Abstract
Objectives
To determine the level of demand and supply of out of hours care from a nationally representative sample of general practice cooperatives.
Design
Observational study based on routinely collected data on telephone calls, patient population data from general practices, and information about cooperatives from interviews with managers.
Setting
20 cooperatives in England and Scotland selected after stratification by region and by size.
Subjects
899 657 out of hours telephone calls over 12 months.
Main outcome measures
Numbers and age and sex specific rates of calls; variation in demand and activity in relation to characteristics of the population; timing of calls; proportion of patients consulting at home, at a primary care centre, or on the telephone; response times; hospital admission rates.
Results
The out of hours call rate (excluding bank holidays) was 159 calls per 1000 patients/year, with rates in children aged under 5 years four times higher than for adults. Little variation occurred by day of the week or seasonally. Cooperatives in Scotland experienced higher demand than those in England. Patients living in deprived areas made 70% more calls than those in non-deprived areas, but this had little effect on the overall variation in demand. 45.4% (408 407) of calls were handled by telephone advice, 23.6% (212 550) by a home visit, and 29.8% (267 663) at a centre. Cooperatives responded to 60% of calls within 30 minutes and to 83% within one hour. Hospital admission followed 5.5% (30 743/554 179) of out of hours calls (8 admissions per 1000 patients/year).
Conclusions
This project provides national baseline data for the planning of services and the analysis of future changes.
Introduction
The provision of care by general practitioners outside normal surgery hours has been revolutionised in the United Kingdom in recent years, and this process will continue with the expansion of the telephone helpline NHS Direct to cover the whole of Great Britain.1 No reliable national information exists, however, about the demand for out of hours care. Previous data come mainly from studies of deputising services,2,3 which underestimate demand because many general practitioners only use them at certain times,4 or from individual practices,5–8 which may not be representative. Many studies have been based on rates of claims for night visit fees,9–12 but only a small proportion of out of hours telephone calls are made at night and many out of hours calls are dealt with on the telephone and do not result in visits.13 Studies that have included telephone consultations have been local and small scale, 6,8,14–17 and underrecording of calls has been a further problem.18 Previous research has shown wide variation in demand, but it is difficult to compare work carried out in different years, different areas, and using different methodologies.
The growth of general practice cooperatives offers an opportunity to address these difficulties, as cooperatives provide out of hours care throughout the United Kingdom, and many record all calls electronically. Several evaluations of individual cooperatives have been published, showing considerable variation in their activity.16,19,20 Little information has been available about the population covered by these cooperatives, preventing an investigation of how the variation in response relates to local demand.
A better understanding of the demand for out of hours care is important in order to plan services, particularly NHS Direct. As demand for health care is related to supply, accurate baseline information is essential to measure the effects of continuing change in organisation. Information about the supply of care by representative cooperatives, and how this varies in different settings, is important for setting benchmarks for clinical governance. In particular, the impact of cooperatives on the number of emergency admissions to hospital has important implications for secondary care services. We aimed to acquire such information by analysing out of hours calls made to a sample of representative cooperatives.
Method
We analysed data from all out of hours calls made to 20 representative cooperatives using Adastra management software over one year. This software is used by more than 100 cooperatives and deputising services providing care for more than half of the UK population.
Selection of cooperatives
Eight cooperatives using Adastra software recorded the postcodes of callers. As postcodes can be matched to underprivileged area scores21 we included all of these cooperatives in the study to show the number of calls from deprived areas. A further 12 cooperatives were randomly selected after stratification by region (southern England, the Midlands, northern England, and Scotland) and by size (more or fewer than 100 members). We selected eight cooperatives from southern England, and four from each of the other regions—this reflected the greater number of cooperatives and population density in the south. No cooperatives in Wales or Northern Ireland used Adastra. To recruit 20 cooperatives, we had to approach 23 (response rate 87%).
Collection of calls data
With Adastra software, calls from patients are entered by receptionists directly on to the system as they are received—all calls that were passed to a doctor or nurse for assessment are included in this study. Some general enquiries are dealt with by receptionists alone and these are not necessarily recorded. They may include cases where a receptionist advises a patient to call a dentist or ambulance instead of the cooperative.
A program was written to extract anonymised details of calls received from 1 September 1997 to 31 August 1998, including the patient's age, sex, postcode, date and time of call, site and timing of consultation, and details of hospital admissions.
Analysis
Data were analysed in SPSS for Windows. “Out of hours” was defined as 1900 to 0700 on weekdays and from 1200 onwards on Saturdays at weekends. We excluded bank holidays from the main analyses because cooperatives' opening times varied, but rates including bank holidays were calculated for a subset of cooperatives that were open throughout. We compared rates of calls at different cooperatives by direct age standardisation using the UK population as a reference.
Where cooperatives recorded patients' postcodes, we matched these to underprivileged area scores and we classified scores of >30 as deprived. In calculating the total number of calls from deprived areas and non-deprived areas, we made adjustment proportionally for each cooperative to allow for calls with missing postcodes.
Patient populations
We asked every practice belonging to each cooperative to provide details of its list size, the age and sex distribution of its patients, the number of patients attracting deprivation payments, and the number of rural practice units that it was paid. Two reminders were sent to practices. In most cases we obtained a total list size for non-responding practices; in other cases we multiplied the number of partners in the practice by the average list size for the local health authority. We assumed that non-responding practices had patient populations with the same demographic characteristics as responding practices in their cooperative. If less than 70% of practices belonging to a cooperative responded, the cooperative was excluded from calculations of rates of calls. We performed a one way sensitivity analysis based on non-responding practices having a mean list size 50% larger or smaller than that assumed.
Organisation of cooperatives
A semistructured interview was conducted with the manager at each cooperative. This reviewed the ways in which calls were received and entered and the factors relating to the locality, structure, or organisation of the cooperative that would influence the interpretation of the analysis of calls.
Results
Of 1 099 401 calls recorded over the year, 899 657 fell within the defined out of hours period and 37 046 occurred during bank holidays between 0700 and 1900.
At three cooperatives less than 70% of member practices provided demographic details of patients, and a further cooperative transferred calls to a deputising service after midnight; four cooperatives were therefore excluded from rate calculations. The average response rate from practices at the remaining 16 cooperatives to our request for population details was 88% (range 71% to 100%).
Demand for out of hours care
The age and sex specific rates of out of hours calls are shown in table 1. The overall out of hours call rate (excluding bank holidays) was 159 calls per 1000 patients/year (95% confidence interval 158.5 to 159.2; range 127 to 299). The sensitivity analysis showed that the rate would lie between 157 and 161 calls per 1000 patients/year if the estimated list sizes of non-responding practices varied by up to 50%.
Table 1.
Age and sex specific rates (per 1000 patients/year) of out of hours calls based on 707 198 calls to 16 cooperatives
| Age group (years) | Males
|
Females
|
|||||
|---|---|---|---|---|---|---|---|
| No of calls | Population | Rate (95% confidence interval) | No of calls | Population | Rate (95% confidence interval) | ||
| 0-4 | 93 151 | 135 307 | 688 (684 to 693) | 80 192 | 129 127 | 621 (617 to 625) | |
| 5-14 | 46 743 | 302 622 | 154 (153 to 156) | 43 650 | 287 407 | 152 (150 to 153) | |
| 15-24 | 19 937 | 267 784 | 74 (73 to 75) | 42 444 | 261 434 | 162 (161 to 164) | |
| 25-44 | 53 323 | 697 888 | 76 (76 to 77) | 99 641 | 685 588 | 145 (144 to 146) | |
| 45-64 | 38 175 | 570 488 | 67 (66 to 68) | 51 651 | 570 343 | 91 (90 to 91) | |
| 65-74 | 22 693 | 191 639 | 118 (117 to 120) | 26 696 | 221 905 | 120 (119 to 122) | |
| ⩾75 | 32 897 | 128 015 | 257 (254 to 260) | 56 005 | 228 308 | 245 (243 to 247) | |
| All ages | 306 919 | 2 293 743 | 134 (133 to 134) | 400 279 | 2 384 112 | 168 (167 to 168) | |
Data on age or sex, or both, were missing in 35 767/742 965 (4.8%) of calls.
At the 12 cooperatives that were open during bank holidays the overall call rate was 144 (143.8 to 144.6) excluding the bank holiday opening times and 151 (150.8 to 151.6) including these times.
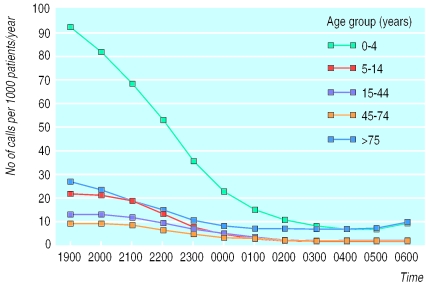
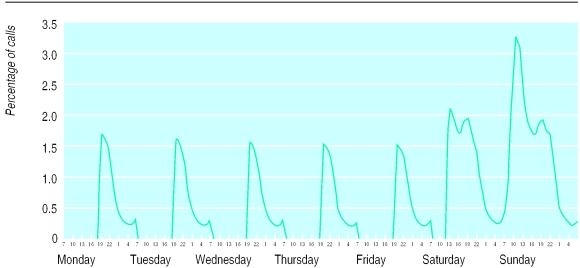
The pattern of calls by time was similar for all age groups, with most calls being made in the early evening, although most of these evening calls related to infants (fig 1). There was little variation by day of the week, although nights at weekends were slightly busier than weekday nights. The distribution of calls over a whole week showed that the peak demand occurred on Sunday mornings (fig 2). Little seasonal variation occurred, with a slightly increased number of calls between November and March and fewest calls in September and October.
Figure 1.
Rate of calls at different times by age groups
Figure 2.
Distribution of out of hours calls over one week based on 888 167 calls to 19/20 cooperatives (the excluded cooperative closed at midnight)
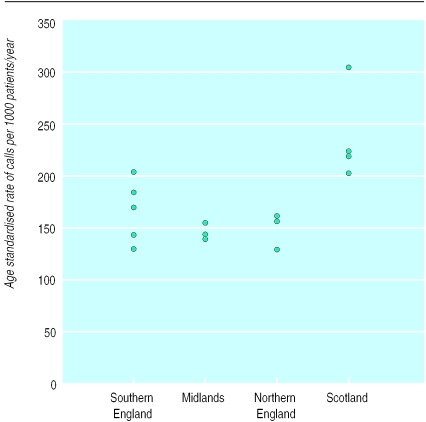
The cooperatives in Scotland experienced higher demand than those in England (standardised rate 221 v 145 calls per 1000 patients/year) (fig 3). We could not show any relation between the rate of out of hours calls at different cooperatives and the age structure of the patient population or the proportion living in rural or deprived areas.
Figure 3.
Rates of calls to cooperatives in different regions
For five cooperatives we obtained details of the underprivileged area scores of callers and calculated the proportion of patients living in deprived areas. For these five cooperatives the average proportion of calls for which details of scores were available was 81% (range 67% to 99%). One of these cooperatives did not cover any deprived areas, leaving data from four cooperatives for analysis. The rate of calls from deprived areas was 70% higher than that from non-deprived areas (table 2).
Table 2.
Annual call rates per 1000 population for four cooperatives that covered deprived populations
| Cooperative
|
Overall (95% CI) | ||||
|---|---|---|---|---|---|
| A | B | C | D | ||
| Rate per 1000 population in deprived areas | 286 | 201 | 267 | 193 | 239 (235 to 242) |
| Rate per 1000 population in non-deprived areas | 190 | 126 | 177 | 131 | 141 (141 to 142) |
| Overall rate | 198 | 127 | 179 | 133 | 144 (143 to 144) |
CI=confidence interval.
Response of cooperatives
Almost half (408 407; 45.4%) of the out of hours calls to all cooperatives (outside bank holidays) were handled by telephone advice from a doctor or nurse; a quarter (212 550; 23.6%) by home visits; and 29.8% (267 663) by the patient attending a primary care centre. For 11 033 (1.2%) calls there were other outcomes, and data were missing for four calls. The telephone advice rate varied between cooperatives from 26% to 66%, and the proportion of patients attending a centre varied from 10% to 57%. The site of consultations was related to the age of the patient, with 53.5% (89 566/167 430) of calls from patients aged over 65 years leading to a home visit.
Cooperatives responded to 60% of all calls within 30 minutes and 83% within one hour. The median response time for a home visit was 39 minutes, with 70% of visits being made within one hour and 92% within two hours.
Hospital admissions
Eleven cooperatives recorded details of all referrals for hospital admission. Admission followed 5.5% (30 743/554 179) of out of hours calls to these cooperatives. This represents a rate of 8.2 (95% confidence interval 8.1 to 8.3) admissions per 1000 patients/year. The age specific out of hours admission rate increased from 3 per 1000 patients/year in young people aged 5-14 years to 21 per 1000 patients/year in patients aged over 75 years. The percentage of calls leading to admission was related to time, from a minimum of 4% of calls during the day at weekends to a peak of 9% between 0200 and 0600.
Discussion
The information that we have provided here about the demand and supply of out of hours care by general practitioners is based on a much larger and more representative sample of calls than has been previously available. The sample of cooperatives in this project is not random because we initially included those that recorded patients' postcodes and because cooperatives using Adastra software might be a selected group. The sample was balanced, however, by size and by region and was drawn from cooperatives covering most of England and Scotland.
One potential weakness of this study is the assumptions about missing data used to estimate patient populations. The sensitivity analysis shows that this is unlikely to affect our results significantly. A further weakness concerns potential variability between cooperatives in the discretion they allow receptionists to redirect callers to another agency without recording the fact.
The overall calls rate is slightly lower than previously reported.6–8,16,18,20 This may represent a change with time or the fact that earlier studies were conducted in small and often atypical (usually urban) areas. Two recent studies reporting higher rates both came from Scotland,16,20 and our results also show high rates of calls at Scottish cooperatives.
The finding that patients living in deprived areas contacted a cooperative far more often than patients living in non-deprived areas supports earlier research.15 In the analysis of overall demand, however, the variation in call rates between different cooperatives could not be accounted for by local demographic features (age structure, deprivation, and rurality). These inconsistent findings may occur because the small proportion of patients living in deprived areas at each cooperative would have little effect on overall call rates.
A survey of cooperatives conducted in 1996 and based on self reported data of unknown reliability suggested wide variation in the proportion of patients being offered consultations at home, at a centre, or over the telephone.22 Our project, which used standardised data collection, has confirmed this variation and has shown a higher level of telephone advice than reported in the earlier survey. The consequences of these widely varying policies in terms of clinical outcomes, patient satisfaction, and cost effectiveness deserve further study.
The pattern of response by cooperatives in England and Scotland is now similar to that observed in Denmark after its reorganisation of out of hours services in 1992.23 The total demand for out of hours services, however, seems to be two to three times greater in Denmark,24 Finland,25 and the Netherlands26 than in England and Scotland. International comparisons should be interpreted cautiously because of varying definitions of the out of hours period and differences in health service organisation.
The findings about hospital admissions suggest that a system of care based on cooperatives would not lead to higher admission rates than would a care system based on practice rotas.27 The findings about response times suggest that cooperatives provide a rapid response to most calls—considerably faster than that reported in studies of deputising services.19,27 The greater accessibility of out of hours care, reinforced by the expansion of NHS Direct,28 may lead to an increase in demand for care. This project provides reliable national baseline data from which to test this hypothesis.
What is already known on this topic
Accurate information about the demand for and supply of out of hours care by general practitioners has been lacking
Much research has centred on night visits (only a small proportion of all out of hours calls) or atypical areas, with little information about the patient population
What this study adds
The rate of out of hours telephone calls to 20 nationally representative general practice cooperatives is 159 per 1000 population a year
Demand seems higher in Scotland than in England and much higher in deprived areas
Only 1 in 20 calls led to hospital admission
Call rates and cooperatives' responses varied with the age and sex of patients
Baseline data are now available for assessing the effect of further changes in service organisation, such as NHS Direct
Acknowledgments
We thank the doctors and staff at the 20 participating cooperatives and Adastra Software, especially Randolph Burt, for their help and support throughout this project. We also thank Debbie Hart and Mike Muirhead for matching patients' postcodes to underprivileged area scores for England and Scotland respectively; Lothian, Lanarkshire, and Ayrshire and Arran Health Boards for providing data about practices; Connie Junghans for entering data about patient populations; and Tim Peters for statistical advice. The views and opinions expressed are those of the authors and do not necessarily reflect those of the NHS Executive.
Footnotes
Funding: This study was funded by the London regional office of the NHS Executive.
Competing interests: None declared.
References
- 1.Pencheon D. NHS Direct: managing demand. BMJ. 1998;316:215–216. doi: 10.1136/bmj.316.7126.215a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bain DJ. Deputising services: the Portsmouth experience. BMJ. 1984;289:471–473. doi: 10.1136/bmj.289.6443.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dixon RA, Williams BT. Twelve months of deputising: 100 000 patient contacts with eighteen services. BMJ. 1977;1:560–563. doi: 10.1136/bmj.1.6060.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salisbury C. Evaluation of a general practice out of hours cooperative: a questionnaire survey of general practitioners. BMJ. 1997;314:1598–1599. doi: 10.1136/bmj.314.7094.1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carlisle RD, Johnstone SP, Pearson JC. Relation between night visit rates and deprivation measures in one general practice. BMJ. 1993;306:1383–1385. doi: 10.1136/bmj.306.6889.1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pitts J, Whitby M. Out of hours workload of a suburban general practice: deprivation or expectation. BMJ. 1990;300:1113–1115. doi: 10.1136/bmj.300.6732.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Robinson G. Night visits in general practice. BMJ. 1993;306:1068. doi: 10.1136/bmj.306.6880.734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Livingstone AE, Jewell JA, Robson J. Twenty four hour care in inner cities: two years' out of hours workload in east London general practice. BMJ. 1989;299:368–370. doi: 10.1136/bmj.299.6695.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Majeed FA, Cook DG, Hilton S, Poloniecki J, Hagen A. Annual night visiting rates in 129 general practices in one family health services authority: association with patient and general practice characteristics. Br J Gen Pract. 1995;45:531–535. [PMC free article] [PubMed] [Google Scholar]
- 10.Whynes D, Baines D. Explaining variations in the frequency of night visits in general practice. Fam Pract. 1996;13:174–178. doi: 10.1093/fampra/13.2.174. [DOI] [PubMed] [Google Scholar]
- 11.Salisbury C. Visiting through the night. BMJ. 1993;306:762–764. doi: 10.1136/bmj.306.6880.762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baker D, Klein R. Explaining outputs of primary health care: population and practice factors. BMJ. 1991;303:225–229. doi: 10.1136/bmj.303.6796.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marsh GN, Horne RA, Channing DM. A study of telephone advice in managing out-of-hours calls. J RColl Gen Pract. 1987;37:301–304. [PMC free article] [PubMed] [Google Scholar]
- 14.McCarthy M, Bollam M. Telephone advice for out of hours calls in general practice. Br J Gen Pract. 1990;40:19–21. [PMC free article] [PubMed] [Google Scholar]
- 15.Carlisle R, Groom LM, Avery AJ, Boot D, Earwicker S. Relation of out of hours activity by general practice and accident and emergency services with deprivation in Nottingham: longitudinal survey. BMJ. 1998;316:520–523. doi: 10.1136/bmj.316.7130.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heaney DJ, Gorman DR. Auditing out-of-hours primary medical care. Health Bull Edin. 1996;54:495–498. [PubMed] [Google Scholar]
- 17.Soler M, Dowers A, Jones RB. Out of hours work in primary care: audit of an urban co-operative deputising service. Health Bull Edin. 1991;49:40–47. [PubMed] [Google Scholar]
- 18.Brogan C, Pickard D, Gray A, Fairman S, Hill A. The use of out of hours services: a cross sectional survey. BMJ. 1998;316:524–527. doi: 10.1136/bmj.316.7130.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Salisbury C. Observational study of a general practice out of hours cooperative: measures of activity. BMJ. 1997;314:182–186. doi: 10.1136/bmj.314.7075.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bain J, Gerrard L, Russell A, Locke R, Baird V. The Dundee out of hours cooperative: preliminary outcomes for the first year of operation. Br J Gen Pract. 1997;47:573–574. [PMC free article] [PubMed] [Google Scholar]
- 21.Jarman B. Identification of underprivileged areas. BMJ. 1983;286:1705–1709. doi: 10.1136/bmj.286.6379.1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jessopp L, Beck I, Hollins L, Shipman C, Reynolds M, Dale J. Changing the pattern out of hours: a survey of general practice cooperatives. BMJ. 1997;314:199–200. doi: 10.1136/bmj.314.7075.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Christensen MB, Olesen F. Out of hours service in Denmark: evaluation five years after reform. BMJ. 1998;316:1502–1505. doi: 10.1136/bmj.316.7143.1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hansen BL, Munck A. Out-of-hours service in Denmark: the effect of a structural change. Br J Gen Pract. 1998;48:1497–1499. [PMC free article] [PubMed] [Google Scholar]
- 25.Vehvilainen AT, Takala JK. Where have all the back pains gone? Changes in the reasons for requiring out-of-hours medical care from a centralized primary care centre after changing to a list system. Fam Pract. 1996;13:373–376. doi: 10.1093/fampra/13.4.373. [DOI] [PubMed] [Google Scholar]
- 26.Van Duijn NP, van Weert HCPM, Scholte D, Bindels PJE. Out of hours: primary care clinic or hospital emergency department? Eur J Gen Pract. 1998;4:69–73. [Google Scholar]
- 27.Cragg DK, McKinley RK, Roland MO, Campbell SM, Van F, Hastings AM, et al. Comparison of out of hours care provided by patients' own general practitioners and commercial deputising services: a randomised controlled trial. I: The process of care. BMJ. 1997;314:187–189. doi: 10.1136/bmj.314.7075.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Beecham L. NHS Direct will cover England by end of 2000. BMJ. 1999;318:1097. doi: 10.1136/bmj.318.7191.1097b. [DOI] [PMC free article] [PubMed] [Google Scholar]