Abstract
Adolescents and young adults account for over 10 million HIV infections worldwide. Prevention of secondary transmission is a major concern as many HIV-positive youth continue to engage in risky sexual behavior. This study pilot-tested “+CLICK”, an innovative, web-based, sexual risk reduction intervention for HIV-positive youth as an adjunct to traditional clinic-based, self-management education. The theory-based application, developed for perinatally and behaviorally infected youth 13–24 years of age, provides tailored activities addressing attitudes, knowledge, skills, and self-efficacy related to sexual risk reduction. HIV-positive youth (N = 32) pilot-tested “+CLICK” to assess usability (ease of use, credibility, understandability, acceptability, motivation) and short-term psychosocial outcomes (importance and self-efficacy related to abstinence and condom use) using a single group, pre-/post-test study design in a hospital-based pediatric clinic and community locations. A subsample of participants (n = 20) assessed feasibility for clinic use. Participants were 62.5% female, 68.8% Black, and 28.1% Hispanic. Mean age was 17.8 years (SD = 2.55), 43.8% were infected behaviorally, 56.2% perinatally, and 68.8% were sexually experienced. Usability ratings were high: 84.4% rated the application very easy to use; 93.8% perceived content as trustworthy; 87.5% agreed most words were understandable; 87.5% would use the application again. Short-term psychosocial outcomes indicate a significant increase in condom use self-efficacy (p = 0.008) and positive trends toward importance (p = 0.067) and self-efficacy (p = 0.071) for waiting before having sex. Regarding feasibility, participants accessed “+CLICK” during waiting periods (average time, 15 minutes) in their routine clinic visit. Clinic staff rated “+CLICK” highly in providing consistent, confidential, and motivational sexual health education without significant disruption to clinic flow. Results suggest that the application is a feasible tool for use in the clinic and has the potential to affect psychological antecedents to sexual behavior change. Further research on long-term and behavioral effects is indicated prior to broader dissemination into clinical practice.
Keywords: HIV-positive, youth, computer-based interventions, behavioral interventions, self-management training
Adolescents and young adults account for forty percent of new HIV infections worldwide (WHO 2008) and almost half of all new HIV infections in the USA (CDC, 2005). Prevention of secondary transmission is a primary concern, given that many HIV-positive youth engage in risky sexual behavior (Rotheram-Borus et al., 2001). Current pediatric clinical care guidelines provide limited recommendations regarding sexual behavior intervention among HIV-positive youth although these guidelines link to prevention information (CDC, 2003). The provision of systematic, confidential, developmentally appropriate sexual health education is critical for enhancing the sexual health of HIV-positive youth and for reducing secondary transmission. Computer-based applications have proved an effective modality for the systematic application of self-management guidelines in other chronic disease areas (Hunt, Haynes, Hanna, & Smith, 1998; Sanders & Aronsky, 2006; Shegog et al., 2006) and may provide a promising approach for HIV self-management. This study investigates the potential of “+CLICK” (Positive Click), an innovative, web-based, sexual risk reduction intervention to provide systematic sexual health education as an adjunct to traditional clinic-based self-management training.
Studies among HIV-positive youth indicate that 40–60% continue to engage in unprotected sexual intercourse after learning their HIV status (Rotheram-Borus et al., 2001), (Lightfoot, Swendeman, Rotheram-Borus, Comulada, & Weiss, 2005), (Murphy et al., 2001), (Sturdevant et al., 2001), (Kadivar, Garvie, Sinnock, Heston, & Flynn, 2006). Among perinatally infected youth it is estimated that 27% of girls became sexually active and 24.2% became pregnant at least once by age 19 (Brogly et al., 2007). Multiple factors have been identified related to lack of condom use among HIV-positive youth including older partner age, having an HIV-positive partner, longer relationship duration, and lack of social support for safer sex (Brown, Lourie, & Pao, 2000a). Only about half of HIV-positive sexually active females use effective contraceptive methods despite accessibility and availability of contraceptives (Belzer et al., 2001). Furthermore, only about half of HIV-positive youth report full disclosure of their serostatus to every sexual partner with implications for secondary transmission (Rotheram-Borus & Miller, 1998). Effective sexual education is critical to help HIV-positive youth make informed decisions regarding their own sexual and reproductive health and to reduce the risk of secondary transmission.
Few theory-based sexual risk reduction interventions for HIV-positive youth have been developed and rigorously evaluated. Teens Linked to Care consisted of 31, two-hour sessions focused on reducing transmission acts and improving quality of life. The intervention reduced the frequency of unprotected sex and reduced the number of HIV-negative and unknown serostatus partners (Lee, Leibowitz, A. & Rotheram-Borus, 2005). However, the small group delivery was problematic – 27% of youth did not attend even one session (Rotheram-Borus et al., 2001). Healthy Choices, a motivational enhancement intervention focused on sexual and substance use behavior, consisted of four, weekly one-hour sessions delivered in a clinic setting. The intervention reported significant reductions in unprotected sex and viral load (Naar-King et al., 2006a). However, attendance was a barrier with 24% not attending a single session. These studies indicate that behavioral interventions related to sexual health can have positive results; however, low attendance may be a barrier if sessions occur outside of routine clinic visits.
Computer-based health education applications can provide a modality to overcome reported barriers to traditional youth HIV educational programs because they offer the potential for individualized, tailored, and confidential skills training through interactive and vicarious methods. Findings have supported the potential of computer-based applications as an adjunct to youth STI/HIV prevention education (Mackenzie et al., 2007; Shegog et al., 2007). However, despite refinements in clinical and behavioral HIV-positive care protocols and the ubiquity of computer-based technology, the potential of computer-based HIV self-management education in the clinical setting has not yet been investigated.
The purpose of this study was to pilot-test “+CLICK,” a tailored, web-based application designed to enhance sexual risk reduction skills among HIV-positive youth. The theory-based application was developed for perinatally and behaviorally infected youth ages 13–24 as an adjunct to traditional clinic-based self-management education. The pilot-test comprised two components: (1) an usability study to assess youths’ reactions to the application and short-term psychosocial outcomes; and (2) a sub-study assessing feasibility for clinic use. Together, these findings provide insight into the potential of web-based training as a systematic approach to clinic-based sexual health education.
Methods
Intervention development
“+CLICK” is based on Social Cognitive Theory (SCT), self-regulation theory, and Brief Motivational Enhancement Therapy (MET). SCT describes the reciprocal interaction of personal (e.g. perceived self-efficacy), environmental (e.g. influential role models), and behavioral influences (e.g. self-regulation of chronic disease) (Bandura, 1991). Self-regulation theory includes three principle sub-functions: behavior self-monitoring; self-judgment of one’s behavior related to personal standards and environmental circumstances; and affective self-reaction (Bandura, 1991). In “+CLICK” this self-regulation framework is represented as Select, Detect, Protect – selecting personal limits ahead of time, detecting signs and situations that challenge those limits, and using effective self-management skills to maintain those limits. MET is a brief intervention based on Motivational Interviewing (MI) which has proved effective for behavioral interventions with HIV-positive youth (Naar-King et al., 2006a). In “+CLICK” MET principles guide the tailoring of activities based on participants’ perceived importance and self-efficacy related to specific behaviors.
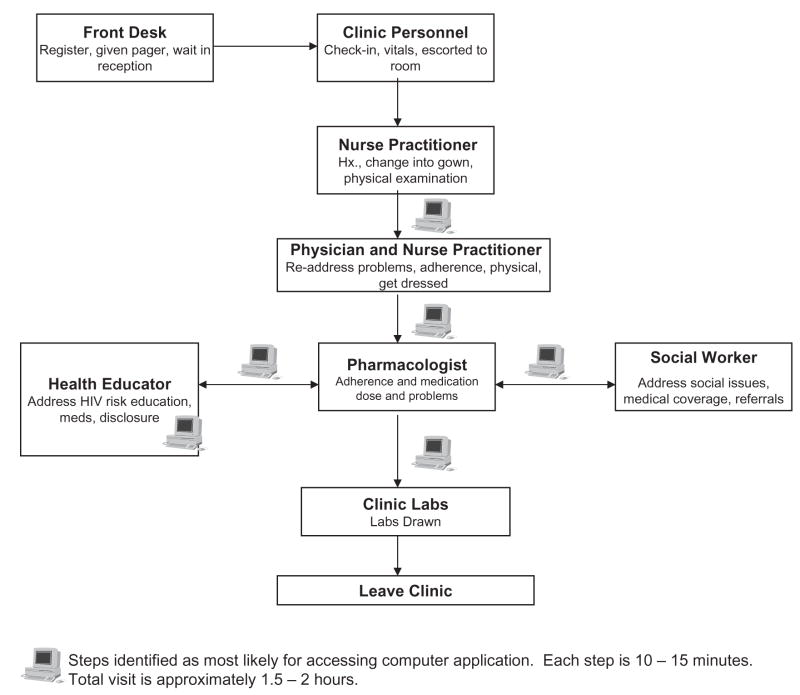
“+CLICK” targets four behaviors: choosing not to have sex, disclosing HIV status to a potential sex partner, using condoms correctly and consistently, and using an effective method of birth control along with condoms. These behaviors, and related psychosocial determinants, were identified through a review of empirical studies with HIV-positive youth and through in-depth interviews with HIV-positive youth (n = 20) and healthcare providers (n = 15), conducted as part of the formative research process. Previous studies have indicated that knowledge, self-efficacy, perceived peer norms, and social support are all important mediating variables for abstinence and/or condom use among HIV-positive youth (Brown et al., 2000b), (Naar-King et al., 2006b), (Wiener, Battles, & Wood, 2006). The in-depth interviews corroborated these findings, and also provided evidence that a computerized self-management application would be appealing to both youth and providers (Leonard et al., 2007a). A final step in the development process included a task analysis of patient flow in a HIV pediatric clinic to determine potential application placement during a routine clinic visit (Figure 1).
Figure 1.
Steps in outpatient clinic flow and proposed access to “+CLICK”.
Intervention
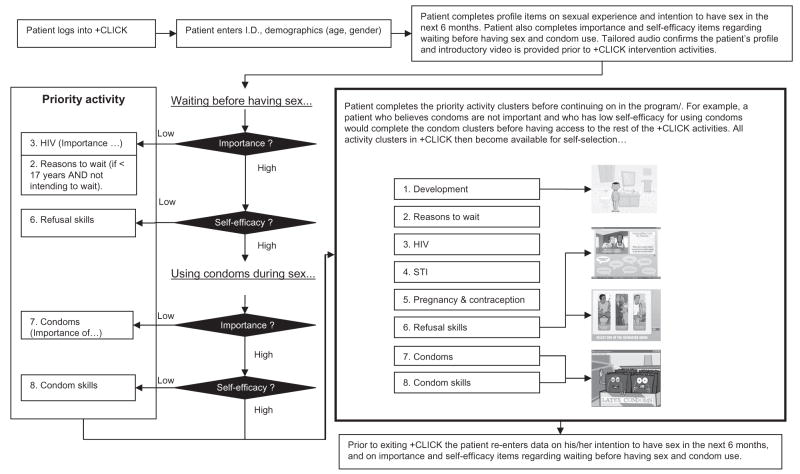
“+CLICK” is a tailored, web-based application, developed in Adobe Flash® that provides activities including animation, interactive activities, peer and expert video. The majority of activities were adapted from an existing computer-based HIV prevention intervention, “It’s Your Game, Keep it Real” (Shegog et al., 2007). The application is designed for individual access via the web within the context of the routine clinic visit. To access the application, youth input an unique identifier and provide demographic, behavioral, and attitudinal data to create a personal profile. The profile then guides the tailoring functions. Activities are tailored on age, gender, self-reported sexual experience and intentions, and perceived importance and self-efficacy related to abstinence and condom use. Perceptions regarding importance and self-efficacy are assessed using semantic differential scales modeled on MI protocols (Velasquez, Maurer, Crouch, & DiClemente, 2001) operated using slider bars. For example, learners are instructed to, “Use the slider bar on this scale from 0 to 10 to show how important you think it is to wait until you are older before you have sex, or have sex again.” Figure 2 depicts the overall flow of the application, the tailoring algorithm, and resulting activity clusters.
Figure 2.
Overall application flow, tailoring algorithm, and resulting activity clusters.
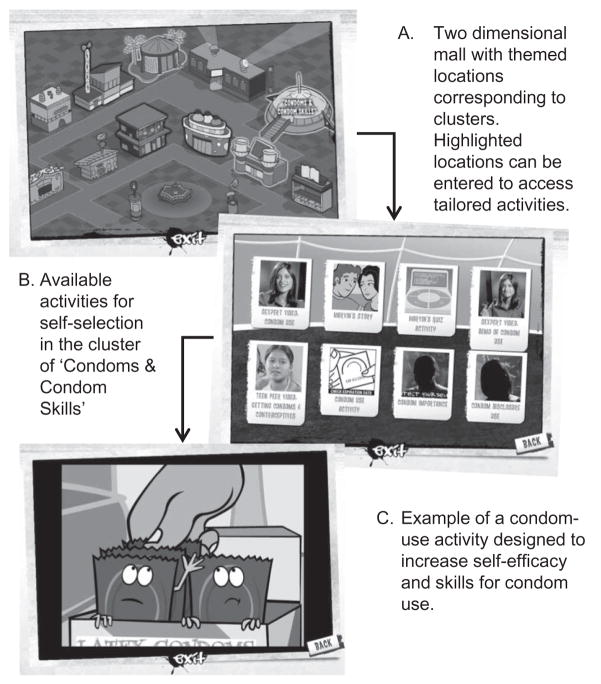
On completion of data entry the youth receives a tailored, audio message confirming his/her profile. The youth continues to the hub of “+CLICK” which is a representation of a two-dimensional mall with themed locations corresponding to activity clusters (Figure 3). Activity clusters are made available on the basis of the individual’s “risk” profile, e.g. low condom use self-efficacy prompts condom self-efficacy activities to be available. Tailored activity clusters are completed prior to accessing other activities. Upon leaving the application, youth re-enter slider bar data on importance and self-efficacy regarding abstinence and condoms, assessing immediate program impact. Youth may re-access the game at a later time from another computer location and resume activities from the point of exit.
Figure 3.
Screen captures illustrating movement from program hub (mall) through an activity cluster, to an individual activity.
Procedure
The pilot study comprised two components: an usability study to assess youth reactions to the application and its effect on short-term psychosocial outcomes, and a sub-study assessing feasibility for clinic use.
Usability study
Study design
A single group, pre-/post-test study was conducted to assess usability and short-term psychosocial outcomes.
Participants
In winter 2007, a convenience sample (N = 32) of HIV-positive youth ages 13–24 years was recruited from two locations in a Southeastern US city: a hospital-based HIV pediatric clinic and a community agency providing support services to HIV-positive youth. Youth were recruited through personal contact with clinic and agency personnel and through flyers posted at both locations. The small sample size was consistent with usability testing protocols that do not require statistical significance to determine major usability problems (Nielsen, 1993), (Faulkner, 2003).
Study protocol
Participants accessed “+CLICK” via the Internet on a hospital computer during their routine medical visit or at the community agency or other community locations using laptop computers on which the application was installed. To facilitate use, a member of the research team reviewed the application’s operational functions with youth prior to use and remained available to assist throughout the session. Active parental consent and youth consent were obtained. To protect confidentiality, each computer was provided with headphones and screens were positioned so as not to be visible to others. The study received Institutional Review Board approval from the authors’ institutions.
Data collection
Questionnaire, computer-based, and observational data were collected. Demographic data included gender, race/ethnicity, and age. Data specific to HIV status included mode of infection, length of time living with HIV, age of awareness of HIV status, recent viral load and CD4 count, current medication status, and number of missed doses in the past week. Data specific to sexual experience included ever had sex, condom use at last intercourse, past three months’ frequency of sex without a condom and number of sexual partners.
Usability parameters including ease of use, credibility, understandability, acceptability, and motivation were assessed using Likert scale ratings adapted from preexisting usability assessment instruments (Shegog et al., 2007). Pre- and post-user ratings on psychosocial outcomes, including the importance of waiting and condom use and self-efficacy in performing these skills, were assessed using semantic differential slider bar scales embedded in the application. These pre- and post-user ratings were measured during the same pilot session, once immediately prior to using “+CLICK”, and again immediately after using “+CLICK”. Open-ended responses on recommendations for improvement were collected within the application and via paper–pencil questionnaire.
Data analysis
Data to assess usability ratings and short-term impact on psychosocial outcomes were analyzed using descriptive statistics and the Wilcoxon Signed-Rank test using SPSS analytic software. Power to detect change in psychosocial outcomes was 0.19 to detect a pre/post change of 0.2 standard units, assuming a two-tailed alpha of 0.05 and n = 30, consistent with previous pilot studies that primarily focus on usability and feasibility.
Feasibility sub-study
Feasibility for clinic use was assessed with the subset of participants (n = 20) who accessed “+CLICK” at the pediatric HIV clinic during their routine medical visit. Clinic staff observed factors related to feasibility including time on task, impact on clinic flow and patient–provider interactions, and motivation to use at subsequent visits. Open-ended questions captured participants’ reactions to the application. Clinical care team members, including case managers and nurse practitioners, were interviewed regarding feasibility. Instruments were adapted from previously validated feasibility protocols (Shegog et al., 2006).
Results
Demographics
Participants (N = 32) were 62.5% female, 68.8% Black, 28.1% Hispanic, and 3.1% White (Table 1). Mean age was 17.8 years (SD = 2.55, range 13–24). Fifty-six percent of participants were infected perinatally, 43.8% behaviorally. Participants had been living with HIV on average for 11.1 years (SD = 7.75); most learned their HIV status at age 12. Forty-seven percent reported an undetectable viral load, whilst 6.2% reported a viral load over 50,000. Just under half (46.9%) reported a normal CD4 count, whilst 6.2% reported having low CD4 counts. Respectively, 28.1 and 21.9% could not report their viral load or CD4 counts. The majority (71.9%) reported taking antiretroviral medications; of these, 56.5% missed one or more doses within the past week.
Table 1.
Characteristics of sample (N = 32).
| Characteristic | N (%) |
|---|---|
| Gender | |
| Female | 20 (62.5) |
| Male | 12 (37.5) |
| Race/ethnicity | |
| Black | 22 (68.8) |
| Hispanic | 9 (28.1) |
| White | 1 (3.1) |
| Mode of HIV transmission | |
| Perinatal | 18 (56.2) |
| Behavioral | 14 (43.8) |
| Recent viral load | |
| Undetectable | 15 (46.9) |
| Less than 10,000 | 3 (9.4) |
| 10,000–50,000 | 2 (6.2) |
| > 50,000 | 2 (6.2) |
| Do not know | 9 (28.1) |
| Recent CD4 count | |
| Normal | 15 (46.9) |
| Slightly low | 7 (21.9) |
| Low | 2 (6.2) |
| Do not know | 7 (21.9) |
| Taking antiretroviral medications | 23 (71.9) |
| Number of times missed a dose in the past weeka | |
| 0 times | 10 (43.5) |
| 1–2 times | 11 (47.8) |
| 3 or more times | 2 (8.7) |
| Ever had sex | 22 (68.8) |
| Used condom at last sexual intercourseb | 16 (72.7) |
| Number of times had sex without a condom in past 3 monthsb | |
| 0 times | 14 (63.6) |
| 1–2 times | 3 (13.6) |
| 3 or more times | 4 (18.1) |
| Number of sexual partners in past 3 monthsb | |
| 0 partners | 5 (22.7) |
| 1 partner | 13 (59.1) |
| 2–3 partners | 3 (13.6) |
| 4 partners | 1 (4.5) |
| Mean years (SD) | |
| Age | 17.8 (2.55) |
| Length of time living with HIV | 11.1 (7.75) |
| Age when became aware of HIV status | 12.0 (4.85) |
Among participants who report taking antiretroviral medications.
Among participants who had ever had sex.
Regarding sexual experience, 22 (68.8%) reported being sexually experienced; of these, 72.7% used a condom at last sexual intercourse. During the past three months, 31.7% of sexually experienced youth had sex one or more times without a condom and 18.1% had more than one sexual partner.
All HIV-positive youth who were invited to participate in the pilot study agreed to do so. One participant initially voiced concerns regarding confidentiality of data entered into the computer; however, use of an unique identification number rather than a personal identifier allayed these concerns.
Access locations
Twenty participants accessed “+CLICK” during their routine medical visit, 11 accessed it at the community agency, and one participant accessed it at another community location.
Usability
Usability parameters were highly rated (Table 2). Ease of use: 84.4% of participants rated the program very easy to use and 93.8% felt the work pace was just right. Credibility: a minimum of 93.8% perceived content as correct and trustworthy. Ninety-four percent felt that information would help them make healthy choices. Understandability: 87.5% agreed most words were understandable. Acceptability: 81.2% liked the overall program a lot; 75.0% liked the cartoons a lot and 75.0% liked the videos a lot. Regarding the name “+CLICK,” 62.5% liked it a lot. Motivation: 87.5% would use the program again and 84.4% would tell their friends about “+CLICK.” Open-ended responses suggested overall satisfaction with the application.
Table 2.
Usability ratings and short-term psychosocial outcomes from “+CLICK” (N = 32).
| Usability ratings | n (%) | |||
|---|---|---|---|---|
| Ease of use | ||||
| Kind of easy to use | 3 (9.4) | |||
| Very easy to use | 27 (84.4) | |||
| Work pace | ||||
| Just right | 30 (93.8) | |||
| Credibility | ||||
| Information could be trusted | 30 (93.8) | |||
| Information was correct | 31 (96.9) | |||
| Information will help to make healthy choices | 30 (93.8) | |||
| Understandability | ||||
| Words were understandable | 28 (87.5) | |||
| Acceptability | ||||
| Liked the overall application | ||||
| Liked a little | 4 (12.5) | |||
| Liked a lot | 26 (81.2) | |||
| Liked the pictures and colors | ||||
| Liked a little | 4 (12.5) | |||
| Liked a lot | 25 (78.1) | |||
| Liked the cartoons | ||||
| Liked a little | 7 (21.9) | |||
| Liked a lot | 24 (75.0) | |||
| Liked the videos | ||||
| Liked a little | 6 (18.8) | |||
| Liked a lot | 24 (75.0) | |||
| Liked the name “+CLICK” | ||||
| Liked a little | 8 (25.0) | |||
| Liked a lot | 20 (62.5) | |||
| Motivation | ||||
| Would use +CLICK again | 28 (87.5) | |||
| Would tell others about +CLICK | 27 (84.4) | |||
| Short-term psychosocial outcomesa | Pre-test mean (SD) | Post-test mean (SD) | P valueb | |
| Importance of waiting to have sex, or to have sex again | 8.1 (2.24) | 9.0 (1.64) | .067 | |
| Self-efficacy to wait to have sex, or to have sex again | 7.8 (2.80) | 8.8 (1.89) | .071 | |
| Importance of condom use | 9.8 (0.57) | 9.8 (0.70) | .889 | |
| Self-efficacy for condom use | 9.1 (2.03) | 9.6 (1.25) | .008 | |
Matching pre- and post-tests missing for four participants (n = 28); range of possible scores, 0–10.
Wilcoxon signed rank test.
Short-term outcomes
Results indicate a trend toward increased perceived importance (p = 0.067) and self-efficacy (p = 0.071) regarding abstinence or waiting until older to have sex again. Regarding perceived importance of condom use, the mean score at pre-test was 9.8 on a scale from 0 to 10, with no significant increase at post-test. However, a significant increase in condom use self-efficacy was observed at post-test (p = 0.008).
Feasibility
The subset of clinic-based participants (n = 20) used the application on average for 15 minutes (range 10–60 minutes) during routine waiting periods in the clinic visit. Time was divided across four settings: waiting for or visiting with the health educator, the pharmacologist, the social worker, or laboratory personnel. One participant used the application for 60 minutes during an extended physician wait time. Application use did not adversely impact clinic flow. Participants liked the autonomy of using the application at their own pace and the confidentiality provided by headphones. Participants reported that the application provided a non-threatening means to receive information on sensitive topics, such as condom and contraceptive use. In addition, participants reported that “+CLICK” was thought-provoking and generated open dialogue with clinic staff regarding reviewed material. Clinic staff rated the application highly as a method for providing consistent self-management education, especially on sensitive topics, and perceived high patient motivation to use the application again.
Several features were identified to enhance the application for clinic use, including provision of a “Pause” button to accommodate frequent interruptions, and an activity menu to access specific activities with a patient as required.
Discussion
This study was designed to assess the usability and feasibility of a tailored, web-based sexual risk reduction application for HIV-positive youth as an adjunct to traditional clinic-based education. Previous behavioral self-management interventions have shown positive outcomes (Lee et al., 2005; Naar-King et al., 2006a); however, their effectiveness has been hampered by poor attendance. The capability of computer-based applications to provide systematic, interactive, and tailored educational experiences during a routine clinic visit may assist in overcoming such limitations.
Short-term psychosocial outcomes from “+CLICK” included significant increase in condom use self-efficacy and positive trends toward importance and self-efficacy for abstinence. These preliminary findings are comparable with short-term psychosocial outcomes reported in previous computer-based HIV prevention programs (Shegog et al., 2007) and are especially encouraging given the limited power to detect significant change in this study. This impact is partly explained by positive usability ratings that indicated the program is easy to use, credible, and motivating for HIV-positive youth. Ninety-four percent of participants believed it would help them to make healthy choices and 87.5% reported they would use it again. This has particular utility for repeated use at subsequent clinic visits. Also promising, is that all youth who were invited to pilot-test the application agreed to do so. This, and the perception of the program as a confidential medium to gain access to sensitive information, indicates the potential for this type of application to appeal to a broad HIV-positive youth population.
This study also assessed the feasibility of accessing a web-based application within the constraints of the clinical encounter and its impact on patient–provider communication. Findings demonstrated the potential to extend the “teachable moment” throughout the clinic encounter because “+CLICK” was accessed during waiting periods that would otherwise be used for non-educational activities. Furthermore, youth reported that it made it easier to talk with clinical providers about sensitive topics, such as condom and contraceptive use. Clinic staff rated “+CLICK” as providing consistent, confidential, and motivational self-management education that, importantly, did not significantly disrupt typical clinical activities or unduly extend appointment time.
The Internet has recognized advantages as a linkage channel for patient self-management monitoring and education (Chan et al., 2007) but there is currently a dearth of readily accessible, appealing, and evidence-based online HIV-positive self-management programs for youth. This pilot study represents a preliminary investigation toward understanding usability and feasibility of this channel. While “+CLICK” shows promise, it is important that these findings be interpreted in the light of study limitations. Although the small sample size was appropriate for the objectives of a feasibility study, the single group, pre-/post-test study design means that reported changes in short-term psychosocial outcomes may be subject to internal threats to validity. Any interpretations regarding causality need to be made with caution. In addition, these effects were measured immediately prior to and following the intervention, thus long-term psychosocial and behavioral outcomes were not assessed. Longer-term follow-up is necessary to assess the degree to which these outcomes are sustainable.
This study represents early work in examining the application of web-based educational technology in clinic-based HIV management training. Usability and feasibility studies of this type have traditionally been the vanguard of informatics research. Maturity of the application of this technology will occur with the emergence of new evidence based on rigorous evaluation of program efficacy, cost-benefit, and long-term effectiveness in increasing safer sex or abstinence behaviors, thus reducing the risk of HIV transmission. These “macro” level outcome analyses will need to be informed by “micro” level process analyses regarding patient information processing, efficacy of tailoring algorithms, impact of message design, and effect of “educational” setting (e.g. clinic vs. home). These studies of process and outcomes represent future research challenges in applying technology to AIDS care.
Conclusions
Provision of systematic, confidential education may positively impact the sexual health of HIV-positive youth and reduce the risk of secondary transmission. “+CLICK”, a tailored, web-based, sexual risk reduction training, may provide a viable adjunct to traditional clinic-based education. The application meets usability and feasibility criteria and shows potential for affecting psychological antecedents to sexual behavior change. Results suggest that further research on long-term and behavioral effects are warranted prior to broader dissemination into clinical practice.
Acknowledgments
This study was conducted with funding from the Baylor College of Medicine-University of Texas at Houston Center for AIDS Research, under grant number, P30 A103621 1-12. Christine Markham, corresponding author, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors made substantial contributions to the study’s conception and design, and to the acquisition, analysis, and interpretation of data; all authors participated in drafting or revising the manuscript for intellectual content, and provided final approval of the version to be published.
Footnotes
Publisher's Disclaimer: Full terms and conditions of use: http://www.informaworld.com/terms-and-conditions-of-access.pdf
This article may be used for research, teaching and private study purposes. Any substantial or systematic reproduction, re-distribution, re-selling, loan or sub-licensing, systematic supply or distribution in any form to anyone is expressly forbidden.
The publisher does not give any warranty express or implied or make any representation that the contents will be complete or accurate or up to date. The accuracy of any instructions, formulae and drug doses should be independently verified with primary sources. The publisher shall not be liable for any loss, actions, claims, proceedings, demand or costs or damages whatsoever or howsoever caused arising directly or indirectly in connection with or arising out of the use of this material.
References
- Bandura A. Social cognitive theory of self-regulation. Organizational Behavior and Human Decision Processes. 1991;50:248–287. [Google Scholar]
- Belzer M, Rogers AS, Camarca M, Fuchs D, Peralta L, Tucker D, et al. Contraceptive choices in HIV infected and HIV at-risk adolescent females. Journal of Adolescent Health. 2001;29:93–100. doi: 10.1016/s1054-139x(01)00282-8. [DOI] [PubMed] [Google Scholar]
- Brogly SB, Watts DH, Ylitalo N, Franco EL, Seage GR, III, Oleske J, et al. Reproductive health of adolescent girls perinatally infected with HIV. American Journal of Public Health. 2007;97:1047–1052. doi: 10.2105/AJPH.2005.071910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown LK, Lourie KJ, Pao M. Children and adolescents living with HIV and AIDS: A review. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2000a;41:81–96. [PubMed] [Google Scholar]
- Brown LK, Schultz JR, Parsons JT, Butler RB, Forsberg AD, Kocik SM, et al. Sexual behavior change among human immunodeficiency virus-infected adolescents with hemophilia. Adolescent Hemophilia Behavioral Intervention Evaluation Project Study Group. Pediatrics. 2000b;106:E22. doi: 10.1542/peds.106.2.e22. [DOI] [PubMed] [Google Scholar]
- CDC. MMWR – Morbidity & Mortality Weekly Report. RR12. Vol. 52. Department of Health and Human Services; 2003. Incorporating HIV prevention into the medical care of persons living with HIV; pp. 1–24. [PubMed] [Google Scholar]
- CDC. [Accessed 10 March, 2008];HIV Prevention Strategic Plan through 2005. 2005 [On-line] from http://www.cdc.gov/nchstp/od/hiv_plan/default.htm.
- Chan DS, Callahan CW, Hatch-Pigott VB, Lawless A, Proffitt HL, Manning NE, et al. Internet-based home monitoring and education of children with asthma is comparable to ideal office-based care: Results of a 1-year asthma in-home monitoring trial. Pediatrics. 2007;119:569–578. doi: 10.1542/peds.2006-1884. [DOI] [PubMed] [Google Scholar]
- Faulkner L. Beyond the five-user assumption: Benefits of increased sample sizes in usability testing. Behavior Research Methods, Instruments. Computers. 2003;35:379–383. doi: 10.3758/bf03195514. [DOI] [PubMed] [Google Scholar]
- Hunt DL, Haynes RB, Hanna SE, Smith K. Effects of computer-based clinical decision support systems on physician performance and patient outcomes: A systematic review. JAMA: Journal of the American Medical Association. 1998;280:1339–1346. doi: 10.1001/jama.280.15.1339. [DOI] [PubMed] [Google Scholar]
- Kadivar H, Garvie PA, Sinnock C, Heston JD, Flynn PM. Psychosocial profile of HIV-infected adolescents in a Southern US urban cohort. AIDS Care. 2006;18:544–549. doi: 10.1080/13548500500228763. [DOI] [PubMed] [Google Scholar]
- Lee MB, Leibowitz A, Rotheram-Borus MJ. Cost-effectiveness of a behavioral intervention for seropositive youth. AIDS Education and Prevention. 2005;17:105–118. doi: 10.1521/aeap.17.3.105.62906. [DOI] [PubMed] [Google Scholar]
- Leonard A, Markham C, Bui TC, Shegog R, Paul M. The young and HAART: Perspectives of HIV + youth and health care providers. Poster presented at the United States Conference on AIDS; Palm Springs, CA. 2007a. [Google Scholar]
- Leonard A, Markham C, Bui TC, Shegog R, Paul M. HIV + youth speak out: Insights for secondary prevention. Oral presentation at the 2007 National HIV Prevention Conference; Atlanta, GA. 2007b. [Google Scholar]
- Lightfoot M, Swendeman D, Rotheram-Borus MJ, Comulada WS, Weiss R. Risk behaviors of youth living with HIV: Pre- and post-HAART. American Journal of Health Behavior. 2005;29:162–171. doi: 10.5993/ajhb.29.2.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenzie SL, Kurth AE, Spielberg F, Severynen A, Malotte CK, St Lawrence J, et al. Patient and staff perspectives on the use of a computer counseling tool for HIV and sexually transmitted infection risk reduction. Journal of Adolescent Health. 2007;40:572e9–572e16. doi: 10.1016/j.jadohealth.2007.01.013. [DOI] [PubMed] [Google Scholar]
- Murphy DA, Durako SJ, Moscicki AB, Vermund SH, Ma Y, Schwarz DF, et al. No change in health risk behaviors over time among HIV infected adolescents in care: Role of psychological distress. Journal of Adolescent Health. 2001;29:57–63. doi: 10.1016/s1054-139x(01)00287-7. [DOI] [PubMed] [Google Scholar]
- Naar-King S, Wright K, Parsons JT, Frey M, Templin T, Lam P, et al. Healthy choices: Motivational enhancement therapy for health risk behaviors in HIV-positive youth. AIDS Education and Prevention. 2006a;18:1–11. doi: 10.1521/aeap.2006.18.1.1. [DOI] [PubMed] [Google Scholar]
- Naar-King S, Wright K, Parsons JT, Frey M, Templin T, Ondersma S. Transtheoretical model and condom use in HIV-positive youths. Health Psychology. 2006b;25:648–652. doi: 10.1037/0278-6133.25.5.648. [DOI] [PubMed] [Google Scholar]
- Nielsen J. Usability Engineering. San Francisco, CA: Morgan Kaufmann; 1993. [Google Scholar]
- Rotheram-Borus MJ, Lee MB, Murphy DA, Futter-man D, Duan N, Birnbaum JM, et al. Efficacy of a preventive intervention for youths living with HIV. American Journal of Public Health. 2001;91:400–405. doi: 10.2105/ajph.91.3.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Miller S. Secondary prevention for youths living with HIV. AIDS Care. 1998;10:17–34. doi: 10.1080/713612347. [DOI] [PubMed] [Google Scholar]
- Sanders DL, Aronsky D. Biomedical informatics applications for asthma care: A systematic review. Journal of the American Medical Informatics Association. 2006;13:418–427. doi: 10.1197/jamia.M2039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shegog R, Bartholomew LK, Sockrider MM, Czyzewski DI, Pilney S, Mullen PD, et al. Computer-based decision support for pediatric asthma management: Description and feasibility of the stop asthma clinical system. Health Informatics Journal. 2006;12:259–273. doi: 10.1177/1460458206069761. [DOI] [PubMed] [Google Scholar]
- Shegog R, Markham C, Peskin M, Dancel M, Coton C, Tortolero S. It’s your game”: An innovative multimedia virtual world to prevent HIV/STI and pregnancy in middle school youth. Medinfo. 2007;12:983–987. [PubMed] [Google Scholar]
- Sturdevant MS, Belzer M, Weissman G, Friedman LB, Sarr M, Muenz LR. The relationship of unsafe sexual behavior and the characteristics of sexual partners of HIV infected and HIV uninfected adolescent females. Journal of Adolescent Health. 2001;29:64–71. doi: 10.1016/s1054-139x(01)00286-5. [DOI] [PubMed] [Google Scholar]
- Velasquez MM, Maurer GG, Crouch C, DiClemente CC. Group treatment for substance abuse: A stage-of-change therapy manual. 1. New York: The Guilford Press; 2001. [Google Scholar]
- WHO. [Accessed August 19, 2008];Highlights: Child and Adolescent Health and Development. Progress Report 2006–2007. 2008 [On-line] from http://www.who.int/child_adolescent_health/en/
- Wiener LS, Battles HB, Wood LV. A longitudinal study of adolescents with perinatally or transfusion acquired HIV infection: Sexual knowledge, risk reduction self-efficacy and sexual behavior. AIDS and Behavior. 2006;11:471–478. doi: 10.1007/s10461-006-9162-y. [DOI] [PMC free article] [PubMed] [Google Scholar]