Abstract
Purpose
To describe the therapeutic effect and possibility of the ultra-early surgery for poor-grade aneurysmal subarachnoid hemorrhage (Hunt-Hess grades IV - V).
Materials and Methods
Nine cases with intracranial aneurysms, demonstrated by computed tomographic angiography (CTA), were treated by ultra-early surgery under general anesthesia within 24 hours from subarachnoid hemorrhage (SAH), 5 cases were treated within 6 hours and 4 cases in 6 - 24 hours. Preoperative Hunt-Hess grade: 6 cases were IV and 3 cases were V. The clinical outcome was evaluated by Glasgow Outcome Scores (GOS).
Results
In operation, difficult dissection occurred in 5 cases (55.6%), and rupture of aneurysm occurred and temporary obstructions were performed in 4 cases (44.4%). After clipping of aneurysm, 2 cases underwent V-P shunt because of hydrocephalus, pulmonary infection occurred in 3 cases, hypothalamus reaction accompanied with upper gastrointestinal hemorrhage in 2 cases. The clinical outcome were favorable (GOS 4 - 5) in 4 cases (44.4%), dissatisfied (GOS 2 - 3) in 3 cases (33.3%), and dead (GOS 1) in 2 cases (22.2%) when patients departed from our hospital.
Conclusion
The ultra-early surgery can avoid early rebleeding of intracranial aneurysm, therefore, should be considered in the treatment of Hunt-Hess grade IV-V intracranial aneurysms. The appliance of CTA can make it possible to use of ultra-early surgery and improve the therapeutic effect.
Keywords: Intracranial aneurysm, ultra-early, surgery
INTRODUCTION
Spontaneous subarachnoid hemorrhage (SAH) is caused mainly by rupture of intracranial aneurysm, and its prognosis is closely related to the pre-operative condition of the patients (such as by Hunt-Hess grade),1 and the prognosis is even poorer in early re-rupture cases than the late re-rupture ones.2 Because early rerupture occurs mostly within 24 hours after subarachnoid hemorrhage, ultra-early surgery for aneurysms is gradually thought as the key to avoid re-rupture, improve curative ratio and decrease mortality and morbidity.3 Because of high post-operative mortality in severe subarachnoid hemorrhage (Hunt-Hess grades IV - V), ultra-early surgery is not historically recommended for those patients unless the patients' general conditions were improved after 24 hours. However, as the incidence of early re-rupture of aneurysm is higher in poor Hunt-Hess grade patients, and current diagnostic technique could not accurately determine the relationship between the extent of brain injury and the prognosis,4 many severe SAH patients are prone to rerupture of aneurysm when they had to wait for the selective early surgery. From January 2005 to September 2007, 9 cases of Hunt-Hess grades IV - V intracranial aneurysm were clipped at ultra-early in our hospital, and the clinical outcome and the possibility of using ultra-early microsurgery for poor-grade aneurismal SAH are discussed.
MATERIALS AND METHODS
General data
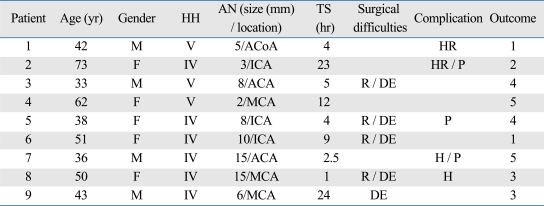
Nine cases of Hunt-Hess grades IV - V intracranial aneurysm were microsurgically clipped at ultra-early (within 24 hours after SAH) (grades IV in 6 cases and V in 3 cases). Four were men and 5 were women with a mean age of 47.6 ± 7.9 years range, (33 - 73 years) (Table 1).
Table 1.
Clinical Data and Outcome
HH, Hunt-Hess grade; AN, aneurysm; TS, time before surgery; ACoA, anterior communicating artery; ICA, internal carotid artery; ACA, anterior cerebral artery; MCA, middle cerebral artery; R, rupture of aneurysm; DE, difficult exposure; HR, hypothalamic reaction; P, pneumonia; H, hydrocephalus.
Radiological features
The aneurysms of the 9 patients were demonstrated by emergency 16-row multislice computed tomographic angiography (CTA) (3 in carotid artery, 3 in middle cerebral artery, 2 in anterior cerebral artery and 1 in anterior communicating artery) and saccular shape. The diameter of the aneurysms was less than 5 mm in 3 cases, 5 - 9 mm in 3 cases and more than 10 mm in 3 cases.
Treatment procedure
Intubation was immediately performed to preserve ventilation and normal oxygen saturation, and central venous catheters were inserted to insure sufficient blood supply during operation. Pre-operative ventricular drainage was performed in patients with intra-ventricular hemorrhage and 250 mL of 20% mannitol was rapidly injected after incision of scalp, together with hyperventilation to reduce the intracranial pressure. Interhemispheric approach was adopted in 2 anterior cerebral artery aneurysms and standard pterional osteotomy was used in other 7 cases. The principles of minimal brain retraction and sharp dissection of subarachnoid membrane under surgical microscope were strictly followed, and the aneurismal neck was clipped after exposure of its parent artery (parent artery was temporarily clipped when intra-operative aneurysm rupture happened); the reliability of aneurysms clipping was determined by routine aneurysm puncture. To avoid vascular spasm, intravenous nimodipine infusion was given during the operation; after clipping of aneurysm, the clot in cistern was removed, and diluted narceine was given. In surgery, the bone flap was also removed to reduce intra-cranial pressure. After operation, continual ventricular drainage or lumbar drainage, routine spasm-releasing treatments and "3H" treatment (hypertension, hypervolume and hemodilution) were performed. Early hyperbaric oxygenation was given if patients showed symptoms of cerebral vasospasm or cerebral infarction.
Outcome assessment
The curative effects were assessed as favorable (grade 4 - 5), dissatisfied (grade 2 - 3), and dead (grade 1) according to Glasgow outcome scores when patients left the hospital.
RESULTS
Intra-operative conditions
Of the 9 cases, 5 were operated within 6 hours and 4 were in 6 - 24 hours after SAH. Intra-operative rupture of aneurysms occurred in 4 cases (44.4%), and 5 cases had high intra-cranial pressure and difficulty in aneurismal exposure (55.6%). All 4 cases of aneurysms rupture had difficulty in aneurismal exposure; superficial cerebral vein thrombosis occurred in 2 cases (22.2%).
Post-operative complications
Pneumonia occurred in 3 cases, hypothalamic reaction with upper gastrointestinal hemorrhage in 2 cases, and V-P shunt was performed in 2 cases because of post-operative hydrocephalus.
Outcomes
When departing from hospital, 4 cases had favorable outcomes, 3 cases had dissatisfied outcomes, and 2 cases were dead. Of the 5 cases operated within 6 hours, 3 cases (60%) had favorable outcome, but only 1 case (25%) operated within 6 - 24 hours had same consequence. Of the 4 cases with intra-operative aneurysm rupture, 1 case was dead and 1 case had dissatisfied outcome; of the rest 5 cases, 1 case was dead and 2 cases had dissatisfied outcomes.
DISCUSSION
The prognosis of patients with Hunt-Hess grades IV - V SAH is very poor, but some achieved complete (or partial) recovery and good outcome if they are treated actively, such as avoiding the re-rupture of aneurysm and preventing from cerebral vascular spasm. Because the current diagnostic technique could not accurately clarify the extent of brain injury. And cerebral function dramatically recovers in a few poor-grade patients,2,4 all Hunt-Hess grades IV - V aneurismal SAH should be treated actively to avoid rerupture.5 Because 87% of early re-rupture of aneurysm occur within 24 hours after SAH6 and the incidence of rerupture is obviously higher in poor-grade (IV - V) SAH than that in low grades (I - III), ultra-early surgery has already been suggested by a few authors.5 Ultra-early surgery not only can avoid re-rupture of intra-cranial aneurysm, but also reduce the risks of delayed cerebral vascular spasm, caused by degradation products of erythrocyte through removal of clot in cistern,6 leading to decrease in mortality and morbidity. By the treatment of 9 severe SAH patients with ultra-early clipping of aneurismal neck, we found that 44.4% of cases achieved favorable outcome, which is in accordance with previous reports, and the mortality was 22.2%, which was lower than previous reports.5,7 Perhaps, this is because the benefits of urgent surgery and decompressive removal of bone-flap after diagnosis of aneurysm by CTA.
Emergency digital subtraction angiography (DSA) is the routine diagnostic method for SAH, however, some authors reported that ultra-early (esp. within 6 hours after SAH) DSA can distinctly increase the incidence of aneurismal re-rupture.8 Higher mortality would, therefore, be caused by rupture of aneurysm and leakage of angiographic agents.9 At the moment, the specificity and sensitivity of 16-row multislice CTA can match that of DSA,10 even in the detection of small aneurym (diameter < 5 mm).11 The advantages such as non-invasive, no-risk and short scanning time of CTA make it more suitable for emergency diagnosis of aneurysm. In addition, excellent image about aneurysm, parent artery and bone can meet the need of surgery thoroughly.10,12 In our patients, all aneurysms were diagnosed by emergency CTA and clipped urgently, thus dramatically reducing the pre-operative preparation time and making it possible to perform ultra-early surgery for aneurysm, esp. within 6 hours after SAH.
The major problems of early and ultra-early surgery for aneurysm are high intra-cranial pressure, difficulty in exposure of aneurismal neck, and rupture of aneurysm followed by temporarily obstruction of the parent artery in operation. In our cases, although ventricular drainage, mannitol, hyperventilation were adopted in operation, 5 cases still had difficulty in exposure, and 4 cases had aneurysm rupture and obstruction of their parent artery, which are obviously higher than the patients with delayed surgery. Therefore, how to decrease intra-cranial pressure in early stage would be the key to a successful ultra-early aneurismal surgery. To avoid surgical trauma, some authors recently inclined to urgent embolization for treatment of poor-grade patients (within 24 - 72 hours), and the favorable outcome was 30 - 48% in aneurysms located in internal carotid circulation,13-15 accordance with surgical outcome.5,7 However, the low complete occlusion rate14 in urgent embolization retains the possibility of recanalization and rebleeding, and sometimes needs further clipping.15 Besides, in our cases, dead and dissatisfied outcome rate (50%) in patients with difficult exposure were not higher than other patients (60%), suggesting that difficult exposure and intra-operative rupture of aneurysm are not the most important factor of poor prognosis and could be relieved by some measures. Therefore, further study should be taken on the choice of embolization and surgery in the treatment of Hunt-Hess grade IV - V.
Early diagnosis and surgery for aneurismal subarachnoid hemorrhage have achieved favorable clinical outcome, however, few studies have been performed on ultra-early surgery for poor-grade SAH. Our study on the ultra-early operation of 9 cases with severe SAH showed favorable outcome, especially, the patients treated within 6 hours after SAH. Although no statistical analysis could be performed because of the limited number of patients, we believe that CTA should be performed for poor-grade aneurismal SAH as soon as possible to get accurate diagnosis, and ultra-early surgery should be considered to save the patients' life.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Vajda J, Pasztor E, Orosz E, Nyary I, Juhasz J, Horvath M, et al. Early surgery for ruptured cerebral aneurysm. Int Surg. 1990;75:123–126. [PubMed] [Google Scholar]
- 2.Aoyagi N, Hayakawa I. Study on early re-rupture of intracranial aneurysms. Acta Neurochir (Wien) 1996;138:12–18. doi: 10.1007/BF01411717. [DOI] [PubMed] [Google Scholar]
- 3.Laidlaw JD, Siu KH. Ultra-early surgery for aneurysmal subarachnoid hemorrhage: outcomes for a consecutive series of 391 patients not selected by grade or age. J Neurosurg. 2002;97:247–249. doi: 10.3171/jns.2002.97.2.0250. [DOI] [PubMed] [Google Scholar]
- 4.Le Roux PD, Elliott JP, Newell DW, Grady MS, Winn HR. Predicting outcome in poor-grade patients with subarachnoid hemorrhage: a retrospective review of 159 aggressively managed cases. J Neurosurg. 1996;85:39–49. doi: 10.3171/jns.1996.85.1.0039. [DOI] [PubMed] [Google Scholar]
- 5.Fujii Y, Takeuchi S, Sasaki O, Minakawa T, Koike T, Tanaka R. Ultra-early rebleeding in spontaneous subarachnoid hemorrhage. J Neurosurg. 1996;84:35–42. doi: 10.3171/jns.1996.84.1.0035. [DOI] [PubMed] [Google Scholar]
- 6.Hosoda K, Fujita S, Kawaguchi T, Shose Y, Hamano S, Iwakura M. Effect of clot removal and surgical manipulation on regional cerebral blood flow and delayed vasospasm in early aneurysm surgery for subarachnoid hemorrhage. Surg Neurol. 1999;51:81–88. doi: 10.1016/s0090-3019(97)00508-9. [DOI] [PubMed] [Google Scholar]
- 7.Laidlaw JD, Siu KH. Poor-grade aneurysmal subarachnoid hemorrhage: outcome after treatment with urgent surgery. Neurosurgery. 2003;53:1275–1280. doi: 10.1227/01.neu.0000093199.74960.ff. [DOI] [PubMed] [Google Scholar]
- 8.Komiyama M, Tamura K, Nagata Y, Fu Y, Yagura H, Yasui T. Aneurysmal rupture during angiography. Neurosurgery. 1993;33:798–803. doi: 10.1227/00006123-199311000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Yasui T, Kishi H, Komiyama M, Iwai Y, Yamanaka K, Nishikawa M. Very poor prognosis in cases with extravasation of the contrast medium during angiography. Surg Neurol. 1996;45:560–564. doi: 10.1016/0090-3019(95)00360-6. [DOI] [PubMed] [Google Scholar]
- 10.Hui Wang, ying Guo, Wensheng Li, Zhuopeng Ye, Dejin Shi, Chaofeng Liang, et al. Possibility of 3D-CTA in place of DSA as the diagnostic and treatment way for intracranial an eurysm the reference 10 was published in Chinese, so it couldn't be found in Pubmed. Chin J Neurosurg. 2007;23:844–846. [Google Scholar]
- 11.Chen W, Wang J, Xin W, Peng Y, Xu Q. Accuracy of 16-row multislice computed tomographic angiography for assessment of small cerebral aneurysms. Neurosurgery. 2008;62:113–121. doi: 10.1227/01.NEU.0000311068.41239.02. [DOI] [PubMed] [Google Scholar]
- 12.Chappell ET, Moure FC, Good MC. Comparison of computed tomographic angiography with digital subtraction angiography in the diagnosis of cerebral aneurysms: a meta-analysis. Neurosurgery. 2003;52:624–631. doi: 10.1227/01.neu.0000047895.82857.eb. [DOI] [PubMed] [Google Scholar]
- 13.Bracard S, Lebedinsky A, Anxionnat R, Neto JM, Audibert G, Long Y, et al. Endovascular treatment of Hunt and Hess grade IV and V aneuryms. AJNR Am J Neuroradiol. 2002;23:953–957. [PMC free article] [PubMed] [Google Scholar]
- 14.Weir RU, Marcellus ML, Do HM, Steinberg GK, Marks MP. Aneurysmal subarachnoid hemorrhage in patients with Hunt and Hess grade 4 or 5: treatment using the Guglielmi detachable coil system. AJNR Am J Neuroradiol. 2003;24:585–590. [PMC free article] [PubMed] [Google Scholar]
- 15.Shin YS, Kim SY, Kim SH, Ahn YH, Yoon SH, Cho KH, et al. One-stage embolization in patients with acutely ruptured poor-grade aneurysm. Surg Neurol. 2005;63:149–154. doi: 10.1016/j.surneu.2004.03.021. [DOI] [PubMed] [Google Scholar]