Abstract
PURPOSE
To compare objective measures of accommodation with the WR-5100K autorefractor and iTrace aberrometer to subjective push-down and defocus tests in normal phakic subjects and pseudophakic subjects with standard monofocal intraocular lenses (IOLs).
SETTING
University of Houston, College of Optometry, Houston, Texas, USA.
METHODS
The push-down test and defocus curves were used to stimulate and measure accommodation subjectively in pseudophakic subjects. For objective testing, a near target was pushed up and refraction measured objectively. For comparison, the same objective measurements were performed in phakic subjects. Calibration tests were performed with soft contact lenses in phakic subjects with varying refractive error and in pseudophakic subjects.
RESULTS
Fifteen phakic subjects (mean age 28.9 years ± 5.52 [SD]) and 10 pseudophakic subjects (mean age 66.2 ± 11.23 years) participated. Subjectively measured accommodative amplitude in the pseudophakic group was 3.28 ± 1.11 diopters (D) in the right eye and 3.64 ± 1.38 D in the left eye. Defocus curves in the pseudophakic group had a range of 2.00 D for distance-corrected visual acuity of 20/40 or better. Objective measurements in the pseudophakic group were 0.11 ± 0.50 D with the autorefractor and 0.10 ± 0.47 D with the aberrometer. Contact lens calibrations showed good agreement with the 1:1 line.
CONCLUSIONS
The subjective tests overestimated accommodative amplitude relative to the objective measures. The autorefractor and aberrometer were accurate, reliable, and appropriate for objective accommodation measurements in pseudophakes. Objective accommodation measurements such as these can be used to evaluate the performance of accommodating IOLs.
Accommodation is defined as a dioptric change in the power of the eye with an effort to focus at near.1,2 This optical change in the power of the eye results in a myopic refractive shift when viewing a near object. In a young phakic eye, the accommodative optical change comes from an increase in the power of the crystalline lens due to increased surface curvatures. In a pseudophakic eye with an accommodating intraocular lens (IOL), the change in the power of the eye could be due to movements of the optic or optics and/or changes in surface curvature.
With the advent of new surgical procedures and accommodating IOLs designed to restore active accommodation to the presbyopic eye, objective accommodation measurement is essential to determine whether these procedures actually restore accommodation. Most clinical testing of so-called accommodating IOLs considers visual acuity without objective accommodation testing.3 Although testing distance-corrected near visual acuity is important for understanding functional near vision benefits to patients, objective accommodation testing is essential to understand the efficacy of the procedures to accomplish what is claimed of them, namely restoration of accommodation.
Results in clinical trials of 2 accommodating IOLs did not include objective accommodation measurements. 4–6 The studies suggest that objective accommodation testing is too difficult to perform or that the effectiveness or “proof of principle” of the IOLs can be determined simply from distance-corrected near visual acuities. Accommodative range has also been defined from defocus curve testing as “the range of lens powers beyond which distance visual acuity was reduced by 2 lines on the ETDRS chart.” 4,5 This is a some-what arbitrary definition. A more stringent, and perhaps more appropriate, criterion might be the range of introduced defocus over which acuity is maintained at 20/40 or better. Although defocus curves offer more information than visual acuity alone, they provide no proof of active accommodation because the functional range of near vision could be attributable to the depth of field of the eye. Defocus testing, if not rigorously performed, can also produce artificially high accommodative amplitudes.7 Although subjective testing may show some level of functional distance-corrected near acuity, it cannot be considered a direct measure of accommodative amplitude. Unequivocal proof of restoration of accommodation requires objective measurement of accommodative change in the power of the eye with an effort to focus at near.
Objective accommodation measurement methods have been used to evaluate accommodating IOLs.8–11 These studies used subjective methods (push-up test, defocus curves, or both) and objective methods (eg, PowerRefractor [PlusOptiX], autorefractor [Shin-Nippon] and changes in anterior chamber depth with pilocarpine 2% measured with an IOLMaster [Carl Zeiss Meditec AG]) to measure accommodation of the 1CU (HumanOptics) or KH-3500 (Len-stec) accommodating IOL. Several methods and instruments have been used to perform objective accommodation measurements in pseudophakic eyes. Some techniques or instruments may not be readily useful in routine clinical studies; however, it is possible and practical to perform objective accommodation measurements in pseudophakic patients.
Many studies12–19 describe objective accommodation measurement in phakic subjects. Two commercially available clinical instruments that appear to be suitable for objective accommodation measurements in pseudophakes are the WR-5100K autorefractor (Grand Seiko Co., Ltd.) and iTrace aberrometer (Tracey Technologies, Inc.). Testing of these instruments has shown them to be reliable and consistent in phakic prepresbyopic eyes20 and demonstrated the precision (repeatability) of the instruments on phakic subjects.
In this study, the ability of the WR-5100K autorefractor and iTrace aberrometer to perform objective accommodation measurements in pseudophakic subjects was tested. The study compared objective measures of accommodation with both instruments to subjective push-down and defocus tests in pseudophakic subjects with standard monofocal IOLs attempting to accommodate at near. Standard monofocal pseudophakic eyes are not expected to show an accommodative change in the power of the eye with an effort to focus at near.
The primary goals of this study were to compare the results from the subjective and objective accommodation tests in pseudophakic eyes, show that objective instruments and protocols can be used in pseudophakic eyes, and evaluate practical clinical methods for verifying the accuracy of the autorefractor and aberrometer. The accuracy of the refraction measurements of the 2 instruments were compared using phakic subjects with a range of uncorrected refractive errors and by inducing known amounts of defocus with soft contact lenses in phakic and pseudophakic subjects.
SUBJECTS AND METHODS
Subjects
The study was comprised of phakic and pseudophakic subjects. The subjects had no known ocular pathology or strabismus and were correctable to at least 20/25 with soft contact lenses. Informed consent was obtained in accordance with the Declaration of Helsinki, and the study was performed in accordance with institutionally approved human subjects protocols.
In 10 phakic subjects, the instruments were evaluated for accuracy of measuring refractive errors by calibration with soft contact lenses and measuring refractive errors on-axis and 5 degrees off-axis temporally and nasally. In 5 additional young phakic subjects, accommodative amplitudes were measured for comparison with the pseudophakic subjects.
In 10 pseudophakic subjects with standard monofocal IOLs, subjective push-down testing, measurement of defocus curves, objective accommodation testing, and calibration tests were performed.
To avoid problems with reflections from spectacle lenses and magnification/minification or optical power issues associated with spectacle vertex distance, all subjects wore their best correction in soft contact lenses. Spherical refractive errors and astigmatism were fully corrected with the contact lenses.
Objective Instrumentation
Autorefractor
Subjects viewed far or near targets through the WR-5100K autorefractor’s 12.5 cm × 22.0 cm open-field beam splitter. Although the instrument allows a binocular open field of view, for comparison with the aberrometer, subjects viewed the targets monocularly while the contralateral eye was blocked with the instrument’s occluder. The instrument software was set to a sensitivity of 0.01 diopter (D) and a 0.0 mm vertex distance for measured refractions.
Aberrometer
The iTrace aberrometer is a monocular system. The Badal optometer for stimulating accommodation that is sold with the instrument was removed so the subject could view far or near targets through the instrument and the last beam splitter in the measurement path. The contralateral eye was covered with an eye patch. Sensitivity of the aberrometer software was set at 0.12 D (the lowest setting) and a 0.0 mm vertex distance.
Testing Setup for Both Instruments
For testing, the subject was seated at the instrument with the head stabilized in the instrument chin rest and forehead strap. The distance target was a 30.55 cm high × 20.33 cm wide, back-illuminated Snellen chart with Sloan letters at 6.0 m. To align the subject and ensure on-axis measurements of the eye with the aberrometer, a laser pointer was strapped to the near point rod attached to the top of the instrument. The position and orientation of the instrument and letter chart were adjusted so the spot from the laser pointer fell on the central letter of the letter chart. The laser pointer was then turned off. When a subject fixated on this central letter on the letter chart and a measurement was made, the subject perceived the aberrometer measurement diode laser spot to be superimposed on this same distance letter. If this was not the case, minor alignment adjustments of the position of the instrument or the letter chart were made. The autorefractor was aligned by taking a measurement and asking the subjects whether the center of the just-visible circular infrared (IR) ring light that appeared during measurements was aligned with the central letter on the letter chart. If not, the instrument or letter chart position was adjusted until this alignment was achieved. Alignment measurements were discarded and were not considered further. Baseline refractions were measured as the distance-corrected subjects fixated on the distance letter chart.
For accommodation testing, the near target was a copy of a portion of the Early Treatment Diabetic Retinopathy Study (ETDRS) near chart containing the 20/10 to 20/100 letters. The chart was suspended on a calibrated near-point rod mounted on the instruments and was illuminated with a white light-emitting diode (LED) light source connected to a battery and a rheostat. The near-target illumination was measured with a photometer through the beam splitters of each instrument. The LED brightness was adjusted to maintain equal letter chart illumination between the 2 instruments. Room illumination was dimmed to maintain large pupil diameters and measured to be 0.1 lux (TL-1 illuminance meter, Konica Minolta Sensing) at the headrest of the instruments. For all testing, 3 consecutive measurements were taken with each instrument. Testing with the instruments was performed in random order.
Testing the Instruments’ Tolerance of Alignment and Accuracy
On-Axis Versus Off-Axis Measurements in Phakic Subjects
To test how slight off-axis viewing affected refraction measurements with the autorefractor and aberrometer, uncorrected distance refractions were measured in 10 phakic subjects while the subjects viewed straight ahead (on axis), 5 degrees temporally, and 5 degrees nasally.
Subjects were aligned at each instrument for on-axis measurements as described above. The position of the distance chart was marked on the floor, and the calculated positions 5 degrees to the right and left of this position were marked. Three measurements were taken in the on-axis position, after which the distance chart was moved 5 degrees temporally and the subject was asked to fixate on the same central letter. Three measurements were taken in this position; then, the chart was moved 5 degrees nasally and the subject was again instructed to maintain fixation on the same letter, after which 3 measurements were taken.
Refractive Error Measurements and Contact Lens Calibrations
To ensure that the instrument refraction measurements were accurate, uncorrected refractive error measurements and contact lens calibrations were performed in 10 phakic subjects with both instruments. For the contact lens calibrations, contact lenses of known spherical power were used to systematically change the refraction in the eye. Then, the contact lens–induced refractive error was measured. To ensure that the subjects did not attempt to change the focus of the eye to compensate for the power of the contact lens, such as by accommodating through the minus-powered contact lenses, vision in the contact-lens-defocused eye was blocked and the subjects fixated on the distance letter chart with the contralateral eye. In the aberrometer testing, vision was blocked in the measured eye with an opaque occluder over the end of the open field of view through the instrument. With the autorefractor, an IR filter (filter #89B, high pass at 720 nm, Kodak) was placed in front of the eye. The subject viewed the distance letter chart with the contralateral seeing eye, corrected for distance if needed with a contact lens. First, refraction was measured in the unseeing eye without a contact lens, after which 3 measurements each were taken with contact lenses of +3.00 D, +2.00 D, +1.00 D, and −1.00 D (CooperVision, frequency 55 spherical) in the unseeing eye.
The contact lens calibration was also performed in the pseudophakic subjects. However, because of bright Purkinje image reflections off the IOL, use of the IR filter was problematic with the autorefractor in these subjects. Therefore, an occluder was used instead to block vision in the measured eye but permit the measurement to be made. This consisted of placing a black card on the examiner side of the autorefractor beam splitter to prevent the subject from seeing the letter chart with the eye being measured. The same occlusion procedure used with the autorefractor above was used with the aberrometer.
Pseudophakic Testing
Visual Acuity
Distance visual acuity was determined for the right eye, left eye, and both eyes with and without a correction. Intermediate visual acuity (near chart at 60.0 cm with a +1.50 D addition [add] in a trial frame in over best distance correction) was determined for the right eye, left eye, and both eyes and again without the +1.50 D add. Near visual acuity (near chart at 40.0 cm with a +2.50 D add in a trial frame over best distance correction) was determined for the right eye, left eye, and both eyes and again without the +2.50 D add. From this, it was determined which eye would be used for the remainder of the testing (best corrected visual acuity at distance or, if equal, best corrected acuity at distance and near).
Subjective Accommodation Testing
Method 1: Push-down Testing with RAF Rule
Subjects wore an eye patch over the nontested eye and sat in a standard examination lane chair during testing. A reading light illuminated the near target from behind the subjects and presented a mean luminance of 95 ± 3.06 cd/m2 (LS-100 luminance meter, Minolta Ltd.) on the copy of the ETDRS near letter chart on the RAF rule. The RAF rule is a calibrated, subjective accommodation, and convergence measuring rod. The subjects slide the letter chart toward or away from their eyes along the rod; the letter chart distance or stimulus amplitude in diopters can be read off the rod.21 Three measurements were taken for the right eye, left eye, and both eyes.
The push-down test was performed with the near target starting at the nose, where the letters are initially blurred and unrecognizable. The target is pushed away until clear focus is first perceived. This is in contrast to the push-up test, in which the target is first presented at 40.0 cm, where the letters can be clearly seen by the subject, and then pushed toward the subject until the first perceived sustained blur. The push-down test is used because it provides a more conservative measurement of the near reading distance than the push-up test.
Method 2: Defocus Curve in Phoropter
Wearing best distance correction in contact lenses if required, subjects sat in a standard examination chair behind a phoropter (Reichert). The nontested eye was occluded in the phoropter, and the tested eye was defocused with a starting lens power of +3.00 D. The subject was asked to read the projected distance Snellen letter chart. If the subject could not read the letters, the projected letter size was increased by 1 letter line. The line in which the subject could read all letters or missed a maximum of 2 letters was recorded as the visual acuity for that lens power. Lens power in the phoropter was decreased in −0.50 D steps to −4.50 D. Three ETDRS Snellen slides were rotated through in the projector so a different slide and line of letters were presented at each lens step to prevent memorization of letters.
Objective Accommodation Testing with Both Instruments
First, distance-corrected distance refraction was measured 3 times. To measure accommodation, a real proximal target of high-contrast black letters on a white background suspended on a near-point rod was moved closer to the subject in 0.50 D steps to stimulate accommodation. Then, the corresponding refraction was measured. Most of the pseudophakic subjects would view the 20/63 line if they could, at the lower accommodative demands and move up to the largest 20/100 line at higher accommodative demands. If the subject could not see the 20/100 line clearly, measurements could no longer be taken or considered for that subject at that stimulus demand or beyond. Four of the 10 subjects could not complete the testing all the way to 3.50 D.
For the 2.0 m target (0.50 D), the distance chart was brought from 6.0 m to 2.0 m in front of the instruments and adjusted so that the subject would be viewing the lowest line of 20/12.5 (which would be equivalent to approximately 20/40 at this distance). For higher accommodative demands, the near target was mounted on the near-point rod attached on top of the instrument in front of the subject’s line of sight at 1.00 m, 0.67 m, 0.50 m, 0.40 m, 0.33 m, and 0.29 m (corresponding to approximately 1.00 D, 1.50 D, 2.00 D, 2.50 D, 3.00 D, and 3.50 D respectively). Subsequently, 3 refraction measurements were taken for each near-target distance. Similar testing was performed with the autorefractor and the aberrometer.
Similar testing was performed in 5 young phakic subjects with both instruments but using higher stimulus amplitudes up to 4.50 D (2.00, 2.50, 3.00, 3.50, 4.00, 4.50 D) for comparison with the pseudophakic subjects.
Statistical Analysis
For both the aberrometer and the autorefractor, only the spherical components of the refractions were used for analysis. Accommodation was calculated for the objectively measured push-up method by subtracting the refraction measurements at each near distance from the baseline distance refraction as follows: Accommodative response = mean for distance baseline – mean for near stimulus.
Bland-Altman graphs22 were used to compare the mean differences and the limits of agreement (LOA) for the on-axis versus off-axis measurements of each instrument. Stimulus response curves were plotted for the accommodative amplitude testing. For all results reported, statistical significance was set at P <.05.
RESULTS
Subjects
Of the 10 phakic subjects, 6 were men and 4 were women with a mean age of 30.3 years ± 5.74 (SD) (range 24 to 41 years). Of the 5 additional young phakic subjects (accommodative amplitudes measured for comparison with pseudophakic subjects), 2 were men and 3 were women with a mean age of 26.2 ± 4.32 years (range 21 to 32 years). In all 15 phakic subjects, the mean uncorrected refractive error measured by the autorefractor and aberrometer was −2.48 ± 4.06 D (range +4.36 to −7.55 D) and the mean astigmatism, −0.35 ± 0.15 D (maximum −0.60 D).
Of the 10 pseudophakic subjects, 5 were men and 5 were women with a mean age of 66.2 ± 11.23 years (range 43 to 76 years). The mean uncorrected refractive error measured by the autorefractor and aberrometer +0.61 ± 0.75 D (range +1.68 to −0.25 D) and the mean astigmatism, −0.61 ± 0.20 D (maximum −0.94 D). Of the pseudophakic subjects, 5 had Advanced Medical Optics IOLs (SI30NB, SI40NB, SI55NB, AR40e), 3 had Alcon AcrySof IOLs (MA60AC, MA30BA, SN60WF), 1 had a Staar AA4203TL IOL, and 1 had a Pharmacia 912 IOL.
Testing and Measurements
Testing was conducted at a mean of 40.3 ± 36.4 months postoperatively (range 1 to 100 months).
Bland-Altman analysis of on-axis measurements compared with nasal and temporal off-axis measurements in phakic subjects showed a mean difference of 0.17 D or less. The 95% LoA (lines representing the upper and lower bounds representing 95% of the range of the data) were slightly larger for the temporal direction than for the nasal direction (Table 1).
Table 1.
Bland-Altman analysis results comparing off-axis measurements and on-axis measurements with the 2 instruments in 10 phakic subjects.
| Instrument | Direction of 5 Degrees Off Axis |
Mean Difference (D) |
95% LoA (D) |
|---|---|---|---|
| Autorefractor | Temporal | −0.17 | 0.92 |
| Autorefractor | Nasal | −0.08 | 0.57 |
| Aberrometer | Temporal | 0.02 | 0.82 |
| Aberrometer | Nasal | 0.10 | 0.54 |
LoA = limits of agreement
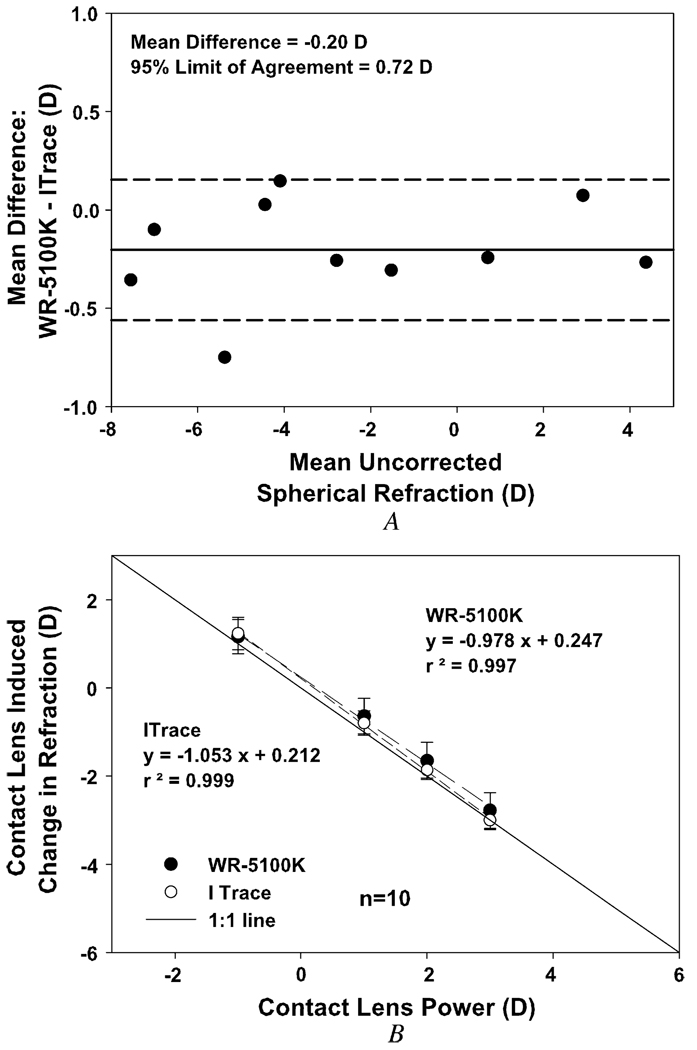
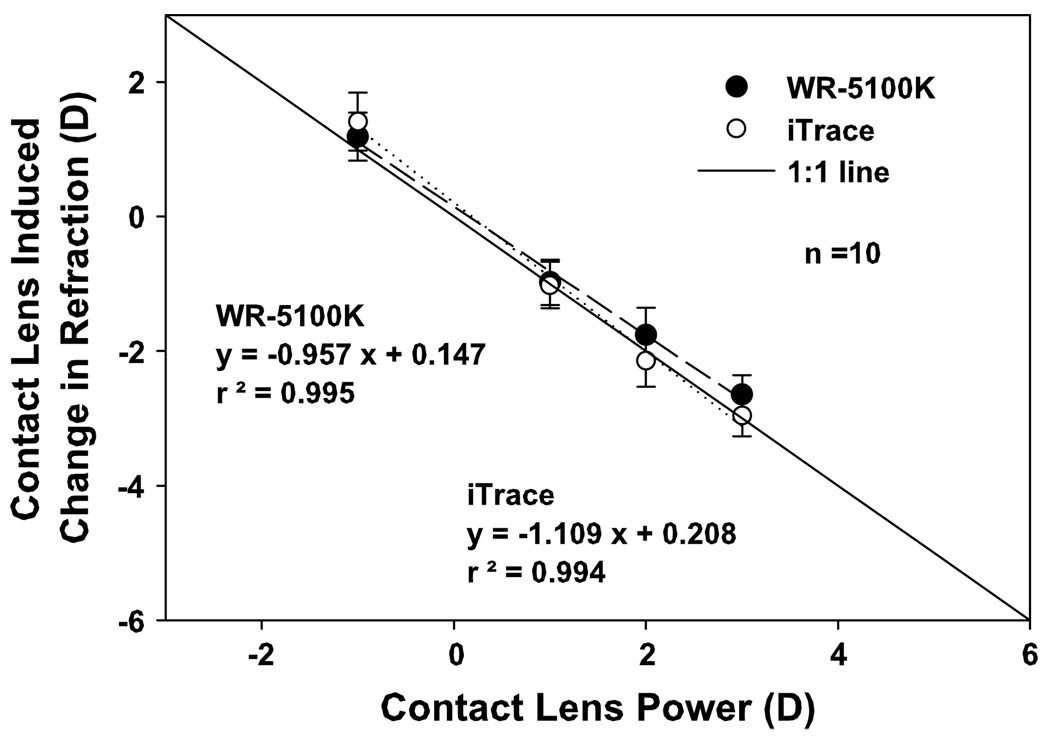
Uncorrected refractive errors in the 10 phakic subjects ranged from +4.25 to −7.55 D with a maximum of −0.94 D of astigmatism. Bland-Altman results comparing the autorefractor and aberrometer measurements show a mean difference of −0.20 D and a 95% LoA of 0.72 D (Figure 1, A). The contact lens–induced refractive errors correlated well with the actual contact lens powers after refractive error was accounted for. When plotted with the 1:1 line, the calibration curve slopes were not significantly different from 1 (autorefractor, P = .92; aberrometer, P = .71) or from each other (F test = 3.79, P = .12) (Figure 1, B).
Figure 1.
A: Bland-Altman graph of the mean difference between the autorefractor and the aberrometer in uncorrected spherical refractive error in 10 phakic subjects. B: Contact lens calibration of the autorefractor and the aberrometer in 10 young phakic subjects. All subjects but 1 were experienced contact lens wearers.
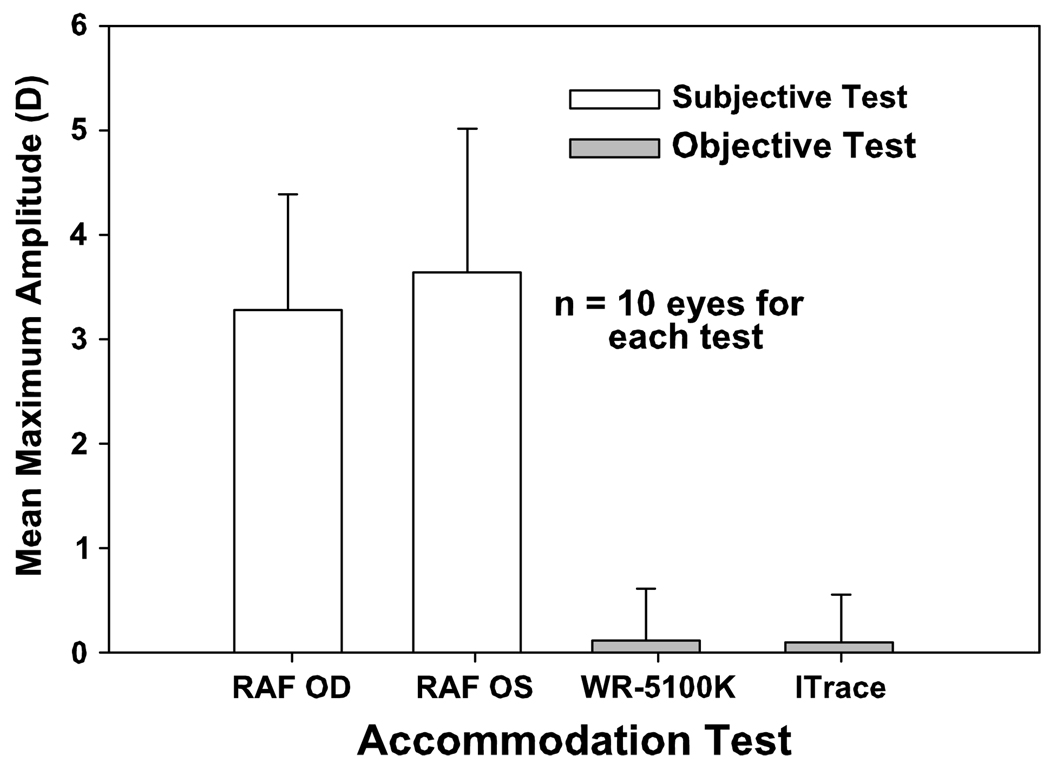
The maximum accommodative amplitudes in the pseudophakic subjects measured with subjective push-down testing with the RAF rule (mean RAF) was 3.28 ± 1.11 D for the right eye, and 3.64 ± 1.38 D for the left eye. The maximum monocular accommodative amplitude measured with objective testing using the autorefractor and aberrometer showed a mean of 0.11 ± 0.50 D for the autorefractor and 0.10 ± 0.47 D for the aberrometer (Figure 2). Objectively measured amplitudes were not significantly different from 0.00 D (autorefractor, P = .56; aberrometer, P = .56).
Figure 2.
Mean maximum amplitudes recorded from subjective push-down testing versus objective accommodation measurement in 10 standard monofocal pseudophakic subjects (OD = right eye; OS = left eye).
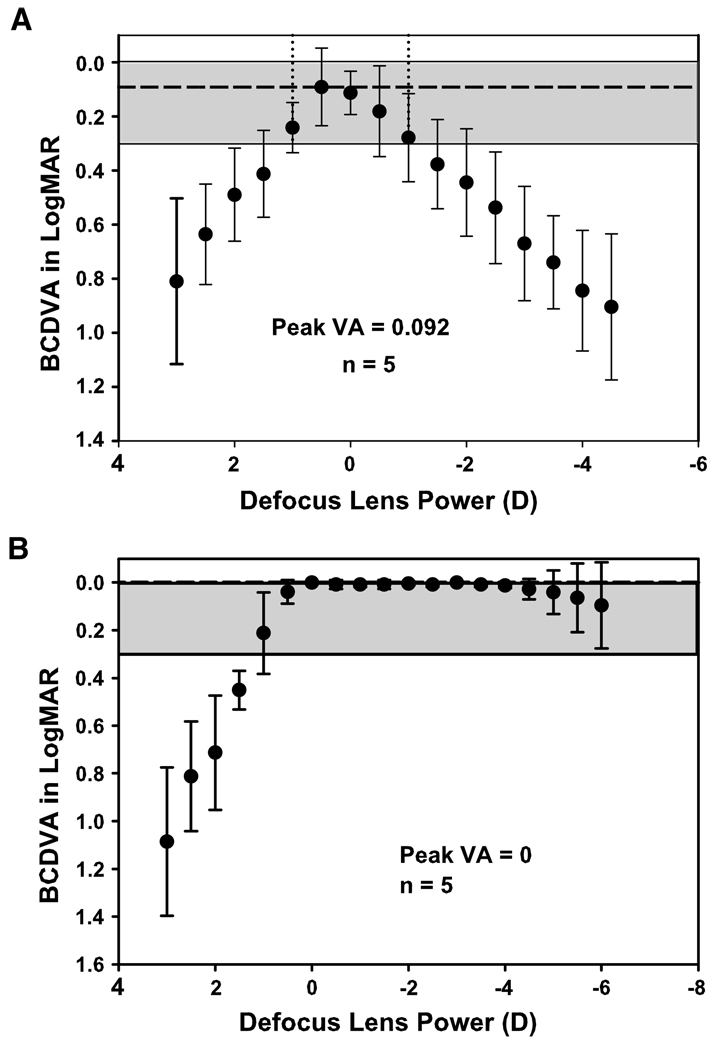
Defocus curves for the pseudophakic subjects who had no accommodation showed a 2.00 D range of distance-corrected visual acuity better than 20/40 (0.30 logMAR). For young phakic subjects with good accommodative abilities, the range was greater than 7.00 D (Figure 3).
Figure 3.
A: Defocus curve from 10 pseudophakic subjects measured behind a phoropter with lens powers ranging from +3.00 to −4.50D in −0.50 D steps. The vertical dashed lines represent the range of distance-corrected visual acuities better than 20/40 (0.30 logMAR), which is represented by the gray area. B: Defocus curve from 5 young phakic subjects measured behind a phoropter with lens powers ranging from +3.00 to −4.50 D in −0.50 D steps. The gray area represents the range of distance-corrected visual acuity better than 20/40 (0.30 logMAR) (BCDVA = best corrected distance visual acuity; Peak VA = mean best starting visual acuity for this population).
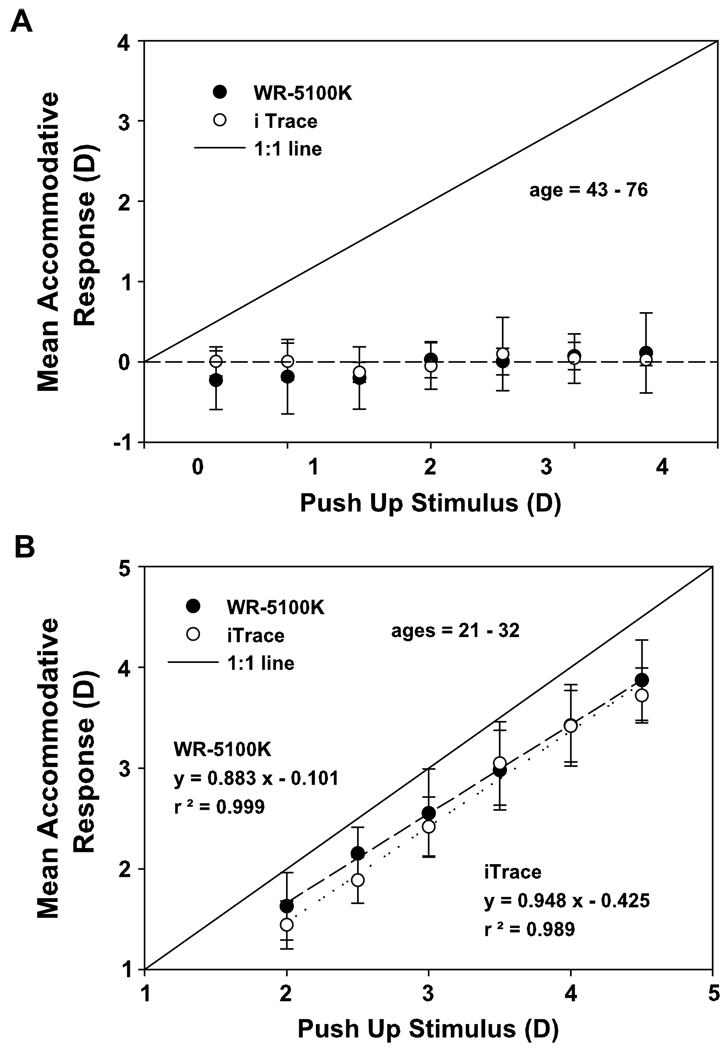
Objective accommodative testing of pseudophakic subjects showed, on average, no significant increase in response amplitude with accommodative effort for all stimulus amplitudes. The autorefractor showed a slight hyperopic shift at the lower stimulus amplitudes; that is, below 2.00 D (mean −0.23 ± 0.37 D) (Figure 4, A). The aberrometer measurements of 1 pseudophakic subject could not be made due to pupils smaller than 2.7 mm. The mean standard deviation of the measurements from all subjects was approximately 0.50 D, which is larger than the resolution of the instruments. Because subjects had different IOLs, were of different ages, and had different distance refractive error and postoperative time, responses differed slightly between subjects. Comparison of the spherical equivalent amplitudes (graph not shown) and the spherical refraction component (Figure 4, A) showed no significant difference (autorefractor: F = 3.96, P = .054; aberrometer: F = 0.312, P = .74).
Figure 4.
A: Accommodative stimulus response curve for 10 pseudophakic subjects measured with the autorefractor and aberrometer (n = 10 for stimuli up to 1.00 D; n = 8 for stimuli up to 1.50 D; n = 6 for stimuli beyond 1.50 D). B: Accommodative stimulus response curve for 5 young phakic subjects measured with the autorefractor and the aberrometer.
Accommodative responses measured in 5 young subjects with the aberrometer and autorefractor for stimuli up to 4.50 D showed linear stimulus/response functions with the expected lag of accommodation (Figure 4, B). The mean standard deviation of the accommodative amplitude measurements from all stimuli of the phakic subjects was slightly smaller than that of the pseudophakic subjects (pseudophakes: autorefractor = 0.10 D, aberrometer = 0.16 D; phakic subjects autorefractor = 0.09 D, aberrometer = 0.11 D). In this study, only the spherical component of the accommodation response was considered. An analysis comparing the accommodative responses determined from spherical equivalent versus those determined from sphere alone for the 5 subjects showed no significant difference (graph not shown) (autorefractor: F = 0.84, P = .48; aberrometer: F = 1.86, P = .23).
Contact lens calibration in the pseudophakic subjects showed that the slopes for both instruments were not significantly different from 1 (autorefractor: P = .82; aberrometer: P = .59) (Figure 5).
Figure 5.
Contact lens calibration of autorefractor and aberrometer in 10 pseudophakic subjects. Refractive errors ranged from −2.25 to +2.50 D with ≤1.25 D of cylinder. Only 2 subjects were experienced contact lens wearers.
DISCUSSION
With the growing interest in determining whether it is possible to restore accommodation to the presbyopic eye with accommodating IOLs, objective accommodation measurements are essential to understand the accommodative capabilities of these IOLs. This study tested the efficacy and capabilities of a commercially available autorefractor and aberrometer to perform objective accommodation measurements in pseudophakic eyes. The pseudophakic subjects tested had standard monofocal IOLs; thus, no accommodation was expected. However, testing with these instruments and protocols in pseudophakic subjects showed that the protocols are appropriate and that such measurements can be done in pseudophakic eyes, even fairly long after surgery. Therefore, objective testing of this nature should be a routine part of clinical studies that evaluate accommodating IOLs so that their accommodative performance can be determined. The results show the subjectively measured accommodative responses from the subjective push-down test, the range of subjectively measured near acuities of 20/40 or better from the defocus curve testing, and the significantly lower objectively measured accommodative amplitudes that are expected in pseudophakic subjects with standard monofocal IOLs. These findings can serve as a reference when using these tests in pseudophakic eyes with a standard monofocal IOL and when determining what improvements might be achieved with accommodating IOLs.
Several recent clinical evaluations of patients with accommodating IOLs4–6,23 did not include objective measurements of accommodation. Only 1 of the studies acknowledged the need for objective accommodation measurements and suggested that the objective methods are more challenging than is immediately obvious. Certainly, challenges (eg, bright Purkinje image reflexes) may exist with IOLs, and these challenges may be more difficult with dual-optic IOLs than single- optic IOLs. However, as shown in our study and in previous studies,9–11 although the measurements take a little longer in pseudophakic eyes than in phakic eyes, it is possible to perform objective accommodation measurements in pseudophakic eyes.
During the testing performed in the present study, when the subjects’ eyes became dry (from constant staring at the targets and from being an older population [8 out of 10 were ≥60 years old]), the autorefractor occasionally gave erroneous measurements; that is, more cylinder than expected. In such cases, artificial tears were instilled and the measurements repeated. Studies of wavefront errors show that the integrity of the tear film can have an effect on the optical quality of the eye and that instilling artificial tears improves the wavefront error in dry-eyed individuals.24 The mean standard deviation of the accommodative amplitude measurements from all stimuli was slightly greater in the pseudophakic group than in the phakic group. This is likely due to a combination of the different IOLs, ocular dryness, and possibly pupil size. Minimizing possible sources of measurement noise is important because the amount of accommodative amplitudes available in pseudophakic eyes is likely to be small.
Although the accommodation testing included rigorous alignment procedures, the off-axis viewing tests in the phakic subjects showed very small mean differences due to off-axis viewing. Therefore, neither instrument appears to be affected by modest deviations in gaze angle. Thus, objective accommodation testing would be accomplished more rapidly without the rigorous alignment procedures, but without loss of accuracy. Similar testing of another autorefractor (FR 5000, Grand Seiko Co., Ltd.) for variations due to proximity of the instrument to the eye showed variations of 0.10 D or less within a range of 10.0 mm toward and 15.0 mm away from the subject’s eye.25 The accuracy of these instruments appears to be largely unaffected by small misalignments.
In a previous study,18 a trial lens calibration was used to test for accuracy of WR-5100K autorefractor measurements. Calibration of an instrument is ideally performed using a standard model eye or by comparing measurements on the same eye with 2 different instruments. 26 Comparing measurements from 2 instruments in eyes with a wide range of refractive errors also offers an opportunity to verify accuracy.27 However, model eyes may not be available, clinicians may not have 2 instruments, and it is time consuming to measure many patients with a wide range of refractive errors; therefore, contact lens calibrations in a limited number of patient eyes provide a simple and useful alternative. Due to the vertex distance of a lens from the eye, trial lenses (especially of higher powers) cause minification or magnification at the pupil plane, which causes inaccuracies in the calibration procedure with the iTrace aberrometer (Win-Hall D, et al. IOVS 2006; 47:ARVO E-Abstract 5847). Therefore, calibrations with both instruments were performed with soft contact lenses. Accommodative amplitudes expected of accommodating IOLs might be up to 3.00 D or more; therefore, the range of soft contact lenses used was chosen to encompass this range. The contact lens calibrations in phakic and pseudophakic subjects show that both instruments measure these refractive changes accurately when they are present and would therefore measure accommodative changes accurately.
A comparison of the performance of the 2 instruments used to measure accommodation is important. The autorefractor and aberrometer use very different measurement methods. A previous study20 found them to be comparable in measuring accommodation in phakic eyes. The results in this study show them to be comparable in their calibrations and in the measurements of pseudophakic eyes. A previous study28 compared the precision of wavefront refraction measured with the Complete Ophthalmic Analysis System (Wavefront Sciences) with that of subjective refraction and autorefraction (measured with the AR-800 (Nidek) and KR-8000 (Topcon) systems in phakic eyes and found that the wavefront refractions were not as precise as autorefraction, although the difference was not clinically significant. Therefore, as long as the instruments are suitable for accommodation testing, wavefront aberrometers and autorefractors can be used.
The limitations of subjective testing of accommodation should be understood. Standard clinical push-up testing of accommodation is quick, taking fewer than 5 minutes to perform, and it is easily administered. A defocus curve obtained using a phoropter is also easy to perform and takes approximately 15 minutes in most cases. Although both provide a measure of functional near vision, neither measures true accommodation, namely the dioptric change in the power of the eye. These subjective tests typically overestimate the objectively measured accommodative response by 2.00 to 3.00 D, as shown here and in previous studies.18,20 If subjective tests are not performed with appropriate caution, this can result in further overestimation of the recorded responses. The subjective push-up test (as opposed to the push-down test) and defocus curve testing are susceptible to overestimation because the subjects might memorize the visual acuity charts. When the subject starts each test viewing the charts in clear focus (ie, chart at distance and viewed through plano power in the phoropter) and then the chart is moved toward the subject in the push-up test or the same chart is read through lenses in the defocus curve tests, the only endpoint is perceived blur. However, if the near target is placed at the nose (initially blurred) and pushed away until clear focus is perceived (the push-down test), the subject does not know what the target is at the start. Similarly, with the defocus curve, if the letter chart is varied between lenses and/or the lens order in the phoropter is randomized, the subject will not be able to guess the letters based on the image that was viewed immediately before.7 In this study, the letters were varied between each new lens presentation in the defocus curve testing and the push-down test was performed. Although the objective accommodation measurements in the pseudophakic subjects showed no significant accommodation, the pushdown test results suggest that these eyes have about 3.50 Davailable and that if the 20/40 cutoff from the defocus curves is used, approximately 2.00 D (in the myopic range) is available. Therefore, even using the more conservative subjective tests significantly overestimates the objectively measured accommodative amplitudes. There should be no expectation that the subjective and objective results are comparable or correlated because they measure 2 completely different things. Objective tests measure only the dioptric change in the power of the eye, whereas subjective tests measure some complex combination of the effects of ocular aberrations, depth of field of the eye, psychophysical blur perception, as well as any dioptric change in the power of the eye. The objectively measured results in pseudophakic subjects who are not expected to have any accommodation are quite different from those in young phakic subjects who have accommodation.
Although distance-corrected near visual acuity testing and subjective tests are good measures of functional vision, they are not sufficient for assessing whether accommodation is present. This study shows that it is readily possible to do objective accommodation measurements in pseudophakic subjects and that through rigorous evaluation and application of both subjective and objective tests, the presence of true accommodation can be evaluated in pseudophakic eyes.
Acknowledgments
Funded in part by NIH Loan Repayment Program (Dr. Win-Hall), P30 EY07551 Core Grant, and a grant from Eyeonics, Inc., Aliso Viejo, California, USA (Dr. Glasser).
Mark Dehn and AIT Industries, Inc. provided the WR-5100K. Jason Cole, PhD, Jill Autry, OD, and Tad Wade, MD, assisted in subject recruitment.
Biography

First author:
Dorothy M. Win-Hall, OD
University of Houston, College of Optometry, Houston, Texas, USA
Footnotes
No author has a financial or proprietary interest in any instrument or method mentioned.
AG serves as a consultant to and has financial interests in several companies with interests in accommodative IO Ls and accommodation restoration concepts, none of which are the subject matter of this study.
Presented in part at the annual meeting of the Association for Research in Vision and Ophthalmology, Fort Lauderdale, Florida, USA, May 2006 and the annual meeting of the American Academy of Optometry, Denver, Colorado, USA, December 2006.
REFERENCES
- 1.Keeney AH, Hagman RE, Fratello CJ. Dictionary of Ophthalmic Optics. Newton, MA, Butterworth-Heinemann. 1995;1345 [Google Scholar]
- 2.Millodot M. Dictionary of Optometry and Vision Science. 4th ed. Oxford, UK: Butterworth-Heinemann; 1997. [Google Scholar]
- 3.Findl O, Leydolt C. Meta-analysis of accommodating intraocular lenses. J Cataract Refract Surg. 2007;33:522–527. doi: 10.1016/j.jcrs.2006.11.020. [DOI] [PubMed] [Google Scholar]
- 4.McLeod SD. Optical principles, biomechanics, and initial clinical performance of a dual-optic accommodating intraocular lens (an American Ophthalmological Society thesis) [Accessed October 23, 2008];Trans Am Ophthalmol Soc. 2006 104:437–452. Available at: http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=1809902&;blobtype=pdf. [PMC free article] [PubMed] [Google Scholar]
- 5.Ossma IL, Galvis A, Vargas LG, Trager MJ, Vagefi MR, McLeod SD. Synchrony dual-optic accommodating intraocular lens. Part 2: pilot clinical evaluation. J Cataract Refract Surg. 2007;33:47–52. doi: 10.1016/j.jcrs.2006.08.049. [DOI] [PubMed] [Google Scholar]
- 6.Sanders DR, Sanders ML. Visual performance results after Tetraflex accommodating intraocular lens implantation. Ophthalmology. 2007;114:1679–1684. doi: 10.1016/j.ophtha.2006.12.017. [DOI] [PubMed] [Google Scholar]
- 7.Gupta N, Naroo SA, Wolffsohn JS. Is randomisation necessary for measuring defocus curves in pre-presbyopes? Cont Lens Anterior Eye. 2007;30:119–124. doi: 10.1016/j.clae.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 8.Dogru M, Honda R, Omoto M, Toda I, Fujishima H, Arai H, Matsuyama M, Nishijima S, Hida Y, Yagi Y, Tsubota K. Early visual results with the 1CU accommodating intraocular lens. J Cataract Refract Surg. 2005;31:895–902. doi: 10.1016/j.jcrs.2004.10.062. [DOI] [PubMed] [Google Scholar]
- 9.Langenbucher A, Huber S, Nguyen NX, Seitz B, Gusek-Schneider GC, Küchle M. Measurement of accommodation after implantation of an accommodating posterior chamber intraocular lens. J Cataract Refract Surg. 2003;29:677–685. doi: 10.1016/s0886-3350(02)01893-x. [DOI] [PubMed] [Google Scholar]
- 10.Wolffsohn JS, Hunt OA, Naroo S, Gilmartin B, Shah S, Cunliffe IA, Benson MT, Mantry S. Objective accommodative amplitude and dynamics with the 1CU accommodative intraocular lens. [Accessed October 23, 2008];Invest Ophthalmol Vis Sci. 2006 47:1230–1235. doi: 10.1167/iovs.05-0939. Available at: http://www.iovs.org/cgi/reprint/47/3/1230. [DOI] [PubMed] [Google Scholar]
- 11.Wolffsohn JS, Naroo SA, Motwani NK, Shah S, Hunt OA, Mantry S, Sira M, Cunliffe IA, Benson MT. Subjective and objective performance of the Lenstec KH-3500 “accommodative” intraocular lens. Br J Ophthalmol. 2006;90:693–696. doi: 10.1136/bjo.2006.090951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abbott ML, Schmid KL, Strang NC. Differences in the accommodation stimulus response curves of adult myopes and emmetropes. Ophthalmic Physiol Opt. 1998;18:13–20. [PubMed] [Google Scholar]
- 13.Hazel CA, Cox MJ, Strang NC. Wavefront aberration and its relationship to the accommodative stimulus-response function in myopic subjects. Optom Vis Sci. 2003;80:151–158. doi: 10.1097/00006324-200302000-00011. [DOI] [PubMed] [Google Scholar]
- 14.McClelland JF, Saunders KJ. The repeatability and validity of dynamic retinoscopy in assessing the accommodative response. Ophthalmic Physiol Opt. 2003;23:243–250. doi: 10.1046/j.1475-1313.2003.00113.x. [DOI] [PubMed] [Google Scholar]
- 15.Ostrin LA, Glasser A. Accommodation measurements in a pre-presbyopic and presbyopic population. J Cataract Refract Surg. 2004;30:1435–1444. doi: 10.1016/j.jcrs.2003.12.045. [DOI] [PubMed] [Google Scholar]
- 16.Plainis S, Ginis HS, Pallikaris A. The effect of ocular aberrations on steady-state errors of accommodative response. [Accessed October 23, 2008];J Vis. 2005 5:466–477. doi: 10.1167/5.5.7. Available at: http://www.journalofvision.org/5/5/7/ [DOI] [PubMed] [Google Scholar]
- 17.Tsukamoto M, Nakajima T, Nishino J, Hara Y, Uozato H, Saishin M. The binocular accommodative response in uncorrected ametropia. Optom Vis Sci. 2001;78:763–768. doi: 10.1097/00006324-200110000-00016. [DOI] [PubMed] [Google Scholar]
- 18.Win-Hall DM, Ostrin LA, Kasthurirangan S, Glasser A. Objective accommodation measurement with the Grand Seiko and Hartinger coincidence refractometer. Optom Vis Sci. 2007;84:879–887. doi: 10.1097/OPX.0b013e3181559ace. [DOI] [PubMed] [Google Scholar]
- 19.Wold JE, Hu A, Chen S, Glasser A. Subjective and objective measurement of human accommodative amplitude. J Cataract Refract Surg. 2003;29:1878–1888. doi: 10.1016/s0886-3350(03)00667-9. [DOI] [PubMed] [Google Scholar]
- 20.Win-Hall DM, Glasser A. Objective accommodation measurements in prepresbyopic eyes using an autorefractor and an aberrometer. J Cataract Refract Surg. 2008;34:774–784. doi: 10.1016/j.jcrs.2007.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Adler P. RAF near point rule modification. Ophthalmic Physiol Opt. 2004;24:469–470. doi: 10.1111/j.1475-1313.2004.00220.x. [DOI] [PubMed] [Google Scholar]
- 22.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 23.Macsai MS, Padnick-Silver L, Fontes BM. Visual outcomes after accommodating intraocular lens implantation. J Cataract Refract Surg. 2006;32:628–633. doi: 10.1016/j.jcrs.2006.01.027. [DOI] [PubMed] [Google Scholar]
- 24.Montés-Micó R. Role of the tear film in the optical quality of the human eye. J Cataract Refract Surg. 2007;33:1631–1635. doi: 10.1016/j.jcrs.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 25.Wolffsohn JS, Ukai K, Gilmartin B. Dynamic measurement of accommodation and pupil size using the portable Grand Seiko FR-5000 autorefractor. Optom Vis Sci. 2006;83:306–310. doi: 10.1097/01.opx.0000216059.54932.3a. [DOI] [PubMed] [Google Scholar]
- 26.Applegate RA, Marcos S, Thibos LN. Aberrometry: clinical and research applications [editorial] Optom Vis Sci. 2003;80:85–86. doi: 10.1097/00006324-200302000-00001. [DOI] [PubMed] [Google Scholar]
- 27.Wang L, Wang N, Koch DD. Evaluation of refractive error measurements of the WaveScan WaveFront system and the Tracey Wavefront aberrometer. J Cataract Refract Surg. 2003;29:970–979. doi: 10.1016/s0886-3350(02)01967-3. [DOI] [PubMed] [Google Scholar]
- 28.Pesudovs K, Parker KE, Cheng H, Applegate RA. The precision of wavefront refraction compared to subjective refraction and autorefraction. Optom Vis Sci. 2007;84:387–392. doi: 10.1097/OPX.0b013e31804f81a9. [DOI] [PubMed] [Google Scholar]