Abstract
This paper aimed to determine whether non-fatal opioid overdose and suicide attempts are distinct behaviours by examining the histories of 1500 opioid-dependent individuals. This paper utilised data collected as part of a large retrospective case-control study. Unintentional non-fatal opioid overdoses were more common than suicide attempts (58% vs. 32%). Overall, the correlates associated with a history of attempted suicide only and non-fatal opioid overdose only were different. Drug-related risk behaviours (including high impulsivity, injection of opioids, sedative dependence) were associated with non-fatal opioid overdose; and a history of mental disorders (depression, anxiety disorder, and screening positive for borderline personality disorder (BPD+) were associated with suicide attempts. Additionally, those who reported a history of both behaviours had a more severe clinical profile including excessive drug use, psychological disorders and childhood trauma. The study concluded that non-fatal opioid overdose and attempted suicide are distinct clinically significant problems that require different approaches for prevention. Additionally, if both behaviours are reported a thorough assessment of underlying comorbid problems should be initiated by treatment services.
Keywords: attempted suicide, drug overdose, heroin dependence, comorbidity, psychosocial factors
1. Introduction
In high income countries, mortality rates among opioid users have been found to be 13 times higher than among the general population (Hulse, English, Milne, & Holman, 1999). Both suicide and opioid overdose contribute to the substantial rates of premature death reported among opioid users (Darke, Degenhardt, & Mattick, 2006). Fatal overdoses and suicides, however, represent only a small proportion of the total number of overdose and suicide events (both fatal and non-fatal) (Darke et al., 2006). Not only has a history of an overdose or a suicide attempt been shown to best predict subsequent mortality, but both behaviours have been associated with substantial morbidity in their own right (Darke et al., 2006; Darke & Ross, 2002). Considering the substantial morbidity and mortality which exists a thorough comparison of the associated correlates is important.
Studies typically suggest around a third of opioid-dependent individuals report a lifetime suicide attempt (Darke & Ross, 2001; Darke, Ross, Lynskey, & Teesson, 2004; Murphy, Rounsaville, Eyre, & Kleber, 1983; Rossow & Lauritzen, 1999). Although limited, research suggests that the risk factors associated with attempted suicide among opioid-dependent individuals include gender (female), psychiatric morbidity, social isolation, family dysfunction, impulsivity and drug dependence (other than opioids) (Darke & Ross, 2002; Dougherty, Mathias, Marsh, Moeller, & Swann, 2004; Maloney, Degenhardt, Darke, Mattick, & Nelson, 2007).
Research has found that 46% to 70% of all opioid users have experienced at least one non-fatal opioid overdose over their lifetime (Darke & Ross, 2001; Darke, Ross, & Hall, 1996; McGregor, Darke, Ali, & Christie, 1998; Rossow & Lauritzen, 1999; Vingoe, Welch, Farrell, & Strang, 1999; Warner-Smith, Darke, & Day, 2002). Although the majority of fatal opioid overdose cases are males, males and females have similar risk for non-fatal opioid overdose (Bennett & Higgins, 1999; Darke et al., 2006; Darke & Hall, 2003; McGregor et al., 1998).
Contrary to popular belief, non-fatal opioid overdoses have been found to be more common among older, more experienced users (Darke et al., 2006; Darke & Hall, 2003). Polydrug use has also been linked to opioid overdose, with central nervous system depressants, such as alcohol and benzodiazepines, commonly associated with non-fatal opioid overdose cases (Darke et al., 2006; Darke & Hall, 2003; Darke, Williamson, Ross, & Teesson, 2005; Warner-Smith, Darke, Lynskey, & Hall, 2001). Other risk factors found to be associated with non-fatal opioid overdose cases are injecting as the primary route of administration, and high risk periods, such as post release from prison (Darke et al., 2006; Darke & Hall, 2003; Farrell & Marsden, 2008; Seaman, Brettle, & Gore, 1998).
There is disagreement concerning the relationship between unintentional non-fatal opioid overdoses and suicide attempts. This disagreement relates firstly, to the extent to which the behaviours can be differentiated based on the observed risk factors, and secondly, the issue of whether research can assess the degree of suicidal intent expressed by opioid-dependent individuals (Cantor, McTaggart, & De Leo, 2001). Research has suggested that around 25% to 30% of opioid users report a history of both a suicide attempt and a non-fatal opioid overdose (Darke & Ross, 2001; Rossow & Lauritzen, 1999; Vingoe et al., 1999). Some studies have found an association between non-fatal opioid overdose and suicide attempts, and have concluded that they can be seen as risk markers for each other (Rossow & Lauritzen, 1999; Vingoe et al., 1999). Additionally, research does suggest that non-fatal overdoses and suicide attempts are predicted by different correlates (Ravndal & Vaglum, 1999). Frequent use of opioids and other opioid use patterns have been found to predict lifetime non-fatal overdose, whereas a diagnosis of borderline personality disorder (BPD) or depression, for example, have been found to predict lifetime suicide attempts (Darke & Hall, 2003; Ravndal & Vaglum, 1999).
A limited number of findings are also consistent with the argument that non-fatal opioid overdoses are not misclassified suicide attempts. Firstly, it has been noted that a high degree of seriousness is generally reported when the suicide attempts of opioid users are examined (Darke & Ross, 2001). Secondly, the finding that opioids are rarely chosen as a method for attempting suicide clearly distinguishes this behaviour from an accidental opioid overdose (Darke & Ross, 2001; Johnsson & Fridell, 1997; Vingoe et al., 1999). Thirdly, a number of studies have found that suicidal intent is not a contributing factor among opioid overdoses (Darke & Ross, 2001; Rossow & Lauritzen, 1999; Vingoe et al., 1999). This view has been disputed, however (Neale, 2000).
Despite the noted importance of assessing non-fatal opioid overdose, few studies have been conducted to carefully assess the issue of whether they are misclassified suicide attempts (Darke et al., 2006). Most studies have examined a few correlates for either suicide attempts or non-fatal opioid overdose, but not a comprehensive list. To our knowledge, only one study (Rossow & Lauritzen, 1999) has compared attempted suicide and non-fatal opioid overdose using mutually exclusive categories. Considering previous studies have demonstrated a substantial overlap exists between the two behaviours (Darke & Ross, 2001; Rossow & Lauritzen, 1999; Vingoe et al., 1999), it is important to also assess the characteristics associated with those who report a history of both behaviours.
This paper goes beyond previous work and compares multiple known correlates for non-fatal opioid overdoses and suicide attempts, including indicators of drug use, psychological disorder and childhood abuse. A comprehensive comparison is essential considering the morbidity, and future risk of mortality associated with both behaviours. This paper aims to determine if it is possible to differentiate correlates for non-fatal opioid overdose and suicide attempts. This aim was addressed by comparing those who reported an overdose only, those who reported a suicide attempt only, and those who reported a history of both behaviours, with those reporting no history of either behaviour.
The specific aims of this paper are:
To assess the reported prevalence of lifetime suicide attempts and non-fatal opioid overdose among a sample of opioid dependent individuals;
To examine the extent to which suicide attempts and opioid overdoses are related among this sample; and
To compare the correlates associated with attempted suicide and non-fatal opioid overdose.
2. Method
2.1 Procedure
This paper utilised data collected as part of an ongoing, large retrospective case-control study examining genetic and environmental factors (e.g. childhood trauma) contributing to opioid dependence liability. This paper only used data collected from the participants defined as “cases”. A full description of the methods used to obtain control participants has been published in a previous paper (Maloney et al., 2007). Cases were defined as such if they had participated in pharmacotherapy maintenance treatment for opioid dependence at some point in their lives. Additionally, they were required to have a good understanding of English and be aged over 18. Cases were recruited from both public and private opioid maintenance treatment clinics in New South Wales, Australia. Data reported here were collected from December 2004 to April 2008. The major demographic characteristics were identified as similar to the NSW sample of heroin users enrolled in the Australian Treatment Outcome Study (ATOS) (Ross et al., 2003). See page 9 for a full description of the demographic and mental health characteristics of the cases.
All interviews were conducted by trained interviewers with graduate and postgraduate qualifications in psychology or social sciences; and who have received comprehensive training in the administration of the structured diagnostic interview used in the study. All participants were guaranteed any information given to the researchers would be kept strictly confidential as part of the consent protocol that was approved by the institutional review boards of University of New South Wales, Washington University, Queensland Institute of Medical Research and, for cases, the Ethics Committee responsible for oversight of research at their opioid maintenance treatment clinic. Participants were reimbursed $50 for out-of-pocket expenses.
2.2 Structured Interview
Researchers administered a structured interview to all participants containing sixteen sections. DSM-IV lifetime diagnoses of substance use disorders (dependence of cannabis, sedatives, opioids, stimulants, cocaine, nicotine and alcohol), DSM-IV diagnosis of PTSD, major depressive episode, anti-social personality disorder (ASPD), and panic disorder were obtained using sections adopted and modified from the Collaborative Study on the Genetics of Alcoholism (COGA) Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA-II) (Bucholz et al., 1994; Hesselbrock, Easton, Bucholz, Schuckit, & Hesselbrock, 1999).
The questions assessing non-fatal opioid overdose were included in the section assessing opioid dependence as described above. Consistent with previous research (Warner-Smith et al., 2001), a non-fatal opioid overdose was defined as an event where loss of consciousness and respiratory depression occurs that does not result in a fatal outcome. Similarly, consistent with the literature, attempted suicide was defined as “deliberate self-harm with the intent of causing death”, which does not result in a fatal outcome (Darke et al., 2004). This section on attempted suicide was adapted from the COGA SSAGA-II (Bucholz et al., 1994; Hesselbrock et al., 1999) with additional questions included to assess suicidal intent and seriousness. Both non-fatal opioid overdoses and suicide attempts were assessed as lifetime events.
The BPD screener was adapted from the International Personality Disorder Examination (IPDE) for use in the Australian National Survey of Mental Health and Wellbeing using the ICD-10 criteria (Jackson & Burgess, 2000; Loranger et al., 1994; World Health Organization, 1993). Sections adapted from the Christchurch Trauma Assessment, used in the Christchurch Health and Development Study (Fergusson, Horwood, & Woodward, 2000) elicited information related to childhood physical and sexual abuse. Two separate binary variables were used and each was endorsed if the participant reported any childhood physical abuse, or any childhood sexual abuse.
Participants also completed the Barratt Impulsiveness Scale version 11 (BIS-11). The BIS is the most frequently used self report measure of impulsivity (Dougherty et al., 2004), and has been found to be valid and reliable in a number of different languages (Moeller et al., 2002; Patton, Stanford, & Barratt, 1995). In order to make the scale more clinically useful the 75th percentile total BIS score for the sample was used as a cut off to differentiate between high impulsivity and low impulsivity (Doran, Spring, McChargue, Pergadia, & Richmond, 2004). Although no established cut offs exist for the BIS-11, other studies have suggested the use of the 75th percentile score (Baca-Garcia et al., 2004).
2.3 Statistical Analysis
A multinomial logistic regression was performed, with odds ratios and 95% confidence intervals reported. The reference category used was no history of either behaviour. This allowed a comparison between those who reported an overdose only, those who reported a suicide attempt only, and those who reported a history of both behaviours. The following variables were used in the regression analysis: age, gender, lifetime alcohol dependence, lifetime sedative dependence, lifetime psycho-stimulant dependence (cocaine or stimulants), lifetime major depressive episode, BPD, lifetime anxiety disorder (PTSD or panic disorder), route of administration (ever injected opioids), longest period of daily opioid use, any childhood abuse (sexual or physical), high impulsivity. All statistical analyses were conducted using SPSS for Windows, version 14.0 (SPSS Inc, 2005).
3. Results
3.1 Sample characteristics
The sample consisted of 1500 opioid-dependent persons. The majority of the sample were male (60%). The male cases were significantly older than the female cases (37.2 versus 35.3, p<0.001, t1516=4.23) and were more likely to report a prison history (66% versus 40%, OR 2.95, 95% CI 2.38–3.65). Males and females were equally likely to report being unemployed at the time of the interview (82% for males, 84% for females), and to report completing only 10 years of education or less (71% for males, 70% for females).
When lifetime drug dependence was examined, males were identified as significantly more likely to report dependence on alcohol (43% versus 35%, OR 1.42, 95% CI 1.15–1.76), stimulants (52% versus 46%, OR 1.29, 95% CI 1.05–1.59) and cannabis (58% versus 52%, OR 1.26, 95% CI 1.03–1.55). No gender differences were identified for a lifetime dependence on sedatives (35% for males, 38% for females) or cocaine (33% for males, 31% for females). Additionally, males reported more lifetime substance dependence diagnoses than females (not including tobacco and opioid dependence) (mean 2.19 versus 1.95, p<0.05, t1336=2.51).
Females were significantly more likely than males to experience a depressive episode over their lifetime (69% versus 54%, OR 1.88, 95% CI 1.52–2.34), report the experience of childhood sexual abuse (70% versus 30%, OR 5.52, 95% CI 4.40–6.93), be classed as highly impulsive (36% versus 31%, OR 1.00–1.60), and to meet criteria for lifetime PTSD (50% versus 31%, OR 2.23, 95% CI 1.80–2.76), BPD (64% versus 55%, OR 1.48, 95% CI 1.20–1.82) and panic disorder (31% versus 20%, OR 1.82, 95% CI 1.43–2.31). Males were significantly more likely than females to be diagnosed with antisocial personality disorder (ASPD) (51% versus 38%, OR 1.71, 95% CI 1.39–2.11). There were no gender differences among those who reported the experience of childhood physical abuse (61% for males, 59% for females) or among those who reported a history of injecting opioids (97% for males, 95% for females).
3.2 Occurrence of non-fatal opioid overdose and attempted suicide
Non-fatal opioid overdoses were more common than suicide attempts (58% vs. 32%). Of those who reported an overdose, the majority (79%) reported that they had required some form of medical assistance. Multiple unintentional non-fatal opioid overdoses and multiple suicide attempts were experienced by around a quarter of participants (24% vs. 20%, respectively).
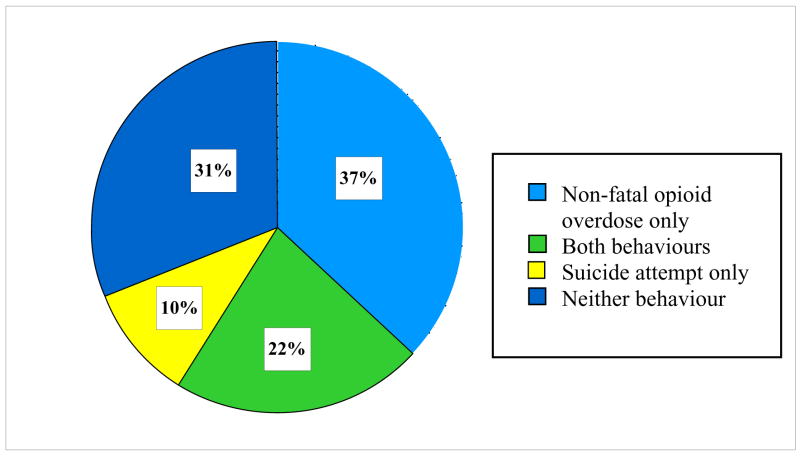
There was considerable overlap between the proportion reporting a non-fatal opioid overdose and the proportion reporting a suicide attempt, with 22% of the sample reporting a history of both behaviours (Figure 1). Sixty-seven percent of those who reported a suicide attempt history also reported an overdose, and 37% of those who reported an overdose history also reported a suicide attempt.
Figure 1.
Occurrence of non-fatal overdose or attempted suicide
3.3 Characteristics associated with a history of non-fatal overdose or attempted suicide
Table 1 compares the prevalence and associated risk for the demographic, substance use and mental health characteristics for each group – i.e. those who reported either a non-fatal overdose or a suicide attempt or both were compared to those who reported no history of either behaviour. The cases who reported a history of a non-fatal overdose only (compared to those who did not experience either behaviour) were more likely to report substance use disorders predominately (including lifetime sedative, psychostimulant and alcohol dependence) and a history of injecting opioids (Table 1). Whereas the cases who reported a history of attempted suicide only (compared to those who did not experience either behaviour) were more likely to be female, report the experience of childhood abuse and report a history of a range of mental health disorders (including an episode of depression, anxiety and BPD) (Table 1). The clinical picture of the cases who reported a history of both behaviours was more severe compared to those who did not experience either behaviour. These individuals were more likely to be female, to report the experience of childhood abuse, to be defined as highly impulsive, to have a history of injecting opioids, and to report each substance use and mental health disorder examined (Table 1).
Table 1.
Characteristics of the sample by non-fatal overdose or suicide attempt history
| Neither behaviour (n=465) |
Non-fatal overdose only (n=552) |
OR1 (95% CI) |
Suicide attempt only (n=162) |
OR1 (95% CI) |
Both behaviours (n=321) |
OR1 (95% CI) |
|
|---|---|---|---|---|---|---|---|
|
Demographics | |||||||
| % Female | 37 | 33 | not significant | 55 | 2.04 (1.42–2.93)** | 48 | * 1.54 (1.16–2.06) |
| Age (mean) | 35.5 (SD 8.6) | 37.7 (SD 8.5) | 1.03 (1.02–1.05)** | 34.1 (SD 7.9) | not significant | 36.7 (SD 8.5) | not significant |
| % Unemployed | 83 | 82 | not significant | 81 | not significant | 84 | not significant |
|
| |||||||
|
Drug dependence | |||||||
| % Cannabis | 49 | 54 | not significant | 65 | 1.97 (1.36–2.85)** | 62 | 1.72 (1.29–2.29)** |
| % Sedative | 26 | 35 | 1.57 (1.20–2.07)** | 36 | 1.67 (1.14–2.44)* | 52 | 3.19 (2.36–4.31)** |
| % Psycho-stimulants (cocaine or stimulants) | 53 | 64 | 1.56 (1.22–2.01)** | 64 | 1.58 (1.09–2.29)* | 78 | 3.05 (2.22–4.20)** |
| % Alcohol | 31 | 40 | 1.47 (1.13–1.91)* | 38 | not significant | 53 | 2.45 (1.83–3.29)** |
|
| |||||||
|
Psychopathology | |||||||
| % Depressive episode | 52 | 50 | not significant | 77 | 3.06 (2.03–4.61)** | 78 | 3.22 (2.34–4.42)** |
| % Anxiety disorder (PTSD or panic disorder) | 39 | 43 | not significant | 69 | 3.44 (2.34–5.05)** | 64 | 2.83 (2.12–3.80)** |
| % Screening for BPD | 47 | 52 | not significant | 72 | 2.92 (1.98–4.31)** | 79 | 4.26 (3.08–5.88)** |
| % High impulsivity | 24 | 32 | 1.55 (1.15–2.09)* | 40 | 2.16 (1.44–3.24)** | 44 | 2.51 (1.81–3.48)** |
| % Any childhood abuse (physical or sexual) | 64 | 68 | not significant | 84 | 3.00 (1.90–4.76)** | 90 | 5.15 (3.41–7.75)** |
| % Ever injected opioids | 92 | 99 | 11.90 (4.18–33.33)** | 92 | not significant | 98 | 4.55 (1.89–10.87)** |
Reference group is ‘Neither behaviour’
p<0.05
p<0.001
Table 1 suggests that it wasn’t such that these correlates were simply related to both behaviours, but that the cases that reported both behaviours also experienced most of the drug use, mental health and the problematic childhood characteristics at much higher rates than those who did not report either behaviour.
3.4 Multivariate correlates of non-fatal opioid overdose and attempted suicide
The results from the multinomial logistic regression confirmed the pattern identified above and suggested that the correlates of non-fatal opioid overdose only and suicide attempts only did differ (Table 2). The correlates of a non-fatal opioid overdose only were age, ever having injected opioids, high impulsivity and a lifetime diagnosis of sedative dependence (Table 2). Screening positively for BPD, experiencing a depressive episode, a lifetime diagnosis of an anxiety disorder, and being female were identified as correlates for suicide attempts only (Table 2). Overall the correlates of non-fatal opioid overdose only were related to drug use behaviours, age (older) and high impulsivity, whereas the correlates of suicide attempts only were related to a range of psychological disorders and being female.
Table 2.
Multivariate correlates of non-fatal overdose and suicide attempt history
| Non-fatal overdose only (n=480) a | Suicide attempt only (n=138) a | Both behaviours (n=278) a | |
|---|---|---|---|
| OR (95% CI) b | |||
| Age | OR 1.03 (1.01–1.04) * | not significant | not significant |
| Route of administration (ever injected opioids) | OR 6.45 (2.22–18.87) ** | not significant | OR 4.37 (1.23–15.63)* |
| High impulsivity | OR 1.43 (1.03–1.98) * | not significant | not significant |
| Lifetime sedative dependence | OR 1.52 (1.11–2.07) * | not significant | OR 2.07 (1.45–2.96)** |
| Major depressive episode | not significant | OR 1.98 (1.23–3.21) * | OR 1.71 (1.17–2.51)* |
| Gender (female) | not significant | OR 1.52 (1.01–2.35)* | not significant |
| Screening positive for BPD | not significant | OR 1.82 (1.13–2.94)* | OR 2.29 (1.55–3.34)** |
| Lifetime anxiety disorder (PTSD or panic disorder) | not significant | OR 1.62 (1.04–2.53) * | OR 1.48 (1.04–2.12)* |
| Any childhood abuse (physical or sexual) | not significant | not significant | OR 2.23 (1.39–3.57)** |
| Longest period daily opioid use (in years) | not significant | not significant | OR 1.04 (1.00–1.07)* |
| Lifetime psycho-stimulant dependence (cocaine or stimulants) | not significant | not significant | OR 1.52 (1.03–2.23)* |
p<0.05
p<0.001
Reference category: no history of a non-fatal opioid overdose or a suicide attempt
OR from multiple logistic regression including all variables listed here: age, gender, alcohol dependence, sedative dependence, psycho-stimulant dependence (cocaine or stimulants), major depressive episode, BPD, an anxiety disorder (PTSD or panic disorder), route of administration (ever injected opioids), longest period of daily opioid use, childhood maltreatment (sexual or physical abuse), high impulsivity.
When the characteristics of those who reported a history of both non-fatal overdose and attempted suicide were examined, a more complex clinical profile was apparent (Table 2). Those who reported a history of both behaviours were more likely to report multiple drug use disorders (lifetime sedative dependence, lifetime psycho-stimulant dependence, a longer history of daily opioid use) and to report a more complex history of mental health problems (major depressive episode, screening positively for BPD, lifetime anxiety disorder). Additionally, this group were more likely to report the experience of childhood abuse, and a history of injecting opioids (Table 2).
4. Discussion
Suicide attempts and non-fatal opioid overdose have been examined among opioid-dependent individuals in a number of different studies, with some disagreement on whether they are distinct behaviours. These studies however, rarely include an exhaustive list of correlates associated with either behaviour. Additionally, only one study has compared the two behaviours using mutually exclusive categories (Rossow & Lauritzen, 1999). Overall, the present study found distinct correlates for suicide attempts and non-fatal opioid overdose.
The correlates identified for non-fatal opioid overdose were consistent with the literature. Older, more experienced heroin users were identified as more at risk of opioid overdose (Darke & Hall, 2003; Gossop, Griffiths, Powis, Williamson, & Strang, 1996). Additionally, injecting opioids (as opposed to using other routes of administration) was associated with increased overdose risk (Bennett & Higgins, 1999; Darke & Hall, 2003; Gossop, Stewart, Treacy, & Marsden, 2002; Stewart, Gossop, & Marsden, 2002).
High impulsivity was also identified as a unique risk factor for non-fatal opioid overdose. The research supporting this finding, however, is limited. In fact more research actually supports a relationship between impulsivity and suicide attempts (Dougherty et al., 2004), which was not identified in this study. It is possible that this discrepancy relates to the type and nature of impulsivity assessed in the current study. The BIS is a self-report measure and as such typically measures lifelong “trait” aspects of impulsivity which generally do not take into account any “state-dependent” fluctuations in impulsivity (include experiencing stress, loss or anxiety), which may lead to attempted suicide (Fawcett, 2001; Moeller, Barratt, Dougherty, Schmitz, & Swann, 2001). Additionally, individuals with impulsive personality traits tend to seek immediate rewards (Kirby, Petry, & Bickel, 1999). Polydrug use or drug use immediately post release from prison could be considered to be impulsive behaviours, and have both been identified as correlates for non-fatal opioid overdose among other studies (Darke & Hall, 2003). Considering this, it is not surprising that high impulsivity was identified as a unique risk factor for non-fatal opioid overdose in this study.
Sedative dependence was also identified as a risk factor for non-fatal opioid overdose. Studies have consistently found that both fatal and non-fatal opioid overdoses often occur with the consumption of other drugs, particularly benzodiazepines and alcohol (Gossop et al., 2002; White & Irvine, 1999). Sedatives appear to be a proximal risk factor for non-fatal overdose as they act as a central nervous system depressant, similarly to opioids (Darke et al., 2006). Additionally, studies have identified polydrug dependence as a marker for comorbid psychiatric diagnoses (Darke & Ross, 1997). It was not possible, however, in this study to determine if the indexed overdose occurred in conjunction with drugs other than opioids.
In agreement with the findings of other studies, it seems that it is possible to differentiate between attempted suicide and non-fatal opioid overdose (Ravndal & Vaglum, 1999). Depression, anxiety disorders, and personality disorders were associated with suicide attempts, whereas drug use variables were associated with non-fatal opioid overdose such as injecting opioids and sedative dependence. A previously published paper on this sample found that the use of opioids (particularly heroin) to attempt suicide is atypical among opioid users (Maloney et al., 2007), which is consistent with the literature (Darke & Ross, 2001; Johnsson & Fridell, 1997; Vingoe et al., 1999). In fact, as mentioned previously, the most commonly reported method for attempting suicide among opioid users is an overdose on benzodiazepines (Darke & Ross, 2001; Maloney et al., 2007). These findings highlight that reported suicide attempts are not misclassified opioid overdoses. We also found that opioid-dependent individuals who reported a lifetime suicide attempt reported high levels of suicidal intent on each measure used. Taken together, these results strengthen the conclusion that opioid-dependent individuals have the capacity to differentiate and report separately on the two behaviours (Maloney et al., 2007). Additionally, a considerable proportion of the sample reported both behaviours, which is consistent with previous research (Darke & Ross, 2001; Rossow & Lauritzen, 1999; Vingoe et al., 1999). This suggests that although they may be distinct behaviours, they may not apply to separate sub-groups of opioid-dependent individuals.
A number of correlates for suicide attempts were identified among this sample. Consistent with previous research, experiencing a major depressive episode, being female and screening BPD+ were identified as being associated with a history of suicide attempts (Darke & Ross, 2001; Darke et al., 2004; Murphy et al., 1983; Roy, 2002). Meeting criteria for an anxiety disorder (either PTSD or panic disorder) was also associated with a history of attempted suicide only. Although research has linked PTSD and attempted suicide among the general population (Sareen, Houlahan, Cox, & Asmundson, 2005), and among opioid dependent individuals (Darke et al., 2004), the literature examining panic disorder as a risk factor for suicide attempts among opioid-dependent individuals is limited. Studies among the general population have found that panic disorder increases an individual’s risk of attempting suicide (Pilowsky, Wu, & Anthony, 1999; Pirkis, Burgess, & Dunt, 2000; Schmidt, Woolaway-Bickel, & Bates, 2001). Considering the findings of this study, research should address how the findings of previous research may translate to opioid-dependent individuals.
This study also found that participants with a history of both non-fatal overdose and attempted suicide were characterised by a more complex clinical profile, which included drug use behaviours, psychological problems, and a history of childhood trauma. Although the literature in this area is limited, these findings are consistent with an international study (Rossow & Lauritzen, 1999). The findings suggest that if a client presenting for treatment discloses a history of both self-destructive behaviours a thorough assessment should be conducted as an underlying comorbid problem could complicate clinical care. To decrease the risk of subsequent non-fatal overdose and suicide attempt events any identified comorbid problems should be dealt with concurrently in conjunction with opioid dependence. Additionally, the identification of a third dual diagnosis group of individuals highlights an important theoretical and conceptual issue for future studies to be aware of. The results suggest that if these groups are not assessed as mutually exclusive categories and the characteristics of this third dual diagnosis group are ignored the findings will be limited.
Non-fatal overdoses and suicide attempts seem to be distinct problems requiring different prevention strategies. For suicide attempts the clinical implications appear to focus on addressing and treating underlying psychological conditions, whereas for non-fatal opioid overdose harm minimisation strategies appear to be paramount to decreasing the associated risk. The findings suggest that individuals seeking treatment for psychological disorders should be primarily assessed for suicidal risk. Alternatively, the findings suggest that those who inject opioids are at an increased risk of overdose; consequently treatment could be focused on educating individuals on how to manage overdose situations, as well as focusing education campaigns on safer injecting practices. Sedative dependence was associated with non-fatal opioid overdose, and polydrug use has been found to be highly prevalent among opioid users (Darke, Ross, & Hall, 1995). Considering this, a component of treatment could also be to educate opioid users on which combinations of drugs increase an individual’s risk of overdose. Additionally, treatment could focus on addressing and stabilising impulsivity levels, as well as teaching individuals to recognise high risk impulsive situations.
A number of limitations exist in the current study. It is unclear if our results are generalisable to other populations of opioid-dependent individuals who have never received methadone maintenance treatment. Our results are, however, comparable with a number of other studies (Ravndal & Vaglum, 1999; Vingoe et al., 1999). It is also possible that we may have failed to measure the contribution of other non-assessed correlates. Additionally, it is not possible to generalise the findings of this study to fatal overdose and suicide cases.
The study relies on self-report data and an amount of recall bias is introduced when assessing lifetime prevalence. These measures are commonly used in studies on illicit drug users, however, and have been shown to be adequately valid and reliable (Darke, 1998; Dougherty et al., 2004). The study was also reliant on the respondents’ determination of suicidal vs. non-suicidal behaviour. This limitation was minimised, however, by the use of standard definitions and the inclusion of questions which assess suicidal intent. There is also the potential that under-reporting existed in this study if the overdose did not result in complete respiratory arrest and occurred among an opioid user who was injecting alone.
Despite these limitations, this study has improved on previous work conducted by comparing multiple known correlates for non-fatal overdose and suicide attempts using mutually exclusive categories. This type of analysis was particularly important considering the substantial overlap which was found to exist between the groups.
5. Conclusions
Non-fatal opioid overdose and attempted suicide were highly prevalent among this sample of opioid-dependent individuals. The two behaviours had distinct correlates. Non-fatal overdose and suicide attempts are nonetheless related behaviours, and individuals with a history of both behaviours presented with a more complex clinical profile. Prevention of non-fatal overdose and attempted suicide is important to decrease the risk of subsequent mortality. Addressing underlying psychological conditions appears to be important for attempted suicide, whereas employing harm minimisation strategies appears to be important for non-fatal opioid overdose.
Acknowledgments
This study was funded by the National Institute of Drug Abuse (DA 17305). Professor Louisa Degenhardt is the recipient of an Australian National Health and Medical Research Council (NH&MRC) Senior Research Fellowship (#510279). The study was a multi-site study involving teams from the National Drug and Alcohol Research Centre, Queensland Institute of Medical Research, Washington University and Prince of Wales Hospital. The National Drug and Alcohol Research Centre is funded by the Australian Government Department of Health and Ageing. Special thanks to Fiona Shand, Elizabeth Conroy, Michelle Torok, Caitlin McCue, Cherie Kam. The authors would like to thank all those persons involved from the collaborating centres for their contribution to the study. We would also like to thank the staff from the treatment centres and agencies involved in the project for their support, and the many participants for their time and willingness to share their experiences.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Baca-Garcia E, Vaquero C, Diaz-Sastre C, Garcia-Resa E, Saiz-Ruiz J, Fernandez-Piqueras J, et al. Lack of association between the serotonin transporter promoter gene polymorphism and impulsivity or aggressive behaviour among suicide attempters and healthy volunteers. Psychiatry Research. 2004;126:99–106. doi: 10.1016/j.psychres.2003.10.007. [DOI] [PubMed] [Google Scholar]
- Bennett GA, Higgins DS. Accidental overdose among injecting drug users in Dorset, UK. Addiction. 1999;94(8):1179–1190. doi: 10.1046/j.1360-0443.1999.94811798.x. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Cadoret R, Cloninger RC, Dinwiddie SH, Hesselbrock VM, Nurnberger JI, et al. A new, semi-structured psychiatric interview for use in genetic linkage studies: A report on the reliability of SSAGA. Journal of Studies on Alcohol. 1994;55:149–158. doi: 10.15288/jsa.1994.55.149. [DOI] [PubMed] [Google Scholar]
- Cantor C, McTaggart P, De Leo D. Misclassification of suicide - The contribution of opiates. Psychopathology. 2001;34(3):140–146. doi: 10.1159/000049297. [DOI] [PubMed] [Google Scholar]
- Darke S. Self-report among injecting drug users: A review. Drug and Alcohol Dependence. 1998;51:253–263. doi: 10.1016/s0376-8716(98)00028-3. [DOI] [PubMed] [Google Scholar]
- Darke S, Degenhardt L, Mattick R. Mortality among illicit drug users: Epidemiology, causes and intervention. Cambridge: Cambridge University Press; 2006. [Google Scholar]
- Darke S, Hall W. Heroin overdose: research and evidence-based intervention. Journal of Urban Health. 2003;80(2):189–200. doi: 10.1093/jurban/jtg022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darke S, Ross J. Polydrug dependence and psychiatric comorbidity among heroin injectors. Drug and Alcohol Dependence. 1997;48:135–141. doi: 10.1016/s0376-8716(97)00117-8. [DOI] [PubMed] [Google Scholar]
- Darke S, Ross J. The relationship between suicide and heroin overdose among methadone maintenance patients in Sydney, Australia. Addiction. 2001;96:1443–1453. doi: 10.1046/j.1360-0443.2001.961014438.x. [DOI] [PubMed] [Google Scholar]
- Darke S, Ross J. Suicide among heroin users: Rates, risk factors and methods. Addiction. 2002;97:1383–1394. doi: 10.1046/j.1360-0443.2002.00214.x. [DOI] [PubMed] [Google Scholar]
- Darke S, Ross J, Hall W. Overdose among heroin users in Sydney Australia: I. Prevalence and correlates of non-fatal overdose. Addiction. 1996;91(3):405–411. [PubMed] [Google Scholar]
- Darke S, Ross J, Lynskey MT, Teesson M. Attempted suicide among entrants to three treatment modalities for heroin dependence in the Australian Treatment Outcome Study (ATOS): Prevalence and risk factors. Drug and Alcohol Dependence. 2004;73:1–10. doi: 10.1016/j.drugalcdep.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Darke S, Williamson A, Ross J, Teesson M. Non-fatal heroin overdose, treatment exposure and client characteristics: Findings from the Australian Treatment Outcome Study (ATOS) Drug and Alcohol Review. 2005;24:425–432. doi: 10.1080/09595230500286005. [DOI] [PubMed] [Google Scholar]
- Darke SG, Ross JE, Hall WD. Benzodiazepine use among injecting heroin users. Medical Journal of Australia. 1995;162:645–647. doi: 10.5694/j.1326-5377.1995.tb126051.x. [DOI] [PubMed] [Google Scholar]
- Doran N, Spring B, McChargue D, Pergadia M, Richmond M. Impulsivity and smoking relapse. Nicotine and Tobacco Research. 2004;6(4):641–647. doi: 10.1080/14622200410001727939. [DOI] [PubMed] [Google Scholar]
- Dougherty DM, Mathias CW, Marsh DM, Moeller GF, Swann AC. Suicidal behaviors and drug abuse: impulsivity and its assessment. Drug and Alcohol Dependence. 2004;76(Supplement 1):s93–s105. doi: 10.1016/j.drugalcdep.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Farrell M, Marsden J. Acute risk of drug-related death among newly released prisoners in England and Wales. Addiction. 2008;103(2):251–255. doi: 10.1111/j.1360-0443.2007.02081.x. [DOI] [PubMed] [Google Scholar]
- Fawcett J. Treating impulsivity and anxiety in the suicidal patient. Annals of the New York Academy of Sciences. 2001;932:94–105. doi: 10.1111/j.1749-6632.2001.tb05800.x. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Woodward LJ. The stability of child abuse reports: A longitudinal study of the reporting behaviour of young adults. Psychological Medicine. 2000;30(3):529–544. doi: 10.1017/s0033291799002111. [DOI] [PubMed] [Google Scholar]
- Gossop M, Griffiths P, Powis B, Williamson S, Strang J. Frequency of non-fatal heroin overdose: survey of heroin users recruited in non-clinical settings. British Medical Journal. 1996;313(7054):402(401). doi: 10.1136/bmj.313.7054.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gossop M, Stewart D, Treacy S, Marsden J. A prospective study of mortality among drug misusers during a 4-year period after seeking treatment. Addiction. 2002;97:39–47. doi: 10.1046/j.1360-0443.2002.00079.x. [DOI] [PubMed] [Google Scholar]
- Hesselbrock M, Easton C, Bucholz KK, Schuckit M, Hesselbrock V. A validity study of the SSAGA - a comparison with the SCAN. Addiction. 1999;94(9):1361–1370. doi: 10.1046/j.1360-0443.1999.94913618.x. [DOI] [PubMed] [Google Scholar]
- Hulse GK, English DR, Milne E, Holman CDJ. The quantification of mortality resulting from the regular use of illicit opiates. Addiction. 1999;94(2):221–229. doi: 10.1046/j.1360-0443.1999.9422216.x. [DOI] [PubMed] [Google Scholar]
- Jackson HJ, Burgess PM. Personality disorders in the community: A report from the Australian National Survey of Mental Health and Wellbeing. Social Psychiatry and Psychiatic Epidemiology. 2000;35:531–538. doi: 10.1007/s001270050276. [DOI] [PubMed] [Google Scholar]
- Johnsson E, Fridell M. Suicide attempts in a cohort of drug abusers: A 5-year follow-up study. Acta Psychiatrica Scandinavica. 1997;96:362–366. doi: 10.1111/j.1600-0447.1997.tb09930.x. [DOI] [PubMed] [Google Scholar]
- Kirby KN, Petry NM, Bickel WK. Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. Journal of Experimental Psychology: General. 1999;128(1):78–87. doi: 10.1037//0096-3445.128.1.78. [DOI] [PubMed] [Google Scholar]
- Loranger AW, Sartorius N, Andreoli A, Berger P, Buchheim P, Channabasavanna SM, et al. The International Personality Disorder Examination: The World Health Organization/Alcohol, Drug Abuse, and Mental Health Administration International Pilot Study of Personality Disorders. Archives of General Psychiatry. 1994;51(3):215–224. doi: 10.1001/archpsyc.1994.03950030051005. [DOI] [PubMed] [Google Scholar]
- Maloney E, Degenhardt L, Darke S, Mattick RP, Nelson EC. Suicidal behaviour and associated risk factors among opioid dependent persons: A case-control study. Addiction. 2007;102:1933–1941. doi: 10.1111/j.1360-0443.2007.01971.x. [DOI] [PubMed] [Google Scholar]
- McGregor C, Darke S, Ali R, Christie P. Experience of non-fatal overdose among heroin users in Adelaide, Australia: circumstances and risk perceptions. Addiction. 1998;93(5):701–711. doi: 10.1046/j.1360-0443.1998.9357016.x. [DOI] [PubMed] [Google Scholar]
- Moeller GF, Barratt ES, Dougherty DM, Schmitz JM, Swann AC. Psychiatric aspects of impulsivity. American Journal of Psychiatry. 2001;158(11):1783–1793. doi: 10.1176/appi.ajp.158.11.1783. [DOI] [PubMed] [Google Scholar]
- Moeller GF, Dougherty DM, Barratt ES, Oderinde V, Mathias CW, Harper AR, et al. Increased impulsivity in cocaine dependent subjects independent of antisocial personality disorder and aggression. Drug and Alcohol Dependence. 2002;68:105–111. doi: 10.1016/s0376-8716(02)00106-0. [DOI] [PubMed] [Google Scholar]
- Murphy SL, Rounsaville BJ, Eyre S, Kleber HD. Suicide attempts in treated opiate addicts. Comprehensive Psychiatry. 1983;24(1):79–89. doi: 10.1016/0010-440x(83)90053-6. [DOI] [PubMed] [Google Scholar]
- Neale J. Suicidal intent in non-fatal illicit drug overdose. Addiction. 2000;95(1):85–93. doi: 10.1046/j.1360-0443.2000.951859.x. [DOI] [PubMed] [Google Scholar]
- Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt Impulsiveness Scale. Journal of Clinical Psychology. 1995;51(6):768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Pilowsky DJ, Wu L, Anthony JC. Panic attacks and suicide attempts in mid-adolescence. American Journal of Psychiatry. 1999;156(10):1545–1549. doi: 10.1176/ajp.156.10.1545. [DOI] [PubMed] [Google Scholar]
- Pirkis J, Burgess P, Dunt D. Suicidal ideation and suicide attempts among Australian adults. Crisis. 2000;21(1):16–24. doi: 10.1027//0227-5910.21.1.16. [DOI] [PubMed] [Google Scholar]
- Ravndal E, Vaglum P. Overdoses and suicide attempts: Different relations to psychopathology and substance abuse? A 5-year prospective study of drug abusers. European Addiction Research. 1999;5:63–70. doi: 10.1159/000018967. [DOI] [PubMed] [Google Scholar]
- Ross J, Teesson M, Darke S, Lynskey M, Hetherington K, Mills K, et al. Characteristics of heroin users entering three treatment modalities in New South Wales: Baseline findings from the Australian Treatment Outcome Study (ATOS) (No. Technical Report No.139) Sydney: National Drug and Alcohol Research Centre, University of New South Wales; 2003. [Google Scholar]
- Rossow I, Lauritzen G. Balancing on the edge of death: suicide attempts and life-threatening overdoses among drug addicts. Addiction. 1999;94(2):209–219. doi: 10.1046/j.1360-0443.1999.9422095.x. [DOI] [PubMed] [Google Scholar]
- Roy A. Characteristics of opiate dependent patients who attempt suicide. Journal of Clinical Psychiatry. 2002;63(5):403–407. doi: 10.4088/jcp.v63n0505. [DOI] [PubMed] [Google Scholar]
- Sareen J, Houlahan T, Cox BJ, Asmundson GJG. Anxiety disorders associated with suicidal ideation and suicide attempts in the National Comorbidity Survey. The Journal of Nervous and Mental Disease. 2005;193(7):450–454. doi: 10.1097/01.nmd.0000168263.89652.6b. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Woolaway-Bickel K, Bates M. Evaluating panic-specific factors in the relationship between suicide and panic disorder. Behaviour Research and Therapy. 2001;39:635–649. doi: 10.1016/s0005-7967(00)00034-6. [DOI] [PubMed] [Google Scholar]
- Seaman SR, Brettle RP, Gore SM. Mortality from overdose among injecting drug users recently released from prison: database linkage study. British Medical Journal. 1998;316:426–428. doi: 10.1136/bmj.316.7129.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SPSS Inc. SPSS for Windows, version 14.0. Chicago: SPSS Inc; 2005. [Google Scholar]
- Stewart D, Gossop M, Marsden J. Reductions in non-fatal overdose after drug misuse treatment: results from the National Treatment Research Study (NTORS) Journal of Substance Abuse Treatment. 2002;22:1–9. doi: 10.1016/s0740-5472(01)00206-9. [DOI] [PubMed] [Google Scholar]
- Vingoe L, Welch S, Farrell M, Strang J. Heroin overdose among a treatment sample of injecting drug misusers: Accident or suicidal behaviour? Journal of Substance Use. 1999;4:88–91. [Google Scholar]
- Warner-Smith M, Darke S, Day C. Morbidity associated with non-fatal heroin overdose. Addiction. 2002;97:963–967. doi: 10.1046/j.1360-0443.2002.00132.x. [DOI] [PubMed] [Google Scholar]
- Warner-Smith M, Darke S, Lynskey M, Hall W. Heroin overdose: causes and consequences. Addiction. 2001;96:1113–1125. doi: 10.1046/j.1360-0443.2001.96811135.x. [DOI] [PubMed] [Google Scholar]
- White JM, Irvine RJ. Mechanisms of fatal opioid overdose. Addiction. 1999;94(7):961–972. [PubMed] [Google Scholar]
- World Health Organization. The International Classification of Diseases, version 10 (ICD-10) Geneva: World Health Organization; 1993. [Google Scholar]