Abstract
Purpose
Intrabdominal actinomycosis is difficult to diagnose preoperatively. This chronic infection has a propensity to mimic many other diseases and may present with a wide variety of symptoms. The aim of this study was to evaluate the characteristic clinical features with review of the literature.
Materials and Methods
We retrospectively analyzed 22 patients with intrabdominal actinomycosis between January 2000 and January 2006.
Results
There were two men and 20 women with a mean age of 42.8 years (range, 24 - 69). Twelve patients presented with masses or abdominal pain, whereas 3 patients presented with acute appendicitis. The rate of performing an emergency surgery was 50% due to symptoms of peritonitis. The mean size of tumor was 5.5 cm (range, 2.5 - 11.0). Sixty percent (n = 12) of female patients had intrauterine device (IUD). The average time to definite diagnosis was 10.6 days.
Conclusion
Intrabdominal abdominal actinomycosis must first be suspected in any women with a history of current or recent IUD use who presents abdominal pain. If recognized preoperatively, a limited surgical procedure, may spare the patient from an extensive operation.
Keywords: Actinomycosis, surgery, intrauterine device
INTRODUCTION
Actinomycosis is a chronic, suppurative, and granulomatous disease caused by an anaerobic Gram-positive bacterium, Actinomyces israelii, manifesting itself as fistula, sinus, inflammatory pseudotumor, or abscess formation.1 Humans are natural reservoirs and there is no documented person-to-person transmission of the disease, and it is commonly cultured from carious teeth, tonsilar crypts.2 It is characterized by a tendency to feign malignancy due to its capacity to invade surrounding tissues and to form masses.3 Therefore, there are multiple clinical presentations, often leading to misdiagnosis. The three main clinical forms of this disease are cervicofacial, thoracic, and abdominopelvic. The cervicofacial region accounts for 50% to 65%, followed by abdomen (20%).4-6
The disease usually shows an indolent course with clinical symtoms and signs that are not specific, resulting in delayed diagnosis. Actinomyces are sensitive to penicillin, but the duration of treatment varies from several weeks to months to achieve permanent recovery.7-10 The aim of this study was to evaluate the characteristic clinical features with short literature review on the topic.
MATERIALS AND METHODS
Between January 2000 and January 2006, 22 patients with abdominopelvic actinomycosis were identified. Patient's demographic data and outcome are summarized in Table 1. The clinical data including age, gender, mass size, preoperative diagnosis, presence and duration of intrauterine device (IUD) were retrospectively analyzed. Intrabdominal mass assessments consisted of physical examination, colonoscopy, ultrasonography, and abdominopelvic CT scan.
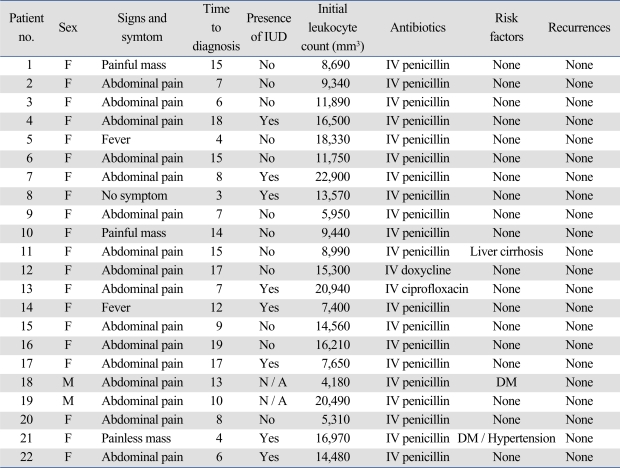
Table 1.
Summary of 22 Patients with Intrabominal Actinomycosis
IUD, intrauterine device.
RESULTS
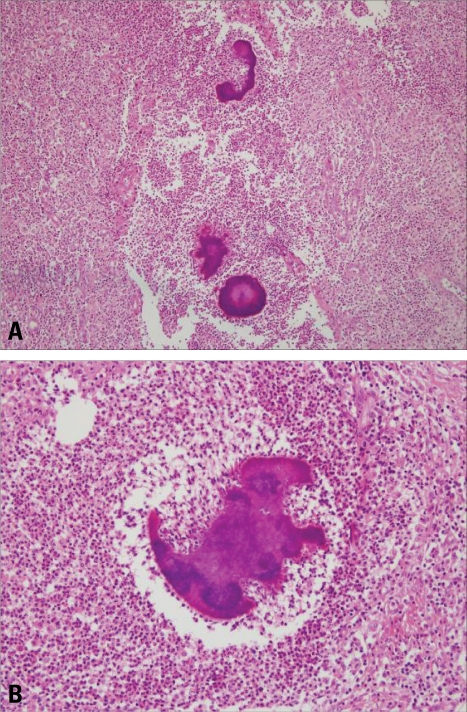
The clinical details of these patients are presented in Table 2. There were two men and twenty women with a mean age of 42.8 (range, 24 - 69) years. Twelve patients presented with masses or abdominal pain, whereas three patients presented with acute appendicitis (Table 3). Among the twenty two patients, only two patients presented with a colonic mass mimicking colon cancer. Fifteen patients (68.2%) had leukocytosis with a mean WBC count of 12,765 mm3 (range; 4,180 - 22,900 mm3). None of the patients presented with small bowel or colon obstruction. However, emergency surgery rate was 50% due to peritonitis symptoms. A preoperative abdominal CT scan or ultrasonography was done in all patients and detected intrabdominal mass or abscess but failed to give a definite diagnosis. The median operative time was 140 (range, 90 - 420) minutes and the median blood loss was 250 (range, 150 - 800) mL. The mean size of tumor was 5.5 (range, 2.5 - 11.0) cm. Sixty percent (n = 12) of female patients had IUD. The patients had been wearing IUD for an average of 7 years, and 15% had been wearing an IUD for 3 years or less. Confirmation of the diagnosis of actinomycosis was done by histology in all cases. Microscopically, each of the specimens showed chronic inflammatory reactions with sulfur granules (Figs. 1 and 2). None of the patients underwent percutaneous biopsy. There were no cancer cells found in all patients. The average time to definitive diagnosis was 10.6 days (range, 4 - 19 days).
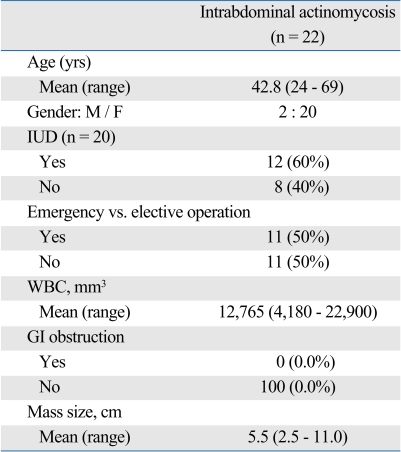
Table 2.
Patients' Characteristics
IUD, intrauterine device; WBC, white blood cell; GI, gastrointestinal.
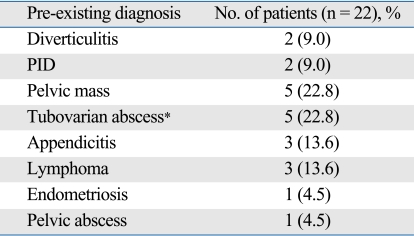
Table 3.
Pre-Existing Diagnosis before Intrabdominal Actinomycosis
*One patient with combined sigmoid colon fistula. PID, pelvic inflammatory disease.
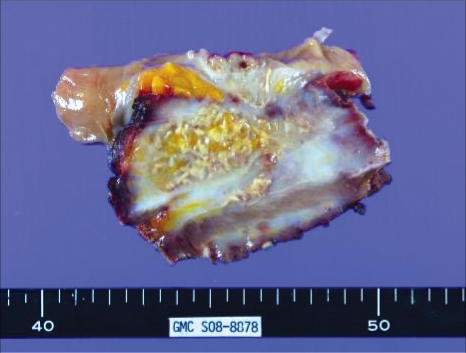
Fig. 1.
10.3 × 9.3 cm ovoid mass on the serosal surface of the cecum and ascending colon with ulceration. The cut surface demonstrates typical light gray color with necrosis.
Fig. 2.
(A) A actinomycotic abscesses containing sulfur granules with radiating filaments (H & E, ×100). (B) A magnified view of the characteristic sulfur granule (H & E, ×200).
After a median follow up of 37.5 months (range, 6.6 - 23.1 months), recurrence was not seen in any patients. The antibiotic of choice was IV penicillin, however, one patient was given ciprofloxacin due to penicillin allergy. The duration of treatment was 3 months in twelve patients, 6 months in five patients, 4 months in two patients and 1 month in two patients who refused to continue.
DISCUSSION
Actinomycosis was first diagnosed in a live patient by Ponfick in 1879.11 It is a chronic suppurative disease caused by an anaerobic, filamentous Gram positive bacteria.12 Actinomycosis Israelii is a constant part of the microflora in the human oral cavity, gastrointestinal and genital tracks.12,13 The organism is unable to cross normal mucosal barrier, therefore, opportunistic infections can occur only in context of underlying local disease such as trauma, surgery, or a foreign body which is significant enough to penetrate this barrier. Once the organisms have penetrated the mucosa, spread by continuity seems to be the primary method of intrabdominal propagation. Lymphatic and hematogenous spread is uncommon,14,15 although there is a hematogenous and lymphatic spread with nodal involvement reported.16
Clinically, the disease follows an indolent course and the initial presentation usually includes lower abdominal pain and fever with or without a palpable mass as was seen in our series. Since symptoms and signs are not specific, the diagnosis is often delayed and only 10% of cases are diagnosed preoperatively.16 In our series, only one patient (4.5%) was diagnosed before surgery.
Intrabdominal actinomycosis can appear as an abdominal mass of ambiguous benignity and can mimic a malignant tumor. For example, actinomycosis of the colon or the greater omentum is a rare differential diagnosis of colonic carcinoma or peritoneal tumor.17-19 The pathogenesis of abdominal actinomycosis is not yet well understood. There are two possibilities suggested that can affect intrabdominal organs: through blood-borne infection or by swallowing.20 Actinomyces can normally inhabit colon, predominating in areas of stagnation i.e. the cecum and appendix. Actinomyces requires injury to the normal mucosa to penetrate and cause disease. Predisposing factors may include appendicitis and diverticulitis, gastrointestinal perforations, previous surgery, foreign bodies, or neoplasia.21 Thus, intrabdominal actinomycosis should be included in differential along with other inflammatory diseases such as ulcerative colitis, Crohn's disease, tuberculosis, diverticulitis and pelvic inflammatory disease.
Pelvic actinomycosis has recently become more prevalent and is associated almost exclusively with women who use IUDs.16 Orogentital tract is thought to be an important mode of acquiring this type of infection in lower genital tract.22 In the uterine cavity, the microorganisms are apparently confined to the superficial layers of the mucosa, a fact perhaps related to its cyclic shedding. The most likely route of spread with subsequent development of pelvic abscess appears to be through patent fallopian tubes. The use of IUD may increase the risk of infection through injury to the normal uterine mucosa.13,23 Pelvic actinomycosis associated with the use of IUDs can mimick pelvic malignancy.24 For such reason, it is often surgically excised. However, if a diagnosis can properly be made preoperatively, antibiotic treatment and removal of IUD may lead to complete remission, avoiding unnecessary surgery. In our series, none of the patients with IUDs was diagnosed of actinomycosis preoperatively. Fiorino25 reported 92 patients with actinomycotic abscess in 63 case reports. In this study, the average duration of IUD implantation was 8 years, and only 16% had been using an IUD for less than 3 years. Likewise, the average duration of IUD was 7 years and only 15% of those patients had IUD for less than 3 years in our study. Although IUD is strongly correlated with intrabdominal actinomycosis, a definite duration of IUD implantation and the risk of developing actinomycosis infection has not yet been established.
The modern principle of therapy for actinomycosis began with Peabody and Seabury in 1960,26 who recommended abscess drainage in combination with high dose antibiotics. Smith et al.27 reported that ciprofloxacin and tetracyclines showed poor performance in antimicrobial susceptibility testing of actinomyces species. Actinomyces species appear to be susceptible to a wide range of beta-lactam agents and, when combined with beta-lactamase inhibitors, they should be regarded as agents of first choice.27
Uncomplicated actinomycosis can be medically treated by antibiotics, although there are differing opinions in the literature about dosage and duration of antibiotic treatment.28,29 A prolonged treatment course is required because of the poor penetration of antibiotics into the fibrotic tissues. Thus, when there are more avascular spaces present due to severe tissue reactions, medical therapy may be less effective, resulting in longer duration of antibiotic treatment, regardless of the site of actinomycosis. Interestingly, two patients in our series (9.0%) who were treated with iv antibiotics less than 4 weeks did not recur during the last 34 months of follow-up. Hence, the clinical impact of surgical resection followed by short-term antibiotics merits for further study.
Even though intrabdominal actinomycosis is very rare in its frequency, it should be included in a list of differential diagnosis, especially in any women with a history of IUD use who presents with abdominal pain or a pelvic mass. If actinomycosis is suspected preoperatively, appropriate handling of cultures will increase the diagnostic yield which may spare the patient from an extensive surgery.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Koren R, Dekel Y, Ramadan E, Veltman V, Dreznik Z. Periappendiceal actinomycosis mimicking malignancy report of a case. Pathol Res Pract. 2002;198:441–443. doi: 10.1078/0344-0338-00279. [DOI] [PubMed] [Google Scholar]
- 2.Uchiyama N, Ishikawa T, Miyakawa K, Iinuma G, Nakajima H, Ushio K, et al. Abdominal actinomycosis: barium enema and computed tomography findings. J Gastroenterol. 1997;32:89–94. doi: 10.1007/BF01213302. [DOI] [PubMed] [Google Scholar]
- 3.Milach J, Ziółkowski P, Orzeł W. [A case of actinomycosis of the sigmoid in a 41-year-old woman with a clinical appearance of cancer.] Wiad Lek. 1989;42:895–898. [PubMed] [Google Scholar]
- 4.Belmont MJ, Behar PM, Wax MK. Atypical presentations of actinomycosis. Head Neck. 1999;21:264–268. doi: 10.1002/(sici)1097-0347(199905)21:3<264::aid-hed12>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 5.Berchtenbreiter C, Brüning R, Auernhammer A, Reiser M. Misleading diagnosis of retroperitoneal actinomycosis. Eur Radiol. 1999;9:1869–1872. doi: 10.1007/s003300050937. [DOI] [PubMed] [Google Scholar]
- 6.Ferrari TC, Couto CA, Murta-Oliveira C, Conceiçäo SA, Silva RG. Actinomycosis of the colon: a rare form of presentation. Scand J Gastroenterol. 2000;35:108–109. doi: 10.1080/003655200750024623. [DOI] [PubMed] [Google Scholar]
- 7.Anteby E, Milvidsky A, Goshen R, Ben-Chetrit A, Ron M. [IUD-associated abdominopelvic actinomycosis.] Harefuah. 1991;121:150–153. [PubMed] [Google Scholar]
- 8.Atad J, Hallak M, Sharon A, Kitzes R, Kelner Y, Abramovici H. Pelvic actinomycosis. Is long-term antibiotic therapy necessary? J Reprod Med. 1999;44:939–944. [PubMed] [Google Scholar]
- 9.Hinnie J, Jaques BC, Bell E, Hansell DT, Milroy R. Actinomycosis presenting as carcinoma. Postgrad Med J. 1995;71:749–750. doi: 10.1136/pgmj.71.842.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Turnbull AE, Cohen ME. Case report: pelvic actinomycosis with the development and resolution of a recto-sigmoid stricture. Clin Radiol. 1991;43:420–422. doi: 10.1016/s0009-9260(05)80575-6. [DOI] [PubMed] [Google Scholar]
- 11.Stringer MD, Cameron AE. Abdominal actinomycosis: a forgotten disease? Br J Hosp Med. 1987;38:125–127. [PubMed] [Google Scholar]
- 12.Scribner DR, Jr, Baldwin J, Johnson GA. Actinomycosis mimicking a pelvic malignancy. A case report. J Reprod Med. 2000;45:515–518. [PubMed] [Google Scholar]
- 13.Cintron JR, Del Pino A, Duarte B, Wood D. Abdominal actinomycosis. Dis Colon Rectum. 1996;39:105–108. doi: 10.1007/BF02048278. [DOI] [PubMed] [Google Scholar]
- 14.Klaaborg KE, Kronborg O, Olsen H. Enterocutaneous fistulization due to Actinomyces odontolyticus. Report of a case. Dis Colon Rectum. 1985;28:526–527. doi: 10.1007/BF02554104. [DOI] [PubMed] [Google Scholar]
- 15.Piper MH, Schaberg DR, Ross JM, Shartsis JM, Orzechowski RW. Endoscopic detection and therapy of colonic actinomycosis. Am J Gastroenterol. 1992;87:1040–1042. [PubMed] [Google Scholar]
- 16.Harris LF, Kakani PR, Selah CE. Actinomycosis. Surgical aspects. Am Surg. 1985;51:262–264. [PubMed] [Google Scholar]
- 17.Baierlein SA, Wistop A, Looser C, Peters T, Riehle HM, von Flüe M, et al. Abdominal actinomycosis: a rare complication after laparoscopic gastric bypass. Obes Surg. 2007;17:1123–1126. doi: 10.1007/s11695-007-9189-9. [DOI] [PubMed] [Google Scholar]
- 18.Huang CJ, Huang TJ, Hsieh JS. Pseudo-colonic carcinoma caused by abdominal actinomycosis: report of two cases. Int J Colorectal Dis. 2004;19:283–286. doi: 10.1007/s00384-003-0568-y. [DOI] [PubMed] [Google Scholar]
- 19.Rose G, Franke FE, Weimar B, Buhr J, Padberg W. [Actinomycosis of the colon as a rare differential diagnosis of colonic carcinoma.] Chirurg. 2000;71:93–97. doi: 10.1007/s001040050016. [DOI] [PubMed] [Google Scholar]
- 20.Alvarado-Cerna R, Bracho-Riquelme R. Perianal actinomycosis--a complication of a fistula-in-ano. Report of a case. Dis Colon Rectum. 1994;37:378–380. doi: 10.1007/BF02053601. [DOI] [PubMed] [Google Scholar]
- 21.Fowler RC, Simpkins KC. Abdominal actinomycosis: a report of three cases. Clin Radiol. 1983;34:301–307. doi: 10.1016/s0009-9260(83)80341-9. [DOI] [PubMed] [Google Scholar]
- 22.Gupta PK, Woodruff JD. Actinomyces in vaginal smears. JAMA. 1982;247:1175–1176. [PubMed] [Google Scholar]
- 23.Luff RD, Gupta PK, Spence MR, Frost JK. Pelvic actinomycosis and the intrauterine contraceptive device. A cyto-histomorphologic study. Am J Clin Pathol. 1978;69:581–586. doi: 10.1093/ajcp/69.6.581. [DOI] [PubMed] [Google Scholar]
- 24.Spagnuolo PJ, Fransioli M. Intrauterine device-associated actinomycosis simulating pelvic malignancy. Am J Gastroenterol. 1981;75:144–147. [PubMed] [Google Scholar]
- 25.Fiorino AS. Intrauterine contraceptive device-associated actinomycotic abscess and Actinomyces detection on cervical smear. Obstet Gynecol. 1996;87:142–149. doi: 10.1016/0029-7844(95)00350-9. [DOI] [PubMed] [Google Scholar]
- 26.Peabody JW, Jr, Seabury JH. Actinomycosis and nocardiosis. A review of basic differences in therapy. Am J Med. 1960;28:99–115. doi: 10.1016/0002-9343(60)90226-6. [DOI] [PubMed] [Google Scholar]
- 27.Smith AJ, Hall V, Thakker B, Gemmell CG. Antimicrobial susceptibility testing of Actinomyces species with 12 antimicrobial agents. J Antimicrob Chemother. 2005;56:407–409. doi: 10.1093/jac/dki206. [DOI] [PubMed] [Google Scholar]
- 28.Kaya E, Yilmazlar T, Emiroğlu Z, Zorluoğlu A, Bayer A. Colonic actinomycosis: report of a case and review of the literature. Surg Today. 1995;25:923–926. doi: 10.1007/BF00311761. [DOI] [PubMed] [Google Scholar]
- 29.Udagawa SM, Portin BA, Bernhoft WH. Actinomycosis of the colon and rectum: report of two cases. Dis Colon Rectum. 1974;17:687–695. doi: 10.1007/BF02587123. [DOI] [PubMed] [Google Scholar]