INTRODUCTION
Approximately 400,000 Americans have multiple sclerosis (MS), and approximately 200 more cases are diagnosed every week. The annual financial toll of therapy for MS—a chronic, often disabling neurological disease that attacks the central nervous system—is estimated at $16 billion. The number of people with MS is only an estimate because health care providers are not required to report new cases of MS to either a state or a federal registry, as they are with measles, hepatitis, and tuberculosis.
Teva Neuroscience, in conjunction with the National Multiple Sclerosis Society (NMSS), surveyed audiences representing 82 managed care organizations (MCOs); 143 neurologists; 68 neurology reimbursement, coding, and billing specialists; 19 specialty pharmacists; 101 case managers; and 1,935 patients. The result is a report that explores trends in treatment, reimbursement, specialty pharmacy, disease management, and benefits design.1
As new drugs for MS reach the marketplace and costs accelerate, it is essential to understand disease progression, the consequences of comorbidities, the importance of maintaining quality of life, and factors influencing cost. This report should increase our awareness and understanding of MS and, in doing so, may improve treatment for patients.
As diverse as the audiences are for this survey, MCOs, health care providers, and patients agree that working together is a primary strategy for managing MS. They consider a collaborative approach to be one that entails managing MS symptoms, relapses, disability, concomitant depression, disease-management strategies, preventive care, reimbursement, communication, and adherence to treatment.
Dr. Nicholas LaRocca, PhD, Vice President of Health Care Delivery and Policy Research at NMSS, states: “These groups are beginning to reach out to each other to find ways to manage MS and improve quality of care. MS is a complex disease to treat; support services are critical to managing the disease and to relieving the burden on practitioners.”
DESIGNING BENEFITS
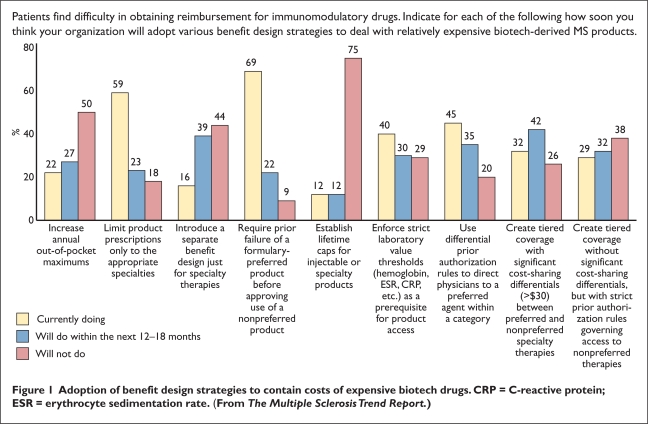
To ensure the appropriate use of and access to biologic products used to treat MS while keeping costs low, MCOs have adopted various approaches, as shown in Figure 1:
requiring that a preferred formulary drug has failed before a non-preferred product can be approved (69%)
limiting prescriptions to the appropriate specialties (59%)
using differential prior authorization to direct physicians to a preferred drug within a category (45%)
Figure 1.
Adoption of benefit design strategies to contain costs of expensive biotech drugs. CRP = C-reactive protein; ESR = erythrocyte sedimentation rate. (From The Multiple Sclerosis Trend Report.)
Almost 23% of MCOs noted that they plan to implement these first two strategies in the next 12 to 18 months, whereas 35% expect to implement the differential prior authorization.
In the survey, 32% of MCOs had already put in place tiered coverage with significant cost-sharing differentials (above $30) between preferred and non-preferred specialty therapies. As many as 75% of respondents did not support establishing lifetime caps for injectable or specialty products.
FINANCIAL COMPENSATION
Most neurologists surveyed (95%) reported using infused corticosteroids to treat MS, mostly to treat acute relapse, and more than 70% noted that they seldom or never encountered problems with receiving payment when prescribing those drugs. However, as many as 74% always, usually, or sometimes experienced difficulty in receiving payment for infused disease-modifying drugs (DMDs), whereas 71% said that their use of such drugs was always, usually, or sometimes restricted.
Neurologists did not express much optimism about salary increases. More than one-third stated that their income remained the same for a period of two years, and 37% admitted that their income had decreased. Only 26% saw an increase in their income over the previous two years. Dr. LaRocca says that declining or static income makes it difficult to recruit neurologists to specialize in MS. In fact, as many as two-thirds of neurologists preferred not to take on more MS patients.
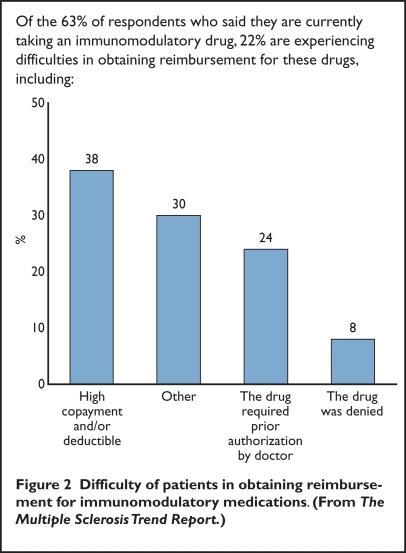
Patients also had concerns about reimbursement. Of the 63% of patients who said that they were currently taking an immunomodulatory drug to treat MS, 22% experienced difficulties in obtaining reimbursement (Figure 2). The primary reasons cited were high copayments or deductibles (38%), necessary prior authorizations (24%), and denial of coverage for the drug (8%).
Figure 2.
Difficulty of patients in obtaining reimbursement for immunomodulatory medications. (From The Multiple Sclerosis Trend Report.)
Almost half of MCOs (49%) covered self-injectable MS drugs under the pharmacy benefit. Only 13% of MCOs paid for these drugs under the medical benefit, and 38% covered them under both categories, depending on various circumstances.
BENEFITING FROM SPECIALTY PHARMACY
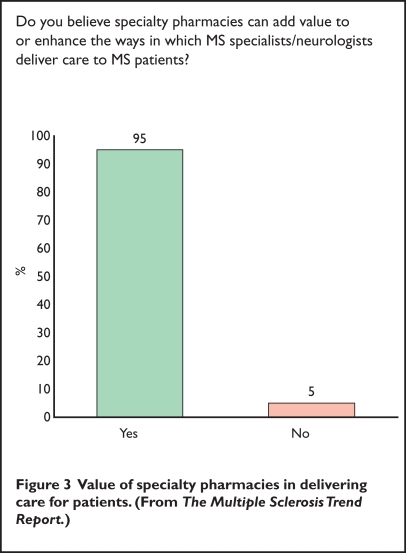
With resources very expensive and MS such a complex disease, 68% of neurologists surveyed say that they would welcome the help of specialty pharmacy in managing the treatment of MS patients. Ideally, case managers or pharmacists would administer the program, which would work with patients and physicians in managing symptoms, depression, adherence, preventive care, and reimbursement. Many neurologists believe that specialty pharmacies ease the burden of administrative duties (Figure 3), which often take up to five hours each week—time that could otherwise be devoted to patient care.
Figure 3.
Value of specialty pharmacies in delivering care for patients. (From The Multiple Sclerosis Trend Report.)
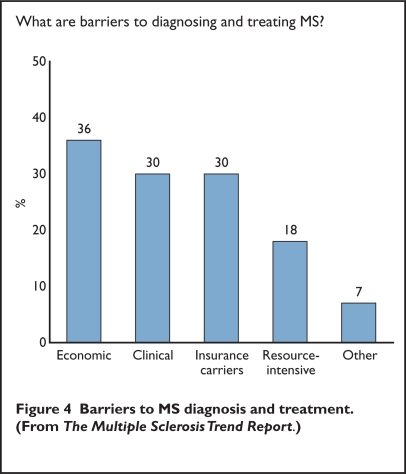
As many as 95% of neurologists indicated a high level of confidence in diagnosing MS, even though the disease is complex and resource-intensive; however, 59% of neurologists acknowledged some barriers to diagnosis and treatment in their practices, including economic concerns (36%), clinical problems (30%), and difficulties with insurance carriers (30%) (Figure 4). Other barriers cited included the large quantity of resources—complex medication regimens, MRIs and the expertise of a variety of specialists, including neurologists, psychologists and occupational therapists—needed for the diagnosis and treatment of MS.
Figure 4.
Barriers to MS diagnosis and treatment. (From The Multiple Sclerosis Trend Report.)
Dr. LaRocca was somewhat surprised by the positive attitude that neurologists expressed toward specialty pharmacies. As the treatment of MS becomes more complex with the growing number of biologics, he anticipates that there will be more contact between physicians and specialty pharmacies.
Of the MCOs that participated in the research, as many as 90% were currently contracting with specialty pharmacies, and 79% indicated that their members with MS would be required or encouraged to use a specialty pharmacy to obtain injectable drugs within the next two years.
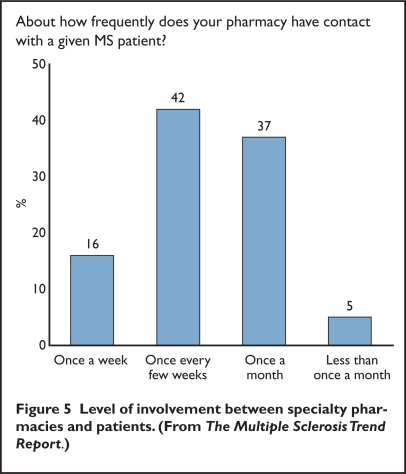
Specialty pharmacies varied in their level of involvement with patients. Of those pharmacies surveyed, 42% reported having contact with patients once every few weeks and 37% had contact once a month. Only 16% interacted with patients on a weekly basis (Figure 5).
Figure 5.
Level of involvement between specialty pharmacies and patients. (From The Multiple SclerosisTrend Report.)
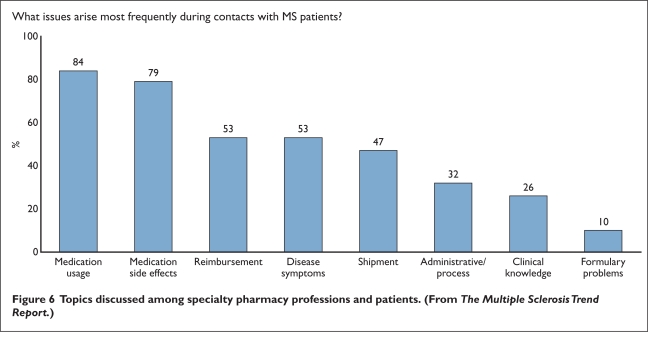
Specialty pharmacy professionals reported that the most frequent topics discussed with MS patients were medication usage (84%), adverse drug effects (79%), reimbursement (53%), and disease symptoms (53%). Formulary problems were discussed only 10% of the time (Figure 6).
Figure 6.
Topics discussed among specialty pharmacy professions and patients. (From The Multiple Sclerosis Trend Report.)
Ben Thrower, MD, Medical Director of Shepherd MS Institute in Atlanta, Georgia, says that surveys such as this can provide needed information about the way in which MS is managed. He adds that understanding the trends and challenges in caring for patients in the community may help MS centers, specialty pharmacies, drug companies, and MCOs collaborate more effectively to provide optimal therapy for these patients.
Readers can order copies of The Multiple Sclerosis Trend Report, which is supported by Teva Neuroscience and the National Multiple Sclerosis Society, by accessing www.mstrendreport.com.
Footnotes
Disclosure: Mr. Sonnenreich received a grant to produce The MS Trend Report from Teva Neuroscience in 2006, but he received no honorarium for this work. Ms. Edlin has no financial relationships to report in regard to this article.
REFERENCE
- 1.The Multiple Sclerosis Trend Report: Perspectives From-Managed Care, Providers, and Patients. Available at: www.mstrendreport.com. Accessed September 8, 2008.