Abstract
Purpose
Surgical treatment in the case of thoracolumbar burst fractures is very controversial. Posterior instrumentation is most frequently used, however, but the number of levels to be instrumented still remains a matter of debate.
Materials and Methods
A total of 94 patients who had a single burst fracture between T11 and L2 were selected and were managed using posterior instrumentation with anterior fusion when necessary. They were divided into three groups as follows; Group I (n = 28) included patients who were operated by intermediate segment fixation, Group II (n = 32) included patients operated by long segment fixation, and Group III (n = 34) included those operated by intermediate segment fixation with a pair of additional screws in the fractured vertebra. The mean follow-up period was twenty one months. The outcomes were analyzed in terms of kyphosis angle (KA), regional kyphosis angle (RA), sagittal index (SI), anterior height compression rate, Frankel classification, and Oswestry Disability Index questionnaire.
Results
In Groups II and III, the correction values of KA, RA, and SI were much better than in Group I. At the final follow up, the correction values of KA (6.3 and 12.1, respectively) and SI (6.2 and 12.0, respectively) were in Groups II and III found to be better in the latter.
Conclusion
The intermediate segment fixation with an additional pair of screws at the fracture level vertebra gives results that are comparable or even better than long segment fixation and gives an advantage of preserving an extra mobile segment.
Keywords: Thoracolumbar burst fracture, posterior instrumentation, intermediate segment fixation, fixation length, selective anterior fusion
INTRODUCTION
Thoracolumbar burst fractures are some of the most common spinal injuries. The goals of treatment in thoracolumbar fractures are to restore vertebral column stability and obtain spinal canal decompression using minimum number of fixation levels so as to preserve as much mobile segments as possible.1-5 After Holdsworth first described vertebral burst fractures in 1963,6 numerous articles and treatment methods, were developed, including posterior fixation with pedicular screws and rods, anterior fusion, or both.7-11 However, the optimal treatment strategy still remains controversial, which ranges from transpedicular screws, advocated by Roy-Camille and Demeulenaer,12 to short segment internal fixation7 and direct anterior decompression.11 Numerous authors have touted the benefits of their procedures. In addition, previous studies that dealt with the segmental range of motion in cases of thoracolumbar fractures operated by posterior instrumentation and fusion reported loss of mobility at the affected levels and more than 50% loss of motion in two adjacent levels.4,13 There are several case reports on initial selective anterior fusion with posterior fixation, followed by implant removal once bony fusion is achieved, for achieving both goals.5,14,15 However, there are no reports comparing the number of levels instrumented by posterior fixation and their respective results. Also, there are no reports which included radiographic and clinical analysis of the patients after the implants were removed.
Posterior short segment fixations without fracture segment fixation result in 5 - 94% failure rate of implant.16-18 Those reports prompted to study of the efficacy of long and intermediate segment fixation. Recently, Mahar et al.19 reported the efficacy and advantages of fracture segment fixation methods, and fixation range (short-, intermediate- or long-segment fixation) became one of the hot topics in the treatment of thoracolumbar burst fractures.8,20,21
Thus, the aim of our study was to find an ideal length of a posterior construct for thoracolumbar fractures to get a stable fixation along with preservation of as many mobile segments as possible.
MATERIALS AND METHODS
The present retrospective study was carried out in 94 patients with single vertebral level traumatic burst fractures between T11 and L2 from February 2001 to February 2006. All the patients were subjected to posterior stabilization with pedicular screws with selective anterior fusion at our institute. The study was approved by the institutional review board of our hospital. Sixty-four of these patients underwent implant removal procedures at around 1 year postoperatively. Inclusion criteria for the study were skeletally mature patients who had 1) a single level fracture with limited involvement of T11-L2, 2) classified as a burst fracture according to McAfee classification22 or type A3 fractures according to AO / ASIF classification,23 and 3) managed by posterior instrumentation with selective anterior fusion. Patients meeting with all three criteria were included in this study.
The indications for surgical intervention were 1) neurological deficit symptoms including motor weakness,24 2) vertebral body compression more than 40%,25,26 3) bony fragment encroachment upon the spinal canal of more than 50%,25,26 4) kyphotic deformity of more than 30 degrees,24,27 and 5) injury to all three vertebral columns. Patients having one of these findings were treated operatively.5,14,25,26
Indications for selective anterior fusion were 1) load sharing score (LSS) of more than 7,15 2) persistent or progressive neurological symptoms in the case of significant neural canal encroachment by bony fragment even after posterior fixation, and 3) significant injury to the posterior ligamentous complex.28 Patients with one of these three findings were treated not only by posterior fixation, but also with anterior fusion.5
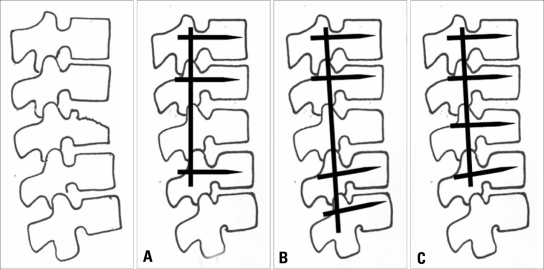
The patients were divided into three groups according to the number of levels of instrumentation. Group I included 28 patients treated by intermediate segment fixation without fracture segment instrumentation (2 levels above the fracture segment and 1 level below the fracture segment). Group II included 32 patients treated by long segment fixation without fracture segment instrumentation (2 levels above the fracture segment and 2 levels below the fracture segment). Group III included 34 patients treated by intermediate segment fixation with fracture segment instrumentation (2 levels above the fracture segment, the fracture segment and 1 level below the fracture segment) (Fig. 1).
Fig. 1.
Schematic figures of the operations performed in each group. (A) Group I, intermediate segment fixation without the fracture segment. (B) Group II, long segment fixation without the fracture segment. (C) Group III, intermediate fixation with the fracture segment.
Demographic data
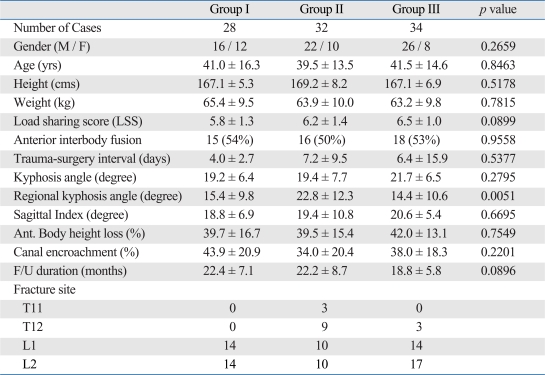
All of the three study groups were similar with regard to age, gender, height, weight, load-sharing scores, trauma-surgery interval, kyphosis angle, sagittal index, anterior compression rate, and canal encroachment. The mean follow-up time was similar between all three groups (21.0 ± 7.4 months). Implant removal procedures were performed in 64 of 94 patients. Of the remaining 30 patients, 19 of them refused an implant removal surgery as they had no complaints and 11 of them were lost to follow up after their visit at the end of 1 year. The mean implant removal duration from the first operation was 14.8 ± 6.1 (range, 6-33 months) (Table 1).
Table 1.
Patient Demographics and Preoperative Radiological Data
Surgical technique
All patients were managed by posterior instrumentation and selective anterior fusion. The number of levels to be instrumented was randomly decided by the operating surgeon. Pedicle instrumentation was applied bilaterally, and the reduction of the fracture was then performed by applying extension and compression-distraction forces. Posterior decompression was not performed. Finally, tightening of the screws was completed. Either interlaminar or intertransverse type of posterior fusion was not attempted by the authors.
Anterior fusion was performed in 49 patients, and 12 of them had less than 7 points on the LSS. Those 12 patients had either neurologic symptoms or definite posterior ligamentous complex injury. Within 9 months to one year postoperatively, implants were removed to save vertebral motion segment.
Radiographic measurements
Perioperative and follow-up radiographs were evaluated. Follow-up radiographs were divided into pre-implant removal and post-implant removal radiographs, and were always taken in standing position. In cases where the removal of implant was not done, pre-implant removal radiographs refer to the last follow-up radiographs. The kyphosis angle (KA) of the vertebral body was measured as the angle between the superior and inferior vertebral endplate. The regional kyphosis angle (RA) was measured as the angle between the superior endplate of the superior adjacent vertebra and the inferior endplate of the inferior adjacent vertebra (Fig. 2). To assess the actual segmental deformity at each vertebral level, the sagittal index (SI) described by Farcy et al.29 was used. Anterior body height (compression rate, AH) was measured as the anterior height of the injured vertebra divided by the mean of the anterior height of the adjacent two vertebrae (Fig. 2). Canal encroachment was assessed by computed tomography scans. The Load-Sharing Classification described by McCormack et al.15 was used to determine anterior column stability.1 The Load-Sharing score was measured by plain radiographs and CT scans. To determine whether anterior decompression was needed, postoperative CT scans were taken in patients to asses the amount of residual canal encroachment. Those patients who were found to have significant canal encroachment with persistent neurological deficit were subjected to second stage anterior surgery.
Fig. 2.
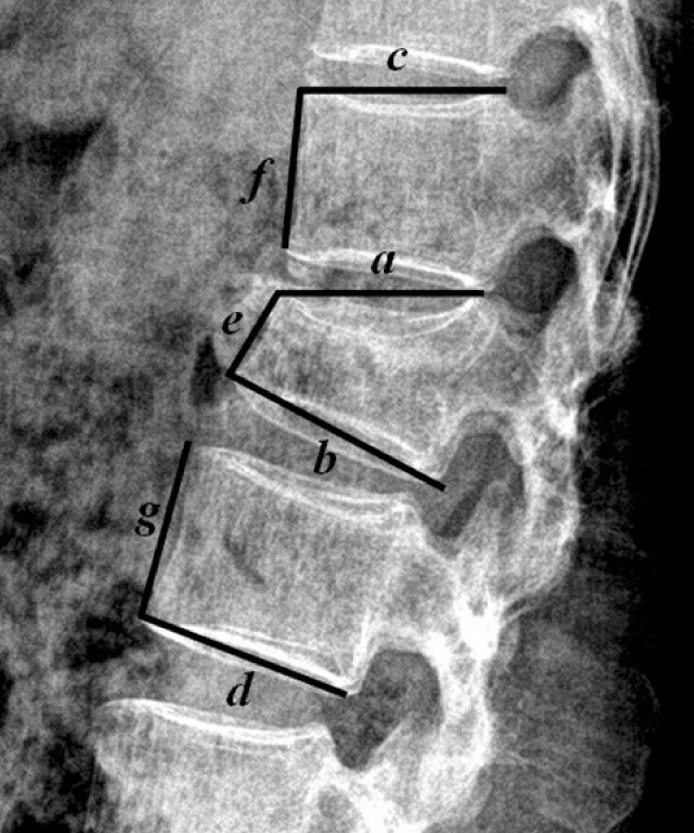
Kyphosis angle (KA), regional kyphosis angle (RA) and anterior body height loss (CR). Kyphosis angle (KA) = Angle between a and b, Regional kyphosis angle (RA) = Angle between c and d, Anterior body height Compression rate (AH) = 2e / (f + g) ×100.
Clinical assessment
Neurological assessment was conducted using the grading scale of Frankel et al.30 The Oswestry Disability Index questionnaire and Denis' Pain and Work scales were used to assess clinical outcomes.31
Statistical methods
The Anova test was performed for comparisons between three groups. Comparisons were also carried out with the T-test for continuous data and the Chi square test for noncontinuous data, taking two groups at a time. A p-value of < 0.05 was considered to be significant.
RESULTS
Radiographic results
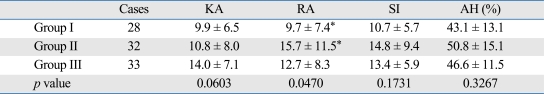
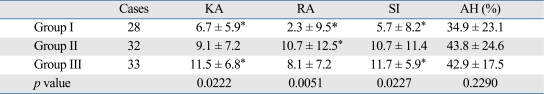
In the immediate postoperative period, KA, RA and SI of all three groups showed a similar tendency of significant reduction (Table 2) followed by a variable increase in the subsequent measurements. AH immediately showed an increase postoperatively (Table 2), then a slight decrease at the last follow up (Table 4).
Table 2.
Degree of Correction Achieved in Immediate Postoperative Period
KA, kyphosis angle; RA, regional kyphosis angle; SI, sagittal index; AH, anterior body height.
*Difference between the marked values in the same column is stastically significant.
Table 4.
Degree of Correction Achieved at Last Follow Up after Implant Removal
KA, kyphosis angle; RA, regional kyphosis angle; SI, sagittal index; AH, anterior body height.
*,†Difference between the marked values in the same column is stastically significant.
On analyzing the measurements taken just before implant removal, KA correction was found to be more significant in Group III than in Group I (p = 0.0222) and RA correction was better in Group II than in Group I (p = 0.0051). AH correction showed no significant differences among the three groups (p > 0.05). In SI correction over the same period, Group III showed the best correction result among the three groups and a statistically significant difference was found between Groups I and III (p = 0.0227) (Table 3).
Table 3.
Degree of Correction Achieved at Last Follow Up before Implant Removal
KA, kyphosis angle; RA, regional kyphosis angle; SI, sagittal index; AH, anterior body height.
*Difference between the marked values in the same column is stastically significant.
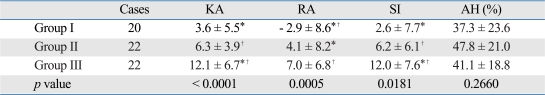
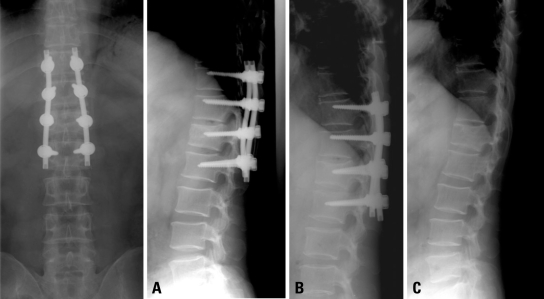
On the other hand, analysis of post implant removal radiographs showed that KA correction was much better in Group III than in Groups I and II (p < 0.0001) (Figs. 3 and 4). RA correction was also found to be significantly better in Groups II and III than in Group I (p = 0.0005). AH corrections again showed no significant differences (p = 0.2660). SI correction was also much better in Group III than in Groups I and II (p = 0.0181) (Table 4).
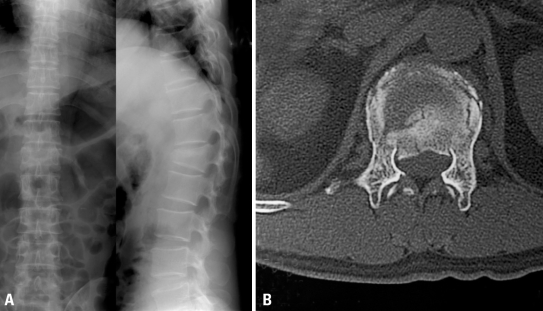
Fig. 3.
A 42-year-old man had fallen at a construction site. He visited the emergency room with back pain as his main complaint. (A) Preoperative plain radiographs showed a burst fracture at L1. Preoperative kyphosis angle, regional kyphosis angle, and sagittal index were 28 degrees, 28 degrees and 24 degrees, respectively. (B) Axial CT demonstrated 45% canal compromise.
Fig. 4.
(A) The patient underwent posterior intermediate segment fixation with fracture segment fixation. Postoperative kyphosis angle, regional kyphosis angle, and sagittal index were 11 degrees, 8 degrees, and 4 degrees, respectively. (B) Postoperative radiograph at 15 months after the initial operation showed no significant changes from immediate postoperative results. (C) He underwent implant removal and the final follow-up kyphosis angle, regional kyphosis angle and sagittal index were 12 degrees, 13 degrees and 7 degrees, respectively. He was ambulating well at time of release but could not go back to work.
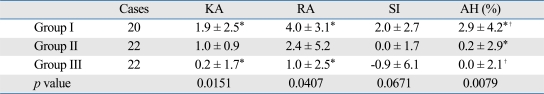
KA and RA correction losses in Group III after hardware removal were less than in Group I (p = 0.0151 and p = 0.0407, respectively). AH correction losses over the same period were much less in Groups II and III than in Group I (p = 0.0079). However, changes in SI showed no significant difference between the three groups (p = 0.0671) (Table 5).
Table 5.
Degree of Loss of Correction after Removal of Implant as Compared to Pre-Implant Removal Stage
KA, kyphosis angle; RA, regional kyphosis angle; SI, sagittal index; AH, anterior body height.
*,†Difference between the marked values in the same column is stastically significant.
Clinical outcome
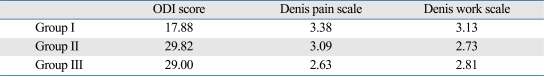
The Frankel classification was used for neurological assessment.30 Sixty-six of the 94 patients were classified as neurologically intact (Frankel classification E). There were 15 patients who were classified as Frankel D and 14 of them were neurologically normal at final follow up. Of the 9 cases of Frankel C, 7 patients improved to Frankel D and 2 patients to Frankel E. There were 4 patients with complete motor and sensory deficits who had undergone additional anterior decompression. In 85 patients, it was possible to assess current subjective status and symptoms through a questionnaire using the Oswestry Disability Index score and Denis' work and pain scale. The assessments were completed by asking questions over a telephone. Of the 85 patients, 25 patients from Group I, 27 patients from Group II and 33 from Group III were included. The mean ODI score was 26.7 (ranging from 11- 47). On the Denis' Pain scale, the mean of Group III was lower than the means of the other two groups. On the Work scale, the scores of Groups II and III were similar, but lower than Group I (Table 6).
Table 6.
Clinical Outcomes (Mean ODI Score, Mean Denis Pain and Work Scale)
ODI, Oswestry disability index.
Complications
There were 7 cases of implant failure (screw breakage or loosening), and one case of root injury in Group I. Because implant failures were confined to only one screw among all the cases and no evidence of kyphotic progression was noted, such cases were not subjected to re-operation prior to implant removal. The patient with an intraoperative root injury recovered from sensory changes several days after operation. In Group II, there were three cases of implant failure. Lastly, two cases of implant failure were reported in Group III. As with the implant failure cases of Group I, the authors did not feel it necessary to revise the implant failure cases of Groups II and III, as there was no significant kyphotic progression.
DISCUSSION
Pedicular screw fixation is well known to afford maximum multidirectional stability to spinal column, therefore, is now being used in almost all types of posterior spinal surgeries. However, the number of levels to be fixed so as to gain maximum stability with minimal loss of mobility is still an issue of debate. Short segment posterior fixation has been a popular method because of fewer motion segments being incorporated and a relatively lesser morbidity, however, due to a high incidence of implant failure and loss of correction which has been reported in the literature, it has fallen into disrepute.18,32 For these reasons, alternative techniques for stabilization of thoracolumbar fractures were developed. The augmentation of the anterior column via methods including transpedicular bone grafting, and polymethylmethaacrylate (PMMA) injection33-35 has been reported. Nevertheless, many authors believe that transpedicular bone grafts do not prevent early implant failure and correction loss, and may lead to low anterior interbody fusion rates in the long term.4,36 As far as PMMA injection is concerned, its long term results are still not known and it has its own complications like epidural leakage. Anterior instrumentation and bone grafting3,37 have been reported to afford good stability, however, it is much more invasive and associated with increased morbidity, so that its use in all patients may not be possible. A new technique that has been reported is the use of a transpedicular body augmenter which is inserted into the collapsed vertebral body through the pedicle. However, long term results of this technique are yet to be seen and the procedure also requires a certain amount of expertise.38,39 Consequently, none of the above techniques has emerged as a definite solution for thoracolumbar fractures.
In the literature, there are numerous reports on surgical outcomes of thoracolumbar fractures using different lengths of fixation constructs. Katonis et al.40 reported that two levels above and one level below the fracture at the thoracolumbar junction and short segment posterior fixation in the lumbar area provided stability and formed a rigid construct with no correction loss, Carl et al.16 reported that segmental pedicular fixation two levels above the kyphosis should be used at the thoracolumbar junction, where compression forces act more anteriorly, and Alvine et al.1 reported that use of four pairs of screws (two above and two below) to lengthen the level arm of the construct enhanced the stability and allowed effective reduction of kyphotic deformity.41,42
In a few previous studies, short segment fixations with an extra pair of screws inserted in the fractured vertebra have been reported.8,13,37 Mahar et al.19 recently reported a biomechanical study of 6 cadaveric spines and a short series of 12 patients in which they concluded that segmental fixation of burst fractures with screws at the level of the fracture offers improved biomechanical stability especially against axial torsion. They also proposed that segmental fixation provides for additional fixation points that may aid in fracture reduction and kyphosis correction. On the other hand, Korovessis et al.20 compared combined anterior plus posterior stabilization versus posterior short segment instrumentation, and stated that short segment fixation with additional screw at the fractured vertebra was not sufficient to prevent kyphotic progression, therefore, they did not recommend this method. However, this statement was later argued because Korovesis et al.20 showed superior clinical results with the fracture segment fixation method in spite of the fact that there was progression in kyphosis.43-45
Our goal of the present study was to find out whether there was any significant difference in stability afforded by intermediate and long segment fixation, and also whether the addition of an extra pair of screws at the fracture segment provided any extra advantage. Our hypothesis was that pedicular disruption does not occur in majority of the burst vertebral fractures, contrary to flexion-distraction or fracture-dislocation injuries. Therefore, the pedicle at the fractured segment level can serve as an additional point of fixation, and a more stable spinal construct incorporating one lesser mobile segment on the lower end can be obtained. This reduction in construct length would lead to more mobile segments spared without compromising the stability.13
We measured the kyphosis angle, regional kyphosis angle and sagittal index in all the three study groups and found that, although there was good immediate initial correction postoperatively in all the three groups, there was a variable amount of loss of correction at the last follow up. These findings are consistent with other previous studies.1-5 The postoperative correction achieved for KA, RA, and SI were found to be much better at the follow up stage just before implant removal in the groups II and III as compared to Group I. These results were comparable with previous studies, and there were superior results in Group II and III because an extra segment was fixed in these groups relative to Group I. In the 64 cases where the implant was removed, comparisons of the corrected KA from the initial fracture to post-implant removal period showed significantly better results in Group III than in Groups I and II. Correction of RA in the implant removed cases at final follow up was significantly more in Groups II and III than in Group I. The better degree of correction seen in groups II and III was expected due to long segment fixation but it was interesting to compare the correction values of KA between Group II and III after implant removal. The KA correction was significantly better in Group III than in Group II (12.1 versus 6.3, respectively). Also, the RA showed the same tendency in comparison of Groups II and III, though it was statistically insignificant (7.0 versus 4.1, respectively). According to our expectation, Group III should have shown slightly inferior correction rates compared to long segment posterior fixation in thoracolumbar fractures, however, Group III showed similar or even slightly better corrective results than Group II. We think that this may be due to the strong pedicle support at the fracture segment by an extra screw, even though Group III had one level shorter fixation than Group II. Other KA, RA, and SI comparisons at various intervals of follow up among the three Groups consistently showed better results in Groups II or III than Group I. We compared our results on variable posterior instrumentation techniques with the study published by Altay et al.;36 the percentage improvement in sagittal index just before implant removal of Groups II and III (54% and 56%, respectively) was quite comparable with the results of Altay et al. (56%).
However, there are a few limitations in our study design which must be considered. Firstly, patients were followed up at irregular intervals. Irregular follow ups may result in variability among patients and comparison between them may become difficult. However, we found no significant difference between the three groups (p > 0.05) in the average period of last follow-up, so that the final outcome measurements might not have been influenced by irregular follow-ups. Secondly, a flexion-extension radiograph to evaluate the spinal movement and stability of the fractured vertebra were not taken. Nevertheless, all the postoperative and follow up radiographs were taken in standing position which does act as a more sensitive indicator of stability than the supine radiographs.
According to preoperative radiographic findings, Group II had more T11 and T12 burst fracture cases than other groups. Consequently, there was a significant difference between Group II and other groups with regard to preoperative regional kyphosis angle (RA) (p < 0.05), since the T11 and T12 fractures are likely to have a greater regional kyphosis angle at the exact transition of spine from a state of kyphosis to lordosis. However, the preoperative sagittal index (SI) which is a more sensitive indicator of actual kyphotic deformity at the thoracolumbar level and kyphosis angle (KA) of the three groups showed no significant difference (p > 0.05) (Table1).
One clear distinction in our study was the pre and post implant removal stage radiographic measurements. After implant removal, further progression of subsidence of fractured vertebrae may occur, therefore, our study design was expanded to the post-implant removal period. Degree of loss of correction after implant removal was 2 degrees or less in RA and SI values of Groups II and III. This result might indicate that safe implant removal could be performed in Groups II and III, thereby preserving the mobile segment after fracture union. Consequently, the intermediate segment fixation with an additional pair of screws at the fracture level vertebra gives results that are comparable or even better than long segment fixation and also provides an advantage of preserving an extra mobile segment.
ACKNOWLEDGEMENTS
This study was supported by a faculty research grant of Yonsei University College of Medicine for 2007.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Alvine GF, Swain JM, Asher MA, Burton DC. Treatment of thoracolumbar burst fractures with variable screw placement or Isola instrumentation and arthrodesis: case series and literature review. J Spinal Disord Tech. 2004;17:251–264. doi: 10.1097/01.bsd.0000095827.98982.88. [DOI] [PubMed] [Google Scholar]
- 2.Briem D, Lehmann W, Ruecker AH, Windolf J, Rueger JM, Linhart W. Factors influencing the quality of life after burst fractures of the thoracolumbar transition. Arch Orthop Trauma Surg. 2004;124:461–468. doi: 10.1007/s00402-004-0710-5. [DOI] [PubMed] [Google Scholar]
- 3.Dimar JR, 2nd, Wilde PH, Glassman SD, Puno RM, Johnson JR. Thoracolumbar burst fractures treated with combined anterior and posterior surgery. Am J Orthop. 1996;25:159–165. [PubMed] [Google Scholar]
- 4.Leferink VJ, Zimmerman KW, Veldhuis EF, ten Vergert EM, ten Duis HJ. Thoracolumbar spinal fractures: radiological results of transpedicular fixation combined with transpedicular cancellous bone graft and posterior fusion in 183 patients. Eur Spine J. 2001;10:517–523. doi: 10.1007/s005860100319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parker JW, Lane JR, Karaikovic EE, Gaines RW. Successful short-segment instrumentation and fusion for thoracolumbar spine fractures: a consecutive 41/2-year series. Spine (Phila Pa 1976) 2000;25:1157–1170. doi: 10.1097/00007632-200005010-00018. [DOI] [PubMed] [Google Scholar]
- 6.Holdsworth F. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg Am. 1970;52:1534–1551. [PubMed] [Google Scholar]
- 7.Dick W, Kluger P, Magerl F, Woersdorfer O, Zach G. A new device for internal fixation of thoracolumbar and lumbar spine fractures: the 'fixateur interne'. Paraplegia. 1985;23:225–232. doi: 10.1038/sc.1985.38. [DOI] [PubMed] [Google Scholar]
- 8.Dick JC, Zdeblick TA, Bartel BD, Kunz DN. Mechanical evaluation of cross-link designs in rigid pedicle screw systems. Spine (Phila Pa 1976) 1997;22:370–375. doi: 10.1097/00007632-199702150-00003. [DOI] [PubMed] [Google Scholar]
- 9.Dickman CA, Yahiro MA, Lu HT, Melkerson MN. Surgical treatment alternatives for fixation of unstable fractures of the thoracic and lumbar spine. A meta-analysis. Spine (Phila Pa 1976) 1994;19(20) Suppl:2266S–2273S. doi: 10.1097/00007632-199410151-00003. [DOI] [PubMed] [Google Scholar]
- 10.Kaneda K, Taneichi H, Abumi K, Hashimoto T, Satoh S, Fujiya M. Anterior decompression and stabilization with the Kaneda device for thoracolumbar burst fractures associated with neurological deficits. J Bone Joint Surg Am. 1997;79:69–83. doi: 10.2106/00004623-199701000-00008. [DOI] [PubMed] [Google Scholar]
- 11.McAfee PC, Bohlman HH, Yuan HA. Anterior decompression of traumatic thoracolumbar fractures with incomplete neurological deficit using a retroperitoneal approach. J Bone Joint Surg Am. 1985;67:89–104. [PubMed] [Google Scholar]
- 12.Roy-Camille R, Roy-Camille M, Demeulenaere C. [Osteosynthesis of dorsal, lumbar, and lumbosacral spine with metallic plates screwed into vertebral pedicles and articular apophyses] Presse Med. 1970;78:1447–1448. [PubMed] [Google Scholar]
- 13.Leferink VJ, Nijboer JM, Zimmerman KW, Veldhuis EF, tenVergert EM, ten DH. Thoracolumbar spinal fractures: segmental range of motion after dorsal spondylodesis in 82 patients: a prospective study. Eur Spine J. 2002;11:2–7. doi: 10.1007/s005860100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dai LY, Jiang SD, Wang XY, Jiang LS. A review of the management of thoracolumbar burst fractures. Surg Neurol. 2007;67:221–231. doi: 10.1016/j.surneu.2006.08.081. [DOI] [PubMed] [Google Scholar]
- 15.McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine (Phila Pa 1976) 1994;19:1741–1744. doi: 10.1097/00007632-199408000-00014. [DOI] [PubMed] [Google Scholar]
- 16.Carl AL, Tromanhauser SG, Roger DJ. Pedicle screw instrumentation for thoracolumbar burst fractures and fracture-dislocations. Spine (Phila Pa 1976) 1992;17(8) Suppl:S317–S324. doi: 10.1097/00007632-199208001-00018. [DOI] [PubMed] [Google Scholar]
- 17.McNamara MJ, Stephens GC, Spengler DM. Transpedicular short-segment fusions for treatment of lumbar burst fractures. J Spinal Disord. 1992;5:183–187. doi: 10.1097/00002517-199206000-00006. [DOI] [PubMed] [Google Scholar]
- 18.McLain RF, Sparling E, Benson DR. Early failure of short-segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. J Bone Joint Surg Am. 1993;75:162–167. doi: 10.2106/00004623-199302000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Mahar A, Kim C, Wedemeyer M, Mitsunaga L, Odell T, Johnson B, et al. Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture. Spine (Phila Pa 1976) 2007;32:1503–1507. doi: 10.1097/BRS.0b013e318067dd24. [DOI] [PubMed] [Google Scholar]
- 20.Korovessis P, Baikousis A, Zacharatos S, Petsinis G, Koureas G, Iliopoulos P. Combined anterior plus posterior stabilization versus posterior short-segment instrumentation and fusion for mid-lumbar (L2-L4) burst fractures. Spine (Phila Pa 1976) 2006;31:859–868. doi: 10.1097/01.brs.0000209251.65417.16. [DOI] [PubMed] [Google Scholar]
- 21.McLain RF. The biomechanics of long versus short fixation for thoracolumbar spine fractures. Spine (Phila Pa 1976) 2006;31(11) Suppl:S70–S79. doi: 10.1097/01.brs.0000218221.47230.dd. [DOI] [PubMed] [Google Scholar]
- 22.McAfee PC, Yuan HA, Fredrickson BE, Lubicky JP. The value of computed tomography in thoracolumbar fractures. An analysis of one hundred consecutive cases and a new classification. J Bone Joint Surg Am. 1983;65:461–473. [PubMed] [Google Scholar]
- 23.Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3:184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 24.Reid DC, Hu R, Davis LA, Saboe LA. The nonoperative treatment of burst fractures of the thoracolumbar junction. J Trauma. 1988;28:1188–1194. doi: 10.1097/00005373-198808000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Benson DR, Burkus JK, Montesano PX, Sutherland TB, McLain RF. Unstable thoracolumbar and lumbar burst fractures treated with the AO fixateur interne. J Spinal Disord. 1992;5:335–343. doi: 10.1097/00002517-199209000-00012. [DOI] [PubMed] [Google Scholar]
- 26.Willén J, Anderson J, Toomoka K, Singer K. The natural history of burst fractures at the thoracolumbar junction. J Spinal Disord. 1990;3:39–46. [PubMed] [Google Scholar]
- 27.Domenicucci M, Preite R, Ramieri A, Ciappetta P, Delfini R, Romanini L. Thoracolumbar fractures without neurosurgical involvement: surgical or conservative treatment? J Neurosurg Sci. 1996;40:1–10. [PubMed] [Google Scholar]
- 28.Tezer M, Erturer RE, Ozturk C, Ozturk I, Kuzgun U. Conservative treatment of fractures of the thoracolumbar spine. Int Orthop. 2005;29:78–82. doi: 10.1007/s00264-004-0619-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Farcy JP, Weidenbaum M, Glassman SD. Sagittal index in management of thoracolumbar burst fractures. Spine (Phila Pa 1976) 1990;15:958–965. doi: 10.1097/00007632-199009000-00022. [DOI] [PubMed] [Google Scholar]
- 30.Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH, et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia. 1969;7:179–192. doi: 10.1038/sc.1969.30. [DOI] [PubMed] [Google Scholar]
- 31.Denis F, Armstrong GW, Searls K, Matta L. Acute thoracolumbar burst fractures in the absence of neurologic deficit. A comparison between operative and nonoperative treatment. Clin Orthop Relat Res. 1984:142–149. [PubMed] [Google Scholar]
- 32.Ferguson RL, Tencer AF, Woodard P, Allen BL., Jr Biomechanical comparisons of spinal fracture models and the stabilizing effects of posterior instrumentations. Spine (Phila Pa 1976) 1988;13:453–460. doi: 10.1097/00007632-198805000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Chen JF, Lee ST. Percutaneous vertebroplasty for treatment of thoracolumbar spine bursting fracture. Surg Neurol. 2004;62:494–500. doi: 10.1016/j.surneu.2003.10.049. [DOI] [PubMed] [Google Scholar]
- 34.Cho DY, Lee WY, Sheu PC. Treatment of thoracolumbar burst fractures with polymethyl methacrylate vertebroplasty and short-segment pedicle screw fixation. Neurosurgery. 2003;53:1354–1360. doi: 10.1227/01.neu.0000093200.74828.2f. [DOI] [PubMed] [Google Scholar]
- 35.Verlaan JJ, van Helden WH, Oner FC, Verbout AJ, Dhert WJ. Balloon vertebroplasty with calcium phosphate cement augmentation for direct restoration of traumatic thoracolumbar vertebral fractures. Spine (Phila Pa 1976) 2002;27:543–548. doi: 10.1097/00007632-200203010-00021. [DOI] [PubMed] [Google Scholar]
- 36.Altay M, Ozkurt B, Aktekin CN, Ozturk AM, Dogan O, Tabak AY. Treatment of unstable thoracolumbar junction burst fractures with short- or long-segment posterior fixation in magerl type a fractures. Eur Spine J. 2007;16:1145–1155. doi: 10.1007/s00586-007-0310-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kirkpatrick JS, Wilber RG, Likavec M, Emery SE, Ghanayem A. Anterior stabilization of thoracolumbar burst fractures using the Kaneda device: a preliminary report. Orthopedics. 1995;18:673–678. doi: 10.3928/0147-7447-19950701-16. [DOI] [PubMed] [Google Scholar]
- 38.Li KC, Hsieh CH, Lee CY, Chen TH. Transpedicle body augmenter: a further step in treating burst fractures. Clin Orthop Relat Res. 2005:119–125. [PubMed] [Google Scholar]
- 39.Chen HH, Wang WK, Li KC, Chen TH. Biomechanical effects of the body augmenter for reconstruction of the vertebral body. Spine (Phila Pa 1976) 2004;29:E382–E387. doi: 10.1097/01.brs.0000139308.65813.70. [DOI] [PubMed] [Google Scholar]
- 40.Katonis PG, Kontakis GM, Loupasis GA, Aligizakis AC, Christoforakis JI, Velivassakis EG. Treatment of unstable thoracolumbar and lumbar spine injuries using Cotrel-Dubousset instrumentation. Spine (Phila Pa 1976) 1999;24:2352–2357. doi: 10.1097/00007632-199911150-00011. [DOI] [PubMed] [Google Scholar]
- 41.Akbarnia BA, Crandall DG, Burkus K, Matthews T. Use of long rods and a short arthrodesis for burst fractures of the thoracolumbar spine. A long-term follow-up study. J Bone Joint Surg Am. 1994;76:1629–1635. doi: 10.2106/00004623-199411000-00005. [DOI] [PubMed] [Google Scholar]
- 42.Gurr KR, McAfee PC. Cotrel-Dubousset instrumentation in adults. A preliminary report. Spine (Phila Pa 1976) 1988;13:510–520. doi: 10.1097/00007632-198805000-00014. [DOI] [PubMed] [Google Scholar]
- 43.Kim C. Letters. Spine (Phila Pa 1976) 2007;32:2639. [Google Scholar]
- 44.Korovessis P. Letters. Spine (Phila Pa 1976) 2007;32:2638–2639. doi: 10.1097/BRS.0b013e318158cbe6. [DOI] [PubMed] [Google Scholar]
- 45.Verlaan JJ, Oner FC. Letters. Spine (Phila Pa 1976) 2006;31:2521. doi: 10.1097/01.brs.0000239148.92211.f1. [DOI] [PubMed] [Google Scholar]