Abstract
Length of hospital stay (LOS) following acute myocardial infarction (AMI) has steadily decreased due both to improved treatments and cost considerations. Early discharge may adversely affect some patients who might benefit from extended monitoring. The Minnesota Heart Survey is a population-based study of AMI in acute-care hospitals in the Minneapolis-St. Paul metropolitan area. Medical records were abstracted on a random sample of patients hospitalized with AMI in 1985, 1990, 1995, and 2001. Case fatality rates, adjusted for age and gender, were identified using mortality data from the index hospitalization and Minnesota death certificates. 4940 patients with validated AMI were identified from the combined 1985 (n=1306), 1990 (n=1550), 1995 (n=1087), and 2001 (n=515) surveys. The median LOS were 9, 8, 6, and 4 days, respectively. Patients hospitalized ≤4 days formed an increasing proportion of the population increasing from 11% (1985) to 58%(2001). In-hospital case fatality declined from 1985 to 2001 (11.6% to 5.4%, p<0.0001 for trend). There was a significant decline in both 1 month (3.3% to 2.4%, p=0.002 for trend) and 6-month (8.9% to 5.4%, p<0.0001) post-discharge mortality from 1985 to 2001. In conclusion, the progressive and substantial reduction in hospital LOS following AMI in the past 2 decades has not been associated with increased post-discharge mortality. These reductions in LOS are associated with increasing use of effective therapies.
Keywords: acute myocardial infarction, length of stay, epidemiology
Introduction
While a substantial proportion of patients destined for a fatal acute myocardial infarction (AMI) die within the first several days, additional patients die in the subsequent days to weeks, both in and out of the hospital. Algorithms that stratify patients into various clinical pathways based on the presence or absence of high risk features have been assessed in both observational studies and clinical trials1–6. Although there is no established minimal length of stay (LOS) following an AMI, there is a concern that premature discharge could result in an increase in early post-discharge mortality. Hospital LOS have continued to decline beyond those considered in the aforementioned studies. We hypothesized a declining hospital LOS is associated with a rise in early post-discharge mortality. We utilized data from the Minnesota Heart Survey (MHS), a longitudinal population-based study of patients with AMI in a large metropolitan area, to address this hypothesis.
Methods
A stratified random study sample included resident patients with AMI, age 30 to 74, hospitalized in the Minneapolis-St. Paul metropolitan area in 1985, 1990, 1995, and 2001. The sampling rates for men were 50%, 50%, 40%, and 50% for 1985, 1990, 1995, and 2001. Among female AMI patients, the corresponding proportion of records sampled was 50%, 100%, 80%, and 100%, respectively. The samples were from most or all acute-care hospitals 1985 (30/31), 1990 (25/25), and 1995 (22/23) and spanned the calendar year. The sample labeled from 2001 included medical records of patients from (20/22) hospitals discharged between July 1 and December 31, 2001. Those hospitals excluded were small, accounting for few cases. Potential cases were identified by ICD-9 discharge diagnosis code 410 and an algorithm was utilized to validate the occurrence of AMI.7 The definition of AMI was based on defined combinations of the following: acute onset of chest pain, increased biomarkers, the electrocardiogram, and/or autopsy findings consistent with AMI. Patients transferred into or out of the index hospital were excluded from the analysis because the LOS from the transferring hospital was usually not available.
The MHS is an ongoing hospital surveillance project of hospitalized AMI patients age 30 to 74 residing in the Minneapolis-St. Paul metropolitan area. Details of the project are described in prior publications.7,8 In brief, surveys are conducted approximately every 5 years in acute-care hospitals and the patient sample is based on an ICD-9 discharge diagnosis of AMI. The random selection of patient records is determined by computer and medical records are abstracted by trained nurses. The extensive abstraction process includes demographic detail, cardiac risk factors, past medical history, clinical presentation, relevant laboratory and electrocardiographic data, medications, in-hospital procedures and complications. In-hospital mortality is identified directly through medical record abstraction; post-discharge mortality is supplied by the Minnesota Death Index (MINNDEX), an algorithm for evaluating potential death certificate matches using mortality tapes provided by the state of Minnesota. In a previous study, MINNDEX had 98% agreement with the National Death Index for death certificates.9 All MHS data is de-identified for purposes of analysis to protect patient confidentiality. The MHS project is IRB approved by the University of Minnesota and the participating hospitals.
The outcome measure was all-cause mortality. Hospital LOS was calculated as date of discharge minus date of admission. Hence, a patient admitted on 1 day and discharged on the next day would have a LOS of 1 day. Patients admitted and discharged on the same date were assigned a LOS of 1 day. In-hospital mortality was measured from date of admission. Post-discharge mortality was calculated as the date of death minus the date of discharge for the index AMI hospitalization. For the post-discharge mortality analysis, day 1 was defined as the date of discharge if patient was discharged alive.
Clinical characteristics of the patients over time were weighted for the stratified sampling design to estimate population wide characteristics in each year. The primary analysis was descriptive and detailed the hospital LOS and mortality at given reference points. In-hospital and post-discharge (1 week, 1-month, 6-month) mortality were compared across the survey years. The duration of hospitalization was compared across the survey years using frequency distribution curves. The LOS did not exhibit a normal distribution and were therefore reported with median and inter-quartile ranges. Trends in LOS were assessed with the Wilcoxon ranked sum test. Hospital LOS was divided into 2 groups based on the median: LOS ≤ 4 days and LOS ≥ 5 days. Post-discharge mortality, measured at 1 month and 6 months, was compared between the 2 groups for each time period to determine whether the reduction in hospital LOS over time had a detrimental effect on patient outcomes. There were an insufficient number of deaths to analyze the association of LOS with 1-week post-discharge mortality. An interaction term was employed to determine whether there was an association between length of stay and year of hospitalization on post-discharge mortality. Clinical characteristics were compared over survey years using general linear models. Trends in post-discharge mortality across different hospital durations were tested with Poisson models, adjusting for age, gender, hospital, and cardiovascular morbidity (congestive heart failure, cardiogenic shock, and malignant ventricular arrhythmias). We also analyzed for potential clustering across hospitals. Both the general linear and Poisson models were weighted to account for the stratified sampling design. All data analyses were performed using SAS 9.12 (SAS Institute, Carey, NC).
Results
We identified 4458 patients with an AMI in the Minneapolis-St. Paul metropolitan area from 1985 (n=1306), 1990 (n=1550), 1995 (n=1087), and 2001 (n=515). A comparison of the demographic and clinical characteristics as well as the treatment of the individual sample frames is shown in Table 1. The mean age of patients with AMI was unchanged over time but the proportion of Caucasians and men fell. History of hypertension, percutaneous transluminal coronary angioplasty (PTCA), coronary artery bypass surgery (CABG) and stroke were more common in recent survey years while previous AMI and angina pectoris fell over time. The use of diagnostic and therapeutic procedures during the index hospitalization increased over time, except for CABG. The utilization of other recommended medical therapies similarly increased.
Table 1.
Comparison of Patient Characteristics Between Survey Samples (Weighted for the stratified sampling design to estimate population wide characteristics in each year)
| 1985 (N = 1,306) | 1990 (N = 1,550) | 1995 (N = 1,087) | 2001 (N = 515) | P for trend | |
|---|---|---|---|---|---|
| Demographics | |||||
| Age (mean ± SD, years) | 60.4±13.4 | 60.9±12.2 | 59.7±14.4 | 60.2±12.6 | NS |
| Male* | 72.4% | 71.4 | 70.6 | 66.6 | 0.02 |
| Caucasian | 94.0% | 92.4 | 84.3 | 87.3 | <0.0001 |
| Past Medical History | |||||
| Diabetes | N/A | N/A | 24.5% | 28.1% | NS |
| Hypertension | 52.1% | 51.7% | 55.2% | 58.5% | 0.007 |
| Myocardial Infarction | 31.0% | 31.3% | 26.7% | 24.0% | 0.0008 |
| Angina pectoris | 32.5% | 32.4% | 29.2% | 22.8% | <0.0001 |
| Cardiac arrest | 1.8% | 2.2% | 1.7% | 1.6% | NS |
| Stroke | 5.6% | 7.6% | 7.9% | 8.7% | 0.03 |
| Coronary Angioplasty | N/A | 6.4% | 11.4% | 17.6% | <0.0001 |
| Coronary Bypass | 7.4% | 10.6% | 9.9% | 12.8% | 0.002 |
| Procedures | |||||
| Coronary angiography | 19.7% | 48.7% | 65.5% | 77.3% | <0.0001 |
| Any Coronary | 3.8% | 19.7% | 34.9% | 50.5% | <0.0001 |
| Angioplasty | |||||
| Primary Coronary | NA | NA | 32.0% | 76.9% | <0.0001 |
| Angioplasty* | |||||
| Coronary Angioplasty 24h* | 34.7% | 37.7% | 46.0% | 73.5% | <0.0001 |
| Stent* | NA | NA | 12.9% | 94.1% | <0.0001 |
| Coronary Bypass | 6.4% | 12.9% | 15.0% | 9.1% | 0.06 |
| In-Hospital Medication | |||||
| Aspirin | N/A | 79.1% | 92.6% | 94.6% | <0.0001 |
| Beta blockers | 55.1% | 50.0% | 71.2% | 88.2% | <0.0001 |
| Calcium blockers | 49.7% | 60.3% | 34.7% | 25.3% | <0.0001 |
| High dose heparin | 25.9% | 56.1% | 80.2% | 81.7% | <0.0001 |
| Angiotensin-Converting | N/A | 20.3% | 39.2% | 62.6% | <0.0001 |
| Enzyme inhibitors | |||||
| Thrombolytic therapy | 12.4% | 28.4% | 28.8% | 7.4% | 0.03 |
| Warfarin | 20.1% | 14.4% | 18.8% | 11.4% | 0.0006 |
| Complications | |||||
| Heart Failure | 29.5% | 27.6% | 27.1% | 20.9% | 0.0004 |
The percentages displayed for primary PTCA, PTCA within 24 hours, and stenting were based on the subgroup of patients who underwent any percutaneous coronary intervention.
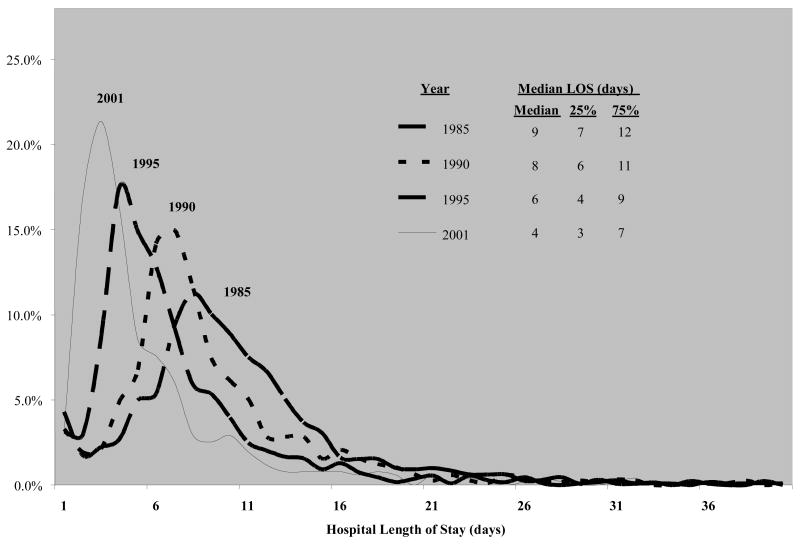
Hospital LOS progressively declined from 1985 to 2001. The median, 25th and 75th percentiles lengths of stay were 9 (7, 12) days, 8 (6, 11) days, 6 (4, 9) days, and 4 (3, 7) days, respectively (Figure 1).
Figure 1.
Hospital Length of Stay Stratified by Sample Year
Mortality following AMI declined over time. Adjusted in-hospital mortality declined from 11.6% in 1985, to 10.1% in 1990, to 9.3% in 1995, to 5.4% in 2001 (p-trend <0.0001) along with diminishing LOS. The mortality, described in terms of the Poisson model (per person week) is illustrated in Table 2. Overall, 1 month mortality (incorporating in-hospital and out-of-hospital mortality) declined from 14.9% in 1985, to 12.8% in 1990 to 10.9% in 1995 to 7.8% in 2001 (p-trend <0.0001). After excluding patients who died during their hospitalization (n = 445), there remained 4013 individuals in whom post-discharge mortality could be assessed. The post-discharge mortality was low across the 3 time frames – 1 week, 1 month and 6 months (Table 2). The trend was downward and significant at one month and six months. There were no trends for 7-day post discharge mortality; it was low, ≈ 1%.
Table 2.
In-Hospital, One-Week, One-Month, and Six-Month Post-Discharge Mortality Following AMI Between Survey Samples (Weighted, Adjusted: age, sex, hospital, CHF, Cardiogenic Shock, Arrhythmias (Asystole, Ventricular Fibrillation, Ventricular Tachycardia))
| 1985 (N = 1,306) | 1990 (N = 1,550) | 1995 (N = 1,087) | 2001 (N = 515) | P for trend | |
|---|---|---|---|---|---|
| In-Hospital Mortality* (95% CI) | 1.8% (.7–4.4) | 1.4% (.6–3.5) | 1.8% (.7–4.6) | 3.6% (1.4–9.2) | <0.0001 |
| Deaths | 149 | 165 | 100 | 30 | |
|
| |||||
| 1985 (N=1,156) | 1990 (N=1,385) | 1995 (N=987) | 2001 (N=485) | P for trend | |
|
| |||||
| Post-Discharge Mortality** | |||||
| One-week (95% CI) | 1.2% (0.7–2.0) | 1.5% (0.9–2.4) | 0.8% (0.4–1.5) | 1.6% (0.7–3.8) | NS |
| Deaths | 12 | 18 | 7 | 6 | |
| One-month (95% CI) | 4.1% (3.0–5.7) | 3.2% (2.3–4.5) | 2.0% (1.3–3.1) | 3.9% (2.2–6.9) | NS |
| Deaths | 38 | 37 | 15 | 13 | |
| Six-month (95% CI) | 9.5% (7.7–11.9) | 6.1% (4.7–7.8) | 4.9% (3.6–6.5) | 7.5% (5.0–11.1) | NS |
| Deaths | 101 | 86 | 41 | 29 | |
In-hospital mortality rates indicate percent deaths per person-week.
Post-discharge mortality rates indicate percent deaths per person-week, per person-month, and per person-6 months, respectively.
The data were median split based on discharge within the first 4 days to characterize shorter and longer hospital stays at 1 months and 6 months (Table 3). Thirty day adjusted mortality was variable but, on average, somewhat lower for patients discharge early (interaction p-value NS). At 6 months, adjusted mortality was higher in those staying ≥ 5 days (interaction p-value NS).
Table 3.
1-Month and 6-Month Post-Discharge Mortality by Length of Stay (LOS) and Sample Year (Weighted, Adjusted: age, sex, hospital, CHF, Cardiogenic Shock, Arrhythmias (Asystole, Ventricular Fibrillation, Ventricular Tachycardia))
| 1985 | 1990 | 1995 | 2001 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LOS | ≤4 (N=52) |
≥5 (N=1104) |
p | ≤4 (N=112) |
≥5 (N=1273) |
p | ≤4 (N=299) |
≥5 (N=688) |
p | ≤4 (N=281) |
≥5 (N=204) |
p | Interaction p-value |
| One-month | 9.0% | 3.9% | 0.05 | 0% | 3.4% | 1.0 | 3.3% | 1.7% | 0.08 | 2.8% | 5.3% | 0.22 | 0.0031 |
| (95% CI) | (3.9–10.0) | (2.1–5.5) | -- | (2.5–4.8) | (1.7–6.4) | (1.0–2.8) | (1.2–6.7) | (2.8–9.9) | |||||
| Deaths | 3 | 35 | 0 | 37 | 4 | 11 | 4 | 9 | |||||
| Six-month | 13.8% | 8.9% | 0.14 | 0.7% | 6.1% | 0.03 | 4.2% | 4.5% | 0.80 | 3.3% | 9.1% | 0.007 | 0.0012 |
| (95% CI) | (7.6–25.3) | (7.0–11.3) | (0.1–5.3) | (4.7–7.9) | (2.5–7.1) | (3.3–6.1) | (1.7–6.4) | (5.9–13.9) | |||||
| Deaths | 6 | 95 | 1 | 85 | 8 | 33 | 7 | 22 | |||||
The demographic and clinical characteristics of patients discharged early (≤ 4 days compared to those discharged later (≥ 5 days) are depicted in Table 4. Those who were hospitalized for a longer time were more likely to receive medical and invasive therapies in the early surveys. For the later surveys (1995 and 2001), a different picture emerges. Early discharge becomes more common, accounting for over 50% of AMI in 2001. The early discharge patients were younger and somewhat more likely to be men. They were less likely to have diabetes, hypertension, prior stroke, prior AMI or prior CABG but were more likely to have had prior PTCA. Patients discharged early were more likely to undergo primary PTCA during their hospitalization. In contrast, patients discharged later were more likely to undergo CABG.
Table 4.
Comparison of Patient Characteristics by Length of Stay (LOS) and Sample Year (Weighted for the stratified sampling design to estimate population wide characteristics in each year)
| Survey Sample Length of Stay | 1985 | 1990 | 1995 | 2001 | ||||
|---|---|---|---|---|---|---|---|---|
| ≤ 4 days (N=144) | ≥ 5 days (N=1,162) | ≤ 4 days (N=190) | ≥ 5 days (N=1,360) | ≤ 4 days (N=350) | ≥ 5 days (N=737) | ≤ 4 days (N=297) | ≥ 5 days (N=218) | |
| Demographics | ||||||||
| Age (mean ± SD, yrs) | 61.0±15.0 | 60.3±13.5 | 59.6±13.8 | 61.0±11.9 | 57.8±14.7 | 60.6±14.1* | 58.4±13.3 | 62.9±10.8* |
| Male | 68.1% | 73.0% | 74.1% | 71.0% | 73.0% | 69.4% | 72.0% | 58.4%* |
| Caucasian | 93.8% | 94.0% | 89.7% | 92.7% | 81.9% | 85.6%* | 88.4% | 85.7% |
| Past medical History | ||||||||
| Diabetes | NA | NA | NA | NA | 15.8% | 28.7%* | 22.2% | 37.0%* |
| Hypertension | 51.4% | 52.2% | 50.3% | 51.9% | 51.2% | 57.1% | 56.9% | 61.0% |
| Myocardial Infarction | 39.6% | 29.9%* | 36.1% | 30.6% | 25.4% | 27.4% | 21.8% | 27.3% |
| Angina pectoris | 30.6% | 32.8% | 34.4% | 32.1% | 31.9% | 27.8% | 24.1% | 20.8% |
| Cardiac arrest | 1.4% | 1.9% | 3.3% | 2.0% | 1.3% | 1.9% | 1.3% | 1.9% |
| Stroke | 6.9% | 5.4% | 4.3% | 8.1% | 7.0% | 8.2% | 6.9% | 11.4% |
| Coronary Angioplasty | NA | NA | 7.0% | 6.3% | 12.2% | 11.0% | 16.6% | 19.2% |
| Coronary Bypass | 12.5% | 6.8%* | 10.9% | 10.6% | 9.8% | 10.0% | 13.4% | 12.0% |
| Procedures | ||||||||
| Coronary angiography | 5.6% | 21.4%* | 33.4% | 50.8%* | 55.9% | 70.2%* | 84.0% | 67.2%* |
| Any Coronary | 0.7% | 4.1% | 17.2% | 20.1% | 34.1% | 35.3% | 62.9% | 31.2%* |
| Angioplasty** | (1) | (48) | (30) | (258) | (114) | (264) | (181) | (68) |
| Primary Coronary | NA | NA | NA | NA | 44.1% | 26.3%* | 76.6% | 77.6% |
| Angioplasty** | ||||||||
| Coronary Angioplasty in 24 hrs** | 100.0% | 33.3% | 76.9% | 32.9%* | 69.7% | 34.8%* | 80.4% | 53.1%* |
| Stent** | NA | NA | NA | NA | 6.9% | 15.8%* | 95.9% | 88.8% |
| Coronary Bypass | 1.4% | 7.0%* | 5.6% | 14.0%* | 2.5% | 21.1%* | 0.9% | 21.4%* |
| In-hospital Medication (%) | ||||||||
| Aspirin | NA | NA | 63.9% | 81.3%* | 89.7% | 94.1%* | 95.9% | 92.5% |
| Beta blockers | 31.9% | 58.0%* | 35.1% | 52.2%* | 66.6% | 73.4%* | 89.0% | 87.0% |
| Calcium Blockers | 35.4% | 51.5%* | 50.0% | 61.8%* | 29.4% | 37.3%* | 19.6% | 33.8%* |
| High dose Heparin | 13.9% | 27.4%* | 43.4% | 57.9%* | 77.5% | 81.6% | 86.0% | 75.3%* |
| Angiotensin-Converting | NA | NA | 9.9% | 21.8%* | 23.0% | 47.0%* | 64.9% | 59.1% |
| Enzyme inhibitors | ||||||||
| Thrombolytic therapy | 9.0% | 12.8% | 17.5% | 29.9%* | 26.0% | 30.1% | 10.3% | 2.9% |
| Warfarin | 4.2% | 22.0%* | 6.6% | 15.6%* | 8.0% | 24.0%* | 6.0% | 19.5%* |
| Complications | ||||||||
| Heart Failure | 42.4% | 27.9%* | 26.5% | 27.8% | 15.4% | 32.9%* | 11.2% | 35.4%* |
| Mortality | ||||||||
| 7 day Post-Discharge | 1.9% | 1.0% | 0.0% | 1.5% | 1.3% | 0.5% | 0.7% | 1.8% |
| one month Post-Discharge | 5.8% | 3.1% | 0.0% | 2.9% | 1.7% | 1.4% | 1.4% | 3.9% |
| 180 day Post-Discharge | 11.5% | 8.6% | 0.5% | 6.3%* | 2.7% | 4.6% | 2.3% | 9.5%* |
p < 0.05 (within sample survey)
Data shown in parentheses represent actual number of patients who underwent percutaneous coronary intervention. The percentages displayed for primary PTCA, PTCA within 24 hours, and stenting were based on the subgroup of patients who underwent any percutaneous coronary intervention.
Discussion
The MHS provided a unique opportunity to examine population trends in AMI mortality and hospital care. We observed a steady decline in hospital LOS from 1985 to 2001. During this 17-year interval, there was also a decrease in 1 month post-discharge mortality.
The safety and feasibility of early discharge following an AMI has been a focus of debate spurred by increasing economic pressures within the healthcare system. Hospital LOS has steadily declined over the past half century. In the 1960s it was routine to hospitalize patients with AMI for several weeks. Decreasing LOS has paralleled a transition from passive care (bed rest, telemetry, and antiplatelet therapy) to active contemporary care (pharmacologic and mechanical reperfusion therapy, the development and utilization of combined pharmacologic agents, and rehabilitation). Ironically, decreasing hospital LOS has been associated with increasing hospital cost. The total average charge for treating a heart attack patient rose from $20,578 in 1993 to $28,663 in 2000, while the average hospital LOS fell by 26%—from 7.4 days to 5.5 days.10 These findings raised concerns that reduced hospital LOS may be compromising patient care leading to poor outcomes.
The complex interaction of factors involved in determining hospital LOS has been illustrated by several studies.11,12 Severity of patient illness, physician practice styles, patient preferences, and financial constraints imposed by hospitals and insurance carriers all play roles. In an analysis of patients undergoing CABG in the Cooperative Cardiovascular Project, Rosen observed significant variability in LOS between institutions after adjusting for both preoperative clinical characteristics and postoperative complications.12 McCormick observed similar variability among 1188 patients admitted to community hospitals with pneumonia.11 Interestingly, patients with a shorter LOS did not have any worse outcome than those with a longer hospital stay. These data support the notion that hospital LOS is driven to some extent by non-clinical factors and that there was room for improved efficiency.
Investigators have attempted to identify patients at low risk of subsequent morbidity and mortality. In the GUSTO trial, Newby defined an “uncomplicated” myocardial infarction as the absence of death, re-infarction, ischemia, stroke, shock, heart failure, bypass surgery, balloon pumping, emergency catheterization or cardioversion/defibrillation during the first 4 hospital days.7 The 30-day mortality in this group was 1% and the rates of re-infarction (1.7%), recurrent ischemia (6.7%), and stroke (0.2%) were quite low.
Several studies have prospectively evaluated hospital LOS following AMI.2–5 Grines, in the PAMI-II trial (1993–1995), randomized 462 low-risk AMI patients (age ≤ 70, left ventricular ejection fraction > 45%, 1 or 2 vessel disease, successful coronary intervention, and no persistent arrhythmias) treated with primary coronary intervention to either discharge on day 3 or to traditional care.2 At 6 months, the accelerated and traditional care groups had similar rates of mortality, unstable ischemia, re-infarction, and stroke. Van der Vlugt, in the SHORT trial (1993–1995), developed a decision rule for identifying low risk AMI patients (absence of ventricular fibrillation, heart failure, recurrent infarction, and advanced AV block during the first 3 days and absence of angina and symptomatic arrhythmias between days 3 and 7) who could be discharged on day 7.3 Among the 43% of the patients who qualified for early discharge, none died within 1 month of discharge and the readmission rate for recurrent myocardial infarction and heart failure was 1.8%. Senaratne evaluated the feasibility of discharging patients directly from the coronary care unit.4 The mean length of hospitalization of 5 days with an in-hospital mortality of 5.8%, and a 6-week post discharge mortality of 2.7%; only 2 deaths occurred within 48 hours of discharge. Most recently, Bogaty et al. randomized 120 low-risk AMI patients to a discharge on day 3 versus a standard stay. Short-stay patients had 25% fewer cardiovascular procedures with similar adverse event and rehospitalization rates at 6 months.5
Our findings in a population-based sample are consistent with the results of these clinical trials, although the mean LOS was slightly longer in this community than in the clinical trials. Our data reflect the natural course of an unselected population of patients with AMI and a diversity of care protocols in community hospitals. In contrast to selected patients enrolled in clinical trials and prospective studies, the patients in the MHS would be expected to have increased morbidity and mortality. Our observations are further supported by recently published data from the Worcester Heart Attack Study.6 Spencer et al. analyzed 4551 AMI discharges from 1986 to 1999 and found no increase in post-discharge mortality among patients with a hospital LOS less than 6 days. In contrast, 30-day and 90-day mortality was increased among patients hospitalized longer than 2 weeks.
The trend toward reduced 30-day post discharge mortality between 1985 and 2001 contrasts with our expectations given the observed reduction in LOS, leading us to reject our initial hypothesis. One explanation may stem from the increased utilization of more sensitive cardiac serum biomarkers in recent years. Patients with limited myocardial injury can now be readily identified and this group of patients may have a better prognosis than those patients with larger myocardial infarctions. A second explanation may rest within better risk stratification and treatment of patients with myocardial infarction. Technologic advances now permit early diagnosis of AMI and allow for more rapid triage of patients. Advances in medical therapy combined with the early use of coronary angiography and revascularization now ensure improved survival to a group of patients traditionally viewed as high risk. This more “streamlined” process is clearly more efficient and presumably leads to earlier discharge while avoiding increased patient risk. There also remains the possibility that the reduced LOS has been primarily driven by hospital policy and insurance carriers.
There were several limitations to our study. First, the overall post-discharge mortality was quite low for all 4 sample frames and was inadequate to permit additional modeling of hospital LOS. However, this low mortality is echoed by other AMI studies, both prospective clinical trials and retrospective observational analyses. Second, the reported mortality rates may be an underestimate of the true mortality since out-of-state mortality was not identified. For this reason, the analysis was restricted to in-state residents. We would not expect a significant relocation of Minnesota residents within a month or even 6 months of a heart attack. Third, HIPAA regulations necessitated the use of a third-party to perform the mortality follow up and prohibited us from analyzing other outcomes such as readmissions for reinfarction and heart failure. Finally, it is possible that the data derived from the MHS project may not reflect national practice and mortality trends. The fact that the MHS incorporates data from all hospitals in the Minneapolis-St. Paul metropolitan area and the similar trend between the MHS and national mortality rates following AMI would argue to the contrary.
Acknowledgments
Supported in part by NIH grant (R01-HL65755), Bethesda, MD: Minnesota Heart Survey–Community Surveillance of Coronary Heart Disease and Sudden Death and NIH grant (1K08-HL083611-02), Bethesda, MD: Treatment of Acute Myocardial Infarction in the Elderly
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Newby L, Califf R, Guerci A, Weaver W, Col J, Horgan J, Mark D, Stebbins A, Van de Werf F, Gore J, Topol E for the GUSTO Investigators. Early discharge in the thrombolytic era: ana analysis of criteria for uncomplicated infarction from the global utilization of streptokinase and t-PA for occluded coronary arteries (GUSTO) trial. J Am Coll Cardiol. 1996;27:625–632. doi: 10.1016/0735-1097(95)00513-7. [DOI] [PubMed] [Google Scholar]
- 2.Grines C, Marsalese D, Brodie B, Griffin J, Donohue B, Costantini C, Balestrini C, Stone G, Wharton T, Esente P, Spain M, Moses J, Nobuyoshi M, Ayres M, Jones D, Mason D, Sachs D, Grines L, O’Neill W for the PAMI-II Investigators. Safety and cost effectiveness of early discharge after primary angioplasty in low risk patients with acute myocardial infarction. J Am Coll Cardiol. 1998;41:967–972. doi: 10.1016/s0735-1097(98)00031-x. [DOI] [PubMed] [Google Scholar]
- 3.van der Vlugt M, Boersma H, Leenders C, Pop G, Veerhoek M, Simoons M, Deckers J. Prospective study of early discharge after acute myocardial infarction (SHORT) Eur Heart J. 2000;21:992–999. doi: 10.1053/euhj.1999.1943. [DOI] [PubMed] [Google Scholar]
- 4.Senaratne M, Irwin M, Shaben S, Griffiths J, Nagendran J, Kasza L, Gulamhusein S, Haughian M. Feasibility of direct discharge from the coronary/intermediate care unit after acute myocardial infarction. J Am Coll Cardiol. 1999;33:1040–1046. doi: 10.1016/s0735-1097(98)00682-2. [DOI] [PubMed] [Google Scholar]
- 5.Bogaty P, Dumont S, O’Hara G, Boyer L, Auclair L, Jobin J, Boudreault J. Randomized trial of a noninvasive strategy to reduce hospital stay for patients with low-risk myocardial infarction. J Am Coll Cardiol. 2001;37:1289–1296. doi: 10.1016/s0735-1097(01)01131-7. [DOI] [PubMed] [Google Scholar]
- 6.Spencer FA, Lessard D, Gore JM, Yarzebski J, Goldberg RJ. Declining length of hospital stay for acute myocardial infarction and postdischarge outcomes: a community-wide perspective. Arch Intern Med. 2004;164:733–740. doi: 10.1001/archinte.164.7.733. [DOI] [PubMed] [Google Scholar]
- 7.McGovern PG, Jacobs DR, Jr, Shahar E, Arnett DK, Folsom AR, Blackburn H, Luepker RV. Trends in acute coronary heart disease mortality, morbidity, and medical care from 1985 through 1997: the Minnesota heart survey. Circulation. 2001;104:19–24. doi: 10.1161/01.cir.104.1.19. [DOI] [PubMed] [Google Scholar]
- 8.McGovern PG, Pankow JS, Shahar E, Doliszny KM, Folsom AR, Blackburn H, Luepker RV. Recent trends in acute coronary heart disease--mortality, morbidity, medical care, and risk factors. The Minnesota Heart Survey Investigators. N Engl J Med. 1996;334:884–890. doi: 10.1056/NEJM199604043341403. [DOI] [PubMed] [Google Scholar]
- 9.Edlavitch SA, Baxter J. Comparability of mortality follow-up before and after the National Death Index. Am J Epidemiol. 1988;127:1164–1178. doi: 10.1093/oxfordjournals.aje.a114910. [DOI] [PubMed] [Google Scholar]
- 10.Agency for Healthcare Research and Quality. Press Release. AHRQ Data Show Rising Hospital Charges, Falling Hospital Stays., September 18, 2002.
- 11.McCormick D, Fine MJ, Coley CM, Marrie TJ, Lave JR, Obrosky DS, Kapoor WN, Singer DH. Variation in hospital length of stay in patients with community-acquired pneumonia: are shorter stays associated with worse outcomes? Am J Med. 1999;107:5–12. doi: 10.1016/s0002-9343(99)00158-8. [DOI] [PubMed] [Google Scholar]
- 12.Rosen AB, Humphries JON, Muhlbaier LH, Kiefe CI, Kresowik T, Peterson E. Effect of clinical factors on length of stay after coronary artery bypass surgery: results of the Cooperative Cardiovascular Project. Am Heart J. 1999;138:69–77. doi: 10.1016/s0002-8703(99)70249-8. [DOI] [PubMed] [Google Scholar]