Abstract
This study determined whether adolescent-onset substance use disorders (SUDs) prospectively predicted early mortality. Among 870 adolescents, 21 young adulthood deaths were observed. Adolescent SUDs, as well as gender, ethnic group, hazardous substance use, and drug trafficking, predicted these deaths. Among African American males with SUDs, 23% died by age 25.
Keywords: substance use disorders, adolescents, mortality
Substance use disorders (SUDs, including abuse and dependence) have been demonstrated to be accompanied by excess mortality in adulthood (1). The extent to which SUDs and related risky behaviors predict young adulthood mortality has not been previously studied in a U.S. adolescent sample. Scandinavian studies have utilized national registries to determine that adolescent-onset substance use disorders (SUDs) predict early mortality (e.g., 6). The generalizability of these findings to U.S. adolescents is uncertain.
In adults, SUD-related deaths are typically caused by the medical complications of substance use, such as alcohol leading to hepatic cirrhosis (2). In adolescents with SUDs, such medical complications are rare (3). Among adolescents with SUDs, however, excess mortality may be related to risky behaviors. In the United States, mortality in young adulthood is most commonly caused by motor vehicle accidents (MVAs), homicides, and suicides (4). Homicides account for high mortality rates among African American young adult males (4). Many of these deaths may be a consequence of high risk behaviors associated with SUDs, including intoxicated driving, drug trafficking and suicide attempts (4, 5, 6). This report describes the first prospective study of SUDs and related risky behaviors as predictors of young adulthood mortality in U.S. adolescents.
METHODS
Subjects
The subjects were 870 adolescents (ages 12 through 18) from clinical programs (n=510) and community sources (n=360) followed for 8.0 ± 2.6 years. Subjects from clinical and community sources were recruited to be similar on gender, age, and ethnic group composition. The majority of subjects from clinical programs were receiving drug and alcohol treatment (n=359, 70%). After the initial contact, subjects were screened by telephone for eligibility (i.e., age, ability to complete the protocol) and willingness to consider participation. Information about recruitment procedures and subjects declining participation has been previously presented (3). Among eligible subjects, 70% of subjects recruited from clinical sources and 77% of subjects recruited from community sources completed the initial assessment. The protocol was approved by the University IRB and written consent was obtained prior to the assessment.
The sample included 432 females (49%) and 442 males (51%), as well as whites (W: n=702, 80.3%) and African Americans (AA: n=168, 19.2%). Additional subjects without known young adult outcomes (n=95) and subjects from other ethnic groups (n=4) were excluded. Comparing subjects from clinical and community recruitment sources, the groups were significantly different on gender (females: n=230, 45%; n=201, 56% for Clinical and Community recruitment sources, respectively; Pearson’s χ2=9.7, d.f.=1, p=.002), age (mean and standard deviation in years:16.5±1.4; 16.1±1.6; t=3.2, d.f.=868, p=.002), socioeconomic status (Hollingshead Two Factor SES Index: 36.0±12.74; 42.6±12.0; t=7.6, d.f.=859, p<.001) and SUDs (n=376, 74%; n=44, 12%; χ2=319.7, d.f.=1, p<.001), and were not significantly different on ethnic group (Whites: n=416, 82%; n=286, 79%; χ2= 0.6, d.f.=1, p=.4). Among community recruits, 3% had received drug and alcohol treatment, and 17% had received psychiatric treatment. The recruitment approach achieved over-sampling of adolescents with SUDs from clinical sources and also provided a normative community sample for comparative purposes.
Measures
Substance use disorders
SUD diagnostic items were collected with an updated version of the Structured Clinical Interview for DSM-IV (7). Subjects who met DSM-IV criteria for substance abuse or dependence involving alcohol or illicit drugs within six months prior to the interview were considered positive for SUDs.
High risk behaviors
Hazardous Use was defined by the criteria for DSM-IV substance abuse symptom A2 (i.e., recurrent substance use in situations in which it is physically hazardous, such as driving a car). Selling Drugs was defined by an affirmative response to any of a set of items inquiring as to whether the subject had sold cannabis or other illicit drugs. The history of suicidal behavior was determined by a screening interview followed by a detailed review of possible suicide attempt incidents (6). Subjects with a history of self-injurious or potentially injurious acts motivated by a wish to die were considered positive for Suicide Attempts.
Survival and cause of death
Subjects survival was confirmed by contacts during tracking or follow-up assessments. After the initial assessment, follow-up assessments occurred at 1-year, 3-years, 5-years, and age 25. Reports of subject deaths acquired in the course of project tracking were confirmed by the federal social security data base (n=14), by newspaper obituaries (n=4) or, if neither of these sources were available, by family members (n=3). We were not able to determine the cause of death in 9 cases.
Data Analyses
The statistical tests examining adolescent characteristics as predictors of young adult mortality utilized the Cox regression model approach, a survival analysis procedure. The independent variables were adolescent characteristics determined at the initial assessment and the dependent variable was the age of death or the last age at which the subject was confirmed to be alive (i.e., censored age). The test statistic was Wald’s Chi-square test (χ2). The first set of analyses examined the main effects of the primary variables of interest (i.e., gender, ethnic group, and SUDs), with the direction of results indicated by relative survival time. Socioeconomic status was also examined as an ethnic group covariate, and recruitment source (clinical or community) was examined as an SUD covariate. Specific high risk behaviors relevant to understanding these relationships, including Hazardous Use, Selling Drugs and Suicide Attempts, were also examined. To avoid colinearity among independent variables, the primary variables were then combined to form an eight subject classes (i.e., gender by ethnic group by SUD).
RESULTS
Among 870 adolescents, 21 deaths at an average age of 22.8±2.9 years were observed. In 12 cases for whom the information could be collected, the causes of death were MVAs (n=5), homicide (n=4), suicide (n=1), drug overdose (n=1), or other accident (n=1). Described by gender, ethnicity and adolescent-onset SUD, the numbers of deaths and rates are presented in Table 1.
Table 1.
Frequencies and proportions of deaths by gender, ethnic group and SUD status
| SUD | No SUD | |||
|---|---|---|---|---|
| n/total | % | n/total | % | |
| White Females | 1/129 | 1 | 0/208 | 0 |
| African American Females | 0/27 | 0 | 0/67 | 0 |
| White Males | 7/233 | 3 | 3/132 | 2 |
| African American Males | 7/31 | 23 | 3/43 | 7 |
Notes: SUD: subjects with substance use disorders; No SUD: subjects without substance use disorders; n: number of deaths; total: total number of subjects in subgroup.
In Cox regression models examining the main effects of individual independent variables, survival time was significantly predicted by gender (χ2=21.5, d.f.=1, p<.001: male < female) and ethnic group (χ2=10.2, d.f.=1, p=.001; AA<W), and was not predicted by SES (χ2=1.4, d.f.=1, p=.2). Survival time (present < absent) was significantly predicted by SUDs (4.1, d.f.=1, p=.04), Hazardous Use (χ2=7.9, d.f.=1, p=.005) and Selling Drugs (χ2=12.1, d.f.=1, p<.001), and was not predicted by Suicide Attempts (χ2=0.4, d.f.=1, p=.5). Recruitment source also predicted survival (χ2=5.6, d.f.=1, p=.02: Clinical < Community). After taking SUDs into consideration, however, recruitment source was not a significant survival time predictor (χ2=2.1, d.f.=1, p=.15).
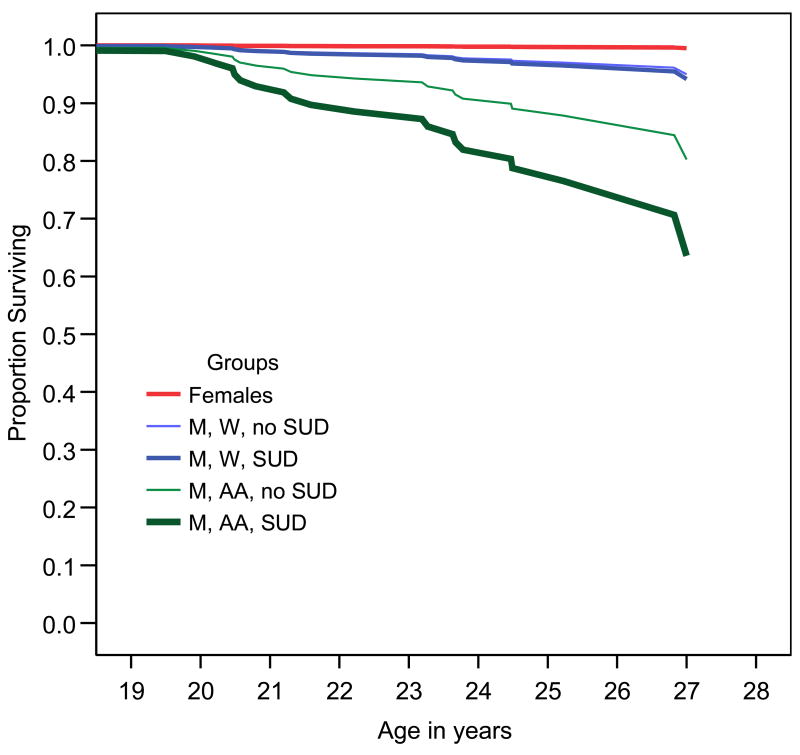
In the analysis with subject categories, the observation of only one death among females resulted in non-converging models when examining female subgroups. Female groups were consequently combined. The resulting five group variable significantly predicted survival time (χ2=38.0, d.f.=1, p<.001: Figure 1). Compared to females, each of the male groups had significantly diminished survival time. Among males, the groups were significantly different (χ2=17.1, d.f.=1, p=.001). Compared to W males without SUDs, W males with SUDs (χ2=0.1, d.f.=1, p=.8) and AA males without SUDs (χ2=3.5, d.f.=1, p=.06) were not significantly different, whereas AA males with SUDs had significantly diminished survival time (χ2=11.1, d.f.=1, p=.001). Utilizing W males without SUDs as a comparison group, mortality risk among AA males with SUDs was increased by an Odds Ratio of 10.3 (95% Confidence Interval 2.6, 40.4).
Figure 1.
Survival plots by gender, ethnic group, and adolescent substance use disorder. Abbreviations: M: male; W: white; AA: African American; SUD: adolescent-onset substance use disorder
DISCUSSION
In this study, young adult mortality was predicted by adolescent SUDs and related high risk behaviors. Males with SUDs in this sample had a mortality rate far in excess of the mortality rate of 137 per 100,000 reported for young adult males in the U.S. general population (4). The study limitations included heterogeneous recruitment sources diminishing generalizability, lack of information on subject status on SUDs and other characteristics proximal to the time of death, and the relatively small number of deaths observed. An ideal study design would include a very large representative sample and frequent assessments of risky behaviors over a 10–20 year follow-up period. While the present results need to be confirmed, the adolescent characteristics predicting death in young adulthood can be readily identified in clinical evaluations.
Adolescents may not be oblivious to the risks their behaviors pose. Among 2694 adolescents, 160 reported that they believed that they would die within the following two years (8). Risk behaviors associated with belief in early mortality included alcohol and drug use, drug selling, and drinking and driving. Unfortunately, this insight on the part of some adolescents apparently does not eliminate these problem behaviors. While successful treatment for SUDs may very well improve the length as well as the quality of life, interventions to address intoxicated driving and drug trafficking may also be helpful. Effective interventions need to be developed to prevent these predictable deaths in young adults.
Acknowledgments
This research was supported by NIAAA K02-AA-00291, K01-AA00324, K02-AA00249, R01-AA13397, P50-AA-08746 and NIDA R01-DA14635.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cornelius JR, Reynolds M, Martz BM, et al. Premature mortality among males with substance use disorders. Addictive Behaviors. doi: 10.1016/j.addbeh.2007.05.001. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Timko C, DeBenedetti A, Moos BS, et al. Predictors of 16-year mortality among individuals initiating help-seeking for an alcohol use disorder. Alcoholism Clin Exp Res. 2006;30(10):1711–1720. doi: 10.1111/j.1530-0277.2006.00206.x. [DOI] [PubMed] [Google Scholar]
- 3.Clark DB, Lynch KG, Donovan JD, et al. Health problems in adolescents with alcohol use disorders: Self-report, liver injury and physical examination findings. Alcoholism Clin Exp Res. 2001;25:1350–1359. [PubMed] [Google Scholar]
- 4.Park MJ, Mulye TP, Adams SH, Brindis CD, Irwin CE. The health status of young adults in the United States. J Adol Health. 2006;39:305–317. doi: 10.1016/j.jadohealth.2006.04.017. [DOI] [PubMed] [Google Scholar]
- 5.Li X, Feigelman S, Stanton B, et al. Drug trafficking and drug use among urban African-American adolescents. J Adolesc Health. 1998;23:280–288. doi: 10.1016/s1054-139x(98)00021-4. [DOI] [PubMed] [Google Scholar]
- 6.Kelly TM, Cornelius JR, Clark DB. Psychiatric disorders and attempted suicide among adolescents with substance use disorders. Drug Alcohol Dep. 2004;73:87–97. doi: 10.1016/j.drugalcdep.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 7.Martin CS, Pollock NK, Bukstein OG, et al. Inter-rater reliability of the SCID alcohol and substance use disorders section among adolescents. Drug Alcohol Depend. 2000;59:173–176. doi: 10.1016/s0376-8716(99)00119-2. [DOI] [PubMed] [Google Scholar]
- 8.Valadez-Meltzer A, Silver TJ, Meltzer AA, D’Angelo LJ. Will I be alive in 2005? Adolescent level of involvement in risk behaviors and belief in near-future death. Pediatrics. 2005;116:24–31. doi: 10.1542/peds.2004-0892. [DOI] [PubMed] [Google Scholar]