Abstract
In this article we systematically and critically review the Chinese and English language literature on human immunodeficiency virus (HIV)-related studies in Yunnan Province, Southwestern China. Yunnan Province had the first Chinese HIV outbreak and is still the worst affected area in the nation. Since 1989, HIV infection has extended from injecting drug users into the general population through sexual transmission. Since the economic reform of the 1980s, changed social norms and increased migration have spawned increases in HIV-related risk behaviors such as drug use and commercial sex work. A smaller size of “bridge” populations and lower sexual contact rates between persons in “bridge” and general populations may explain the slower expansion of the HIV epidemic in Yunnan compared to nearby Southeast Asian nations. In 2004, women in antenatal care had a 0.38% HIV prevalence province wide, although >1% infection rates are seen in those counties with high injection drug rates. Patterns of drug trafficking have spread the unusual recombinant HIV subtypes first seen in Yunnan to far-flung regions of China. Increased efforts of Yunnan’s HIV control program are correlated with an improved general HIV awareness, but risk behaviors continue at worrisome rates. Future efforts should focus on changing risk behaviors, including harm reduction and condom promotion, especially among the “bridge” groups. The resurgence of commercial sex work in Yunnan, and the high frequency of workers migrating into provinces far from home and family are all sociocultural factors of considerable importance for future HIV and sexually transmitted disease control in China.
Keywords: HIV, Prostitution, Drug abuse, Epidemiology, China, Yunnan
Introduction
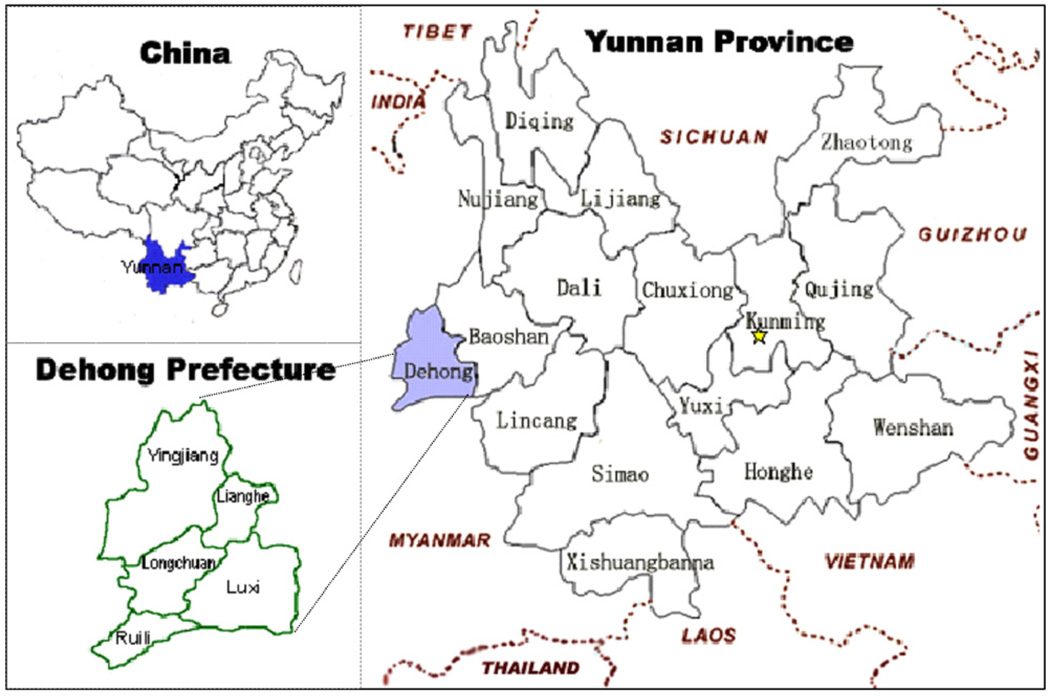
Yunnan Province is located in southwestern China and borders Myanmar, Laos, and Vietnam (Fig. 1). Ethnic minorities account for 33.4% of Yunnan’s population of 43 million, compared to 8.4% of the entire nation (National Bureau of Statistics of China, 2001). Yunnan experienced the first human immunodeficiency virus (HIV) outbreak recognized in China (Ma et al., 1990) and has had the greatest number of HIV-infected people of any province in the 1989–2004 period (China Ministry of Health (MOH) & UN Theme Group (UNTG), 2004). Little is known about the network dynamics of sexual or parenteral risk within the social, cultural, and political environment of Yunnan. At the early epidemic stage, a “Ruili Epidemic Pattern” was described, with HIV concentrated in injection drug users (IDUs) near Ruili City (Fig. 1), where the first HIV outbreak was identified (Xia, 1995). From 1989–2004, however, HIV transmission has expanded geographically and into the general population through heterosexual transmission.
Fig. 1.
Map of Yunnan Province.
We systematically and critically reviewed the Chinese and English language literature on HIV-related studies in Yunnan. The goal of our review was to understand the transmission dynamics and behavioral antecedents of the HIV epidemic in Yunnan by seeking lessons learned from the first 16 years of HIV spread to guide future public health policies and promulgate effective prevention and care programs.
Methods
We searched for all articles published about HIV/acquired immunodeficiency syndrome (AIDS) and referencing the Yunnan Province in three databases: (1) PUBMED for both English and Chinese-language articles; (2) Chongqing VIP Information (CQVIP); and (3) China National Knowledge Infrastructure (CNKI). Key references cited in pertinent articles were also obtained. We obtained reports from the Yunnan Center for Disease Control and Prevention and the Chinese Center for Disease Control and Prevention. Since HIV was identified in Yunnan in 1989, database searches included human studies from August 1989 to August 2005. Our search terms included topics (HIV, sexually transmitted infection (STI) or disease (STD), drug abuse, sexual behavior, and condom) and locations (China, Yunnan, Kunming, Dehong, Ruili, and Longchuan). The inclusion criteria were relevant type of study, i.e., population-based epidemiological and behavioral HIV/AIDS/STI studies from Yunnan were considered. These included molecular epidemiology studies, studies on knowledge, attitudes, practices, and behaviors (KAPB), health care utilization, and review articles. All papers identified were screened by a fluently bilingual reviewer (YX) for relevance. Key information was extracted, including study design, outcome, duration, region, and population.
Results
There were 230 papers in Chinese and 30 in English that met our inclusion criteria (Table 1). Among these, epidemiological studies accounted for 53%, KAPB studies for 26%, and preventive interventional studies for 9%.
Table 1.
Summary of the HIV/STI-related literature related to Yunnan
| Year | Epidemiology | KAPBa | Intervention | Othersb | Total |
|---|---|---|---|---|---|
| 1989–1993 | 13 | 3 | 0 | 0 | 16 |
| 1994–1997 | 34 | 11 | 4 | 2 | 51 |
| 1998–2001 | 41 | 22 | 5 | 7 | 75 |
| 2002–2005c | 51 | 32 | 14 | 21 | 118 |
| Total | 139 | 68 | 23 | 30 | 260 |
KAPB = knowledge, attitudes, practices, and behaviors.
Includes studies on HIV-related health services and review articles.
Through August 2005.
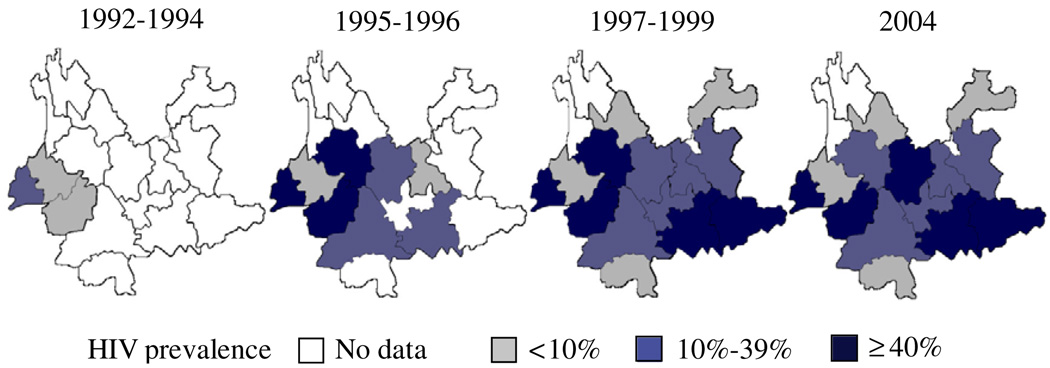
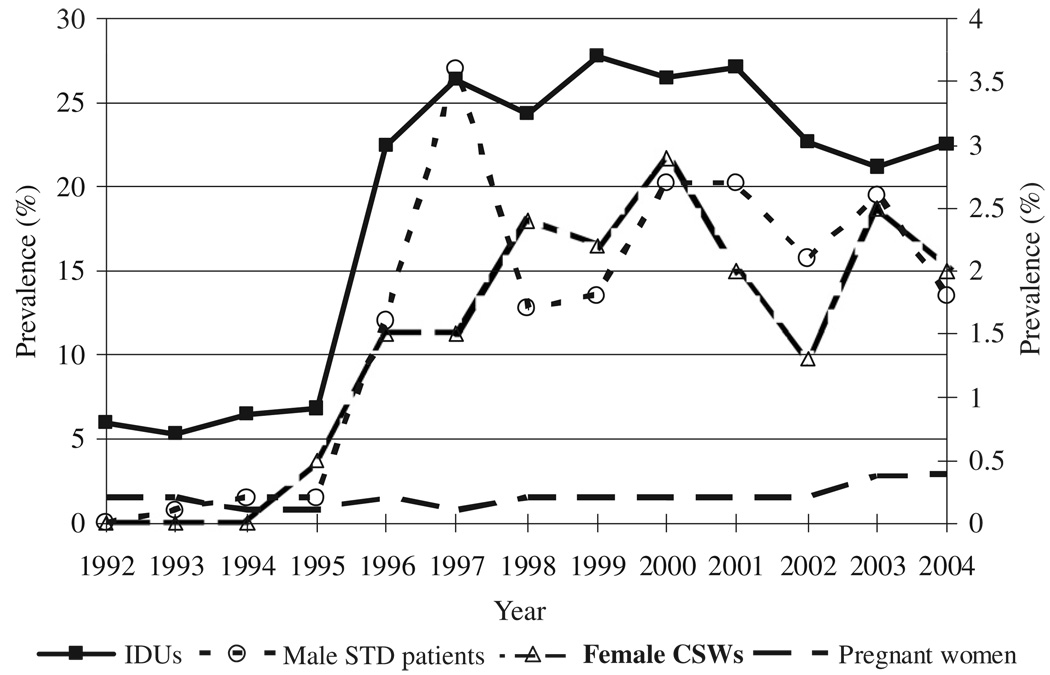
Evolution of the HIV epidemic
The first 146 HIV positive cases from IDUs in Ruili City, in Yunnan Province, represented China’s first recognized HIV outbreak (Fig. 1) (Ma et al., 1990). The 1989 HIV/AIDS outbreak served as the transition from the epidemic’s “introduction phase,” in which the HIV infection was associated mostly with foreign contacts, to its “concentrated spread phase” (MOH & UNTG, 1997). Through 1994, the HIV epidemic was mostly concentrated among IDUs. HIV was rarely identified among other risk groups or in other areas (Cheng et al., 1995). By 1995 the Yunnan HIV epidemic had undergone a substantial expansion, all over Yunnan and into other provinces as well (Lu et al., 2004), marking the transition from the “concentrated spread phase” into the “expansion phase” of the epidemic in China (MOH & UNTG, 1997). The HIV prevalence among IDUs in Yunnan increased from less than 7% to 22.4% in 1995 (Lu et al., 2004). As HIV continued to expand to other areas, the average prevalence among IDUs fluctuated between 21.2% and 27.8% through 2004 (Fig. 2 and Fig. 3) (Lu et al., 2004, 2005). Although needle sharing during drug injection was and still is the main mode of HIV transmission, the proportion of HIV reports attributable to sexual transmission increased steadily from 5.3% in 1996 to 11.8% in 2004 (Cheng et al., 1995; Lu et al., 2005). HIV seroincidence rates among pregnant women fluctuated between 0.14% and 0.25% from 1992 to 2002, rising to 0.37% in 2003 and 0.38% in 2004 (Fig. 3) (Lu et al., 2004, 2005). Prevalence among pregnant women in Dehong has exceeded 1% since 2003 (Lu et al., 2004; Yunnan CDC, 2005). HIV prevalence among persons obtaining premarital HIV tests (typically young, reproductive-aged adults) was as high as 0.6–0.8% in 2001–2003 (Hesketh et al., 2003; Kong et al., 2004). It should be noted that all these figures come from sentinel surveillance in higher risk counties and therefore overestimate the prevalence in the whole province.
Fig. 2.
HIV prevalence among IDUs in Yunnan Province, 1992–2004.
Figure 3.
HIV prevalence among high-risk populations in Yunnan Province (Note: HIV prevalence among IDUs on the left axis, HIV prevalence among other populations on the right axis).
HIV spread in Yunnan occurs from rural to urban areas and from border communities to those deeper inside China. The epidemic has also shifted from ethnic minorities to the majority Han population. Since infection has increased over time due to sexual risk, the male-to-female ratio has dropped from 40:1 in 1990 to 3.8:1 in 2004 (Lu et al., 2005; Zhang, Cheng, Jia, & Zhang, 1999).
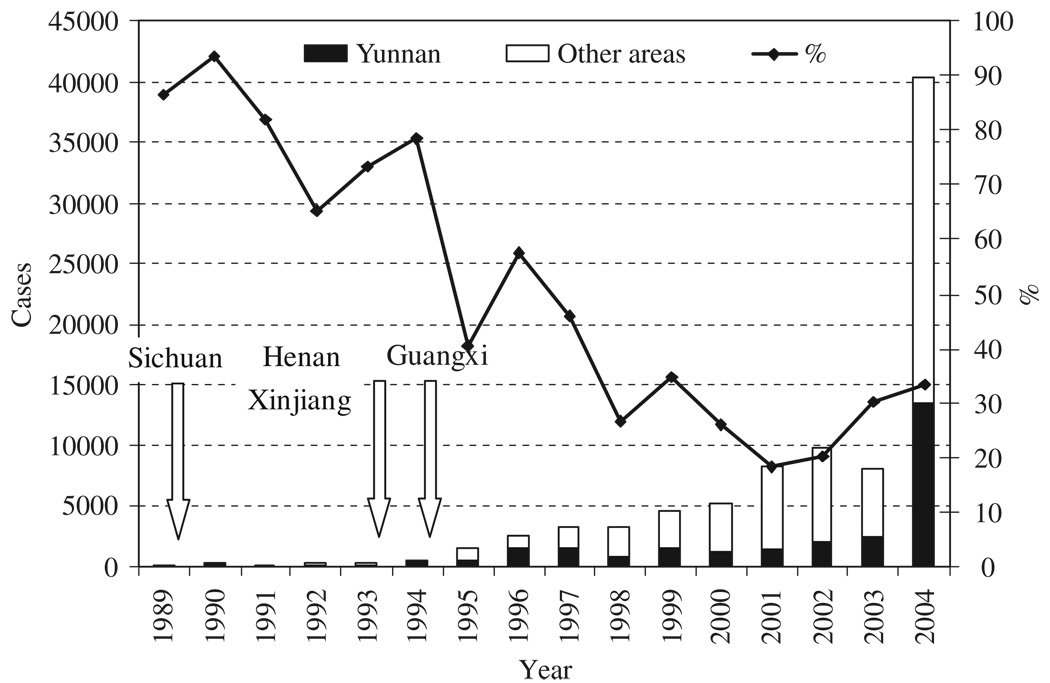
By the end of 2004, Yunnan had cumulatively reported 28,391 HIV infections. Among them, 1223 had developed AIDS, and 744 had died. From 1989 to 2004, Yunnan reported the highest number of annual HIV/AIDS cases in Mainland China (excluding Hong Kong, Macao, and Taiwan) (Fig. 4). In terms of the rate of cumulative cases from 1989 to 2004 inclusive, we calculated that Yunnan also ranks the first in China (66 cases/100,000), followed by Xinjiang (51 cases/100,000) and Henan (27 cases/100,000) (Chinese CDC, 2004a, b;Lu et al., 2005). More than 80,000 persons were estimated to be living with HIV in Yunnan in 2003 (Yunnan CDC, 2004b).
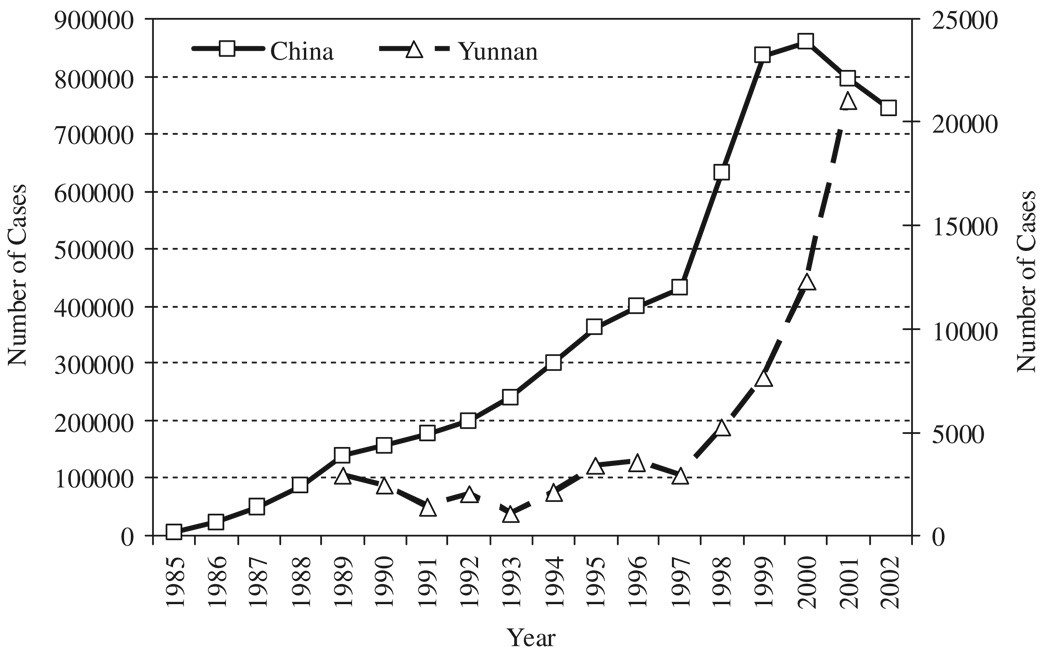
Fig. 4.
Annual reported HIV cases in Yunnan Province and China and the percentage of Yunnan HIV cases among China#x02019;s cases (Note: 1. the arrows indicate the years that other high HIV prevalent provinces/regions found their first HIV infections; 2. the increase of HIV cases in 2004 is due to the large-scale HIV testing program in Yunnan Province).
Molecular epidemiology
In 1990–1993, subtype B was prevalent (Shao et al., 1994). In 1992, HIV subtype C emerged (Shao et al., 1996) and accounted for a third of the specimens sequenced in two studies in 1994 (a total of 90 specimens) (Li, Zheng, & Zhang, 1996; Teng et al., 1995). HIV subtype E was also identified in Yunnan in 1993 (Cheng, Zhang, Capizzi, Young, & Mastro, 1994). In early 2000, subtypes C, E, and B′ (B′ is a Thai variant of subtype B) were identified, as well as three recombinant forms of B and C (CRF07_BC, CRF08_BC, and a unique recombinant form of B′ and C) and a recombinant form of A and E (CRF01_AE) (Li et al., 2004; Yang et al., 2002; Yang et al., 2003; Yin et al., 2003). HIV viruses sequenced in Sichuan, Xinjiang, and Guangxi were found to have many gene sequences identical to those of the previously identified Yunnan strains but had somewhat lower genetic divergence, suggesting that viruses in these areas were likely introduced from Yunnan (Shao, Zhao, Yang, Zhang, & Gong, 1999; Yang et al., 2003; Yin et al., 2003). Yunnan is thus thought to be the origin of many of the currently circulating HIV strains in China.
Risk factors for HIV transmission
Illicit drug use
Yunnan is a major point of entry of drugs from the “Golden Triangle” and is used for major drug trafficking routes (Beyrer et al., 2000; Dong & Wu, 1997). The resurgence of drug use in Yunnan began mostly with opium in the early 1980s (Dong & Wu, 1997; Wu, Zhang, & Duan, 1996; Zhao et al., 2004). Since 1990, heroin use has increased in Yunnan, and there has also been a shift from nasal (“chasing the dragon”) to injection use (Dong & Wu, 1997; Luo et al., 2003; McCoy & Lai, 1997; McCoy et al., 2001; Sha et al., 1993; Wu, Zhang, & Duan, 1996). In Longchuan, a retrospective cohort study found that 72% of 161 non-IDUs in 1991 had become injectors by 1994, an annual incidence of drug injection of 20% (Wu et al., 1996). In contrast, in Kunming City, the prevalence of injection among drug users was high early (80% in 1992) and has been maintained near this level subsequently (Luo, Yang, Li, & Zhu, 2002; Zhang, Cheng, & Duan, 1994). Syringe sharing is very common (>70%) among IDUs and has been documented repeatedly since the early 1990s (Cheng et al., 2003; Liu, Lian et al., 2001; Wu, Zhang, & Li, 1999; Zheng, 1991; Zheng & Wang, 2003). In the counties bordering Myanmar, drug use has been disproportionately high among minority ethnic residents. In contrast, drug users in Kunming City are most often of the majority Han ethnic group (Jia, Luo, Zhang, & Ren, 2003; Sha et al., 1993). There are few female drug users in the rural border areas (<4%) (Zhang et al., 1996; Zheng, 1991; Zheng, Zhang, & Chen, 1995), but women represent about one-third of drug users in urban Yunnan (Jia et al., 2003; Luo et al., 2003; Sha et al., 1993). Most drug users in Yunnan are unmarried (62%) and ages 21–40 (88%) (Luo et al., 2003). Drug treatment programs have been based in the criminal justice system and rely mostly on detoxification (McCoy & Lai, 1997). However, the Chinese government has recently expanded methadone maintenance treatment programs in recognition of high relapse rates from traditional models of intervention (MOH & UNTG, 2004).
Unsafe sexual behavior and STIs
Due to greater internal migration within China, many young Chinese men leave their homes (Pan, 1999; Tucker et al., 2005). This fuels the sex work industry, as does tourism. Since sex work remains illegal, the sex industry has developed in many covert forms (Pan, 1999). Studies conducted between 1995 and 2000 indicate that over 80% of girls who worked in entertainment and service establishments (e.g., hair salon, bar, dancing and karaoke hall, or massage salon) (Guo et al., 2002; Wu et al., 1997), as well as 45% of females who worked in service businesses along a main national highway (e.g., hair salon, karaoke bar, hotel, and restaurant) (Jin et al., 2004), were involved in the sex trade. Sex work is typically perceived as a transient occupation—means for a young women to make money to start a business or help their families before they settle down to have their own families (Hesketh, Zhang, & Qiang, 2005).
In Yunnan, more than 80% of female sex workers (FSWs) had fewer than 8 years of education, and more than 70% of them were of Han Chinese (Jin et al., 2004; Lu, Jia, Luo, & Zhang, 2003; Luo et al., 2005; Wu et al., 1997). Behavioral surveillance among 362 FSWs in a popular tourist city (Baoshan) in Yunnan in 2002 suggested that the average customer throughput was 6 per week per worker, ranging from 2 per week for higher class FSWs, to 11 per week for lower class FSWs (Lu et al., 2003).
Although male homosexual behavior has only rarely been reported in Yunnan, 1.6% of drug users reported having had sex with men in surveys from Yunnan and Sichuan Provinces (Liu et al., 2003).
Several studies suggest that Chinese male clients were very reluctant to use condoms (Cheng et al., 2004; Luo Yang, & Jing, 2005; Luo et al., 2005). Behavioral surveillance in 1996–1999 demonstrated that 39% of Kunming residents used condoms during commercial sex (Ma et al., 2001). An interesting corroboration of this estimate came from a province-wide survey among 5898 FSWs in 2004 which reported that 37% of the FSWs insisted on condom use with their commercial partners but that only 18% did so with their steady partners (Luo et al., 2005). A 2002 behavioral survey found an even lower condom use rate among Kunming male IDUs: 13% of them used condoms with their regular partners, 21% did so with commercial partners, and 27% used condoms with other non-regular partners (Lu et al., 2003).
Yunnan reported its first documented STI patient in 1984 (Xia, 1994). The reported numbers of STI cases represented a 41% annual increase during the 1992–2001 period (Fig. 5) (Liu, 2003). True numbers of STI cases are currently estimated to be 10–15 times higher than the reported numbers (Liu, Zhang et al., 2001). A 2000 study found disturbingly high STI prevalence rates among 505 surveyed FSWs in Kunming (WHO Regional Office for the Western Pacific, National Center for STD and Leprosy Control & MOH, 2001): 58.6% had chlamydia (by PCR diagnosis), 43.2% had trichomoniasis (PCR), 37.8% had gonorrhea (PCR), and 9.5% had syphilis (screened by RPR and confirmed by TPHA). Fully, 85.7% of these FSWs had at least one infection, and 35.4% had more than one infection.
Figure 5.
Annual reported STI cases in Yunnan Province and China (Note: number of national STI cases on the left axis, number of Yunnan STI cases on the right axis. Although the first STI found in Yunnan Province was in 1984, the available Yunnan STI data is from 1989 to 2001).
Multiple risk behaviors
Risk behaviors such as drug use and multiple sexual partners tend to cluster with one another. A cohort of 1548 young male farmers in Longchuan in the early 1990s revealed that those who had pre- or extramarital sex were 1.5 times more likely to initiate drug use than those who did not (Wu et al., 1999). A 2002 Kunming study found that the percentage of persons who had ever had more than 1 sex partner was 82% among drug users and 18% among other local residents (our calculated p<0.001) (Luo, Yang et al., 2005).
Migration
Yunnan has a large-scale migrant or transient population, accounting for an estimated 9% of the provincial population (Mo, Wu, & Yuan, 2004). A study in Kunming found that a higher proportion of the floating population than of local residents had multiple sex partners (28% vs. 18%; our calculated p = 0.02) (Luo et al., 2005). Another study in Ruili reported that 9% of migrant construction workers had visited FSWs in the past year (Lu et al., 2003). The prevalence of HIV (0.5%), gonorrhea (0.5%) and chlamydia (9.3%) were also found among miners in Yunnan Province because of their heterosexual risk (Zhao et al, 2005).Migrants return to their hometowns periodically (e.g., for Spring Festival); thus, STI/HIV acquired elsewhere may be spread to partners.
Minority ethnicity
Before 1995, more than 77% of HIV infections in Yunnan were among Jingpo and Dai people (Cheng et al., 1995). Jingpo ethnic people accounted for 9% of all new HIV infections in 2004 and only 0.3% of the general population (30:1 ratio), while Dai ethnic people accounted for 7% of all new HIV infections and 2.5% of the population (2.8:1 ratio) (Lu et al., 2005). A cohort study of male farmers in Longchuan during the early 1990s found that Jingpo men were twice as likely to initiate drug use (Wu et al., 1999) and that Jingpo men were six times as likely to share syringes as other ethnic groups (Wu et al., 1996).
Low HIV knowledge and discrimination
Studies in Dehong in 1994 found that more than half of the young farmers had never heard of HIV and that drug users were not aware of their HIV risk (Wu, Zhang, & Dong, 1998; Zheng et al., 1995). Behavioral surveillance has demonstrated a significant increase in HIV knowledge in the general population since 1998; more than 80% of the people surveyed knew the principal HIV transmission routes (Ma et al., 2001; Zhang et al., 2001). However, rural residents and minority ethnic people still had lower HIV knowledge (Duo, Li, Dong, & Jiang, 2003; Huang, Li, Xiao, Li, & Huang, 2002; Yu et al., 2003). Discriminatory attitudes towards HIV-infected persons remain deeply rooted. A 2002 survey revealed that 30% of doctors did not want to serve HIV-infected patients and that 75% of surveyed pregnant women did not want to be close to HIV-infected people (Hesketh, Duo, Li, & Tomkins, 2005).
Response to HIV/AIDS
Compared to other regions, Yunnan has a relatively effective surveillance system because it has the greatest number of sentinel surveillance sites and the largest proportion of population surveyed. HIV surveillance in Yunnan dates from 1986 and now includes sentinel surveillance, cross-sectional surveys, case finding, and behavioral surveillance (Yunnan CDC, 2004a). An estimated 173,549 persons have been tested for HIV within the sentinel surveillance system from 1992 to 2003 (Lu et al., 2004).
The Yunnan government has made a strong political commitment to HIV prevention and control. Several policies have been issued by the Yunnan government to support and promote HIV prevention programs, especially “The Regulation of AIDS Prevention and Control in Yunnan,” issued in 2004. This document specified several recommended harm reduction approaches such as needle exchange, condom promotion, and methadone maintenance treatment (Yunnan CDC, 2004a). Behavioral intervention projects have been greatly promoted in Yunnan since the issue of “The Regulation of AIDS Prevention and Control in Yunnan,” in 2004, including pilot projects of needle exchange and methadone maintenance treatment, condom promotion programs, and community-based and educational interventions (Guo et al., 2002; Jia et al., 1999; Jin et al., 2004; Li et al., 2001; Lin et al. 2004; Wu, Detels, Zhang, Li, & Li, 2002; Yunnan CDC, 2004a). The significant increase in HIV awareness among the general population since 1998 suggests some success in the HIV educational programs in Yunnan (Ma et al., 2001). HIV voluntary counseling and testing (VCT) have been provided since 1990. Antiretroviral treatment services started in 2002, and the free treatment program for the poor started in 2004. Yunnan began to provide free VCT to pregnant women and free antiretroviral prophylaxis to HIV positive pregnant women in 2003 (Yunnan, 2004a; Zhu & Wang, 2005).
Despite these efforts, both HIV and STI continue to spread. Although Yunnan has a stronger HIV prevention program than other areas do, daunting obstacles still exist. Current funding and professional capacity are still very limited, restricting the breadth of coverage for prevention and care programs. Uneven access to care and information among the poor, and deeply rooted discriminatory attitudes in the general population, further reduce the access to these expanded HIV/AIDS prevention and care programs. Hence, limited financial and professional resources, combined with a severe HIV/AIDS stigma, inhibit progress in addressing the expanding HIV epidemic in Yunnan (Yunnan CDC, 2004a).
Discussion
Yunnan Province was the first to identify an HIV outbreak in China (excluding Hong Kong, Macao, and Taiwan) and, in 2005, is still likely to have the highest HIV incidence rates in the country. Molecular epidemiology suggests that the Yunnan epidemic is the source of HIV now circulating in the rest of China. Yunnan has played a major role in all three phases of the HIV epidemic in China: the 1989 HIV outbreak in Ruili in Yunnan marked China’s transition from the “introduction phase” to the “concentrated spread phase,” and the expansion of substantial HIV incidence beyond Yunnan’s borders marked the epidemic shift from the “concentrated spread phase” to the “expansion phase” (MOH & UNTG, 1997). Thus, Yunnan can be considered a key HIV epicenter in China.
The Yunnan HIV epidemic began in the late 1980s among rural IDUs of minority ethnic origin living along the border of Myanmar. HIV spread within this community near Ruili for about 6 years (1989–1994)—the so-called Ruili epidemic pattern (Xia, 1995). After the HIV infections were noted in FSW groups in 1995, HIV infections were noted continually, but prevalence among FSWs remained below 3% through 2004 (Lu et al., 2005). In comparison, the first HIV outbreak in nearby Thailand was reported among urban IDUs about one year earlier than in Yunnan; however, the virus spread rapidly into FSWs within just 1 year, with very high HIV prevalence noted (e.g., 44% in Chiang Mai FSWs in 1989) (Punpanich, Ungchusak, & Detels, 2004). Similarly, rapid and severe heterosexual HIV transmission was also observed in Cambodia (Saphonn et al., 2004) and neighboring Myanmar (Thwe, 2004).
Why has heterosexually mediated HIV transmission in Yunnan lagged behind that of its neighboring and nearby nations? Our review led us to suggest several factors related to the nature of the “bridge” populations. The number of FSWs and male customers, although growing in China, may be lower than in nearby nations. The rates of sexual contact and sexual mixing, the frequencies of multiple risk behaviors (e.g., IDU and FSW), and the frequency with which different risk groups mingle may all be comparatively lower in China. The social, cultural, and political environment in China may be less supportive and/or permissive of high-risk personal risk behaviors than in other countries. Although sharing contaminated injecting equipment has high efficiency in HIV transmission anywhere in the world wherever HIV is introduced, the IDU community is comparatively small and isolated in Yunnan Province. With sexual behaviors that are still more conservative in China, heterosexual spread has been less dramatic to date. The existence of clearly defined “bridge” populations, however, gives cause for alarm for the future spread of HIV in Yunnan.
We speculate that the comparatively smaller size of the “bridge” population, the lower number of high-risk sexual encounters, and the lower contact rate between “bridge” and risk populations play an important role in the slower HIV expansion rate from IDUs to FSWs and from FSWs to the general population via male clients. Little work has been done to study the “bridge” population between IDUs and FSWs. Persons with multiple HIV-related risk behaviors, such as the FSWs and their male customers who also share needles for injecting drugs, are of special importance. The lower rates of female IDUs noted in China may also diminish risk for an expanded epidemic. A generic point in public health risk assessment is that risk behaviors are not distributed randomly in populations but tend to cluster with one another and to correlate to individuals’ positions in their social structures. People who have low levels of education or are socially isolated are more likely to engage in a wide range of risk-related behaviors, such as drug use and unsafe sex. Such behavioral responses, patterned by the social structure, have led to the recognition of situations that place individuals “at risk of risks” (Aral, Padian, & Holmes, 2005).
The “bridge” population between the FSWs and the general population is principally their male clients. Although commercial sex is theoretically illegal in all Southeast Asian countries, the commercial sex trade is more widespread in Thailand and Cambodia, for example, than in China. While social norms towards casual sex have changed since the 1980s in China, more than 70% of the general population still opposes casual sex (He, Yang, & Zhang, 2000; Huang et al., 2002; Li et al., 2003). Periodic “yellow crackdown campaigns” (in China yellow is a symbol of prostitution) result in the arrest of FSWs.
In Yunnan only 1.6% of urban residents had visited FSWs in the past month (Ma et al., 2001); and 9% of construction workers had visited FSWs in the past year (Lu et al., 2003); in comparison, around 30% of young men had visited FSWs in the past year in Thailand and Cambodia (De Lay, 2001). Spread from FSWs has been relatively confined to certain risk groups, such as drug users, migrant workers, and traveling businessmen. Thus, the low HIV prevalence among FSWs, the relatively limited “bridge” populations, and the low contact rate may explain the comparatively slower expansion of HIV into the general population in Yunnan compared to Thailand and Cambodia.
We are not sanguine about these observations, however, as several factors may lead to faster future HIV epidemic growth. First, HIV continues to be highly prevalent among IDUs, resulting in a large pool of infected and infectious persons. Second, the sex trade in Yunnan is increasing steadily, and condom use in commercial sex is still low, suggesting that commercial sex workers can contribute to epidemic spread in the future. Third, the large flow of migrants through Yunnan may also catalyze HIV spread. Although a high proportion of HIV infections will continue to occur among IDUs, we believed that heterosexual spread will continue to increase and will become the principal mode of HIV transmission in Yunnan in the near future in the absence of more effective prevention measures.
Given increasing political commitment within the national and provincial governments and the support of international organizations, a variety of HIV/AIDS/STI prevention programs have been carried out in Yunnan, although joint HIV/tuberculosis programs lag behind in development. The general increase in HIV awareness suggests that these programs have been somewhat successful. However, further HIV education is needed to expand the programs into rural areas and reach out to the minority ethnic groups, where HIV knowledge lags. Innovative interventions that seek to change risk behaviors among key “bridge” populations are needed, as demonstrated by ongoing high syringe/needle sharing among IDUs and low condom use rates by FSWs. More must be learned about men who have sex with men. More must be learned about Chinese attitudes toward condom use, especially among the male customers of FSWs. Better strategies must be developed to increase condom use and acceptability among FSWs and their male customers. Population coverage of harm reduction programs is very limited. Needle exchange and methadone pilot projects that were started in 2003 are a vital first step and are already producing promising information related to their effectiveness and their applicability in the Chinese context. Expanded HIV treatment opportunities may reduce HIV stigma and reduce infectiousness of HIV-infected persons. Yunnan Province has been at the leading edge of the HIV epidemic; we hope it will be leading prevention innovation and application as well.
Acknowledgements
I gratefully acknowledge support from the AITRP/FIC Program at the University of Alabama at Birmingham (TWOO103-5, S. Kristensen, subcontract PI).
Contributor Information
Yan Xiao, Email: xiaoyan@chinaaids.cn.
Sibylle Kristensen, Email: sibylle@uab.edu.
Jiangping Sun, Email: jpsun@chinaids.org.cn.
Lin Lu, Email: ynll60@public.km.yn.cn.
Sten H. Vermund, Email: sten.vermund@vanderbilt.edu.
References
- Aral SO, Padian NS, Holmes KK. Advances in multilevel approaches to understanding the epidemiology and prevention of sexually transmitted infections and HIV: An overview. Journal of Infectious Diseases. 2005;191 Suppl. 1:S1–S6. doi: 10.1086/425290. [DOI] [PubMed] [Google Scholar]
- Beyrer C, Razak MH, Lisam K, Chen J, Lui W, Yu X. Overland heroin trafficking routes and HIV-1 spread in south and south-east Asia. AIDS. 2000;14(1):75–83. doi: 10.1097/00002030-200001070-00009. [DOI] [PubMed] [Google Scholar]
- Cheng H, Zhang J, Capizzi J, Young NL, Mastro TD. HIV-1 subtype E in Yunnan, China. Lancet. 1994;344(8927):953–954. doi: 10.1016/s0140-6736(94)92304-3. [DOI] [PubMed] [Google Scholar]
- Cheng H, Zhang J, Jia M, Kuo J, Zhang Y, Bi X, et al. The study on HIV epidemic and trend in Yunnan Province. Journal of Chinese AIDS/STD Prevention and Control. 1995;1(2):8–11. [Google Scholar]
- Cheng F, Chen H, Li JH, Zhang L, Hu H, Zhang J, et al. SASH survey on high risk behaviors of IDUs in four cities of Yunnan and Sichuan. Chinese Journal of Drug Dependence. 2003;12(4):56–60. [Google Scholar]
- Cheng F, Chen H, Luan R, Zhang L, Hu H, Zhang J, et al. Study on condom use and its determinant among commercial sex workers. Chinese Journal of Public Health. 2004;20(1):72–73. [Google Scholar]
- Chinese CDC. Henan reconfirms HIV epidemic situation. 2004a September 29; 〈 www.chinaids.org.cn〉.
- Chinese CDC. Xinjiang’s HIV epidemic: the number of infections ranking the 4th nationwide. 2004b December 27; 〈 www.chinaids.org.cn〉. [Google Scholar]
- De Lay PR. The global AIDS pandemic: Why the differences? 2001 July 20; 〈 www.iipi.org〉. [Google Scholar]
- Dong L, Wu Z. Dynamics in drug use in Longchuan County, Yunnan Province during 1982 to 1995. Chinese Journal of Drug Dependence. 1997;8(1):22–23. [Google Scholar]
- Duo L, Li H, Dong Y, Jiang Z. Knowledge about AIDS of the Lahus in Yunnan Province. Chinese Journal of Health Education. 2003;19(7):516. [Google Scholar]
- Guo J, Yang G, Li C, Huo G, Wu T, Ding Y, et al. Analysis on an HIV/STD interventional program among female servants in Baoshan area of Yunnan. Journal Dermatology and Venereology. 2002;24(3):F003. [Google Scholar]
- He Z, Yang T, Zhang L. A survey of general population's knowledge about HIV/AIDS in Yunnan Province. Modern Preventive Medicine. 2000;27(4):512–514. [Google Scholar]
- Hesketh T, Huang X, Wang Z, Xing Z, Cubitt DW, Tomkins AM. Using the premarital examination for population-based surveillance for HIV in China: A pilot study. AIDS. 2003;17(10):1574–1576. doi: 10.1097/01.aids.0000076266.76134.23. [DOI] [PubMed] [Google Scholar]
- Hesketh T, Duo L, Li H, Tomkins AM. Attitudes to HIV and HIV testing in high prevalence areas of China: Informing the introduction of voluntary counselling and testing programmes. Sexually Transmitted Infections. 2005;81(2):108–112. doi: 10.1136/sti.2004.009704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hesketh T, Zhang J, Qiang D. HIV knowledge and risk behaviour of female sex workers in Yunnan Province, China: Potential as bridging groups to the general population. AIDS Care. 2005;17(8):958–966. doi: 10.1080/09540120500100676. [DOI] [PubMed] [Google Scholar]
- Huang Y, Li J, Xiao X, Li X, Huang Y. A research of cognition and related factors on HIV/AIDS of rural women in four counties of Yunnan Province. Soft Science of Health. 2002;16(3):13–15. [Google Scholar]
- Jia M, Kang Y, Kong X, Liang Y, An J, Li Q, et al. A behavior intervention research on AIDS prevention at entertainment places in a County of Yunnan Province. Journal of Chinese AIDS/STD Prevention and Control. 1999;5(2):62–64. [Google Scholar]
- Jia M, Luo H, Zhang X, Ren L. Analysis on surveillance result of the first round BSS among intravenous drug users in Yunnan Province. Disease Surveillance. 2003;18(7):249–252. [Google Scholar]
- Jin Y, Yin G, Bao W, Liu C, He L, Mao B, et al. Effect of health education and behavioral intervention of AIDS/STD among female attendants of roadside inn. Chinese Journal of Health Education. 2004;20(1):17–20. [Google Scholar]
- Kong X, Su J, Zhang Y, Hou W, Kang Y, Wang J. Analysis on HIV/AIDS surveillance among premarital examination receptors in Chengjiang County, Yunnan. Soft Science of Health. 2004;18(4):188–189. [Google Scholar]
- Li D, Zheng X, Zhang G. Study on the distribution of HIV-1 C subtype in Ruili and other counties, Yunnan, China. Chinese Journal of Epidemiology. 1996;17(6):337–339. [PubMed] [Google Scholar]
- Li G, Chen Z, Chen Z, Wei FL, Mei S, Huang Y, et al. Study on the distribution of human immunodeficiency virus-1 subtypes in different regions of China and mother-to-child transmission. Chinese Journal of Epidemiology. 2004;25(12):1013–1018. [PubMed] [Google Scholar]
- Li J, Luo J, Yang F, Zhu H. Evaluation on peer education program among injecting drug users. Chinese Journal of Epidemiology. 2001;22(5):334–336. [PubMed] [Google Scholar]
- Li N, Zhang H, He P, Zhao H, Tu X, Zhang L, et al. The changes in sexual perception and behaviors of college students in Yunnan Province. Chinese Journal of School Health. 2003;24(2):114–116. [Google Scholar]
- Lin P, Fan ZF, Yang F, Wu ZY, Wang Y, Liu YY, et al. Evaluation of a pilot study on needle and syringe exchange program among injecting drug users in a community in Gangdong, China. Zhonghua Yu Fang Yi Xue Za Zhi. 2004;38(5):305–308. [PubMed] [Google Scholar]
- Liu C, Zhang C, He L, Liang J, Sheng Q, Li W, et al. Investigation on STD underreport situation from surveillance system in Yunnan. Chinese Journal of Leprosy and Skin Diseases. 2001;17(1):32. [Google Scholar]
- Liu Z, Lian Z, Mu Y, Zhou W, Wang Z, Guli Z, et al. Knowledge and risk behavior on HIV/AIDS among drug addicts in four areas in China. Chinese Journal of Drug Dependence. 2001;10(1):48–52. [Google Scholar]
- Liu H. Analysis of STD epidemic trend in the last ten years in Yunnan. Journal of Dermatology and Venereology. 2003;25(2):57–59. [Google Scholar]
- Liu Z, Cao J, Liu X, Lian Z, Zhao C, Zhao D, et al. Epidemiological study on the high risk factors of HIV/AIDS among drug abusers in Sichuan and Yunnan Provinces. Chinese Journal Drug Dependence. 2003;12(3):204–214. [Google Scholar]
- Lu L, Jia M, Luo H, Zhang X. Analysis of the first round of HIV behavioral surveillance in Yunnan. Disease Surveillance. 2003;18(11):414–417. [Google Scholar]
- Lu L, Jia M, Zhang X, Luo H, Ma Y, Fu L, et al. Analysis for epidemic trend of acquired immunodeficiency syndrome in Yunnan Province of China. Zhonghua Yu Fang Yi Xue Za Zhi. 2004;38(5):309–312. [PubMed] [Google Scholar]
- Lu L, Jia MH, Lu JY, Luo HB, Zhang XP, Ma YL, et al. Analysis of HIV/AIDS prevalence in Yunnan province. Journal of Chinese AIDS/STD Prevention and Control. 2005;11(3):172–174. 164. [Google Scholar]
- Luo J, Yang F, Li J, Zhu H. Knowledge of attitude towards HIV/AIDS and risk behavior of 306 drug addicts in Kunming. Chinese Journal of Drug Dependence. 2002;11(4):62–64. [Google Scholar]
- Luo J, Li J, Li H, Yang F, Li P, Zheng J, et al. An investigation on substance abuse situation among drug users in Yunnan. Chinese Journal of Drug Dependence. 2003;9(6):5–9. [Google Scholar]
- Luo H, Yang X, Jing K. A comparison analysis on HIV high risk behaviors among different populations in urban areas—taking Kunming City as an example. Chinese Public Health Management. 2005;202(4):248–251. [Google Scholar]
- Luo J, Li X, Cai L, Yang Z, Li X, Lei Y. Investigation and analysis of epidemiology about unlicensed prostitutes’ knowledge of AIDS behavior in Yunnan province. Soft Science of Health. 2005;19(1):35–37. [Google Scholar]
- Ma Y, Li Z, Zhang K, et al. HIV was first discovered among injection drug users in China. Chinese Journal of Epidemiology. 1990;11(3):184–185. [Google Scholar]
- Ma J, Chen L, Shu G, Wang R, Shen L, He L, et al. Dynamic surveillance of risk behaviors facilitating sexually transmitted disease/acquired immunodeficiency syndrome transmission among permanent residents in Kunming city in 1996–1999. Chinese Journal of Epidemiology. 2001;22(5):323–325. [PubMed] [Google Scholar]
- McCoy CB, Lai S. No pain no gain, establishing the Kunming, China, drug rehabilitation center. Journal of Drug Issues. 1997;27(1):73. [Google Scholar]
- McCoy CB, McCoy HV, Lai S, Yu Z, Wang X, Meng J. Reawakening the dragon: Changing patterns of opiate use in Asia, with particular emphasis on China’s Yunnan province. Substance Use and Misuse. 2001;36(1–2):49–69. doi: 10.1081/ja-100000228. [DOI] [PubMed] [Google Scholar]
- Mo G, Wu Y, Yuan X. Floating population and HIV spreading in Yunnan Province. Population and Economics. 2004;2(143):14–19. [Google Scholar]
- MOH & UNTG. China responds to AIDS. 1997 November [Google Scholar]
- MOH & UNTG. A joint assessment of HIV/AIDS prevention, treatment and care in China. 2004 December 1; [Google Scholar]
- National Bureau of Statistics of China. Bulletin of the fifth national population census in 2000. 2001 March 28; 〈 www.stats.gov.cn〉.
- Pan S. Three “red light districts” in China. Beijing, China: Qunyuan Publishing House; 1999. [Google Scholar]
- Punpanich W, Ungchusak K, Detels R. Thailand’s response to the HIV epidemic: Yesterday, today, and tomorrow. AIDS Education and Prevention. 2004;16(3 Suppl A):119–136. doi: 10.1521/aeap.16.3.5.119.35520. [DOI] [PubMed] [Google Scholar]
- Saphonn V, Sopheab H, Sun LP, Vun MC, Wantha SS, Gorbach PM, et al. Current HIV/AIDS/STI epidemic: Intervention programs in Cambodia, 1993–2003. AIDS Education and Prevention. 2004;16(3 Suppl A):64–77. doi: 10.1521/aeap.16.3.5.64.35522. [DOI] [PubMed] [Google Scholar]
- Sha L, Zhu H, Liu Z, Cheng L, Pan C, Zhang Y. Social investigation of the narcotic in Kunming district. Chinese Social Medicine. 1993;44(1):39–40. [Google Scholar]
- Shao Y, Zhao Q, Wang B, Chen Z, Su L, Zeng Y, et al. Sequence analysis of HIV env genes among HIV-infected drug injecting users in Dehong epidemic area of Yunnan Province, China. Chinese Journal of Virology. 1994;10(4):291–299. [Google Scholar]
- Shao Y, Guan Y, Bi Q, Zeng Y, Zhang J, Zhang Y, et al. Genetic variations and molecular epidemiology of the Ruili HIV-1 strains of Yunnan in 1995. Chinese Journal of Virology. 1996;12(1):9–17. [Google Scholar]
- Shao Y, Zhao F, Yang W, Zhang Y, Gong X. The identification of recombinant HIV-1 strains in IDUs in southwest and northwest China. Chinese Journal of Experimental and Clinical Virology. 1999;13(2):109–112. [PubMed] [Google Scholar]
- Teng Z, Zhu T, Duan Y, Zhang J, Zeng Y, Ho DD. HIV molecular epidemiological analysis among HIV infected persons in Ruili City, Yunnan. Journal of Chinese AIDS/STD Prevention and Control. 1995;1(1):1–5. [Google Scholar]
- Thwe M. HIV/AIDS education and prevention in Myanmar. AIDS Education and Prevention. 2004;16(3 Suppl A):170–177. doi: 10.1521/aeap.16.3.5.170.35524. [DOI] [PubMed] [Google Scholar]
- Tucker JD, Henderson GE, Wang TF, Huang YY, Parish W, Pan SM, et al. Surplus men, sex work, and the spread of HIV in China. AIDS. 2005;19(6):539–547. doi: 10.1097/01.aids.0000163929.84154.87. [DOI] [PubMed] [Google Scholar]
- WHO Regional Office for the Western Pacific, National Center for STD and Leprosy Control & Ministry of Health of China. Prevalence survey of sexually transmitted infections among female sex workers and truck drivers in China (1999–2000) 2001 September; 〈 www.wpro.who.int〉.
- Wu Z, Detels R, Zhang J, Duan S, Cheng H, Li ZR, et al. Risk factors for intravenous drug use and sharing equipment among young male drug users in Longchuan County, south-west China. AIDS. 1996;10(9):1017–1024. doi: 10.1097/00002030-199610090-00013. [DOI] [PubMed] [Google Scholar]
- Wu Z, Zhang J, Duan S. A survey on drug abuse in young males in Longchuan County, Yunnan Province. Zhonghua Yu Fang Yi Xue Za Zhi. 1996;30(6):327–329. [PubMed] [Google Scholar]
- Wu Z, Zhang J, Dong L, Li Z, Wu P, Duan S, et al. Commercial sex establishments and sex workers in Dehong Prefecture, Yunnan Province. Journal of Chinese AIDS/STD Prevention and Control. 1997;3(1):14–16. [Google Scholar]
- Wu Z, Zhang J, Dong L. Relationship between risk-taking behavior and knowledge for HIV infection among young men in Longchuan, Yunnan of China. Chinese Journal of Epidemiology. 1998;32(3):171–173. [PubMed] [Google Scholar]
- Wu Z, Zhang J, Li Z. Risk factors for initiation of drug use among young males in Longchuan, Yunnan. Chinese Journal Epidemiology. 1999;20(1):15–18. [PubMed] [Google Scholar]
- Wu Z, Detels R, Zhang J, Li V, Li J. Community-based trial to prevent drug use among youths in Yunnan, China. American Journal of Public Health. 2002;92(12):1952–1957. doi: 10.2105/ajph.92.12.1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia Z. Analysis on 8638 STD cases from 1989 to 1992 in Yunnan Province. Journal of Dermatology and Venereology. 1994;16(4):48–50. [Google Scholar]
- Xia L. Heterosexual transmitted HIV and the change of “Ruili epidemic pattern” in Yunnan. Journal of Chinese AIDS/STD Prevention and Control. 1995;1(2):19. [Google Scholar]
- Yang R, Xia X, Kusagawa S, Zhang C, Ben K, Takebe Y. On-going generation of multiple forms of HIV-1 intersubtype recombinants in the Yunnan Province of China. AIDS. 2002;16(10):1401–1407. doi: 10.1097/00002030-200207050-00012. [DOI] [PubMed] [Google Scholar]
- Yang R, Kusagawa S, Zhang C, Xia X, Ben K, Takebe Y. Identification and characterization of a new class of human immunodeficiency virus type 1 recombinants comprised of two circulating recombinant forms, CRF07_BC and CRF08_BC, in China. Journal of Virology. 2003;77(1):685–695. doi: 10.1128/JVI.77.1.685-695.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin N, Mei S, Li L, Wei F, Zhang L, Cao Y. Study on the epidemiology and distribution of human immunodeficiency virus-1 and hepatitis C virus infection among intravenous drug users and illegal blood donors in China. Chinese Journal of Epidemiology. 2003;24(11):962–965. [PubMed] [Google Scholar]
- Yu J, Shen J, Yang F, Luo H, Jiang W, Xiong D. A survey on STD/AIDS awareness among people in minority residence area. Chinese Journal of Leprosy and Skin Diseases. 2003;19(6):581–582. [Google Scholar]
- Yunnan CDC. HIV/AIDS epidemic and response of Yunnan. 2004a January [Google Scholar]
- Yunnan CDC. Report on HIV epidemic in Yunnan Province. 2004b
- Yunnan CDC. HIV epidemic in Dehong Prefecture. 2005 [Google Scholar]
- Zhang J, Cheng H, Duan S. Survey on the current situation of epidemic of HIV infection in Yunnan Province. Chinese Journal of Epidemiology. 1994;15(5):259–262. [PubMed] [Google Scholar]
- Zhang J, Zheng X, Cheng H, Chen Y, Duan S, Qu S, et al. An analysis on the risk factors of HIV epidemic in intravenous drug users in Dehong Prefecture of Yunnan Province. Journal of Chinese AIDS/STD Prevention and Control. 1996;2(3):110–113. [Google Scholar]
- Zhang J, Cheng H, Jia M, Zhang Y. Ten years of experience on AIDS control in Yunnan (1989–1998) Chinese Journal of Epidemiology. 1999;20(6):377–380. [Google Scholar]
- Zhang G, Pan S, Yang C, Cheng H, Wang W, Ma Y, et al. A survey on HIV/AIDS awareness among the general population in Yunnan. Soft Science of Health. 2001;15(4):35–36. [Google Scholar]
- Zhao C, Liu Z, Zhao D, Liu Y, Liang J, Tang Y, et al. Drug abuse in China. Annals of the New York Academy of Sciences. 2004;1025:439–445. doi: 10.1196/annals.1316.054. [DOI] [PubMed] [Google Scholar]
- Zhao R, Gao H, Shi X, Tucker JD, Yang Z, Min X, et al. Sexually transmitted disease/HIV and heterosexual risk among miners in townships of Yunnan Province, China. AIDS Patient Care STDS. 2005;19(12):848–852. doi: 10.1089/apc.2005.19.848. [DOI] [PubMed] [Google Scholar]
- Zheng X. A preliminary study on the behavior of 225 drug abusers and the risk factors of HIV infection in Ruili county Yunnan Province. Chinese Journal of Epidemiology. 1991;12(1):12–14. [PubMed] [Google Scholar]
- Zheng X, Wang L. An epidemiology study on HIV transmission through IDU and blood collection or transfusion. Chinese Journal of Epidemiology. 2003;24(11):1057–1059. [Google Scholar]
- Zheng X, Zhang J, Chen Y. A cohort study and KAP investigation of HIV infected persons in Ruili, and other counties in Yunnan, 1994. Chinese Journal of Epidemiology. 1995;16(2):67–70. [PubMed] [Google Scholar]
- Zhu X, Wang X. Analysis of the pilot project for HIV prevention through mother-to-child transmission in Yunnan Province. China Maternal and Child Health Care. 2005;20(12):1430–1431. [Google Scholar]