Abstract
Objectives
To examine whether a weight loss program delivered to one spouse has beneficial effects on the untreated spouse and the home environment.
Methods
We assessed untreated spouses of participants in 3 sites of Look AHEAD, a multi-center randomized controlled trial evaluating the impact of intentional weight loss on cardiovascular outcomes in overweight individuals with type 2 diabetes. Participants and spouses (n=357 pairs) were weighed and completed measures of diet and physical activity at 0 and 12 months. Spouses completed household food and exercise environment inventories. We examined differences between spouses of participants assigned to the Intensive Lifestyle Intervention (ILI) or to enhanced usual care (DSE).
Results
Spouses of ILI participants lost -2.2±4.5 kg vs. -0.2±3.3 kg in spouses of DSE participants (p<.001). In addition, more ILI spouses lost ≥ 5% of their body weight than DSE spouses (26% vs. 9%, p<.001). Spouses of ILI participants also had greater reductions in reported energy intake (p=.007) and percentage of energy from fat (p=.012) than DSE spouses. Spouse weight loss was associated with participant weight loss (p<.001) and decreases in high-fat foods in the home (p=.05).
Conclusion
The reach of behavioral weight loss treatment can extend to a spouse, suggesting that social networks can be utilized to promote the spread of weight loss thus creating a ripple effect.
It is well established that the weights of marital partners are correlated at the start of marriage,1-4 that weight gain after marriage is common,5-7 and that the weights of husbands and wives change in a similar fashion over time.5,8 Although there is increasing evidence that interpersonal relationships can exert a social influence on obesity,9 it is not known whether delivering a weight loss intervention to one spouse has a beneficial effect on the untreated spouse.
There are many reasons to hypothesize that weight loss in one spouse will have a “ripple effect” on the other spouse. If one spouse changes his or her eating and exercise habits, the other spouse might emulate these new health behaviors. Correlations between the diet and exercise patterns of spouses have been reported,3,10 suggesting that spouses model each others' health behaviors. Untreated spouses might also be influenced by cues within the shared home environment. Cross-sectional examinations have found associations between the number of high-fat foods in the home and fat intake,11 fruit and vegetable availability and intake of these foods,12, 13 and exercise equipment availability and physical activity.14 Behavioral weight loss treatment includes recommendations to change the home food and exercise environment to prompt healthy behaviors.15 To the extent to which such changes are made, the untreated spouse should demonstrate improvements in diet, physical activity, and weight similar to the treated spouse.
Reports from the cardiovascular disease and cancer literatures indicate that health behavior interventions can have a ripple effect on spouses.16-19 In the Women's Health Trial, for example, untreated husbands of participants assigned to a low-fat intervention reported consuming less fat and losing more weight than untreated husbands of control group participants.18 However, none of the prior interventions focused on weight loss and none included measured weights of spouses.
The present study prospectively examined the influence of behavioral weight loss treatment on untreated spouses and the home environment in 3 sites of Look AHEAD (Action for Health in Diabetes),20 a multicenter randomized controlled trial evaluating the long-term impact of intentional weight loss interventions on cardiovascular outcomes in overweight individuals with type 2 diabetes. We hypothesized that untreated spouses of participants assigned to the intensive lifestyle intervention (ILI) would lose more weight and make more changes in their diet and exercise than untreated spouses of participants assigned to an enhanced usual care program (DSE; Diabetes Support and Education); that changes in weight and corresponding behaviors would be correlated between participants and untreated spouses; and that changes in the shared home food and exercise environment would be related to improvements observed in untreated spouses.
Methods
Participants
During the Look AHEAD screening process, participants at 3 clinical sites (The Miriam Hospital, University of Minnesota, University of Alabama at Birmingham) who indicated they were married or living with a significant other were asked to participate in this ancillary study. There were no specific eligibility requirements for spouses other than a willingness to participate in the research. Both partners were required to sign consent forms approved by each site's Institutional Review Board and we certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research. Participants were paid $20 for completing each assessment and spouses were paid $25 for completing each assessment.
Intervention
The ILI was modeled after the Diabetes Prevention Program (DPP)21 intervention and was designed to produce a weight loss of ≥ 7% of body weight and increase physical activity to ≥ 175 minutes per week of moderately intense activity.22 During months 1-6, ILI participants received 3 group meetings and 1 individual session per month; this contact decreased to 2 group meetings and 1 individual session per month in months 7-12. Treatment included training in core behavioral skills such as self-monitoring, problem-solving, goal setting, and relapse prevention. Two meetings in this first year focused on stimulus control, with one lesson addressing physical cues (e.g., storing food out of sight) and the other addressing social cues (e.g., how to avoid tempting foods at a party). Spouses were not formally involved in treatment and were not required or expected to attend group meetings; however, ILI participants were taught ways to enhance social support for their weight loss efforts (e.g., how to communicate assertively with family members about desired recipe modifications; how to involve friends and family members in their exercise routines). DSE participants were offered 3 informational group meetings per year that provided basic information on diabetes, nutrition, and physical activity. Spouses were not formally involved in treatment and were not required or expected to attend these meetings. Strategies for enlisting social support were not discussed in this treatment arm.
Measures
The following measures were completed prior to randomization and at 1-year by participants and spouses, unless noted.
Demographic characteristics
Basic demographic information was assessed at baseline.
Weight and Height
Weight was measured on a digital scale in light-weight clothing. Height was measured on a wall-mounted stadiometer.
Dietary intake
Dietary intake was assessed using a self-administered 130-item food frequency questionnaire similar to the dietary assessment used in DPP.21 We examined daily energy intake and percent of energy from fat over the 6-month recall period.
Physical activity
The Paffenbarger Activity Questionnaire (PAQ)24 was used to estimate energy expended in overall leisure time activity in the past week including activities of light (5 kcal/min), medium (7.5 kcal/min), and high (10 kcal/min) intensity.
Weight control practices
At one year, spouses indicated whether they tried to lose weight and/or joined an organized weight control program in the past year. They also indicated whether they used any of 24 strategies to control their weight including healthy strategies (e.g., self-weighing), dietary modifications, strategies to increase physical activity, and unhealthy strategies (e.g., fasting).
Household food inventory
A questionnaire to assess household food availability was modified from Raynor et al.25 based upon the 60-item Block Food Frequency Questionnaire.26 It included 26 common food categories that represented items high in fat (> 45% energy from fat – 14 items; e.g., cookies) or low in fat (< 18% energy from fat – 12 items; e.g., apples). These items were included because behavioral weight control participants are encouraged to change the availability of high and low-fat foods in their homes to promote adherence to their dietary prescription. Spouses completed this measure at home. They were instructed to check all places where food might be stored and indicate whether each food category was available regardless of amount on that day. Total number of food categories available in the home was calculated, as well as the number of high-fat and low-fat food categories.
A subset of participants (n=156) also completed the food inventory. At baseline and 1-year, there was strong agreement between participant and spouse reports on the total number of foods (r=.67 and .70, p<.001), high-fat foods (r=.72 and .77, p<.001), and low-fat foods (r=.59 and .56, p<.001). Paired t-tests revealed no mean differences between participant and spouse reports at baseline or 1-year follow-up.
Exercise environment
The Exercise Environment Questionnaire, a 14-item measure with high test-retest and inter-rater reliability,14 was completed by spouses and used to assess the amount of exercise equipment available in the home.
Statistical analyses
Data were analyzed using Statistical Package for the Social Sciences (SPSS for Windows, version 14.0, SPSS Inc., Chicago, IL, USA). Baseline group differences were examined using Chi Square or independent t-tests. Time-related changes were analyzed using analyses of variance for repeated measures. We ran two models to address missing weight data. The first model included only spouses with weights at baseline and 1-year, while the second model assumed that spouses with missing weight data at 1-year had remained weight stable. Because of the greater attrition in DSE spouses, the intent-to-treat models gave a weight loss advantage to the ILI condition. To be more conservative, we present in the text the models that included only spouses with complete data. Entering the number of household members and days since grocery shopping as covariates in the home environment models did not affect the results and are not presented. Chi Square tests assessed group differences in the use of weight control strategies. Partial correlations controlling for relevant baseline values from both participants and spouses were used to examine associations between participants and spouses in changes in weight and behaviors. Partial correlations controlling for relevant spouse and home environment variables were used to examine relationships between changes in the home environment, weight, and behaviors in spouses.
Results
Of the 607 potentially eligible couples, 357 pairs (58.8%) agreed to participate in this substudy. Baseline characteristics of these Look AHEAD participants and their untreated spouses are presented in Table 1. There were no differences between spouses of ILI participants and spouses of DSE participants on any measures. Overall, 95.8% of participating pairs were married with the remainder cohabiting. Most were heterosexual couples (97.5%), with 9 same-sex pairs participating in the study.
Table 1.
Demographics of participants and untreated spouses by condition
| Participants | Untreated Spouses | |||
|---|---|---|---|---|
| ILI N=188 |
DSE N=169 |
ILI N=188 |
DSE N=169 |
|
| Age | 59.4±6.5 | 60.3±6.9 | 58.6±7.5 | 59.8±9.0 |
| Gender (% Female) | 45.7 | 40.8 | 54.8 | 59.2 |
| Ethnicity (%Caucasian) | 88.3 | 94.7* | 89.4 | 93.5 |
| Education (% attending some college or more) | 75.5 | 80.5 | 66.7 | 69.9 |
| Baseline BMI (kg/m2) | 36.3±5.9 | 35.3±5.4 | 31.0±6.2 | 30.1±6.0 |
| BMI Status | ||||
| Normal weight (%) | -- | -- | 17.0 | 23.1 |
| Overweight (%) | 10.1 | 14.2 | 30.9 | 30.2 |
| Obese (%) | 89.9 | 85.8 | 52.1 | 46.7 |
Significant difference between ILI and DSE participants, p=.033
Ninety percent of spouses completed the 1-year weight assessment with better completion rates in ILI spouses than DSE spouses (94.1% vs 85.2%, p=.005). Spouses who did not complete the 1-year assessment were younger (56.6±7.0 vs. 59.5±8.4 years, p=.053) than those who did complete the assessment but did not differ in initial BMI or other demographic variables.
Weight loss
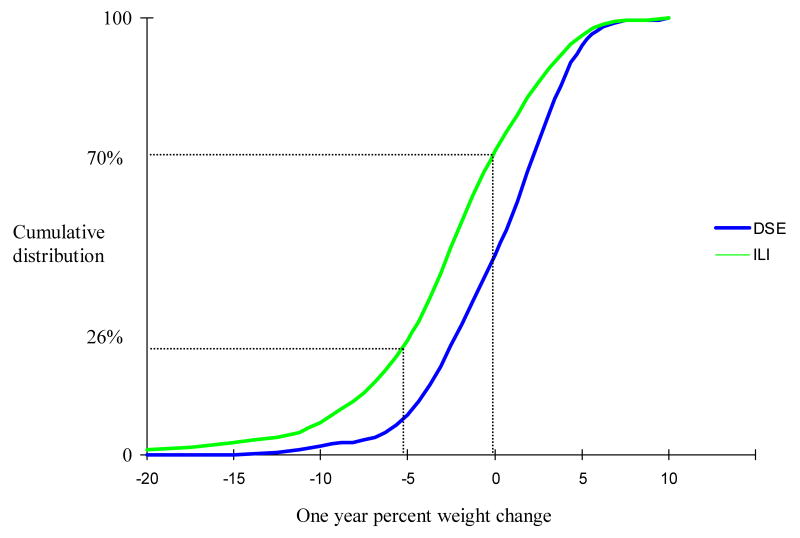
As in the full trial,27 ILI participants in this ancillary study lost more weight than DSE participants during the first year (-9.9±7.6 vs. -1.2±4.9 kg, p<.001). The spouses of ILI participants also lost more weight over the 1-year period than spouses of DSE participants (p<.001), even though they did not receive active intervention. Spouses of ILI participants lost -2.4±4.5 kg or 2.7±4.9% of their body weight versus -0.2±3.3 kg or -0.2±3.8% in spouses of DSE participants. This pattern was not affected by the gender or baseline weight status of the spouse (Table 2). Overall, more ILI spouses lost ≥ 5% of their body weight compared DSE spouses (26.0% vs. 9.0%; p<.001), and more ILI spouses stayed at or below their starting weight than DSE spouses (69.5% vs. 45.8%, p<.001) (Figure 1).
Table 2.
Weights (kg) at baseline and 1-year of untreated spouses (Mean ± SD)
| Intensive Lifestyle Intervention | Diabetes Support and Education Controls | p value ILI spouses vs. DSE spouses |
||||
|---|---|---|---|---|---|---|
| Group | Time | Group × Time | ||||
|
Overall sample (n=357) |
BL | 87.96 ± 19.36 | 83.67 ± 18.51 | .128 | <.001 | <.001 |
| 1 Year | 85.58 ± 19.21 | 83.43 ± 18.38 | ||||
| Untreated husbands (n=154) | BL | 95.94 ± 16.76 | 93.04 ± 19.03 | .525 | <.001 | .005 |
| 1 Year | 93.53 ± 16.40 | 92.60 ± 18.92 | ||||
| Untreated wives (n=203) | BL | 81.52 ± 18.98 | 76.97 ± 14.96 | .181 | <.001 | <.001 |
| 1 Year | 79.17 ± 18.98 | 76.89 ±14.95 | ||||
| Normal weight spouses (n=71) | BL | 63.28 ± 9.95 | 66.03 ± 9.03 | .110 | .021 | .002 |
| 1 Year | 61.60 ± 9.57 | 66.30 ± 9.06 | ||||
| Overweight spouses (n=109) | BL | 80.48 ± 9.00 | 77.90 ± 10.44 | .404 | .004 | .016 |
| 1 Year | 78.61 ± 9.76 | 77.74 ± 11.42 | ||||
|
Obese spouses (n=177) |
BL | 100.45 ± 15.61 | 96.77 ± 16.65 | .332 | <.001 | .003 |
| 1 Year | 97.55 ± 16.00 | 96.23 ± 16.45 | ||||
Figure 1.
Distribution of 1-year changes in percent weight among untreated spouses
Note: Dashed lines are used to indicate the percentages of spouses of ILI participants who achieved 5% weight losses and the percentage of spouses of ILI participants who had no weight gain.
The weight changes of participants and untreated spouses were correlated (partial r = .28, p<.001). These correlations remained significant when looking at ILI and DSE couples separately (ILI: partial r = .19, p=.01; DSE: partial r = .17, p=.047).
Dietary and physical activity changes in untreated spouses
Spouses of ILI participants had greater reductions in self-reported energy intake (p=.007) and percent of energy from fat (p=.012) than spouses of DSE participants, but did not differ in changes in self-reported physical activity (Table 3). Changes in energy intake and percent of energy from fat were correlated with weight loss in spouses (partial r = .22, p<.001; partial r = .12, p=.04, respectively).
Table 3.
Dietary intake and physical activity at baseline and 1-year of untreated spouses (Mean ± SD)
| Intensive Lifestyle Intervention | Diabetes Support and Education Controls | p value | ||||
|---|---|---|---|---|---|---|
| Group | Time | Group × Time | ||||
| Energy Intake (kcal/day) | BL | 1809 ± 830 | 1715 ± 771 | .882 | <.001 | .007 |
| 1 Year | 1532 ± 650 | 1601 ± 733 | ||||
| % of Energy from Fat | BL | 38.24 ± 7.00 | 38.86 ± 7.22 | .03 | .004 | .012 |
| 1 Year | 36.14 ± 7.15 | 38.74 ± 7.50 | ||||
| Physical Activity (kcal/week) | BL | 1100.2 ± 1286.3 | 1236.1 ± 1520.7 | .376 | .127 | .938 |
| 1 Year | 1225.9 ± 1371.6 | 1349.6 ± 1744.6 | ||||
Changes in percent of energy from fat were correlated between participants and spouses (partial r = .21, p<.001) and remained significant when looking separately at ILI couples (partial r = .16, p=.048) but not DSE couples (partial r = .10, p=.25). There were no correlations between participants and spouses in changes in energy intake or physical activity.
Weight control practices in untreated spouses
Over 70% of spouses reported trying to lose weight in the 1-year study period (74.9% of ILI spouses vs. 71.5% of DSE spouses, p=.50), yet few participated in an organized weight loss program (10.8% of ILI spouses vs. 15.3% of DSE spouses, p=.23). Spouses of ILI participants were more likely than spouses of DSE participants to endorse strategies recommended in behavioral weight control programs such as self-weighing (p=.003), counting calories (p=.003) and fat grams (p=.007), cutting out between meal snacking (p=.004), and using meal replacement products (p<.0001). No differences were observed in strategies related to physical activity or in unhealthy weight control strategies.
Changes in the shared home environment
Total number of foods available decreased in both ILI and DSE homes (Table 4, p=.03) but was not significantly different between the two groups. However, the availability of high-fat foods decreased more in ILI homes than DSE homes (p=.034) and the availability of low-fat foods increased more in ILI homes than DSE homes (p=.04). Decreases in high-fat foods in the home were associated with reductions in energy intake (partial r = .24, p<.001) and weight loss (partial r = .12, p=.049) in spouses. The relationship between changes in high-fat foods and energy intake, but not weight loss, remained significant when examining ILI spouses (partial r = .27, p=.001). No relationships were observed when examining only DSE spouses (ps>.25). There were no associations between changes in low-fat foods in the home and dietary intake or weight losses in spouses.
Table 4.
Home food and exercise environment at baseline and 1-year (Mean ± SD)
| Intensive Lifestyle Intervention | Diabetes Support and Education Controls | p value | ||||
|---|---|---|---|---|---|---|
| Group | Time | Group × Time | ||||
| Total Number of Foods in the Home | BL | 15.95 ± 3.79 | 16.35 ± 3.32 | .11 | .03 | .30 |
| 1 Year | 15.37 ± 3.65 | 16.15 ± 3.08 | ||||
| Number of High-Fat Foods in the Home | BL | 8.25 ± 2.76 | 8.44 ± 2.54 | .003 | .004 | .034 |
| 1 Year | 7.44 ± 2.78 | 8.43 ± 2.47 | ||||
| Number of Low-Fat Foods in the Home | BL | 7.69 ± 2.02 | 7.91 ± 1.75 | .989 | .833 | .04 |
| 1 Year | 7.93 ± 2.00 | 7.72 ± 1.72 | ||||
| Total Amount of Exercise Equipment in the Home | BL | 5.08 ± 2.57 | 4.97 ± 2.70 | .97 | .89 | .22 |
| 1 Year | 4.97 ± 2.69 | 5.06 ± 2.82 | ||||
The amount of exercise equipment in the home did not change significantly over time or in a differential fashion between ILI and DSE homes (Table 4). Changes in the exercise home environment were not associated with changes in physical activity or weight loss in spouses.
Discussion
This study is the first to document that behavioral weight loss treatment delivered to one spouse has a clinically significant impact on the measured weight of the untreated spouse. Over a 1-year period, we found that untreated spouses of participants randomly assigned to behavioral weight loss intervention lost nearly 3% of their body weight compared to weight losses of less than 0.25% in untreated spouses of participants randomly assigned to an enhanced usual care condition. This pattern held true regardless of the spouses' gender or initial weight status. We also found that spouses of the active intervention participants were more likely to achieve clinically significant weight losses (≥ 5% of initial body weight) and were more likely to remain at or below their starting weight than spouses of the DSE (control) group participants. Of the measured variables, the weight control benefits appeared to be due primarily to dietary modifications. Spouses of the ILI participants reported greater reductions in energy intake and percent of energy from fat than control spouses and these changes were associated with weight loss. While the weight losses of the spouses of the ILI participants were smaller than those observed in their actively treated spouses, these benefits were obtained without the assistance of a structured behavioral program.
Our findings are consistent with evidence from the cardiovascular disease and cancer prevention literatures that health behavior interventions can have a ripple effect on the lipid profiles,16 self-reported weights,18 and diets17-19 of untreated spouses. These prior investigations, while intriguing, relied on retrospective self-report measures of weight change, assessed only husbands or wives, and studied interventions that did not target weight loss. In contrast, the present study explored the ripple effect within the context of a weight loss intervention and measured weight at baseline and 1-year, assessing both husbands and wives.
The weight losses and dietary improvements observed in untreated spouses may have resulted from untreated spouses emulating their partners' new health behaviors. Lending support to this hypothesis is that changes in weight and fat intake were correlated between spouses. In addition, spouses of ILI participants were more likely than spouses of DSE participants to engage in dietary strategies recommended in behavioral weight control programs such as counting calories and self-weighing, further supporting a modeling effect.
Improvements in untreated spouses may also have been prompted by healthier food cues in the shared home environment. As expected, spouses of ILI participants reported a greater decrease in the number of high-fat foods available in their homes and an increase in the number of low-fat foods compared to spouses of control participants. Reduced availability of high-fat foods was associated with greater reductions in energy intake and better weight losses in spouses, underscoring the potential role home food cues play in weight control. Correlational studies have found relationships between the types of food in the home and dietary intake;25, 28,29 however, this is the first study to report that a change in the home food environment is associated with weight control benefits in untreated adults.
Unlike the dietary changes observed, spouses of ILI participants did not report more physical activity than spouses of control participants over time. Intervention and control homes also did not differ in the availability of exercise equipment and changes in the availability of exercise equipment were not were not associated with weight loss or physical activity in spouses. Increasing physical activity may require more self-initiated behavior change than dietary modifications, which perhaps occur passively in response to food cues. Additional research is needed to determine what aspects of the home environment to modify to promote weight control.
Limitations of this study include the use of self-report measures of the home environment. Although we did not conduct independent observations of the home, there was good agreement between participant and spouse reports. Another concern is that most households in this study (70%) consisted only of the participant and spouse. Controlling for number of household members did not affect our results; however, future research should explore the ripple effect in homes with children. Effects on spouses may have been magnified in this study because all participants had type 2 diabetes, perhaps creating added motivation for spouses to modify their own eating and exercise habits. Also, many eligible couples declined participation in this substudy. It may be that only the most supportive spouses were willing to enroll in this research, perhaps further inflating the magnitude of effects in both ILI and DSE spouses. Moreover, participants and spouses in this study were well-educated, with over 65% of untreated spouses having attended at least some college. Replication of our findings in a non-medical and more diverse sample is warranted. Randomized controlled trials are also needed to examine ways to best engage spouses in weight loss treatment, particularly among weight loss participants who indicate low levels of support from their marital partners.
A clear implication of this research is that by assessing only individual participants, the existing literature on behavioral weight loss treatment may have underestimated the reach and cost effectiveness of these interventions. While the potential negative influence of social ties on weight status has been documented,9 this is the first study to provide objective evidence that treating one spouse can have a beneficial, and clinically significant, impact on the weight of the untreated spouse. This benefit was achieved without any additional cost to treatment providers. From our examination of the shared home environment, it appears that assisting individuals decrease the amount of high-fat food in their homes might promote the spread of weight loss to spouses, and buffer against some of the weight gain typically observed after marriage. Effective models for changing the home food environment exist30-33 but their impact on untreated family members has yet to be assessed. More research is needed to determine how best to utilize the social network of marriage and the shared home environment to influence the weights and behaviors of both treated and untreated spouses.
Acknowledgments
This paper represents the collective efforts of the Home Environment Research Group (noted below) as well as the Look AHEAD Research Group. The full list of acknowledgments has been previously published in the Look AHEAD 1-year results paper.27
Home Environment Research Group
The Miriam Hospital/Brown Medical School Renee Bright, MS2; Vincent Pera, MD3; Deborah Tate, PhD3; Kara Gallagher, PhD3; Amy Bach, PhD; Barbara Bancroft, RN, MS; Anna Bertorelli, MBA, RD; Richard Carey, BS; Tatum Charron, BS; Heather Chenot, MS; Kimberley Chula-Maguire, MS; Pamela Coward, MS, RD; Lisa Cronkite, BS; Julie Currin, MD; Maureen Daly, RN; Caitlin Egan, MS; Erica Ferguson, BS, RD; Linda Foss, MPH; Jennifer Gauvin, BS; Don Kieffer, PhD; Lauren Lessard, BS; Deborah Maier, MS; JP Massaro, BS; Tammy Monk, MS; Rob Nicholson, PhD; Erin Patterson, BS; Suzanne Phelan, PhD; Hollie Raynor, PhD, RD; Douglas Raynor, PhD; Natalie Robinson, MS, RD; Deborah Robles; Jane Tavares, BS
The University of Alabama at Birmingham Cora E. Lewis, MD, MSPH1; Sheikilya Thomas MPH2; Monika Safford, MD3; Charlotte Bragg, MS, RD, LD; Amy Dobelstein; Stacey Gilbert, MPH; Stephen Glasser, MD; Sara Hannum, MA; Anne Hubbell, MS; Jennifer Jones, MA; DeLavallade Lee; Ruth Luketic, MA, MBA, MPH; Karen Marshall; L. Christie Oden; Janet Raines, MS; Cathy Roche, RN, BSN; Janet Truman; Nita Webb, MA; Audrey Wrenn, MAEd
University of Minnesota Carolyn Thorson, CCRP2; John P. Bantle, MD3; J. Bruce Redmon, MD3; Richard S. Crow, MD3; Scott Crow, MD3; Susan K Raatz, PhD, RD3; Carolyne Campbell; Jeanne Carls, MEd; Tara Carmean-Mihm, BA; Emily Finch, MA; Anna Fox, MA; Elizabeth Hoelscher, MPH, RD, CHES; La Donna James; Vicki A. Maddy, BS, RD; Therese Ockenden, RN; Birgitta I. Rice, MS, RPh CHES; Tricia Skarphol, BS; Ann D. Tucker, BA; Mary Susan Voeller, BA; Cara Walcheck, BS, RD
Funding and Support. This ancillary study was supported through the National Institute of Nursing Research NR07960. The parent trial was supported by the Department of Health and Human Services through the following cooperative agreements from the National Institutes of Health: DK57136, DK57149, DK56990, DK57177, DK57171, DK57151, DK57182, DK57131, DK57002, DK57078, DK57154, DK57178, DK57219, DK57008, DK57135, and DK56992. The following federal agencies also contributed support: National Institute of Diabetes and Digestive and Kidney Diseases; National Heart, Lung, and Blood Institute; National Institute of Nursing Research; National Center on Minority Health and Health Disparities; Office of Research on Women's Health; and the Centers for Disease Control and Prevention. This research was supported in part by the Intramural Research Program of the National Institute of Diabetes and Digestive and Kidney Diseases. All researchers are independent of the funding agencies.
Footnotes
Principal Investigator
Program Coordinator
Co-Investigator
All other Look AHEAD staffs are listed alphabetically by site.
Contributor Information
Amy A. Gorin, Department of Psychology, Center for Health, Intervention and Prevention, University of Connecticut, 2006 Hillside Road, Unit 1248, Storrs, CT 06269-1248
Rena R. Wing, Department of Psychiatry, Brown Medical School, The Miriam Hospital, 196 Richmond Street, Providence, RI 02903
Joseph L. Fava, The Miriam Hospital, 196 Richmond Street, Providence, RI 02903
John M. Jakicic, Department of Health and Physical Activity, University of Pittsburgh, Suite 600, Birmingham Towers, 2100 Wharton Street, Pittsburgh, PA 15203
Robert Jeffery, Division of Epidemiology and Community Health, University of Minnesota, 1300 South Second Street, Suite 300, Minneapolis, MN 55454-1015.
Delia Smith West, Fay W. Boozman College of Public Health, University of Arkansas for Medical Sciences, 4301 West Markham St, #820, Little Rock, AR 72205.
Kerrin Brelje, Division of Epidemiology and Community Health, University of Minnesota, 1300 South Second Street, Suite 300, Minneapolis, MN 55454-1015.
Vicki G. DiLillo, Department of Psychology, Ohio Wesleyan University, 61 S. Sandusky Street, Delaware, OH 43015
References
- 1.Jacobson P, Torgerson JS, Sjöström L, Bouchard C. Spouse resemblance in body mass index: effects on adult obesity prevalence in the offspring generation. Am J Epidemiol. 2007;166:101–8. doi: 10.1093/aje/kwj342. [DOI] [PubMed] [Google Scholar]
- 2.Katzmarzyk PT, Hebebrand J, Bouchard C. Spousal resemblance in the Canadian population: implications for the obesity epidemic. Int J Obes Relat Metab Disord. 2002;26:241–6. doi: 10.1038/sj.ijo.0801870. [DOI] [PubMed] [Google Scholar]
- 3.Macken LC, Yates B, Blancher S. Concordance of risk factors in female spouses of male patients with coronary heart disease. J Cardiopulm Rehabil. 2000;20:361–8. doi: 10.1097/00008483-200011000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Maes HM, Neale MC, Eaves LJ. Genetic and environmental factors in relative body weight and human adiposity. Behav Genet. 1997;27:325–51. doi: 10.1023/a:1025635913927. [DOI] [PubMed] [Google Scholar]
- 5.Jeffery RW, Rick AM. Cross-sectional and longitudinal associations between body mass index and marriage related factors. Obes Res. 2002;10:809–15. doi: 10.1038/oby.2002.109. [DOI] [PubMed] [Google Scholar]
- 6.Kahn HS, Williamson DF. The contributions of income, education and changing marital status to weight change among US men. Int J Obes. 1990;14:1057–68. [PubMed] [Google Scholar]
- 7.Sobal J, Rauschenbach B, Frongillo EA. Marital status changes and body weight changes: a US longitudinal analysis. Soc Sci Med. 2003;56:1543–45. doi: 10.1016/s0277-9536(02)00155-7. [DOI] [PubMed] [Google Scholar]
- 8.Katzmarzyk PT, Perusse L, Rao DC, Bouchard C. Spousal resemblance and risk of 7-year increases in obesity and central adiposity in the Canadian population. Obes Res. 1999;7:545–51. doi: 10.1002/j.1550-8528.1999.tb00712.x. [DOI] [PubMed] [Google Scholar]
- 9.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357:370–9. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- 10.Hur YM, Bouchard TJ, Eckert E. Genetic and environmental influences on self-reported diet: a reared-apart twin study. Physiol Behav. 1998;64:629–36. doi: 10.1016/s0031-9384(98)00101-2. [DOI] [PubMed] [Google Scholar]
- 11.Patterson RE, Kristal AR, Shannon J, Hunt JR, White E. Using a brief household food inventory as an environmental indicator of individual dietary practices. Am J Public Health. 1997;87:272–75. doi: 10.2105/ajph.87.2.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Newmark-Sztainer D, Wall M, Perry C, Story M. Correlates of fruit and vegetable intake among adolescents. Findings from Project EAT. Prev Med. 2003;37:198–08. doi: 10.1016/s0091-7435(03)00114-2. [DOI] [PubMed] [Google Scholar]
- 13.Zabinki MF, Daly T, Norman GJ, et al. Psychosocial correlates of fruit and vegetable, and dietary fat intake among adolescent boys and girls. J Am Diet Assoc. 2006;106:814–21. doi: 10.1016/j.jada.2006.03.014. [DOI] [PubMed] [Google Scholar]
- 14.Jakicic JM, Wing RR, Butler BA, Jeffery RW. The relationship between presence of exercise equipment in the home and physical activity level. Am J Health Promot. 1997;11:363–65. doi: 10.4278/0890-1171-11.5.363. [DOI] [PubMed] [Google Scholar]
- 15.Wing RR, Gorin AA, Tate DF. Strategies for changing eating and exercise behavior. In: Bowman BA, Russell RM, editors. Present knowledge in Nutrition. 9th. Washington, DC: ILSI Press; 2006. pp. 822–37. [Google Scholar]
- 16.Sexton M, Bross D, Hebel JR, et al. Risk-factor changes in wives with husbands at high risk of coronary heart disease (CHD) J Behav Med. 1987;10:251–61. doi: 10.1007/BF00846539. [DOI] [PubMed] [Google Scholar]
- 17.Shattuck AL, White E, Kristal AR. How women's adopted low-fat diets affect their husbands. Am J Public Health. 1992;82:1244–50. doi: 10.2105/ajph.82.9.1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.White E, Hurlich M, Thompson RS, et al. Dietary changes among husbands of participants in a low-fat dietary intervention. Am J Prev Med. 1991;7:319–25. [PubMed] [Google Scholar]
- 19.Zimmerman RS, Gerace TA, Smith JC, Benezra J. The effects of a worksite health promotion program on the wives of fire fighters. Soc Sci Med. 1988;26:537–43. doi: 10.1016/0277-9536(88)90386-3. [DOI] [PubMed] [Google Scholar]
- 20.Ryan DH, Espeland MA, Foster GD, et al. Look AHEAD (Action for Health in Diabetes): design and methods for a clinical trial of weight loss for the prevention of cardiovascular disease in type 2 diabetes. Control Clin Trials. 2003;24:610–28. doi: 10.1016/s0197-2456(03)00064-3. [DOI] [PubMed] [Google Scholar]
- 21.The Diabetes Prevention Program. Design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes Care. 1997;22:623–34. doi: 10.2337/diacare.22.4.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wadden TA, West DS, Delahanty L, et al. The Look AHEAD Research Group The Look AHEAD study: a description of the lifestyle intervention and the evidence supporting it. Obesity. 2006;14:737–52. doi: 10.1038/oby.2006.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Block G, Woods M, Potosky A, Clifford C. Validation of a self-administered diet history questionnaire design using multiple diet records. J Clin Epidemiol. 1990;43:1327–35. doi: 10.1016/0895-4356(90)90099-b. [DOI] [PubMed] [Google Scholar]
- 24.Paffenbarger RS, Wing AL, Hyde RT. Physical activity as an index of heart attack risk in college alumni. Am J Epidemiol. 1978;108:161–75. doi: 10.1093/oxfordjournals.aje.a112608. [DOI] [PubMed] [Google Scholar]
- 25.Raynor HA, Polley BA, Wing RR, Jeffery RW. Is dietary fat intake related to liking or household availability of high- and low-fat foods? Obes Res. 2004;12:816–23. doi: 10.1038/oby.2004.98. [DOI] [PubMed] [Google Scholar]
- 26.Block G, Hartman AM, Naughton D. A reduced dietary questionnaire: Development and validation. Epidemiol. 1990;1:58–64. doi: 10.1097/00001648-199001000-00013. [DOI] [PubMed] [Google Scholar]
- 27.Pi-Sunyer X, Blackburn G, Brancati FL, et al. The Look AHEAD Research Group Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the Look AHEAD trial. Diabetes Care. 2007;30:1374–83. doi: 10.2337/dc07-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Campbell KJ, Crawford DA, Salmon J, Carver A, Garnett SP, Baur LA. Associations between the home food environment and obesity promoting eating behaviors in adolescence. Obesity. 2007;15:719–30. doi: 10.1038/oby.2007.553. [DOI] [PubMed] [Google Scholar]
- 29.Hanson NI, Neumark-Sztainer D, Eisenberg ME, Story M, Wall M. Associations between parental report of the home food environment and adolescent intake of fruits, vegetables, and dairy foods. Public Health Nutr. 2005;8:77–85. doi: 10.1079/phn2005661. [DOI] [PubMed] [Google Scholar]
- 30.Ebbeling CB, Feldman HA, Osganian SK, Chomitz VR, Ellenbogen SJ, Ludwig DS. Effects of decreasing sugar-sweetened beverage consumption on body weight in adolescents: a randomized, controlled pilot study. Pediatrics. 2006;117:673–80. doi: 10.1542/peds.2005-0983. [DOI] [PubMed] [Google Scholar]
- 31.Gorin AA, Raynor HA, Niemeier HM, Wing RR. Home grocery delivery improves the household food environments of behavioral weight loss participants: Results of an 8-week pilot study. Int J Beh Nutr Phys Act. 2007;4:58. doi: 10.1186/1479-5868-4-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jeffery RW, Wing RR, Thorson C, Burton LR. Strengthening behavioral interventions for weight loss: a randomized trial of food provision and monetary incentives. J Consult Clin Psychol. 1993;6:1038–45. doi: 10.1037//0022-006x.61.6.1038. [DOI] [PubMed] [Google Scholar]
- 33.Wing RR, Jeffery RW, Burton LR, Thorson C, Nissinoff KS, Baxter JE. Food provision vs. structured meal plans in the behavioral treatment of obesity. Int J Obes Relat Metab Disord. 1996;20:56–62. [PubMed] [Google Scholar]