Abstract
To determine the distribution and antimicrobial drug resistance in bacterial pathogens causing nosocomial infections, surveillance data on nosocomial infections documented from 1981 to 1999 at National Taiwan University Hospital were analyzed. During this period, 35,580 bacterial pathogens causing nosocomial infections were identified. Candida species increased considerably, ranking first by 1999 in the incidence of pathogens causing all nosocomial infections, followed by Staphylococcus aureus and Pseudomonas aeruginosa. Candida species also increased in importance as bloodstream infection isolates, from 1.0% in 1981-1986 to 16.2% in 1999. The most frequent isolates from urinary tract infections were Candida species (23.6%), followed by Escherichia coli (18.6%) and P. aeruginosa (11.0%). P. aeruginosa remained the most frequent isolates for respiratory tract and surgical site infections in the past 13 years. A remarkable increase in incidence was found in methicillin-resistant S. aureus (from 4.3% in 1981-1986 to 58.9% in 1993-1998), cefotaxime-resistant E. coli (from 0% in 1981-1986 to 6.1% in 1993-1998), and cefotaxime-resistant Klebsiella pneumoniae (from 4.0% in 1981-1986 to 25.8% in 1993-1998). Etiologic shifts in nosocomial infections and an upsurge of antimicrobial resistance among these pathogens, particularly those isolated from intensive care units, are impressive and alarming.
Key words: nosocomial infections, antimicrobial resistance, Taiwan, bacterial pathogens, hospital-based surveillance
The emergence of resistance to antimicrobial agents is a global public health problem, particularly in pathogens causing nosocomial infections 1–5. Antimicrobial resistance results in increased illness, deaths, and health-care costs 1,2,6–10. The distribution of pathogens causing nosocomial infections, especially antimicrobial-resistant pathogens, changes with time and varies among hospitals and among different locations in the same hospital 11–15. The increasing number of immunocompromised patients and increased use of indwelling devices, as well as widespread use of antimicrobial agents in hospital settings, particularly in intensive care units (ICUs), contributes to antimicrobial resistance among pathogens causing nosocomial infections 1,4,6,10.
Surveillance data reported by the National Nosocomial Infections Surveillance (NNIS) System for 1993-1997 compared with January-November 1998 show a continuing increase in antimicrobial-resistant pathogens associated with nosocomial infections in ICU patients from U.S. hospitals 2. The increase is particularly marked for vancomycin-resistant enterococci (VRE) (55%), methicillin-resistant Staphylococcus aureus (MRSA) (31%), third-generation cephalosporin-resistant Escherichia coli (29%), imipenem-resistant Pseudomonas aeruginosa (32%), and quinolone-resistant P. aeruginosa (89%) 2. Studies since 1990 have clearly demonstrated that Candida species continue to be an important cause of nosocomial infections, particularly of bloodstream infections (BSI). Furthermore, the proportion of BSI caused by Candida species other than C. albicans is increasing 14,16–20.
We describe the distribution of major bacterial pathogens causing nosocomial infections from 1981 to 1999 in National Taiwan University Hospital and demonstrate the emergence of antimicrobial drug resistance among these pathogens during this period.
Materials and Methods
Data Collection
National Taiwan University Hospital is a 2,000-bed tertiary referral center in Taipei, northern Taiwan. Available data for inpatient-days at the hospital ranged from 294,946 in 1990 to 566,165 in 1999. The number of ICU beds increased from 40-50 before 1993 to 100-120 in 1998-99. The Nosocomial Infection Control Committee of the hospital was established in 1980 to identify pathogens causing nosocomial infections and to obtain and analyze antimicrobial susceptibility results of these pathogens from the hospital’s clinical microbiology laboratory. NNIS definitions were used for nosocomial infections (e.g., bloodstream; respiratory tract, including lower respiratory tract and pneumonia; urinary tract; and surgical site infections) 21,22. Isolates were considered nosocomial if the culture was dated >2 days after admission. All isolates were identified by standard methods and confirmed by using Vitek or API products (bioMerieux Vitek, Inc., Hazelwood, MO). For determining the percentage of resistance, the same organisms from multiple blood cultures or from the same sources with identical antibiotype were considered a single isolate. The amount of use for each indicated antimicrobial agent (including oral and parenteral forms) was expressed in grams per 1,000 inpatient-days.
Antimicrobial Susceptibility Testing
Antimicrobial susceptibility testing of the bacterial isolates was performed by the disk diffusion method as described by the National Committee for Clinical Laboratory Standards (NCCLS) 23. S. aureus ATCC 25923, E. coli ATCC 25922, and P. aeruginosa ATCC 27853 were included as control strains. Interpretive criteria for susceptibility or resistance followed NCCLS guidelines 23. For this report, we present susceptibility data for penicillin, oxacillin, vancomycin, gentamicin, cefotaxime, ceftazidime, imipenem, and ciprofloxacin. The susceptibility data for imipenem and ciprofloxacin were available only since 1993; those for other agents were available from 1981 to 1999.
Antifungal susceptibility testing of amphotericin B and fluconazole against 150 blood isolates of Candida species collected from October 1997 to September 1999 was performed by the E test (AB BIODISK, Solna, Sweden) according to the manufacturer’s instructions. Quality control was performed by testing C. parapsilosis ATCC 2019 and C. krusei ATCC 6258. MIC results were interpreted in accordance with NCCLS guidelines (24).
Results
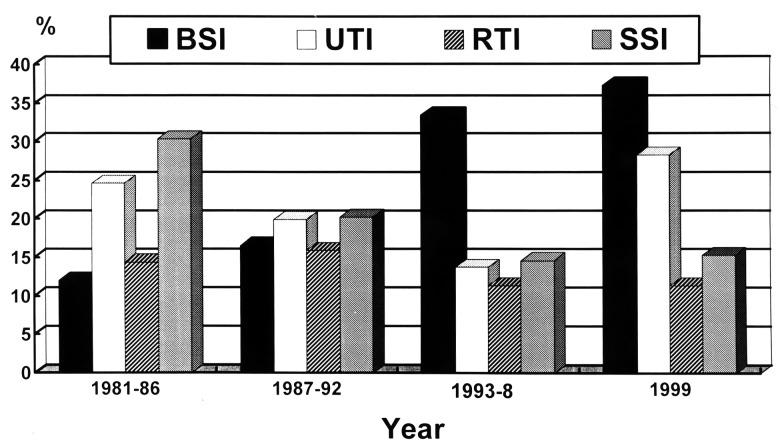
During the 19-year period, 35,580 bacterial pathogens causing nosocomial infections were identified. The hospital’s overall rate of nosocomial infections during the 19-year period ranged from 3.9% to 6.1%. For the four major sites of nosocomial infections, data are presented as numbers of infection per 10,000 patient-days from 1991 to 1999 (Figure 1). BSI ranked first in nosocomial infection sites in 1999, followed by urinary tract, surgical site, and respiratory tract infections.
Figure 1.
Rates of four major nosocomial infections expressed as number of infections per 10,000 patient-days at National Taiwan University Hospital from 1991 to 1999. BSI, bloodstream infection; UTI, urinary tract infection; SSI, surgical site infection; RTI, respiratory tract infection.
Data for the catheter- and ventilator-days of the hospitalized patients were not available. However, the mean percentages of patients who stayed in ICUs (six medical ICUs and six surgical ICUs) and used urinary catheters, arterial and central venous catheters, and ventilators were 75.0%, 77.9%, 63.2%, respectively, in 1996 and 79.4%, 81.4%, and 65.2%, respectively, in 1999. The incidence (number of infections/patient-days x 1,000) of urinary catheter-related urinary tract infection, vascular catheter-associated BSI, and ventilator-associated pneumonia in the ICUs was 4.4, 5.6, and 2.7, respectively, in 1996 and 6.0, 7.1, and 3.4, respectively, in 1999.
Gram-negative bacteria remained the predominant pathogens (66.1% in 1981, 51.3% in 1993, and 53.4% in 1999); however, incidences of fungal infections have increased recently (Table 1). In a comparison of data grouped into four time periods (1981-1986, 1987-1992, 1993-1998, and 1999), E. coli decreased from 12.1% of all nosocomial infections in 1981-1986 to 9.5% in 1993-1998; however, infections caused by S. aureus increased from 5.2% (1981-1986) to 12.1% (1993-1998). Candida species showed a considerable increase (from 3.7% in 1981-1986 to 16.2% in 1999) and have ranked first since 1993, followed by S. aureus and P. aeruginosa (Table 1).
Table 1. Incidences of 10 top-ranking pathogens causing nosocomial infections and infections from four body sites at National Taiwan University Hospital, 1981 to 1999.
| Pathogen | % of indicated pathogen causing nosocomial infection (1981-1986/1987-1992/1993-1998/1999)a |
||||
|---|---|---|---|---|---|
| All | BSI | RTI | UTI | SSI | |
|
Candida spp. |
3.7/9.1/14.4/16.2 |
1.0/9.2/16.4/16.2 |
2.0/5.8/2.1/2.2 |
8.4/16.0/23.6/14.3 |
2.4/5.1/5.9/6.4 |
|
Staphylococcus aureus
|
5.2/9.1/12.1/12.0 |
5.2/9.3/11.5/13.0 |
4.0/8.4/16.9/12.6 |
1.4/2.6/3.3/2.1 |
5.5/5.2/13.0/15.4 |
|
Pseudomonas aeruginosa
|
12.7/14.0/11.1/11.8 |
10.0/9.4/7.2/7.8 |
19.6/21.9/23.8/25.7 |
11.7/11.2/11.0/10.4 |
11.1/17.4/14.3/16.0 |
|
Escherichia coli
|
12.1/8.4/9.5/9.9 |
18.7/9.7/8.7/9.0 |
4.8/2.4/3.5/3.7 |
19.1/19.9/18.6/18.4 |
11.7/5.8/5.8/6.8 |
|
Klebsiella pneumoniae
|
8.1/5.5/7.2/6.8 |
11.6/6.6/7.7/7.0 |
10.9/9.4/11.5/10.8 |
9.0/7.0/8.6/8.2 |
6.9/3.5/4.2/4.6 |
|
Enterobacter spp. |
6.0/7.6/7.4/6.4 |
8.0/8.6/7.3/6.9 |
5.2/8.1/11.8/8.6 |
9.0/8.4/6.7/6.3 |
4.5/7.9/7.8/5.5 |
|
Enterococcus spp. |
8.8/7.8/6.7/6.2 |
8.7/6.2/6.3/7.6 |
|
11.6/9.7/8.1/6.5 |
10.1/12.6/9.6/7.9 |
|
Acinetobacter spp. |
4.4/5.1/4.9/5.4 |
6.1/8.8/7.2/7.6 |
11.0/13.4/9.3/13.0 |
|
|
| CoNS |
2.8/6.9/6.6/5.1 |
2.7/8.5/7.9/4.9 |
|
|
3.2/7.1/9.1/6.8 |
| Other NFGNB |
5.7/6.1/4.8/4.1 |
5.9/7.7/6.8/6.7 |
12.3/13.1/7.8/8.2 |
7.4/6.5/4.4/2.8 |
|
|
S. marcescens
|
|
|
3.5/1.9/3.7/4.1 |
|
|
|
Proteus spp. |
|
|
3.2/2.2/2.4/1.1 |
3.8/3.8/3.8/3.7 |
|
|
Citrobacter spp. |
|
|
|
5.9/4.4/2.4/2.4 |
|
|
Viribans streptococci
|
|
|
|
|
5.2/5.8/4.2/3.5 |
| Bacteroides spp. | 9.7/4.7/5.0/3.1 | ||||
aAbbreviations: BSI = bloodstream infection; RTI = respiratory tract infection; UTI = urinary tract infection; SSI = surgical site infection; CoNS = coagulase-negative staphylococci; NFGNB = nonfermentative gram-negative bacilli.
Candida species, S. aureus, and Acinetobacter species were also important bloodstream isolates (Table 1), increasing from 1.0%, 5.2%, and 6.1%, respectively, in 1981-1986 to 16.2%, 13.0%, and 7.6%, respectively, in 1999. Although E. coli was also a frequent isolate, it declined in percentage of all BSI from 18.7% in 1981-1986 to 9.0% in 1999. Other pathogens declining in percentage of BSI from 1981-1986 to 1999 included K. pneumoniae, P. aeruginosa, and Enterococcus species.
From 1992 to 1999, 1,065 isolates of Candida species were recovered from patients with nosocomial BSIs. C. glabrata (8.8%) ranked fourth in incidence behind C. albicans (59.3%), C. tropicalis (17.6%), and C. parapsilosis (8.2%) in 1999. Only four blood isolates of C. krusei were identified during the 8-year period.
The most frequent isolates from urinary tract infections in 1993-1998 were Candida species (23.6%), followed by E. coli (18.6%) and P. aeruginosa (11.0%). However, in 1999, E. coli (18.4%) replaced Candida species (14.3%) as the top-ranking pathogen causing urinary tract infections. P. aeruginosa remained the most frequent isolate for respiratory tract and surgical site infections in the past 13 years. Candida species increased in incidence in surgical site infections, from 1.8% in 1981-1986 to 6.4% in 1999. Among pathogens causing respiratory tract infections, Acinetobacter species ranked fifth in 1993-1998 (9.3%) but second in 1999 (13.0%); Candida species accounted for only 2.2% in 1999.
The distributions of selected antimicrobial drug-resistant pathogens causing all nosocomial infections and BSIs of patients hospitalized in intensive care units or general wards is shown in Table 2. Antimicrobial drug-resistant pathogens causing BSIs that increased markedly over the study period were methicillin-resistant S. aureus (4.3% in 1981-1986, 58.9% in 1993-1998, and 69.2% in 1999), cefotaxime-resistant E. coli (0% in 1981-1986, 6.1% in 1993-1998, and 12.5% in 1999), and cefotaxime-resistant Klebsiella pneumoniae (4.0% in 1981-1986, and 25.8% in 1993-1998). The frequencies of these three resistant pathogens were considerably higher in isolates from ICUs than those from general wards (84.6% vs. 48.3% for MRSA, 17.1% vs. 5.1% for cefotaxime-resistant E. coli, and 51.1% vs. 18.3% for cefotaxime-resistant K. pneumoniae in 1993-1998). The incidence of methicillin-resistant coagulase-negative staphylococci (MRCoNS) remained high (72%-90%) during the 19-year period.
Table 2. Selected antimicrobial resistant pathogens associated with nosocomial infection at National Taiwan University Hospital from 1981 to 1999.
| Resistant pathogen | % resistance (all patients/in intensive care unit patients/in patients in general wards) | |||
|---|---|---|---|---|
| 1981-1986 | 1987-1992 | 1993-1998 | 1999 | |
| Methicillin-resistant Staphylococcus aureus | 20.2/27.8/19.5 | 31.4/58.5/26.6 | 64.8/86.9/56.7 | 69.3/87.4/60.2 |
| Methicillin-resistant CoNSa | 72.2/88.2/70.8 | 74.0/83.9/71.5 | 79.0/88.7/75.1 | 90.6/90.9/90.5 |
| Penicillin-resistant enterococci | 5.9/6.8/5.8 | 20.7/30/19.6 | 19.5/22.6/18.7 | 35.9/40.9/27.8 |
| Gentamicin-resistant enterococci | 0.0/0.0/0.0 | 71.0/71.4/70.9 | 61.5/67.2/60.0 | 50.0/39.3/55.2 |
| Cefotaxime-resistant Escherichia coli | 1.6/0.0/1.7 | 2.8/8.6/2.5 | 6.8/13.1/6.2 | 12.3/10.3/12.7 |
| Cefotaxime-resistant Klebsiella pneumoniae | 4.9/8.8/3.9 | 7.4/16.9/5.6 | 22.8/50.5/15.6 | 16.5/40.0/9.3 |
| Cefotaxime-resistant Enterobacter spp. | 35.8/52.4/32.4 | 49.7/55.7/47.7 | 57.6/67.0/53.6 | 50.9/61.8/46.2 |
| Cefotaxime-resistant Pseudomonas aeruginosa | 24.2/20.0/25.0 | 16.1/24.3/12.1 | 10.2/16.9/7.8 | 11.2/17.6/8.1 |
| Imipenem-resistant P. aeruginosa | NA | NA | 8.5/18.2/4.9 | 6.7/4.5/7.7 |
| Ciprofloxacin-resistant P. aeruginosa | NA | NA | 8.7/11.6/5.8 | 14.0/18.2/2.9 |
| Imipenem-resistant Acinetobacter baumannii | NA | NA | 6.7/9.1/4.4 | 12.5/23.3/7.6 |
aCoNS = coagulase-negative staphylococci; NA = not available.
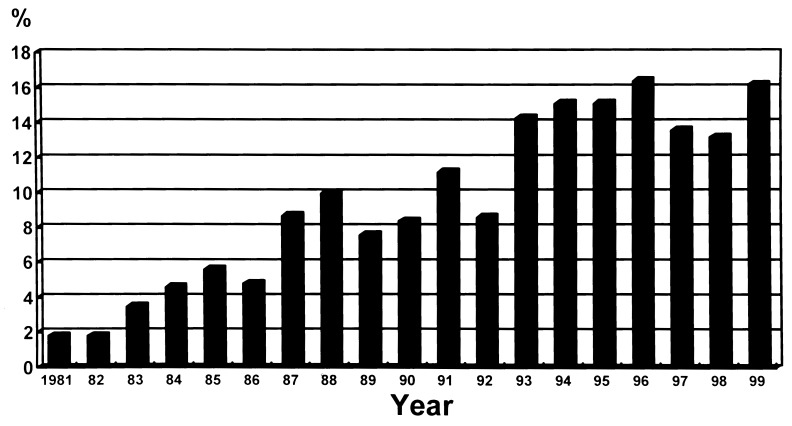
Ceftazidime use is associated with trends of several antimicrobial-resistant pathogens during the period 1991 to 1999 (Figure 2). Restriction of third-generation cephalosporins (particularly ceftazidime) was implemented in 1997. In 1999, resistance to cefotaxime in K. pneumoniae diminished; however, resistance to cefotaxime in E. coli and resistance to ceftazidime in P. aeruginosa slightly increased.
Figure 2.
Changes in major antimicrobial-resistant nosocomial pathogens in relation to ceftazidime use at National Taiwan University Hospital from 1991 to 1999.
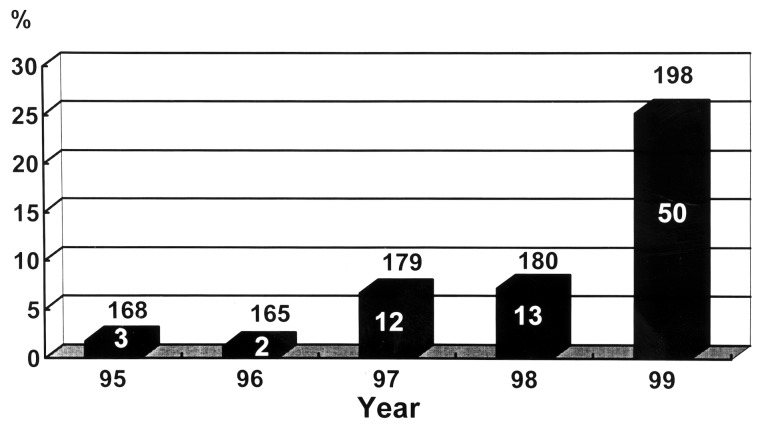
The first clinical isolate of VRE was recognized in 1995 25,26. Since then, 80 isolates of VRE (49 of E. faecalis and 31 of E. faecium) have been recovered from hospitalized patients. The incidence of VRE in isolates causing nosocomial infection increased from 1.8% in 1995 to 6.7% in 1997 and 25.2% in 1999 (Figure 3). Among these VRE isolates, 4 were from blood, 15 from urine, and the rest were pus or drainage fluid. Only 12 (15%) of these isolates were from patients admitted to ICUs, and 6 of these 12 isolates were recovered in 1999. The incidence of VRE in enterococci causing nosocomial infections in ICUs was 7.0%. The relationship of increasing vancomycin use and the increase in vancomycin resistance in enterococci is shown in Figure 3.
Figure 3.
Incidences of vancomycin-resistant enterococci (VRE) among all enterococcal isolates causing nosocomial infections in relation to vancomycin use at National Taiwan University Hospital, 1995-1999. Numbers above the bars denote the number of enterococcal isolates causing nosocomial infections. Numbers within the bars denote the numbers of VRE.
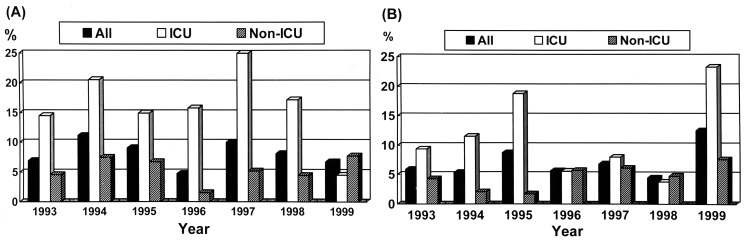
The incidences of imipenem-resistant P. aeruginosa (1993 to 1998) and imipenem-resistant Acinetobacter baumannii (1999) isolated from ICUs were five- to ten-fold higher than isolates recovered from non-ICU settings. However, this was not the case with imipenem-resistant P. aeruginosa in 1999 or imipenem-resistant A. baumannii in 1993-1998 (Figure 4).
Figure 4.
Proportions of Pseudomonas aeruginosa (A) and Acinetobacter baumannii (B) isolates causing nosocomial infections resistant to imipenem in National Taiwan University Hospital, 1993-1999. ICU = intensive care unit.
All 150 isolates of Candida species were inhibited by 1 μg/mL of amphotericin B (MIC range 0.03 to 1 μg/mL). The MIC50 and MIC90 of C. glabrata were 16 μg/mL and >32 μg/mL, respectively. Twenty-one isolates (70%) of C. glabrata were nonsusceptible to fluconazole (MICs >8 μg/mL). Four (15.4%) of the C. parapsilosis isolates had MICs >8 μg/mL (2 had MICs 16 μg/mL and the other 2 had MICs 64 μg/mL).
Discussion
Hospitals worldwide are continuing to face the crisis of the upsurge and dissemination of antimicrobial-resistant bacteria, particularly those causing nosocomial infections in ICU patients 1,27–29. Among resistant bacteria, MRSA, MRCoNS, VRE, third-generation cephalosporin-resistant Enterobacteriaceae, and imipenem- or ciprofloxacin-resistant P. aeruginosa and A. baumannii are of great concern because these bacteria have spread worldwide and ultimately will compromise the antimicrobial therapy of infections caused by these organisms 2,25–28,30.
This report describes trends in major nosocomial pathogens and shifts in antimicrobial resistance during a 19-year period in a large teaching hospital in Taiwan. In a comparison of data from a recent NNIS study and other surveillance systems 2,4,9,31, our results suggest four conclusions. First, Candida species, rather than P. aeruginosa, E. coli, or staphylococci, now are the most frequent pathogens causing overall nosocomial infections and BSIs in this hospital. The upward trend in coagulase-negative staphylococci, which was the leading cause of BSI in the recent NNIS study, was not confirmed in our study. Second, we observed a remarkably high incidence of MRSA, especially in ICUs, contrasted with a relatively low incidence of VRE. Third, we report an increase in incidence of cefotaxime-resistant Enterobacteriaceae, especially in the incidence of cefotaxime-resistant K. pneumoniae in ICUs. Fourth, although the overall incidence of imipenem resistance among P. aeruginosa and A. baumannii in recent years has remained stable (4% to 11%), higher incidences of imipenem-resistant P. aeruginosa or A. baumannii were found in ICUs than in general wards in most time periods.
Since 1990, Candida species have continued to be an important cause of nosocomial BSI in the United States, and the proportion (40%-50%) of these infections due to species of Candida other than C. albicans may be increasing (12,19,20,31,32). Among the species of Candida other than C. albicans, C. glabrata (prone to be resistant to fluconazole) and C. krusei (intrinsically resistant to fluconazole) are of clinical importance 31,33. Although the proportion (40%) of candidemia due to non-albicans Candida species in 1999 in our hospital was similar to that (48%) reported in the United States from April 1995 to June 1996, the incidences of C. glabrata (8.8%) and C. krusei (0%) in our hospital were lower than those (20% and 5%, respectively) in the United States 31.
Although an upsurge in the incidences of K. pneumoniae and E. coli isolates resistant to cefotaxime was noted in our ICUs, an investigation is under way into the mechanisms of resistance and potential outbreaks (clonal dissemination or gene transfer) 34. The abrupt increase in the proportion of A. baumannii isolates resistant to imipenem in 1999 resulted from wide dissemination of several multidrug-resistant clones in ICUs and many general wards in the hospital (data not shown).
In summary, surveillance of the microbial etiology of nososcomial infections over prolonged time periods not only can provide important information for day-to-day decision making in antimicrobial therapy in individual hospitals but also can reflect local trends and shifts in etiology and antimicrobial drug resistance. Nosocomial pathogens have shifted away from easily treated bacteria toward more resistant bacteria and even to Candida species with fewer options for therapy. These shifts continue to present challenges for nosocomial infection control and prevention.
Biography
Dr. Hsueh is an assistant professor in the departments of Laboratory Medicine and Internal Medicine, National Taiwan University College of Medicine. His research interests include epidemiology of emerging and nosocomial infections and mechanisms of antimicrobial drug resistance. He is actively involved in developing a national research program for antimicrobial drug resistance (Surveillance for Multicenter Antimicrobial Resistance in Taiwan).
Footnotes
Suggested Citation: Hsueh P, Chen M, Sun C, Chen W, Pan H, Yang L, et al. Antimicrobial Drug Resistance in Pathogens Causing Nosocomial Infections at a University Hospital in Taiwan, 1981-1999. Emerg Infect Dis. [serial on the Internet]. 2002 Jan [date cited]. Available from http://www.cdc.gov/ncidod/eid/vol8no1/00-0454.htm
References
- 1.Archibald L, Phillips L, Monnet D, McGowan JE Jr, Tenover FC, Gaynes RP. Antimicrobial resistance in isolates from inpatients and outpatients in the United States: increasing importance of the intensive care unit. Clin Infect Dis. 1997;24:211–5. [DOI] [PubMed] [Google Scholar]
- 2.CDC NNIS System. National Nosocomial Infections Surveillance (NNIS) system report, data summary from January 1990-May 1999, issued June 1999. Am J Infect Control. 1999;27:520–32. 10.1016/S0196-6553(99)70031-3 [DOI] [PubMed] [Google Scholar]
- 3.Emori TG, Gaynes RP. An overview of nosocomial infections, including the role of the microbiology laboratory. Clin Microbiol Rev. 1993;6:428–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fridkin SK, Steward CD, Edwards JR. Surveillance of antimicrobial use and antimicrobial resistance in United States hospitals: project ICARE phase 2. Clin Infect Dis. 1999;29:245–52. 10.1086/520193 [DOI] [PubMed] [Google Scholar]
- 5.Sahm DF, Marsillio MK, Piazza G. Antimicrobial resistance in key bloodstream bacterial isolates: electronic surveillance with the surveillance network database-USA. Clin Infect Dis. 1999;29:259–63. 10.1086/520195 [DOI] [PubMed] [Google Scholar]
- 6.Fraser VJ, Jones M, Dunkel J. Candidemia in a tertiary care hospital: epidemiology, risk factors, and predictors of mortality. Clin Infect Dis. 1992;15:414–21. [DOI] [PubMed] [Google Scholar]
- 7.Husni RN, Goldstein LS, Arroliga AC, Hall GS, Fatica C, Stoller JK, et al. Risk factors for an outbreak of multi-drug-resistant Acinetobacter nosocomial pneumonia among intubated patients. Chest. 1999;115:1378–82. 10.1378/chest.115.5.1378 [DOI] [PubMed] [Google Scholar]
- 8.Rello J. Acinetobacter baumannii infections in the ICU. Chest. 1999;115:1226–8. 10.1378/chest.115.5.1226 [DOI] [PubMed] [Google Scholar]
- 9.Richards MJ, Edwards JR, Culver DH, Gaynes RP. Nosocomial infections in medical intensive care units in the United States. Crit Care Med. 1999;27:887–92. 10.1097/00003246-199905000-00020 [DOI] [PubMed] [Google Scholar]
- 10.Valles J, Leon C, Alvarez-Lerma F; Spanish Collaborative Group for Infections in Intensive Care Units of Sociedad Espanola de Medicina Intensiva y Unidades Coronarias (SEMIUC). Nosocomial bacteremia in critically ill patients: a multicenter study evaluating epidemiology and prognosis. Clin Infect Dis. 1997;24:387–95. [DOI] [PubMed] [Google Scholar]
- 11.Banerjee SN, Emori TG, Culver DH, Gaynes RP, Jarvis WR, Horan T, et al. Secular trends in nosocomial primary bloodstream infections in the United States, 1980-1989. National Nosocomial Infections Surveillance System. Am J Med. 1991;91(suppl 3B):S86–9. 10.1016/0002-9343(91)90349-3 [DOI] [PubMed] [Google Scholar]
- 12.Beck-Sague CM, Jarvis WR; National Nosocomial Infections Surveillance System. Secular trends in the epidemiology of nosocomial fungal infections in the United States, 1980-1990. J Infect Dis. 1993;167:1247–51. [DOI] [PubMed] [Google Scholar]
- 13.Edmond MB, Wallace SE, McClish DK, Pfaller MA, Jones RN, Wenzel RP. Nosocomial bloodstream infections in United States hospitals: a three-year analysis. Clin Infect Dis. 1999;29:239–44. 10.1086/520192 [DOI] [PubMed] [Google Scholar]
- 14.Chen ML, Chen YC, Pan HJ, Chang SC, Yang LS, Ho SW, et al. Secular trends in the etiology of nosocomial infection at a teaching hospital in Taiwan, 1981-1994. Chinese Journal of Microbiology and Immunology. 1995;28:203–17. [PubMed] [Google Scholar]
- 15.Schaberg DR, Culver DH, Gaynes RP. Major trends in the microbial etiology of nosocomial infection. Am J Med. 1991;91(suppl 3B):S72–5. 10.1016/0002-9343(91)90346-Y [DOI] [PubMed] [Google Scholar]
- 16.Bodey GP. The emergence of fungi as major hospital pathogens. J Hosp Infect. 1988;11(suppl A):411–26. 10.1016/0195-6701(88)90220-4 [DOI] [PubMed] [Google Scholar]
- 17.Borg-von Z, Eiffert MH, Kann M, Ruchel R. Changes in the spectrum of fungal isolates: results from clinical specimens gathered in 1987/88 compared with those in 1991/92 in the University Hospital Gottingen, Germany. Mycoses. 1993;36:247–53. [DOI] [PubMed] [Google Scholar]
- 18.Harvey RL, Myers JP. Nosocomial fungemia in a large community teaching hospital. Arch Intern Med. 1987;147:2117–20. 10.1001/archinte.147.12.2117 [DOI] [PubMed] [Google Scholar]
- 19.Pfaller MA. Epidemiology and control of fungal infections. Clin Infect Dis. 1994;19(suppl 1):S8–13. [DOI] [PubMed] [Google Scholar]
- 20.Rangel-Frausto MS, Wiblin T, Blumberg HM, Saiman L, Patterson J, Rinaldi M, et al. National Epidemiology of Mycoses Survey (NEMIS): variation in rates of bloodstream infections due to Candida species in seven surgical intensive care units and six neonatal intensive care units. Clin Infect Dis. 1999;29:253–8. 10.1086/520194 [DOI] [PubMed] [Google Scholar]
- 21.Emori TG, Culver DH, Horan TC, Jarvis WR, White JW, Olson DR, et al. National nosocomial infections surveillance system (NNIS): description of surveillance methods. Am J Infect Control. 1991;19:19–35. 10.1016/0196-6553(91)90157-8 [DOI] [PubMed] [Google Scholar]
- 22.Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988;16:128–40. 10.1016/0196-6553(88)90053-3 [DOI] [PubMed] [Google Scholar]
- 23.National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial disk susceptibility tests-sixth edition. Approved standard M2-A6. Wayne (PA): The Committee; 1998. [Google Scholar]
- 24.National Committee for Clinical Laboratory Standards. Reference method for broth dilution antifungal susceptibility testing of yeasts: Approved standard M27-A. Wayne (PA): The Committee; 1997. [Google Scholar]
- 25.Hsueh PR, Wu JJ, Lu JJ, Teng LJ, Luh KT. Antimicrobial susceptibilities of clinical isolates of vancomycin-resistant enterococci in Taiwan. J Formos Med Assoc. 1999;98:45–8. [PubMed] [Google Scholar]
- 26.Hsueh PR, Teng LJ, Pan HJ, Chen YC, Wang LH, Chang SC, et al. Emergence of vancomycin-resistant enterococci at a university hospital in Taiwan: persistence of multiple species and multiple clones. Infect Control Hosp Epidemiol. 1999;20:828–33. 10.1086/501592 [DOI] [PubMed] [Google Scholar]
- 27.Hsueh PR, Teng LJ, Yang PC, Chen YC, Ho SW, Luh KT. Persistence of a multidrug-resistant Pseudomonas aeruginosa clone in an intensive care burn unit. J Clin Microbiol. 1998;36:1347–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Troillet N, Samore MH, Carmeli Y. Imipenem-resistant Pseudomonas aeruginosa: risk factors and antibiotic susceptibility patterns. Clin Infect Dis. 1997;25:1094–8. 10.1086/516092 [DOI] [PubMed] [Google Scholar]
- 29.Weber DJ, Raasch R, Rutala WA. Nosocomial infections in the ICU: the growing importance of antibiotic-resistant pathogens. Chest. 1999;115:S34–41. 10.1378/chest.115.suppl_1.34S [DOI] [PubMed] [Google Scholar]
- 30.Gaynes RP, Culver DH. The National Nosocomial Infections Surveillance System: resistance to imipenem among selected gram-negative bacilli in the United States. Infect Control Hosp Epidemiol. 1992;13:10–4. [DOI] [PubMed] [Google Scholar]
- 31.Pfaller MA, Jones RN, Messer SA, Edmond MB, Wenzel RP. National Surveillance of Nosocomial Bloodstream Infection due to Candida albicans: frequency of occurrence and antifungal susceptibility in the SCOPE program. Diagn Microbiol Infect Dis. 1998;31:327–32. 10.1016/S0732-8893(97)00240-X [DOI] [PubMed] [Google Scholar]
- 32.Iwata K. Drug resistance in human pathogenic fungi. Eur J Epidemiol. 1992;8:407–21. 10.1007/BF00158576 [DOI] [PubMed] [Google Scholar]
- 33.Siu LK, Lu PR, Hsueh PR, Lin FM, Chang SC, Luh KT, et al. Bacteremia due to extended spectrum beta-lactamase producing Escherichia coli and Klebsiella pneumoniae in a pediatric oncology ward: clinical features and identification of different plasmids carrying both SHV-5 and TEM-1. J Clin Microbiol. 1999;37:402–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fridkin SK, Jarvis WR. Epidemiology of nosocomial fungal infections. Clin Microbiol Rev. 1996;9:499–511. [DOI] [PMC free article] [PubMed] [Google Scholar]