As all of these investigations attempted to generate or generated fatigue in muscles acting about the glenohumeral joint, the scapular and clavicular kinematic changes have primarily been speculated to be positive compensations to maintain range of motion.22 Although it is clear from these investigations that fatigue of shoulder muscles can alter scapulothoracic kinematics, direct relationships between fatigue of specific and isolated muscles and changes in scapulothoracic kinematics are not presently known. Also, all of these investigations were completed in healthy subjects; thus the clinical significance for patient populations is unknown.
Soft tissue tightness of muscles or structures that can restrict normal scapular motions during arm elevation is another potential mechanism for development of the scapulothoracic alterations seen in patients. Two that have been investigated are pectoralis minor and posterior shoulder tightness.2,6 The pectoralis minor, based on its attachments from the coracoid process to the third to fifth ribs, is capable of producing scapular internal rotation, downward rotation, and anterior tilt.6 Excess active or passive tension in this muscle could subsequently resist the normal scapular upward rotation, posterior tilt, and potentially scapular external rotation that should occur during arm elevation. When healthy subjects were categorized as having a short versus a long pectoralis minor resting length, those with a short pectoralis minor indicative of muscle tightness demonstrated significantly less scapular posterior tilt and greater scapular internal rotation during arm elevation.6
Tightness in the posterior capsule of the glenohumeral joint or posterior shoulder has also been theorized as a potential mechanism for altering scapular kinematics by passively “pulling” the scapula laterally over the thorax, particularly during humeral internal rotation in elevated arm positions.54 In a subsequent investigation, subjects who had no shoulder symptoms but a glenohumeral internal rotation range-of-motion deficit on their dominant arm (indicative of posterior shoulder tightness), were compared to a control group of subjects with no such deficit.2 Scapular positioning was measured at end range humeral internal rotation, with the humerus elevated 90° into both flexion and abduction positions.2 The group with less glenohumeral joint internal rotation range of motion demonstrated significantly greater scapular anterior tilt at end range humeral internal rotation positions.2 Both of these investigations tested subjects without shoulder pain or symptoms, removing any confounding effects of pain on the kinematic findings.2,6 This investigative approach suggests that these areas of soft tissue tightness are potential risk factors for scapular kinematic alterations associated with shoulder impingement, but findings need to be confirmed in patient populations.
Thoracic posture has also been related to alterations in scapular positioning. When healthy subjects were asked to assume a “slouched” sitting posture and elevate the arm, significantly reduced scapular upward rotation and posterior tilt were reported, as well as increased scapular internal rotation and scapular elevation.53 Increased scapular anterior tilt and scapular internal rotation have also been demonstrated with the arm relaxed at the side in women with increased thoracic kyphosis, as well as increased scapular anterior tilt with increased age.18 Significant correlations between increased age and reductions in posterior tilt and upward rotation have also been identified in elevated arm postures,26 although thoracic posture as a possible contributing factor was not assessed in that investigation.
In addition to evidence of scapular kinematic alterations associated with glenohumeral joint pathologies, there is scientific support for a number of biomechanical factors as potential contributing mechanisms to these scapular kinematic alterations. These include alterations in muscle activation (in particular, increased upper trapezius activation and reduced serratus anterior activation), pectoralis minor or posterior shoulder tightness, and thoracic kyphosis or flexed thoracic postures (TABLE 3). These factors should be considered in the clinical evaluation and intervention for such shoulder conditions.
TABLE 3.
Proposed Biomechanical Mechanisms of Scapular Kinematic Deviations
| Mechanism | Associated Effects |
|---|---|
| Inadequate serratus activation | Lesser scapular upward rotation and posterior tilt |
| Excess upper trapezius activation | Greater clavicular elevation |
| Pectoralis minor tightness | Greater scapular internal rotation and anterior tilt |
| Posterior glenohumeral joint soft tissue tightness | Greater scapular anterior tilt |
| Thoracic kyphosis or flexed posture | Greater scapular internal rotation and anterior tilt, lesser scapular upward rotation |
EVALUATION
It is beyond the scope of this manuscript to fully discuss the examination and evaluation process for each of these glenohumeral joint pathologies.74,126 We will therefore provide an overview of the evaluation process and attempt to highlight and integrate considerations of scapular kinematic and biomechanical factors. Assessment of the patient is assumed to include history, systems review, range of motion, quality of movement, strength, and special tests, such as joint laxity, labral tests, and impingement tests.74 Based on the previous discussion of potential scapular contributions to pathologies, assessing the strength of scapulothoracic musculature is important in addition to that of the glenohumeral joint. When a patient presents with shoulder pain and or dysfunction, it is important to rule out cervical pathologies, thoracic outlet syndrome, circulatory and cardiac disorders, symptoms originating from the periscapular region rather than the glenohumeral joint, and glenohumeral arthritis.74 The latter requires radiographic imaging. Although there are clinical tests that attempt to diagnose full-thickness rotator cuff tears, we believe accurate diagnosis of these pathologies requires diagnostic imaging, such as ultrasound or magnetic resonance.74,111,112
Assessment of joint hypermobility or hypomobility is also inherent to clinical examinations. Glenohumeral instability may be a distinct diagnosis without substantive rotator cuff irritation (pain is not the primary complaint). However, often glenohumeral instability contributes to secondary shoulder impingement or rotator cuff tendinopathy. Adhesive capsulitis can also contribute to secondary impingement, but is generally easily identifiable due to the substantive losses in both active and passive range of motion in multiple directions of motion. In addition to understanding the medical pathology, we believe that it is important to identify an underlying movement disorder whenever possible.10,88,89
One of the challenges of the clinical diagnostic process in persons presenting with shoulder pain is the reliable and valid determination of the presence or absence of scapular position or motion alterations. In one investigation, using blinded evaluators who assessed videotaped subjects, moderate kappa values for intertester and intratester reliability were obtained.56 Poorer interrater reliability was obtained in another investigation in which subjects were videotaped and analyzed by therapists who did not know the symptom status of the subjects.45 These reliability values are less than optimally desirable for routine clinical usage. It is possible that improved reliability could be obtained with direct evaluation (as compared to videotape), improved training, or refinement of definitions of movement categories. General recommendations for visual assessment of dynamic scapular motion alterations, or “dyskinesia,” include observation of the scapular medial border and inferior angle during repetitive concentric and eccentric motion (particularly into flexion), and with the addition of hand loads or manual resistance. Additionally, acceptable interrater reliability has been demonstrated for a “scapular assistance test,” by which abnormal scapular motions are attempted to be improved through manual assistance provided by the examiner.97 Symptom reduction during manual scapular repositioning may help to confirm a scapular contribution to pathology.109 Several investigators have ongoing work in the area of visual assessment and scapular assistance tests.32,108
More promising in the current literature is the objective measurement of static scapular positions with clinically available tools such as inclinometers.49,59,96,124 Johnson et al49 demonstrated that a modified digital inclinometer placed along the spine of the scapula could produce good to excellent validity and intrarater reliability of measurements at rest and in elevated arm positions. This high level of intrarater, within-day reliability was also replicated by a second group of investigators using similar methods.124 Although not yet investigated, such methods seem quite plausible for the measurement of clavicular elevation, and may have the potential to be adapted to other scapular position measures. Inclinometer methods have also been demonstrated to have excellent intrarater within-session reliability in the measurement of thoracic kyphosis.62
Recent recommendations are available in the literature regarding the performance of shoulder strength tests.83 In general, greater objectivity and reliability can be obtained by using handheld dynamometers during strength testing.83 Michener et al83 demonstrated high intra-rater reliability between days using handheld dynamometry to assess strength of the 3 portions of the trapezius and the serratus anterior in subjects with shoulder pain and functional loss. Based on the previous discussion of scapular protraction position affecting glenohumeral muscle strength testing, control of scapular protraction position during shoulder strength testing is advised. This premise is supported by significantly higher strength values for supraspinatus testing in a scapular retraction position in patients, healthy controls, and overhead athletes with and without impingement symptoms.55,109
Recommendations regarding impingement tests can also be made based on recent literature. Typically, if used in isolation, these tests have demonstrated high diagnostic sensitivity but low specificity.11,61 Subsequently, accurate diagnosis of impingement requires multiple positive impingement tests, as well as a cluster of other positive findings such as a painful arc of motion and pain with resisted shoulder motions.11,61 Recent literature suggests these traditional impingement tests are potentially creating internal impingement, as well as, or rather than, subacromial impingement.94 A posterior internal impingement test should be considered as well, which involves pain reproduction by placing the subject's arm in 90° abduction and external rotation.36
In addition to the more traditional evaluation procedures, we believe each of the potential biomechanical contributing factors discussed previously should also be considered in the evaluation of patients with shoulder pain. As noted above, thoracic kyphosis can be reliably assessed using inclinometer methods.62 Pectoralis minor resting length can be accurately assessed clinically using a tape measure or caliper placed between attachment landmarks.3 Clinical measurement of posterior and anterior shoulder tightness has been reported to be highly reliable within and between sessions by several investigators.67,86,114 However, the measures may be less reliable over extended periods during which clinical intervention might occur.7 Additional investigation is warranted to expand the battery of reliable and valid clinical tools to assist in the evaluation process for patients presenting with shoulder pain.
INTERVENTION
The intervention plan should follow directly from the clinical evaluation and should incorporate a current understanding of shoulder biomechanics, kinematic alterations, and proposed biomechanical mechanisms of kinematic alterations. In addition to pain control, the current state of practice predominately incorporates therapeutic exercise into the conservative management of shoulder disorders.127 Consistent with the emphasis of this manuscript, our discussion will focus on treatment directed at identified scapular kinematic and muscle activity alterations. We are not advocating lack of attention to the glenohumeral joint in the treatment plan. In fact, recent investigations of eccentric training in the rehabilitation of tendon pathology suggest that consideration of this approach may be beneficial for some patients with rotator cuff tendinopathy.50,98 Greater emphasis on training of the rotator cuff is also likely required for patients for whom glenohumeral instability is the primary complaint, or contributing to secondary impingement. However, this manuscript focuses on scapular aspects of rehabilitation, as well as rehabilitation for shoulder impingement and rotator cuff disease rather than instability or adhesive capsulitis.
In general, we recommend targeting muscles or structures that can limit desired scapular motions for stretching and targeting muscles that can produce desired scapular motions for strengthening (TABLE 4). It is important to recognize that muscle strengthening is not specific to the production of muscle hypertrophy, but also includes neuromuscular contributions to the increase of muscle force production or improvement of muscle activation or timing. Many exercise programs in clinical practice use light or moderate resistance below a threshold that would generate muscular hypertrophy. Subsequently, strength improvements noted from such exercises are related to neuromuscular adaptations. Resistance exercises targeting specific muscles are most commonly investigated in the literature and will be discussed below. However, other neuromuscular exercise approaches127 deserve further investigation.
TABLE 4.
Summary Intervention Considerations for Subacromial Shoulder Impingement
| Scientifically Supported Scapular Interventions |
|---|
| Serratus anterior strengthening or retraining |
| Upper trapezius activation reduction |
| Posterior shoulder stretching |
| Pectoralis minor stretching |
| Thoracic extension posture and exercise |
Based on the biomechanical factors discussed above, with regard to stretching, the pectoralis minor and posterior shoulder and glenohumeral joint capsule are potential candidates for stretching in patients with scapular kinematic alterations.2,6 This approach presumes confirming concerns with the targeted muscles or structures during the clinical evaluation process. For instance, if a patient does not present with any indications of posterior shoulder tightness, posterior shoulder stretching is not advocated. The rationale for stretching at the posterior glenohumeral joint relates to the alterations in scapular position demonstrated in subjects with posterior shoulder tightness.2 Various methods of stretching have been advocated for both of these tissues. Although the literature is limited, there are investigations that have compared across methods regarding improvements in range of motion or potential to adequately lengthen the targeted tissue.5,75 McClure et al75 compared the effectiveness of a “sleeper stretch,” believed to better stabilize the scapula, to a more traditional cross-body stretch for posterior capsule tightness. Asymptomatic subjects' passive internal rotation range of motion was the outcome measure after a 4-week stretching program.75 Both stretching groups were also compared to a control group who did not stretch. Both stretching groups showed significant within-subject improvements in range of motion, as compared to their nonstretched side.75 Surprisingly, however, only the cross-body stretch group demonstrated significant improvement as compared to the control group.75 The mean length change with 3 proposed stretches for the pectoralis minor has also been compared in healthy subjects.5 The stretches included a unilateral self stretch or “corner stretch,” and sitting and supine manual stretches.5 The unilateral corner stretch involves standing facing the corner of 2 walls, placing the hand of the shoulder to stretch on the wall with the humerus abducted 90° and the elbow flexed 90°. The patient then rotates the torso away from the shoulder to be stretched until a gentle stretch of the pectoral muscles is perceived.5 The corner stretch demonstrated the greatest length change, followed by the supine manual stretch.5 This suggests that a corner stretch may be more effective in lengthening the pectoralis minor; however, subjects were not followed over time in a randomized controlled trial.5 Further investigation is warranted regarding the most effective approaches for stretching both of these tissues.
We also believe strengthening or retraining of the serratus anterior muscle deserves substantial attention in the treatment of patients with shoulder pain and associated scapular motion alterations. This recommendation is based on the biomechanical capabilities of the serratus anterior, as the only scapulothoracic muscle that can produce all of the desired 3-dimensional scapular rotations of upward rotation, AC joint posterior tilting, and AC joint external rotation.21,29,115 It has large moment arms for producing these scapular rotations,21,29,115 and the literature demonstrates reduced activation in subjects with shoulder pain and impingement.64,71 The role of the serratus anterior as an external rotator of the scapula may at first seem counterintuitive, as its lateral line of pull around the thorax has resulted in the serratus anterior often being described as creating shoulder protraction. This protraction occurs with the clavicle protracting on the thorax at the SC joint.115 Before this secondary joint rotation can occur, the line of action of the serratus anterior will first pull the vertebral border and inferior angle of the scapula towards the chest wall, creating external rotation of the scapula at the AC joint, and stabilizing the scapula on the thorax as protraction of the clavicle occurs.115
Based on electromyographic assessments, typically in healthy subjects, a number of exercises have been advocated to activate the serratus anterior muscle.19,42,60,72 These have included push-up plus and push-up progression exercises, the “dynamic hug,” supine “punch,” and wall slide exercises.19,42,60,72 If a patient is also demonstrating excess clavicular elevation during humeral elevation, excess activation of the upper trapezius may be occurring. If so, high serratus activation may be desired in the presence of lesser upper trapezius activation, where push-up plus and supine punch exercises may be beneficial, as these exercises demonstrate minimal upper trapezius activation.72 Other considerations in the choice of serratus exercises include the ability of the patient to prevent excess scapular internal rotation, or winging, during the performance of the exercise, and avoidance of impingement positions. Patients having difficulty with scapular control may benefit from the initial use of an exercise, such as the supine punch, where the scapula is stabilized against the table. The “dynamic hug” exercise, as originally described,19 should also be used judiciously, as it places the glenohumeral joint into a position of flexion, adduction, and internal rotation that may be painful for a patient with subacromial impingement. Modification of the dynamic hug into glenohumeral external rotation theoretically should produce similar levels of serratus activation, with less potential risk of reducing the subacromial space.
Another muscle that can be used to stabilize the scapula and facilitate upward rotation is the lower trapezius. Exercises that have been shown to elicit a favorable ratio of lessening upper trapezius activity and increasing lower trapezius activity are shoulder flexion in the side-lying position up to 135°, prone horizontal abduction with external rotation, and shoulder external rotation in side lying.15 If improved scapular external rotation during arm elevation is the therapeutic goal, strengthening of middle and lower trapezius will be an important focus of rehabilitation.29 Because currently there is less evidence for excess scapular internal rotation in persons with subacromial shoulder impingement,44,71 our therapeutic exercise programs70 focus more on serratus anterior exercises and less on middle trapezius or rhomboid exercises. As the available literature continues to expand, it is anticipated that a greater understanding of the appropriate balance of muscular control for producing optimal scapular kinematics will further refine therapeutic exercise approaches.
We believe that prior to strengthening of the rotator cuff muscles the clinician should also work on facilitating correct timing of muscular recruitment.16,120 Aggressive strengthening in the presence of faulty scapular control will only serve to reinforce poor kinematics and likely not provide relief for the patient in terms of pain or improved function.
Given the evidence for altered scapular kinematics with thoracic kyphosis or flexed thoracic postures,18,53 thoracic posture should also be addressed in the rehabilitation of patients with shoulder impingement or rotator cuff tendinopathy. This includes attention to maintaining erect postures during the performance of daily activities involving elevation of the arm, as well as during shoulder exercises. Exercises directed toward improving thoracic extension range of motion, strength, and endurance should also be considered where appropriate to the patient presentation, while also realizing that normal thoracic extension during arm elevation is only 10° or less.116 We would caution, however, to avoid excessive emphasis on shoulder retraction exercises for rhomboid strengthening as part of a postural exercise program, given this muscles' capabilities as a downward rotator of the scapula. Joint mobilization to the thoracic spine may be another rehabilitation approach to consider. In a randomized clinical trial, the addition of manual therapy to a supervised exercise program for shoulder impingement demonstrated significantly greater improvement than supervised exercise alone.1 It should be noted, however, that any use of thoracic mobilization in this trial was case specific and clearly not the only difference between the 2 treatment groups.1
The use of therapeutic taping in shoulder pain has also been recently investigated.63,101 Using thoracic and scapular taping intended to change posture in both subjects with shoulder impingement and healthy subjects, significant changes in posture and increases in arm elevation pain-free range of motion were noted with taping in both groups.63 No significant reduction in pain during arm elevation was achieved in the group with impingement. However, the point in the range of motion at which increased pain was first perceived was significantly higher (average of 15° and 16° increase in pain-free range of motion for scapular plane abduction and flexion, respectively).63 Another investigation demonstrated reduced upper trapezius and increased lower trapezius electromyographic activation with use of taping in subjects with shoulder impingement during arm elevation.101 Further study of this approach in patient populations appears warranted.
Through clinical trials, there is mounting evidence to support the effectiveness of therapeutic exercise approaches in the management of shoulder impingement and rotator cuff tendinopathy.1,8,9,13,33,34,39,40,70,76,85,102,122 There is also some evidence that the addition of manual therapy to stretching and strengthening exercises can further improve outcome.1,13,102 However, the evidence that scapular kinematic alterations identified in these populations can be changed is less strong.57,76,121 One investigation demonstrated significantly decreased thoracic spine “anterior inclination,” decreased scapular upward rotation, and decreased scapular elevation after a 6-week exercise program in healthy subjects.121 Another demonstrated that a 6-week program, which included stretching for anterior shoulder muscles and strengthening for posterior shoulder muscles, significantly reduced “forward shoulder posture” in competitive swimmers as compared to a control group of swimmers.57 However, in the only published investigation, where both functional outcome and scapular kinematics were assessed in subjects with impingement, no significant kinematic differences were found after a 6-week exercise program, despite significant improvements in functional status and reductions in pain.76 It should be recognized that the clinical trials currently available in the literature vary substantially with regard to the choice of specific stretching and strengthening exercises used, “doses” of exercise application, additional interventions, length of intervention and follow-up, and subject demographics and clinical presentation. A further confounder of the effectiveness of any exercise program is patient compliance.
Although there is substantive evidence that therapeutic exercise programs are beneficial, it is also clear that not all subjects are improving, nor do the overall levels of improvement represent complete elimination of symptoms.70 We are hopeful that the ability to clinically discern and diagnose specific shoulder movement dysfunctions, and our understanding of the underlying tissue pathologies, will improve in the future. If that can be achieved, clinicians and researchers may be better able to target specific exercise programs to identified movement deviations and develop and refine clinical practice guidelines supported by research data. For example, a patient presenting with a medical diagnosis of subacromial shoulder impingement consistent with subacromial pain and a primary movement dysfunction of scapular anterior tilting during arm elevation may benefit most from a program of serratus anterior strengthening and pectoralis minor and posterior capsule stretching, as well as attention to thoracic posture. Based on biomechanical considerations, such a patient is less likely to benefit from trapezius strengthening, as the trapezius cannot substantively posteriorly tilt the scapula.29,48,115 Alternatively, another patient presenting with a medical diagnosis of shoulder impingement consistent with posterior impingement and a primary movement dysfunction of excess scapular internal rotation during arm elevation may benefit from a program of both trapezius and serratus anterior strengthening, pectoral stretching, and attention to thoracic posture.29 This premise of targeted exercise programs requires further investigation in patient populations. Clearly, despite the growing expanse of clinically applicable literature regarding glenohumeral joint pathologies, there remains much work to be done.
SUMMARY
In summary, there is evidence of scapular kinematic alterations associated with shoulder impingement, rotator cuff tendinopathy, rotator cuff tears, glenohumeral instability, adhesive capsulitis, and stiff shoulders. There is also evidence for altered muscle activation in these patient populations, in particular, reduced serratus anterior and increased upper trapezius activation. Scapular kinematic alterations similar to those found in patient populations have been identified in subjects with a short rest length of the pectoralis minor, tight posterior shoulder, thoracic kyphosis, or with flexed thoracic postures. This suggests that attention to these factors is warranted in the clinical evaluation and treatment of these patients. The available evidence in clinical trials supports the use of therapeutic exercise in rehabilitating these patients, while further gains in effectiveness should continue to be pursued.
ACKNOWLEDGEMENTS
This work was supported by NIH grants K01HD042491 and R03HD053399 from the National Institute of Child Health and Human Development. The content is solely the responsibility of the authors and does not necessarily represent the views of the National Institute of Child Health and Human Development or the National Institutes of Health.
REFERENCES
- 1.Bang MD, Deyle GD. Comparison of supervised exercise with and without manual physical therapy for patients with shoulder impingement syndrome. J Orthop Sports Phys Ther. 2000;30:126–137. doi: 10.2519/jospt.2000.30.3.126. [DOI] [PubMed] [Google Scholar]
- 2.Borich MR, Bright JM, Lorello DJ, Cieminski CJ, Buisman T, Ludewig PM. Scapular angular positioning at end range internal rotation in cases of glenohumeral internal rotation deficit. J Orthop Sports Phys Ther. 2006;36:926–934. doi: 10.2519/jospt.2006.2241. http://dx.doi.org/10.2519/jospt.2006.2241. [DOI] [PubMed]
- 3.Borstad JD. Measurement of pectoralis minor muscle length: validation and clinical application. J Orthop Sports Phys Ther. 2008;38:169–174. doi: 10.2519/jospt.2008.2723. http://dx.doi.org/10.2519/jospt.2008.2723. [DOI] [PubMed]
- 4.Borstad JD, Ludewig PM. Comparison of scapular kinematics between elevation and lowering of the arm in the scapular plane. Clin Biomech (Bristol, Avon) 2002;17:650–659. doi: 10.1016/s0268-0033(02)00136-5. [DOI] [PubMed] [Google Scholar]
- 5.Borstad JD, Ludewig PM. Comparison of three stretches for the pectoralis minor muscle. J Shoulder Elbow Surg. 2006;15:324–330. doi: 10.1016/j.jse.2005.08.011. http://dx.doi.org/10.1016/j.jse.2005.08.011. [DOI] [PubMed]
- 6.Borstad JD, Ludewig PM. The effect of long versus short pectoralis minor resting length on scapular kinematics in healthy individuals. J Orthop Sports Phys Ther. 2005;35:227–238. doi: 10.2519/jospt.2005.35.4.227. http://dx.doi.org/10.2519/jospt.2005.1669. [DOI] [PubMed]
- 7.Borstad JD, Mathiowetz KM, Minday LE, Prabhu B, Christopherson DE, Ludewig PM. Clinical measurement of posterior shoulder flexibility. Man Ther. 2007;12:386–389. doi: 10.1016/j.math.2006.07.014. http://dx.doi.org/10.1016/j.math.2006.07.014. [DOI] [PubMed]
- 8.Brox JI, Gjengedal E, Uppheim G, et al. Arthroscopic surgery versus supervised exercises in patients with rotator cuff disease (stage II impingement syndrome): a prospective, randomized, controlled study in 125 patients with a 2 1/2-year follow-up. J Shoulder Elbow Surg. 1999;8:102–111. doi: 10.1016/s1058-2746(99)90001-0. [DOI] [PubMed] [Google Scholar]
- 9.Brox JI, Staff PH, Ljunggren AE, Brevik JI. Arthroscopic surgery compared with supervised exercises in patients with rotator cuff disease (stage II impingement syndrome) BMJ. 1993;307:899–903. doi: 10.1136/bmj.307.6909.899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caldwell C, Sahrmann S, Van Dillen L. Use of a movement system impairment diagnosis for physical therapy in the management of a patient with shoulder pain. J Orthop Sports Phys Ther. 2007;37:551–563. doi: 10.2519/jospt.2007.2283. http://dx.doi.org/10.2519/jospt.2007.2283. [DOI] [PubMed]
- 11.Calis M, Akgun K, Birtane M, Karacan I, Calis H, Tuzun F. Diagnostic values of clinical diagnostic tests in subacromial impingement syndrome. Ann Rheum Dis. 2000;59:44–47. doi: 10.1136/ard.59.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chipchase LS, O'Connor DA, Costi JJ, Krishnan J. Shoulder impingement syndrome: preoperative health status. J Shoulder Elbow Surg. 2000;9:12–15. doi: 10.1016/s1058-2746(00)90003-x. [DOI] [PubMed] [Google Scholar]
- 13.Conroy DE, Hayes KW. The effect of joint mobilization as a component of comprehensive treatment for primary shoulder impingement syndrome. J Orthop Sports Phys Ther. 1998;28:3–14. doi: 10.2519/jospt.1998.28.1.3. [DOI] [PubMed] [Google Scholar]
- 14.Cools AM, Declercq GA, Cambier DC, Mahieu NN, Witvrouw EE. Trapezius activity and intramuscular balance during isokinetic exercise in overhead athletes with impingement symptoms. Scand J Med Sci Sports. 2007;17:25–33. doi: 10.1111/j.1600-0838.2006.00570.x. http://dx.doi.org/10.1111/j.1600-0838.2006.00570.x. [DOI] [PubMed]
- 15.Cools AM, Dewitte V, Lanszweert F, et al. Rehabilitation of scapular muscle balance: which exercises to prescribe? Am J Sports Med. 2007;35:1744–1751. doi: 10.1177/0363546507303560. http://dx.doi.org/10.1177/0363546507303560. [DOI] [PubMed]
- 16.Cools AM, Witvrouw EE, Declercq GA, Danneels Cambier DC. Scapular muscle recruitment patterns: trapezius muscle latency with and without impingement symptoms. Am J Sports Med. 2003;31:542–549. doi: 10.1177/03635465030310041101. [DOI] [PubMed] [Google Scholar]
- 17.Cools AM, Witvrouw EE, Declercq GA, Vanderstraeten GG, Cambier DC. Evaluation of isokinetic force production and associated muscle activity in the scapular rotators during a protraction-retraction movement in overhead athletes with impingement symptoms. Br J Sports Med. 2004;38:64–68. doi: 10.1136/bjsm.2003.004952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Culham E, Peat M. Functional anatomy of the shoulder complex. J Orthop Sports Phys Ther. 1993;18:342–350. doi: 10.2519/jospt.1993.18.1.342. [DOI] [PubMed] [Google Scholar]
- 19.Decker MJ, Hintermeister RA, Faber KJ, Hawkins RJ. Serratus anterior muscle activity during selected rehabilitation exercises. Am J Sports Med. 1999;27:784–791. doi: 10.1177/03635465990270061601. [DOI] [PubMed] [Google Scholar]
- 20.Deutsch A, Altchek DW, Schwartz E, Otis JC, Warren RF. Radiologic measurement of superior displacement of the humeral head in the impingement syndrome. J Shoulder Elbow Surg. 1996;5:186–193. doi: 10.1016/s1058-2746(05)80004-7. [DOI] [PubMed] [Google Scholar]
- 21.Dvir Z, Berme N. The shoulder complex in elevation of the arm: a mechanism approach. J Biomech. 1978;11:219–225. doi: 10.1016/0021-9290(78)90047-7. [DOI] [PubMed] [Google Scholar]
- 22.Ebaugh DD, McClure PW, Karduna AR. Effects of shoulder muscle fatigue caused by repetitive overhead activities on scapulothoracic and glenohumeral kinematics. J Electromyogr Kinesiol. 2006;16:224–235. doi: 10.1016/j.jelekin.2005.06.015. http://dx.doi.org/10.1016/j.jelekin.2005.06.015. [DOI] [PubMed]
- 23.Ebaugh DD, McClure PW, Karduna AR. Scapulothoracic and glenohumeral kinematics following an external rotation fatigue protocol. J Orthop Sports Phys Ther. 2006;36:557–571. doi: 10.2519/jospt.2006.2189. http://dx.doi.org/10.2519/jospt.2006.2189. [DOI] [PubMed]
- 24.Ellenbecker TS, Derscheid GL. Rehabilitation of overuse injuries of the shoulder. Clin Sports Med. 1989;8:583–604. [PubMed] [Google Scholar]
- 25.Endo K, Ikata T, Katoh S, Takeda Y. Radiographic assessment of scapular rotational tilt in chronic shoulder impingement syndrome. J Orthop Sci. 2001;6:3–10. doi: 10.1007/s007760170017. [DOI] [PubMed] [Google Scholar]
- 26.Endo K, Yukata Yasui N. lnfuence of age on scapulo-thoracic orientation. Clin Biomech (Bristol, Avon) 2004;19:1009–1013. doi: 10.1016/j.clinbiomech.2004.07.011. http://dx.doi.org/10.1016/j.clinbiomech.2004.07.011. [DOI] [PubMed]
- 27.Falla D, Farina D, Graven-Nielsen T. Experimental muscle pain results in reorganization of coordination among trapezius muscle subdivisions during repetitive shoulder flexion. Exp Brain Res. 2007;178:385–393. doi: 10.1007/s00221-006-0746-6. http://dx.doi.org/10.1007/s00221-006-0746-6. [DOI] [PubMed]
- 28.Fayad F, Roby-Brami A, Yazbeck C, et al. Threedimensional scapular kinematics and scapulohumeral rhythm in patients with glenohumeral osteoarthritis or frozen shoulder. J Biomech. 2008;41:326–332. doi: 10.1016/j.jbiomech.2007.09.004. http://dx.doi.org/10.1016/j.jbiomech.2007.09.004. [DOI] [PubMed]
- 29.Fey AJ, Dorn CS, Busch BP, Laux LA, Hassett DR, Ludewig PM. Potential torque Capabilities of the trapezius [abstract] J Orthop Sports Phys Ther. 2007;37:A44–A45. [Google Scholar]
- 30.Flatow EL, Soslowsky LJ, Ticker JB, et al. Excursion of the rotator cuff under the acromion. Patterns of subacromial contact. Am J Sports Med. 1994;22:779–788. doi: 10.1177/036354659402200609. [DOI] [PubMed] [Google Scholar]
- 31.Fleisig GS, Barrentine SW, Zheng N, Escamilla RF, Andrews JR. Kinematic and kinetic comparison of baseball pitching among various levels of development. J Biomech. 1999;32:1371–1375. doi: 10.1016/s0021-9290(99)00127-x. [DOI] [PubMed] [Google Scholar]
- 32.Gard K, Finocchiaro J, Ebaugh DD. lnterrter reliability of a propsed scapular classification system [abstract] J Orthop Sports Phys Ther. 2006;36:A10. [Google Scholar]
- 33.Ginn KA, Cohen ML. Conservative treatment for shoulder pain: prognostic indicators of outcome. Arch Phys Med Rehabil. 2004;85:1231–1235. doi: 10.1016/j.apmr.2003.09.013. http://dx.doi.org/10.1016/j.apmr.2003.09.013. [DOI] [PubMed]
- 34.Ginn KA, Herbert RD, Khouw W, Lee R. A randomized, controlled clinical trial of a treatment for shoulder pain. Phys Ther. 1997;77:802–809. doi: 10.1093/ptj/77.8.802. discussion 810-801. [DOI] [PubMed] [Google Scholar]
- 35.Glousman R, Jobe F, Tibone J, Moynes D, Antonelli D, Perry J. Dynamic electromyographic analysis of the throwing shoulder with glenohumeral instability. J Bone Joint Surg Am. 1988;70:220–226. [PubMed] [Google Scholar]
- 36.Gold GE, Pappas GP, Blemker SS, et al. Abduction and external rotation in shoulder impingement: an open MR study on healthy volunteers initial experience. Radiology. 2007;244:815–822. doi: 10.1148/radiol.2443060998. http://dx.doi.org/10.1148/radiol.2443060998. [DOI] [PubMed]
- 37.Graichen H, Bonel H, Stammberger T, et al. Three-dimensional analysis of the width of the subacromial space in healthy subjects and patients with impingement syndrome. AJR Am J Roentgenol. 1999;172:1081–1086. doi: 10.2214/ajr.172.4.10587151. [DOI] [PubMed] [Google Scholar]
- 38.Graichen H, Stammberger T, Bonel H, et al. Three-dimensional analysis of shoulder girdle and supraspinatus motion patterns in patients with impingement syndrome. J Orthop Res. 2001;19:1192–1198. doi: 10.1016/S0736-0266(01)00035-3. http://dx.doi.org/10.1016/S0736-0266(01)00035-3. [DOI] [PubMed]
- 39.Haahr JP, Andersen JH. Exercises may be as efficient as subacromial decompression in patients with subacromial stage ll impingement: 4-8-years' follow-up in a prospective, randomized study. Scand J Rheumatol. 2006;35:224–228. doi: 10.1080/03009740600556167. http://dx.doi.org/10.1080/03009740600556167. [DOI] [PubMed]
- 40.Haahr JP, Ostergaard S, Dalsgaard J, et al. Exercises versus arthroscopic decompression in patients with subacromial impingement: a randomised, controlled study in 90 cases with a one year follow up. Ann Rheum Dis. 2005;64:760–764. doi: 10.1136/ard.2004.021188. http://dx.doi.org/10.1136/ard.2004.021188. [DOI] [PMC free article] [PubMed]
- 41.Hagberg M, Wegman DH. Prevalence rates and odds ratios of shoulder-neck diseases in different occupational groups. Br J Ind Med. 1987;44:602–610. doi: 10.1136/oem.44.9.602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hardwick DH, Beebe JA, McDonnell MK, Lang CE. A comparison of serratus anterior muscle activation during a wall slide exercise and other traditional exercises. J Orthop Sports Phys Ther. 2006;36:903–910. doi: 10.2519/jospt.2006.2306. http://dx.doi.org/10.2519/jospt.2006.2306. [DOI] [PubMed]
- 43.Hebert LJ, Moffet H, Dufour M, Moisan C. Acromiohumeral distance in a seated position in persons with impingement syndrome. J Magn Reson Imaging. 2003;18:72–79. doi: 10.1002/jmri.10327. http://dx.doi.org/10.1002/jmri.10327. [DOI] [PubMed]
- 44.Hebert LJ, Moffet H, McFadyen BJ, Dionne CE. Scapular behavior in shoulder impingement syndrome. >Arch Phys Med Rehabil. 2002;83:60–69. doi: 10.1053/apmr.2002.27471. [DOI] [PubMed] [Google Scholar]
- 45.Hickey BW, Milosavljevic S, Bell ML, Milburn PD. Accuracy and reliability of observational motion analysis in identifying shoulder symptoms. Man Ther. 2007;12:263–270. doi: 10.1016/j.math.2006.05.005. http://dx.doi.org/10.1016/j.math.2006.05.005. [DOI] [PubMed]
- 46.lllyes A, Kiss RM. Kinematic and muscle activity characteristics of multidirectional shoulder joint instability during elevation. Knee Surg Sports Traumatol Arthrosc. 2006;14:673–685. doi: 10.1007/s00167-005-0012-7. http://dx.doi.org/10.1007/s00167-005-0012-7. [DOI] [PubMed]
- 47.ltoi E, Motzkin NE, Morrey BF, An KN. Scapular inclination and inferior stability of the shoulder. J Shoulder Elbow Surg. 1992;1:131–139. doi: 10.1016/1058-2746(92)90090-P. [DOI] [PubMed] [Google Scholar]
- 48.Johnson G, Bogduk N, Nowitzke A, House D. Anatomy and actions of the trapezius muscle. Clin Biomech (Bristol, Avon) 1994;9:44–50. doi: 10.1016/0268-0033(94)90057-4. [DOI] [PubMed] [Google Scholar]
- 49.Johnson MP, McClure PW, Karduna AR. New method to assess scapular upward rotation in subjects with shoulder pathology. J Orthop Sports Phys Ther. 2001;31:81–89. doi: 10.2519/jospt.2001.31.2.81. [DOI] [PubMed] [Google Scholar]
- 50.Jonsson P, Wahlstrom P, Ohberg L, Alfredson H. Eccentric training in chronic painful impingement syndrome of the shoulder: results of a pilot study. Knee Surg Sports Traumatol Arthrosc. 2006;14:76–81. doi: 10.1007/s00167-004-0611-8. http://dx.doi.org/10.1007/s00167-004-0611-8. [DOI] [PubMed]
- 51.Karduna AR, Kerner PJ, Lazarus MD. Contact forces in the subacromial space: effects of scapular orientation. J Shoulder Elbow Surg. 2005;14:393–399. doi: 10.1016/j.jse.2004.09.001. http://dx.doi.org/10.1016/j.jse.2004.09.001. [DOI] [PubMed]
- 52.Karduna AR, McClure PW, Michener LA, Sennett B. Dynamic measurements of three-dimensional scapular kinematics: a validation study. J Biomech Eng. 2001;123:184–190. doi: 10.1115/1.1351892. [DOI] [PubMed] [Google Scholar]
- 53.Kebaetse M, McClure P, Pratt NA. Thoracic position effect on shoulder range of motion, strength, and three-dimensional scapular kinematics. Arch Phys Med Rehabil. 1999;80:945–950. doi: 10.1016/s0003-9993(99)90088-6. [DOI] [PubMed] [Google Scholar]
- 54.Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26:325–337. doi: 10.1177/03635465980260022801. [DOI] [PubMed] [Google Scholar]
- 55.Kibler WB, Sciascia A, Dome D. Evaluation of apparent and absolute supraspinatus strength in patients with shoulder injury using the scapular retraction test. Am J Sports Med. 2006;34:1643–1647. doi: 10.1177/0363546506288728. http://dx.doi.org/10.1177/0363546506288728. [DOI] [PubMed]
- 56.Kibler WB, Uhl TL, Maddux JW, Brooks PV, Zeller B, McMullen J. Qualitative clinical evaluation of scapular dysfunction: a reliability study. J Shoulder Elbow Surg. 2002;11:550–556. doi: 10.1067/mse.2002.126766. http://dx.doi.org/10.1067/mse.2002.126766. [DOI] [PubMed]
- 57.Kluemper M, Uhl TL, Hazelrigg H. Effect of stretching and strengthening shoulder muscles on forward shoulder posture in competitive swimmers. J Sport Rehab. 2006;15:58–70. [Google Scholar]
- 58.Laudner KG, Myers JB, Pasquale MR, Bradley JP, Lephart SM. Scapular dysfunction in throwers with pathologic internal impingement. J Orthop Sports Phys Ther. 2006;36:485–494. doi: 10.2519/jospt.2006.2146. http://dx.doi.org/10.2519/jospt.2006.2146. [DOI] [PubMed]
- 59.Laudner KG, Stanek JM, Meister K. Differences in scapular upward rotation between baseball pitchers and position players. Am J Sports Med. 2007;35:2091–2095. doi: 10.1177/0363546507305098. http://dx.doi.org/10.1177/0363546507305098. [DOI] [PubMed]
- 60.Lear LJ, Gross MT. An electromyographical analysis of the scapular stabilizing synergists during a push-up progression. J Orthop Sports Phys Ther. 1998;28:146–157. doi: 10.2519/jospt.1998.28.3.146. [DOI] [PubMed] [Google Scholar]
- 61.Leroux JL, Thomas E, Bonnel F, Blotman F. Diagnostic value of clinical tests for shoulder impingement syndrome. Rev Rhum Engl Ed. 1995;62:423–428. [PubMed] [Google Scholar]
- 62.Lewis JS, Green A, Wright C. Subacromial impingement syndrome: the role of posture and muscle imbalance. J Shoulder Elbow Surg. 2005;14:385–392. doi: 10.1016/j.jse.2004.08.007. http://dx.doi.org/10.1016/j.jse.2004.08.007. [DOI] [PubMed]
- 63.Lewis JS, Wright C, Green A. Subacromial impingement syndrome: the effect of changing posture on shoulder range of movement. J Orthop Sports Phys Ther. 2005;35:72–87. doi: 10.2519/jospt.2005.35.2.72. http://dx.doi.org/10.2519/jospt.2005.1578. [DOI] [PubMed]
- 64.Lin JJ, Hanten WP, Olson SL, et al. Functional activity characteristics of individuals with shoulder dysfunctions. J Electromyogr Kinesiol. 2005;15:576–586. doi: 10.1016/j.jelekin.2005.01.006. http://dx.doi.org/10.1016/j.jelekin.2005.01.006. [DOI] [PubMed]
- 65.Lin JJ, Lim HK, Yang JL. Effect of shoulder tightness on glenohumeral translation, scapular kinematics, and scapulohumeral rhythm in subjects with stiff shoulders. J Orthop Res. 2006;24:1044–1051. doi: 10.1002/jor.20126. http://dx.doi.org/10.1002/jor.20126. [DOI] [PubMed]
- 66.Lin JJ, Wu YT, Wang SF, Chen SY. Trapezius muscle imbalance in individuals suffering from frozen shoulder syndrome. Clin Rheumatol. 2005;24:569–575. doi: 10.1007/s10067-005-1105-x. http://dx.doi.org/10.1007/s10067-005-1105-x. [DOI] [PubMed]
- 67.LIN JJ, Yang JL. Reliability and validity of shoulder tightness measurement in patients with stiff shoulders. Man Ther. 2006;11:146–152. doi: 10.1016/j.math.2005.05.002. http://dx.doi.org/10.1016/j.math.2005.05.002. [DOI] [PubMed]
- 68.Lo YP, Hsu YC, Chan KM. Epidemiology of shoulder impingement in upper arm sports events. Br J Sports Med. 1990;24:173–177. doi: 10.1136/bjsm.24.3.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ludewig PM, Behrens SA, Meyer SM, Spoden SM, Wilson LA. Three-dimensional clavicular motion during arm elevation: reliability and descriptive data. J Orthop Sports Phys Ther. 2004;34:140–149. doi: 10.2519/jospt.2004.34.3.140. http://dx.doi.org/10.2519/jospt.2004.1020. [DOI] [PubMed]
- 70.Ludewig PM, Borstad JD. Effects of a home exercise programme on shoulder pain and functional status in construction workers. Occup Environ Med. 2003;60:841–849. doi: 10.1136/oem.60.11.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80:276–291. [PubMed] [Google Scholar]
- 72.Ludewig PM, Hoff MS, Osowski EE, Meschke SA, Rundquist PJ. Relative balance of serratus anterior and upper trapezius muscle activity during push-up exercises. Am J Sports Med. 2004;32:484–493. doi: 10.1177/0363546503258911. [DOI] [PubMed] [Google Scholar]
- 73.Lukasiewicz AC, McClure P, Michener L, Pratt N, Sennett B. Comparison of 3-dimensional scapular position and orientation between subjects with and without shoulder impingement. J Orthop Sports Phys Ther. 1999;29:574–583. doi: 10.2519/jospt.1999.29.10.574. discussion 584-576. [DOI] [PubMed] [Google Scholar]
- 74.Magee DJ. Orthopedic Physical Assessment. 4th ed. Saunders Publishing Company; Philadelphia, PA: 2002. [Google Scholar]
- 75.McClure P, Balaicuis J, Heiland D, Broersma ME, Thorndike CK, Wood A. A randomized controlled comparison of stretching procedures for posterior shoulder tightness. J Orthop Sports Phys Ther. 2007;37:108–114. doi: 10.2519/jospt.2007.2337. http://dx.doi.org/10.2519/jospt.2007.2337. [DOI] [PubMed]
- 76.McClure PW, Bialker J, Neff N, Williams G, Karduna A. Shoulder function and 3-dimensional kinematics in people with shoulder impingement syndrome before and after a 6-week exercise program. Phys Ther. 2004;84:832–848. [PubMed] [Google Scholar]
- 77.McClure PW, Michener LA, Karduna AR. Shoulder function and 3-dimensional scapular kinematics in people with and without shoulder impingement syndrome. Phys Ther. 2006;86:1075–1090. [PubMed] [Google Scholar]
- 78.McClure PW, Michener LA, Sennett BJ, Karduna AR. Direct 3-dimensional measurement of scapular kinematics during dynamic movements in vivo. J Shoulder Elbow Surg. 2001;10:269–277. doi: 10.1067/mse.2001.112954. http://dx.doi.org/10.1067/mse.2001.112954. [DOI] [PubMed]
- 79.McCully SP, Suprak DN, Kosek P, Karduna AR. Suprascapular nerve block disrupts the normal pattern of scapular kinematics. Clin Biomech (Bristol, Avon) 2006;21:545–553. doi: 10.1016/j.clinbiomech.2006.02.001. http://dx.doi.org/10.1016/j.clinbiomech.2006.02.001. [DOI] [PubMed]
- 80.McQuade KJ, Dawson J, Smidt GL. Scapulothoracic muscle fatigue associated with alterations in scapulohumeral rhythm kinematics during maximum resistive shoulder elevation. J Orthop Sports Phys Ther. 1998;28:74–80. doi: 10.2519/jospt.1998.28.2.74. [DOI] [PubMed] [Google Scholar]
- 81.Mehta S, Gimbel JA, Soslowsky LJ. Etiologic and pathogenetic factors for rotator cuff tendinopathy. Clin Sports Med. 2003;22:791–812. doi: 10.1016/s0278-5919(03)00012-7. [DOI] [PubMed] [Google Scholar]
- 82.Mell AG, LaScalza S, Guffey P, et al. Effect of rotator cuff pathology on shoulder rhythm. J Shoulder Elbow Surg. 2005;14:58S–64S. doi: 10.1016/j.jse.2004.09.018. http://dx.doi.org/10.1016/j.jse.2004.09.018. [DOI] [PubMed]
- 83.Michener LA, Boardman ND, Pidcoe PE, Frith AM. Scapular muscle tests in subjects with shoulder pain and functional loss: reliability and construct validity. Phys Ther. 2005;85:1128–1138. [PubMed] [Google Scholar]
- 84.Michener LA, McClure PW, Karduna AR. Anatomical and biomechanical mechanisms of subacromial impingement syndrome. Clin Biomech (Bristol, Avon) 2003;18:369–379. doi: 10.1016/s0268-0033(03)00047-0. [DOI] [PubMed] [Google Scholar]
- 85.Michener LA, Walsworth MK, Burnet EN. Effectiveness of rehabilitation for patients with subacromial impingement syndrome: a systematic review. J Hand Ther. 2004;17:152–164. doi: 10.1197/j.jht.2004.02.004. http://dx.doi.org/10.1197/j.jht.2004.02.004. [DOI] [PubMed]
- 86.Myers JB, Oyama S, Wassinger CA, et al. Reliability, precision, accuracy, and validity of posterior shoulder tightness assessment in overhead athletes. Am J Sports Med. 2007;35:1922–1930. doi: 10.1177/0363546507304142. http://dx.doi.org/10.1177/0363546507304142. [DOI] [PubMed]
- 87.Neer CS., 2nd Impingement lesions. Clin Orthop Relat Res. 1983:70–77. [PubMed] [Google Scholar]
- 88.Norton BJ. Diagnosis dialog: progress report. Phys Ther. 2007;87:1270–1273. doi: 10.2522/ptj.2007.87.10.1270. http://dx.doi.org/10.2522/ptj.2007.87.10.1270. [DOI] [PubMed]
- 89.Norton BJ. Harnessing our collective professional power: diagnosis dialog. Phys Ther. 2007;87:635–638. doi: 10.2522/ptj.2007.87.6.635. http://dx.doi.org/10.2522/ptj.2007.87.6.635. [DOI] [PubMed]
- 90.Ogston JB, Ludewig PM. Differences in 3-dimensional shoulder kinematics between persons with multidirectional instability and asymptomatic controls. Am J Sports Med. 2007;35:1361–1370. doi: 10.1177/0363546507300820. http://dx.doi.org/10.1177/0363546507300820. [DOI] [PubMed]
- 91.Ozaki J. Glenohumeral movements of the involuntary inferior and multidirectional instability. Clin Orthop Relat Res. 1989:107–111. [PubMed] [Google Scholar]
- 92.Paletta GA, Jr., Warner JJ, Warren RF, Deutsch A, Altchek DW. Shoulder kinematics with two-plane x-ray evaluation in patients with anterior instability or rotator cuff tearing. J Shoulder Elbow Surg. 1997;6:516–527. doi: 10.1016/s1058-2746(97)90084-7. [DOI] [PubMed] [Google Scholar]
- 93.Paley KJ, Jobe FW, Pink MM, Kvitne RS, ElAttrache NS. Arthroscopic findings in the overhand throwing athlete: evidence for posterior internal impingement of the rotator cuff. Arthroscopy. 2000;16:35–40. doi: 10.1016/s0749-8063(00)90125-7. [DOI] [PubMed] [Google Scholar]
- 94.Pappas GP, Blemker SS, Beaulieu CF, McAd-ams TR, Whalen ST, Gold GE. In vivo anatomy of the Neer and Hawkins sign positions for shoulder impingement. J Shoulder Elbow Surg. 2006;15:40–49. doi: 10.1016/j.jse.2005.04.007. http://dx.doi.org/10.1016/j.jse.2005.04.007. [DOI] [PubMed]
- 95.Peat M, Grahame RE. Electromyographic analysis of soft tissue lesions affecting shoulder function. Am J Phys Med. 1977;56:223–240. [PubMed] [Google Scholar]
- 96.Plafcan DM, Turczany PJ, Guenin BA, Kegerreis S, Worrell TW. An objective measurement technique for posterior scapular displacement. J Orthop Sports Phys Ther. 1997;25:336–341. doi: 10.2519/jospt.1997.25.5.336. [DOI] [PubMed] [Google Scholar]
- 97.Rabin A, Lrrgang JJ, Fitzgerald GK, Eubanks A. The intertester reliability of the Scapular Assistance Test. J Orthop Sports Phys Ther. 2006;36:653–660. doi: 10.2519/jospt.2006.2234. http://dx.doi.org/10.2519/jospt.2006.2234. [DOI] [PubMed]
- 98.Rees JD, Wilson AM, Wolman RL. Current concepts in the management of tendon disorders. Rheumatology (Oxford) 2006;45:508–521. doi: 10.1093/rheumatology/kel046. http://dx.doi.org/10.1093/rheumatology/kel046. [DOI] [PubMed]
- 99.Rundquist PJ. Alterations in scapular Kinematics in subjects with idiopathic loss of shoulder range of motion. J Orthop Sports Phys Ther. 2007;37:19–25. doi: 10.2519/jospt.2007.2121. http://dx.doi.org/10.2519/jospt.2007.2121. [DOI] [PubMed]
- 100.Scovazzo ML, Browne A, Pink M, Jobe FW, Kerrigan J. The painful shoulder during freestyle swimming. An electromyographic cinematographic analysis of twelve muscles. Am J Sports Med. 1991;19:577–582. doi: 10.1177/036354659101900604. [DOI] [PubMed] [Google Scholar]
- 101.Selkowitz DM, Chaney C, Stuckey SJ, Vlad G. The effects of scapular taping on the surface electromyographic signal amplitude of shoulder girdle muscles during upper extremity elevation in individuals with suspected shoulder impingement syndrome. J Orthop Sports Phys Ther. 2007;37:694–702. doi: 10.2519/jospt.2007.2467. http://dx.doi.org/10.2519/jospt.2007.2467. [DOI] [PubMed]
- 102.Senbursa G, Baltaci G, Atay A. Comparison of conservative treatment with and without manual physical therapy for patients with shoulder impingement syndrome: a prospective, randomized clinical trial. Knee Surg Sports Traumatol Arthrosc. 2007;15:915–921. doi: 10.1007/s00167-007-0288-x. http://dx.doi.org/10.1007/s00167-007-0288-x. [DOI] [PubMed]
- 103.Smith J, Dietrich CT, Kotajarvi BR, Kaufman KR. The effect of scapular protraction on isometric shoulder rotation strength in normal subjects. J Shoulder Elbow Surg. 2006;15:339–343. doi: 10.1016/j.jse.2005.08.023. http://dx.doi.org/10.1016/j.jse.2005.08.023. [DOI] [PubMed]
- 104.Smith J, Kotajarvi BR, Padgett DJ, Eischen JJ. Effect of scapular protraction and retraction on isometric shoulder elevation strength. Arch Phys Med Rehabil. 2002;83:367–370. doi: 10.1053/apmr.2002.29666. [DOI] [PubMed] [Google Scholar]
- 105.Solem-Bertoft E, Thuomas KA, Westerberg CE. The influence of scapular retraction and protraction on the width of the subacromial space. An MRI study. Clin Orthop Relat Res. 1993:99–103. [PubMed] [Google Scholar]
- 106.Soslowsky LJ, Thomopoulos S, Esmail A, et al. Rotator cuff tendinosis in an animal model: role of extrinsic and overuse factors. Ann Biomed Eng. 2002;30:1057–1063. doi: 10.1114/1.1509765. [DOI] [PubMed] [Google Scholar]
- 107.Su KP, Johnson MP, Gracely EJ, Karduna AR. Scapular rotation in swimmers with and without impingement syndrome: practice effects. Med Sci Sports Exerc. 2004;36:1117–1123. doi: 10.1249/01.mss.0000131955.55786.1a. [DOI] [PubMed] [Google Scholar]
- 108.Tate AR, McClure P, Lrwin D, Kareha S, Stuckey E. Validity of a new test for scapular dyskinesia [abstract] J Orthop Sports Phys Ther. 2007;37:A25. [Google Scholar]
- 109.Tate AR, McClure PW, Kareha S, Lrwin D. Effect of the Scapula Reposition Test on shoulder impingement symptoms and elevation strength in overhead athletes. J Orthop Sports Phys Ther. 2008;38:4–11. doi: 10.2519/jospt.2008.2616. http://dx.doi.org/10.2519/jospt.2008.2616. [DOI] [PubMed]
- 110.Teece RM, Lunden JB, Lloyd AS, Kaiser AP, Cieminski CJ, Ludewig PM. Three-dimensional acromioclavicular joint motions during elevation of the arm. J Orthop Sports Phys Ther. 2008;38:181–190. doi: 10.2519/jospt.2008.2386. http://dx.doi.org/10.2519/jospt.2008.2386. [DOI] [PMC free article] [PubMed]
- 111.Teefey SA, Middleton WD, Payne WT, Yamaguchi K. Detection and measurement of rotator cuff tears with sonography: analysis of diagnostic errors. AJR Am J Roentgenol. 2005;184:1768–1773. doi: 10.2214/ajr.184.6.01841768. [DOI] [PubMed] [Google Scholar]
- 112.Teefey SA, Rubin DA, Middleton WD, Hildebolt CF, Leibold RA, Yamaguchi K. Detection and quantification of rotator cuff tears. Comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am. 2004;86-A:708–716. [PubMed] [Google Scholar]
- 113.Tsai NT, McClure PW, Karduna AR. Effects of muscle fatigue on 3-dimensional scapular kinematics. Arch Phys Med Rehabil. 2003;84:1000–1005. doi: 10.1016/s0003-9993(03)00127-8. [DOI] [PubMed] [Google Scholar]
- 114.Tyler TF, Roy T, Nicholas SJ, Gleim GW. Reliability and validity of a new method of measuring posterior shoulder tightness. J Orthop Sports Phys Ther. 1999;29:262–269. doi: 10.2519/jospt.1999.29.5.262. discussion 270-264. [DOI] [PubMed] [Google Scholar]
- 115.van der Helm FC. Analysis of the kinematic and dynamic behavior of the shoulder mechanism. J Biomech. 1994;27:527–550. doi: 10.1016/0021-9290(94)90064-7. [DOI] [PubMed] [Google Scholar]
- 116.van der Helm FC, Pronk GM. Three-dimensional recording and description of motions of the shoulder mechanism. J Biomech Eng. 1995;117:27–40. doi: 10.1115/1.2792267. [DOI] [PubMed] [Google Scholar]
- 117.van der Windt DA, Koes BW, de Jong BA, Bouter LM. Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis. 1995;54:959–964. doi: 10.1136/ard.54.12.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Vermeulen HM, Stokdijk M, Eilers PH, Meskers CG, Rozing PM, Vliet Vlieland TP. Measurement of three dimensional shoulder movement patterns with an electromagnetic tracking device in patients with a frozen shoulder. Ann Rheum Dis. 2002;61:115–120. doi: 10.1136/ard.61.2.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.von Eisenhart-Rothe R, Matsen FA, 3rd, Eckstein F, Vogl T, Graichen H. Pathomechanics in atraumatic shoulder instability: scapular positioning correlates with humeral head centering. Clin Orthop Relat Res. 2005:82–89. [PubMed] [Google Scholar]
- 120.Wadsworth DJ, Bullock-Saxton JE. Recruitment patterns of the scapular rotator muscles in freestyle swimmers with subacromial impingement. Int J Sports Med. 1997;18:618–624. doi: 10.1055/s-2007-972692. [DOI] [PubMed] [Google Scholar]
- 121.Wang CH, McClure P, Pratt NE, Nobilini R. Stretching and strengthening exercises: their effect on three-dimensional scapular kinematics. Arch Phys Med Rehabil. 1999;80:923–929. doi: 10.1016/s0003-9993(99)90084-9. [DOI] [PubMed] [Google Scholar]
- 122.Wang SS, Trudelle-Jackson EJ. Comparison of customized versus standard exercises in rehabilitation of shoulder disorders. Clin Rehabil. 2006;20:675–685. doi: 10.1191/0269215506cre991oa. [DOI] [PubMed] [Google Scholar]
- 123.Warner JJ, Micheli LJ, Arslanian LE, Kennedy J, Kennedy R. Scapulothoracic motion in normal shoulders and shoulders with glenohumeral instability and impingement syndrome. A study using Moire topographic analysis. Clin Orthop Relat Res. 1992:191–199. [PubMed] [Google Scholar]
- 124.Watson L, Balster SM, Finch C, Dalziel R. Measurement of scapula upward rotation: a reliable clinical procedure. Br J Sports Med. 2005;39:599–603. doi: 10.1136/bjsm.2004.013243. http://dx.doi.org/10.1136/bjsm.2004.013243. [DOI] [PMC free article] [PubMed]
- 125.Weiser WM, Lee TQ, McMaster WC, McMahon PJ. Effects of simulated scapular protraction on anterior glenohumeral stability. Am J Sports Med. 1999;27:801–805. doi: 10.1177/03635465990270061901. [DOI] [PubMed] [Google Scholar]
- 126.Wilk KE, Andrews JR, Arrigo CA. The physical examination of the glenohumeral joint: emphasis on the stabilizing structures. J Orthop Sports Phys Ther. 1997;25:380–389. doi: 10.2519/jospt.1997.25.6.380. [DOI] [PubMed] [Google Scholar]
- 127.Wilk KE, Meister K, Andrews JR. Current concepts in the rehabilitation of the overhead throwing athlete. Am J Sports Med. 2002;30:136–151. doi: 10.1177/03635465020300011201. [DOI] [PubMed] [Google Scholar]
- 128.Yamaguchi K, Sher JS, Andersen WK, et al. Glenohumeral motion in patients with rotator cuff tears: a comparison of asymptomatic and symptomatic shoulders. J Shoulder Elbow Surg. 2000;9:6–11. doi: 10.1016/s1058-2746(00)90002-8. [DOI] [PubMed] [Google Scholar]
- 129.Zuckerman JD, Kummer FJ, Cuomo F, Simon J, Rosenblum S, Katz N. The influence of coracoacromial arch anatomy on rotator cuff tears. J Shoulder Elbow Surg. 1992;1:4–14. doi: 10.1016/S1058-2746(09)80010-4. [DOI] [PubMed] [Google Scholar]