Abstract
Background
Limited information is available about potentially changing, and contemporary, trends in the incidence and hospital death rates of cardiogenic shock complicating acute myocardial infarction (AMI). The objectives of our study were to examine 3 decade long trends (1975-2005) in the incidence rates of cardiogenic shock complicating AMI, patient characteristics and treatment practices associated with this clinical complication, and hospital death rates in residents of a large central New England community hospitalized at all area medical centers with AMI.
Methods and Results
The study population consisted of 13,663 residents of the Worcester (MA) metropolitan area hospitalized with AMI at all greater Worcester medical centers during 15 annual periods between 1975 and 2005. Overall, 6.6% of patients developed cardiogenic shock during their index hospitalization. The incidence rates of cardiogenic shock remained stable between 1975 and the late 1990's, but declined in an inconsistent manner thereafter. Patients in whom cardiogenic shock developed had a significantly greater risk of dying during hospitalization (65.4%) than those who did not develop cardiogenic shock (10.6%) (p<0.001). Encouraging increases in hospital survival in patients with cardiogenic shock were, however, observed from the mid-1990s to our most recent study years. Several patient demographic and clinical characteristics were associated with an increased risk for developing cardiogenic shock.
Conclusions
Our findings indicate improving trends in the hospital prognosis associated with cardiogenic shock. Given the high death rates associated with this clinical complication, monitoring future trends in the incidence and death rates, and factors associated with an increased risk for developing cardiogenic shock, remain warranted.
Keywords: epidemiology, cardiogenic shock, myocardial infarction, population
Introduction
While there are numerous clinical complications that are associated with the development of acute myocardial infarction (AMI), none are more potentially devastating or carry a worse prognosis than cardiogenic shock (1-7).
Despite marked advances in medical treatment, revascularization techniques, and mechanical support during the past 2 decades, cardiogenic shock is still the most common cause of hospital mortality associated with AMI (7,8). On the other hand, data obtained from a limited number of recent studies suggest possible declines in the hospital mortality associated with cardiogenic shock (5,7,9-13), partially associated with the implementation of early revascularization therapy based on recent practice guidelines (14). Few studies, however, have examined contemporary, and changing, trends in the magnitude or mortality associated with cardiogenic shock, particularly from the more generalizable perspective of a population-based investigation.
In 2 prior publications from the Worcester (MA) Heart Attack Study, we described changing trends in the magnitude of, and hospital outcomes associated with, cardiogenic shock in residents of this large central New England metropolitan area hospitalized with AMI at all area medical centers (6,7). In the present study, we provide an extended 3 decades long perspective (1975-2005) into changing trends in the incidence rates of cardiogenic shock, factors associated with the occurrence of cardiogenic shock complicating AMI, hospital treatment practices, and short-term death rates (15-17).
Methods
The study population consisted of greater Worcester residents hospitalized with a discharge diagnosis of AMI at all teaching and community hospitals in the Worcester metropolitan area during the 15 individual study years of 1975 (n=781), 1978 (n=845), 1981 (n=998), 1984 (n=714), 1986 (n=765), 1988 (n=659), 1990 (n=766),1991 (n=848), 1993 (n=953), 1995 (n=949), 1997 (n=1,059), 1999 (n=1,027), 2001 (n=1,239), 2003 (n=1,157), and 2005 (n=903). There were originally 16 hospitals included in this population-based investigation but there are presently 11 due to hospital closures or conversion to chronic care or rehabilitation facilities. Potentially eligible patients were identified through the review of computerized hospital databases of patients with International Classification of Disease discharge diagnoses consistent with the possible presence of AMI (e.g., AMI, unstable angina). The medical records of all potentially eligible patients, who had to be residents of the Worcester metropolitan area since this study is population-based, were reviewed in a standardized manner and the diagnosis of AMI was confirmed according to pre-established criteria that have been previously described (15-17).
Cardiogenic shock was defined as a systolic blood pressure of less than 80 mm Hg in the absence of hypovolemia and associated with cyanosis, cold extremities, changes in mental status, persistent oliguria, or congestive heart failure (6,7). The definition of cardiogenic shock remained the same during all periods studied. This disorder was defined so that patients with classic signs and symptoms of this clinical syndrome would be included.
Data Collection
Information was abstracted from the hospital medical records of greater Worcester residents with independently validated AMI by trained nurse and physician reviewers. Information was collected with regards to patient's demographic characteristics, medical history, clinical findings, and use of cardiac medications and specialized cardiac procedures as these therapies became available in clinical practice.
Data Analysis
Differences in the demographic and clinical characteristics as well as treatment practices of patients with, as compared to those without, cardiogenic shock, as well as short-term death rates, were examined using chi square tests of statistical significance; differences in selected continuous variables between patients with and without cardiogenic shock were examined using t-tests (Tables 1 and 2). Differences in the characteristics of patients with cardiogenic shock who survived the acute hospitalization as compared to those who did not were examined using similar analytic tests.
Table 1. Characteristics of Patients With Acute Myocardial Infarction (AMI) According to the Presence of Cardiogenic Shock.
| Total Sample | Patients Hospitalized in 2001, 2003, and 2005 | |||||
|---|---|---|---|---|---|---|
| Shock Present (+) (n=905) |
Shock Absent (-) (n=12,758) |
p Value | Shock Present (+) (n=173) |
Shock Absent (-) (n=3,126) |
p Value | |
| Characteristic | ||||||
| Age (mean, yrs) | 71.8 | 68.7 | <0.001 | 72.6 | 71.5 | 0.32 |
| Male (%) | 53.4 | 58.9 | <0.01 | 57.8 | 55.3 | 0.51 |
| Body mass index (%) | ||||||
| <25 | 40.3 | 36.5 | 0.10 | 38.5 | 33.8 | 0.09 |
| 25-29.9 | 38.0 | 36.3 | 40.8 | 36.9 | ||
| ≥30 | 21.7 | 27.2 | 20.8 | 29.4 | ||
| Duration of prehospital delay (mean, hrs)** | 2.0 | 3.6 | 0.10 | 3.8 | 4.1 | 0.69 |
| Do not resuscitate orders*** | 42.8 | 20.6 | <0.001 | 41.0 | 25.1 | <0.001 |
| Pre-Existing Conditions (%) | ||||||
| Angina | 25.4 | 24.9 | 0.43 | 20.2 | 20.4 | 0.97 |
| Diabetes | 32.2 | 27.8 | <0.01 | 41.0 | 33.2 | <0.05 |
| Heart failure | 23.2 | 18.8 | <0.001 | 28.3 | 24.9 | 0.31 |
| Hypertension | 56.4 | 57.7 | 0.43 | 74.0 | 72.4 | 0.65 |
| Stroke | 11.3 | 9.6 | 0.12 | 6.4 | 12.4 | <0.05 |
| Acute Presenting Symptoms (%) | ||||||
| Chest pain* | 69.0 | 72.7 | 0.16 | 68.2 | 72.2 | 0.26 |
| Diaphoresis* | 39.6 | 37.6 | 0.48 | 36.4 | 36.4 | 0.99 |
| Dyspnea* | 64.5 | 57.5 | <.05 | 65.9 | 60.0 | 0.12 |
| AMI type (%) | ||||||
| Initial | 60.0 | 65.5 | <0.01 | 60.7 | 65.2 | 0.23 |
| Q wave | 56.2 | 39.7 | <0.001 | 30.1 | 19.6 | <0.01 |
| Clinical Complications (%) | ||||||
| Third degree heart block | 15.7 | 3.3 | <0.001 | 9.8 | 2.1 | <0.001 |
| Atrial fibrillation | 30.3 | 16.2 | <0.001 | 45.1 | 20.5 | <0.001 |
| Heart failure | 69.4 | 37.4 | <0.001 | 75.1 | 36.9 | <0.001 |
| Stroke** | 1.4 | 1.6 | 0.62 | 1.2 | 1.9 | 0.48 |
| Physiologic findings at the time of hospital admission (mean) | ||||||
| Systolic blood pressure (mmHg) | 119.5 | 143.7 | <0.001 | 118.5 | 143.5 | <0.001 |
| Diastolic blood pressure (mmHg) | 69.2 | 77.8 | <0.001 | 68.6 | 77.0 | <0.001 |
| Heart rate (bpm)** | 88.1 | 86.2 | 0.05 | 90.1 | 86.8 | 0.08 |
| Laboratory findings at the time of hospital admission (mean, mg/dl) | ||||||
| Serum glucose**** | 228.7 | 182.1 | <0.001 | 221.2 | 183.0 | <0.01 |
| Estimated GFR findings (%)**** | 51.0 | 61.3 | <0.001 | 50.5 | 58.5 | <0.001 |
| Serum cholesterol | 194.3 | 208.7 | <0.001 | 156.3 | 177.6 | <0.001 |
97-05 only
86-05 only
91-05 only
95-05 only
Table 2. Treatment Practices in Patients Hospitalized With Acute Myocardial Infarction According to the Presence of Cardiogenic Shock.
| Total Sample | Patients Hospitalized in 2001, 2003, and 2005 | |||||
|---|---|---|---|---|---|---|
| Shock Present (+) (n=905) |
Shock Absent (-) (n=12,758) |
p Value | Shock Present (+) (n=173) |
Shock Absent (-) (n=3,126) |
p Value | |
| Medications (%) | ||||||
| Angiotensin converting enzyme inhibitors/angiotensin receptor blockers**** | 48.6 | 47.9 | 0.74 | 62.4 | 68.1 | 0.13 |
| Aspirin | 52.2 | 65.7 | <.001 | 90.2 | 91.4 | 0.60 |
| Beta blockers | 40.2 | 63.4 | <.001 | 76.9 | 90.2 | <0.001 |
| Calcium channel blockers** | 26.0 | 38.2 | <.001 | 20.2 | 25.4 | 0.12 |
| Lipid lowering agents*** | 20.2 | 31.0 | <.001 | 56.7 | 66.8 | <0.01 |
| Thrombolytics*** | 18.8 | 15.9 | 0.05 | 6.4 | 5.3 | 0.55 |
| Procedures (%) | ||||||
| Cardiac catheterization | 35.8 | 30.7 | <.001 | 74.0 | 55.5 | <0.001 |
| Coronary artery bypass graft surgery* | 6.9 | 3.8 | <.001 | 7.5 | 6.0 | 0.44 |
| Percutaneous coronary intervention*** | 28.8 | 19.3 | <.001 | 57.8 | 38.6 | <0.001 |
| Intraortic balloon counterpulsation | 29.7 | 2.0 | <.001 | 54.3 | 3.5 | <0.001 |
81-05 only
84-05 only
86-05 only
90-05 only
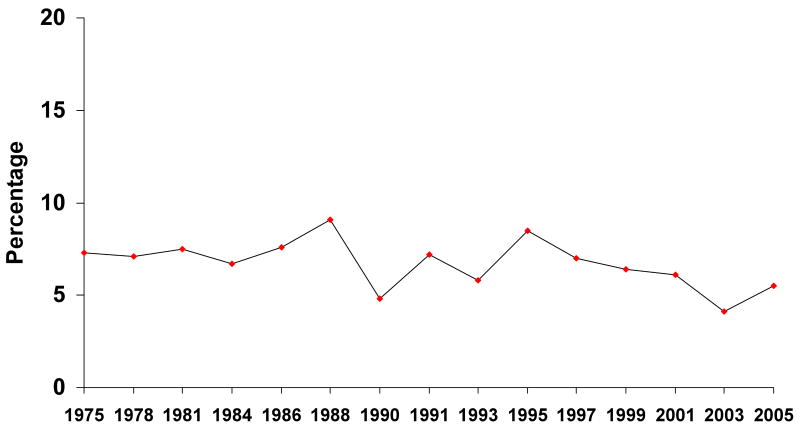
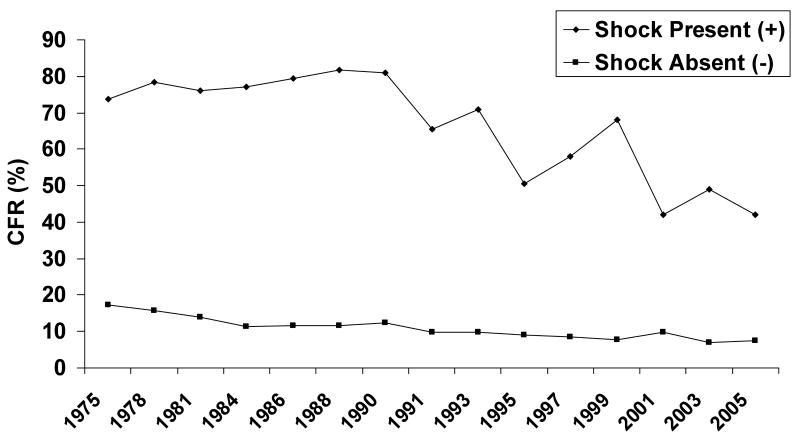
Changes over time in the incidence rates of cardiogenic shock were assessed using the Mantel-Haenszel chi-square test for trends (Figure 1). Trends in hospital case-fatality rates, stratified according to the presence of cardiogenic shock, were analyzed using Mantel-Haenszel methods (Figure 2). Multivariable logistic regression models were used to assess differences from baseline in the incidence rates of cardiogenic shock over the period under study while controlling for potentially confounding demographic and clinical factors (Table 3). The variables controlled for in our regression models were included either because they differed between our respective comparison groups or because they had been previously shown to be possible risk factors for cardiogenic shock.
Figure 1.
Trends in the Incidence Rates of Cardiogenic Shock in Patients With Acute Myocardial Infarction
Figure 2.
Trends in Hospital Case-Fatality Rates (CFR's) in Patients With Acute Myocardial Infarction According to the Presence of Cardiogenic Shock
Table 3. Odds of Developing Cardiogenic Shock in Patients With Acute Myocardial Infarction Over Time.
| Study Period | n | Patients With Shock % | Regression #1 | Regression #2 |
|---|---|---|---|---|
| 1975 | 781 | 7.3 | 1.0 | -- |
| 1978 | 845 | 7.1 | 0.93 (0.64,1.35) |
-- |
| 1981 | 998 | 7.5 | 0.95 (0.66,1.30) |
-- |
| 1984 | 714 | 6.7 | 0.87 (0.58,1.30) |
-- |
| 1986 | 765 | 7.6 | 0.94 (0.64,1.37) |
-- |
| 1988 | 659 | 9.1 | 1.16 (0.79,1.71) |
-- |
| 1990 | 766 | 4.8 | 0.56 (0.36,0.86) |
-- |
| 1991 | 848 | 7.2 | 0.84 (0.57,1.23) |
-- |
| 1993 | 953 | 5.8 | 0.65 (0.44,0.97) |
-- |
| 1995 | 949 | 8.5 | 1.00 (0.68,1.44) |
-- |
| 1997 | 1059 | 7.0 | 0.78 (0.53,1.13) |
1.0 |
| 1999 | 1027 | 6.4 | 0.70 (0.48,1.03) |
1.00 (0.65,1.53) |
| 2001 | 1239 | 6.1 | 0.65 (0.44,0.94) |
0.85 (0.56,1.30) |
| 2003 | 1157 | 4.1 | 0.42 (0.28,0.63) |
0.58 (0.37,0.92) |
| 2005 | 903 | 5.5 | 0.58 (0.38,0.87) |
0.95 (0.61,1.47) |
Regression #1 - Adjusted for patient's age, sex, length of hospital stay, history of diabetes, heart failure, or stroke, and AMI order
Regression #2 - Adjusted for patient's age, sex, length of hospital stay, history of diabetes, heart failure, or stroke, AMI order, admission blood pressure, serum glucose, and estimated GFR findings, hospital discharge status, and receipt of do not resuscitate orders during hospitalization.
Because of the nonrandomized nature of the present study, and because our methods of data collection did not allow us to determine whether a medical therapy or surgical intervention preceded or came after the occurrence of cardiogenic shock, we did not control for the use of various coronary reperfusion/revascularization procedures or medical therapies in our regression analyses. Our approach to model building focused on the hypothesis that changes in the incidence rates of cardiogenic shock over time were the result of changes in the characteristics of the hospitalized study sample.
We examined the impact of cardiogenic shock on hospital mortality by calculating in-hospital case-fatality rates (CFRs). Multivariable logistic regression analyses were utilized to assess the overall effect of cardiogenic shock on hospital mortality, and to study changes over time in the hospital CFR's associated with cardiogenic shock, while controlling for several potentially confounding factors that have previously been shown to be of prognostic importance (Table 4). This approach to model development was similar to that described for the development of cardiogenic shock. Human subjects approval for the review of hospital medical records in this cold pursuit disease surveillance project was obtained from the Committee for the Protection of Human Subjects in Research at the University of Massachusetts Medical School.
Table 4. Adjusted Odds of Dying During Selected Periods in Patients With Cardiogenic Shock Complicating Acute Myocardial Infarction.
| Study Period | n | Hospital Case-Fatality Rates % | Regression #1 | Regression #2 |
|---|---|---|---|---|
| 1975 | 57 | 73.7 | 1.0 | -- |
| 1978 | 60 | 78.3 | 0.94 (0.33,2.69) |
-- |
| 1981 | 75 | 76.0 | 0.76 (0.29,2.01) |
-- |
| 1984 | 48 | 77.1 | 0.56 (0.19,1.67) |
-- |
| 1986 | 58 | 79.3 | 1.05 (0.35,3.13) |
-- |
| 1988 | 60 | 81.7 | 1.48 (0.50,4.38) |
-- |
| 1990 | 37 | 81.1 | 0.60 (0.18,1.97) |
-- |
| 1991 | 61 | 65.6 | 0.52 (0.19,1.42) |
-- |
| 1993 | 55 | 70.9 | 0.49 (0.17,1.40) |
-- |
| 1995 | 81 | 50.6 | 0.20 (0.08,0.51) |
-- |
| 1997 | 74 | 58.1 | 0.22 (0.09,0.57) |
1.0 |
| 1999 | 66 | 68.2 | 0.30 (0.11,0.78) |
1.07 (0.36,3.16) |
| 2001 | 76 | 42.1 | 0.14 (0.05,0.34) |
0.90 (0.32,2.56) |
| 2003 | 47 | 48.9 | 0.12 (0.04,0.32) |
0.66 (0.22,1.97) |
| 2005 | 50 | 42.0 | 0.08 (0.03,0.23) |
0.31 (0.10,0.95) |
Regression #1 - Adjusted for patient's age, sex, length of hospital stay, history of diabetes, heart failure, or stroke, and AMI order
Regression #2 - Adjusted for patient's age, sex, length of hospital stay, and prior history of diabetes, heart failure, or stroke, AMI order, complete heart block, admission blood pressure, serum glucose, and estimated GFR findings, and receipt of do not resuscitate orders during hospitalization.
The authors had full access to, and take full responsibility for, the integrity of the data. All authors have read and agree to the manuscript as written.
Results
Patient Characteristics
The total study sample consisted of 13,663 greater Worcester residents hospitalized with AMI of whom 6.6% (n=905) developed cardiogenic shock. The mean age of the study sample was 68.9 years, 58.5% were men, and 95.2% were Caucasian.
Baseline Demographic and Clinical Characteristics
Patients who developed cardiogenic shock during hospitalization for AMI were significantly older, were more likely to be women, to have a do not resuscitate order, have a history of diabetes, heart failure, or MI, to present to greater Worcester hospitals with dyspnea, and develop a Q wave MI during hospitalization as compared to patients who did not develop cardiogenic shock (Table 1). Patients with cardiogenic shock had significantly lower blood pressure, total serum cholesterol, and estimated GFR findings at the time of hospital admission, but higher heart rates and serum glucose levels, than patients who did not develop shock.
To provide more contemporary insights into the characteristics of patients with AMI who were at risk for developing cardiogenic shock, we examined differences in these characteristics in patients hospitalized with AMI during our 3 most recent study years (Table 1); differences in the demographic characteristics of patients who did, as compared to those who did not, develop cardiogenic shock were no longer apparent whereas differences in previously observed clinical and physiologic factors remained.
Hospital Treatment Practices
Patients who developed cardiogenic shock during hospitalization for AMI were significantly less likely to be treated with aspirin, beta blockers, calcium channel blockers, and lipid lowering agents during hospitalization than patients who did not develop shock. Patients who developed cardiogenic shock were more likely to have been prescribed thrombolytic therapy, and to have undergone cardiac catheterization, coronary artery bypass surgery, and a PCI, than patients who did not experience cardiogenic shock (Table 2). Patients who developed cardiogenic shock were significantly more likely to have received mechanical support during hospitalization through intra-aortic balloon counterpulsation.
With specific regards to the elderly (≥65 years), those who developed cardiogenic shock were significantly less likely to have undergone cardiac catheterization (39.9%, 28.8%, 21.7%), a PCI (23.0%, 15.8%, 15.8%), coronary artery bypass surgery (7.0%, 6.0%, 0%), and received intra-aortic balloon counterpulsation (34.1%, 23.5%, 13.3%) with advancing age (65-74, 75-84, ≥85 years, respectively) (p<.001); similar age-related differences in the use of cardiac diagnostic and interventional procedures were observed in patients who did not develop cardiogenic shock.
In examining differences in the use of these treatment practices in patients who were hospitalized in our 3 most recent study years (Table 2), differences in the use of various treatment approaches either no longer remained apparent or became attenuated. The use of beneficial cardiac medications increased markedly over time in patients with AMI, irrespective of the development of cardiogenic shock. The use of thrombolytic therapy considerably declined in both patient groups during recent years while the use of PCI and intra-aortic balloon counterpulsation increased markedly.
Changing Trends in the Incidence Rates of Cardiogenic Shock
Between 1975 and the late 1980's, the incidence of cardiogenic shock remained relatively stable averaging approximately 7.5% over this period (Figure 1). While the proportion of patients with AMI who developed cardiogenic shock during hospitalization was somewhat inconsistent thereafter, beginning in 1990 declines in the incidence rates of cardiogenic shock were observed reaching a nadir in incidence rates of 4.1% in 2003. Overall, there were significant changes in the frequency of cardiogenic shock complicating AMI during the years under study (p<0.01). Of the patients who developed cardiogenic shock, approximately 78% of these patients either presented with, or developed, this hemodynamic disturbance during the first day of hospitalization during our first 3 study years (1975/78/81) as compared to approximately 77% in our 3 most recent years under investigation.
Among the elderly, the overall incidence rates of cardiogenic shock did not vary appreciably (65-74 years 7.3%; 75-84 years 8.2%; ≥85 years 7.0%). In 2003 and 2005, the incidence rates of cardiogenic shock declined with advancing age (65-74 years 6.8%; 75-84 years 4.9%; ≥85 years 4.1%).
We carried out a series of regression analyses to examine differences from the baseline study year of 1975 in the rates of cardiogenic shock while controlling for several factors that might affect the likelihood of developing shock in patients with AMI (Table 3). The results of these analyses were similar to those of our unadjusted analyses of declines in the incidence rates of cardiogenic shock during the most recent years under investigation. Statistically significant declines in the proportion of patients with AMI who developed cardiogenic shock were noted during 2001, 2003, and 2005 (compared to the referent year of 1975). Similar, albeit attenuated, changes were observed in the risk of developing shock between 1997 and 2005 when information about whether the MI was an ST segment, or non ST segment, elevation MI was available as well as when data were collected about additional physiologic findings.
Hospital Case-Fatality Rates
Overall, 65.4% of patients with AMI who developed cardiogenic shock died during hospitalization in comparison to 10.6% of patients who did not develop cardiogenic shock (p<.001). In elderly patients with AMI, the overall hospital CFR's associated with cardiogenic shock increased with advancing age (65-74 years 65.1%; 75-84 years 75.8%; ≥85 years 75.2%).
A logistic regression analysis was carried out for purposes of examining the association between occurrence of cardiogenic shock and hospital CFR's while controlling for several demographic and clinical factors of prognostic importance. The results of this analysis confirmed the markedly higher risk of dying during hospitalization among patients who developed cardiogenic shock as compared to those who did not (adjusted O.R. = 17.8, 95% CI 14.5, 20.9). When we restricted our analysis to patients hospitalized during 2003 and 2005, patients with cardiogenic shock remained at markedly increased risk for dying during hospitalization in comparison to patients who did not develop cardiogenic shock, though the absolute risk of dying for patients with cardiogenic shock was considerably lower than during earlier study years (adjusted O.R. = 12.5; 95% CI 7.81,19.83).
In examining changing short-term death rates associated with cardiogenic shock (Figure 2), in 1975/1978, 76.1% of patients who developed cardiogenic shock died in the hospital compared with 16.5% of patients who did not develop this complication. However, in 2003 and 2005, 45.4% of patients with shock died during hospitalization compared to 7.3% of patients who did not develop shock (p<.001) (Table 4).
Patients who developed cardiogenic shock during the most recent years under study were significantly less likely to have died in comparison to patients hospitalized with AMI in the 1970's and 1980's (Table 4). These trends were apparent irrespective of the demographic or clinical characteristics controlled for.
In 2003/2005, the hospital death rates associated with cardiogenic shock increased with advancing age in the elderly from 35.7% in patients 65-74 years to 57.1% and 64.7% in patients 75-84 and ≥85 years, respectively.
Since the length of hospital stay has markedly declined in our study population over the past 30 years (mean = 18 days in 1975; mean = 5 days in 2005), we examined changing trends in the 30 day CFR's after hospital presentation in patients who developed cardiogenic shock. The results of this analysis confirmed the declining short-term death rates in patients who developed cardiogenic shock over time. In 1975/78, the 30 day death rates after hospital admission for patients with cardiogenic shock were 20.7%; these death rates were 17.0% in 1990/91 and 12.8% in 2003/05.
Characteristics of Hospital Survivors With Cardiogenic Shock
Patients who survived an episode of cardiogenic shock were significantly younger, were less likely to have had a history of coronary disease or heart failure, were more likely to have higher diastolic blood pressure findings and higher levels of eGFR, and were more likely to have been treated with effective cardiac medications and interventional procedures than patients who died from cardiogenic shock (Table 5). Similar findings were observed when we compared patients who died from cardiogenic shock from those who survived this clinical syndrome in our 3 most recent study years.
Table 5. Characteristics of Patients With Cardiogenic Shock Complicating Acute Myocardial Infarction (AMI) According to Hospital Survival Status.
| Total Sample | |||
|---|---|---|---|
| Survived (n=312) |
Died (n=592) |
P Value | |
| Characteristic | |||
| Age (mean, yrs) | 67.7 | 73.9 | <.001 |
| Male sex (%) | 55.6 | 52.2 | 0.33 |
| Body mass index (%) | |||
| <25 | 41.2 | 39.5 | 0.83 |
| 25-29.9 | 38.6 | 37.4 | |
| ≥30 | 20.3 | 23.1 | |
| Duration of prehospital delay (mean hrs)** | 4.3 | 1.0 | 0.09 |
| Do not resuscitate order*** | 18.4 | 59.9 | <0.001 |
| Medical history (%) | |||
| Angina | 21.1 | 27.7 | <0.05 |
| Diabetes | 32.0 | 32.3 | 0.92 |
| Heart failure | 17.3 | 26.4 | <0.01 |
| Hypertension | 58.5 | 55.2 | 0.35 |
| Stroke | 9.3 | 12.3 | 0.16 |
| Acute Presenting Symptoms (%) | |||
| Chest pain* | 69.0 | 72.7 | 0.16 |
| Diaphoresis* | 39.6 | 37.6 | 0.48 |
| Dyspnea* | 64.5 | 57.5 | <.05 |
| AMI characteristics (%) | |||
| Initial | 63.9 | 57.9 | 0.08 |
| Q wave | 52.1 | 58.5 | 0.07 |
| Clinical Complications (%) | |||
| Atrial fibrillation | 32.6 | 29.1 | 0.27 |
| Third degree heart block | 14.4 | 16.4 | 0.43 |
| Heart failure | 74.7 | 66.5 | 0.01 |
| Stroke** | 1.2 | 1.5 | 0.75 |
| Physiologic findings at the time of hospital admission (mean) | |||
| Systolic blood pressure (mmHg) | 120.7 | 118.4 | 0.60 |
| Diastolic blood pressure (mmHg) | 72.0 | 66.6 | <0.05 |
| Heart rate (bpm)** | 90.1 | 86.9 | 0.18 |
| Laboratory findings at the time of hospital admission (mean, mg/dl) | |||
| eGFR (%)**** | 55.5 | 46.7 | <0.001 |
| Serum glucose**** | 241.3 | 217.3 | 0.07 |
| Serum cholesterol | 191.7 | 195.6 | 0.53 |
| Medications (%) | |||
| Angiotensin converting enzyme inhibitors* | 75.1 | 28.0 | <.001 |
| Aspirin | 71.9 | 41.7 | <0.001 |
| Beta blockers | 62.6 | 28.4 | <0.001 |
| Calcium channel blockers | 28.5 | 24.4 | 0.24 |
| Lipid lowering agents** | 36.3 | 10.0 | <0.001 |
| Thrombolytics | 24.2 | 15.4 | <0.01 |
| Procedures (%) | |||
| Cardiac catheterization | 58.8 | 23.7 | <0.001 |
| Coronary artery bypass graft | 11.9 | 4.0 | <0.001 |
| Percutaneous coronary intervention | 46.5 | 17.7 | <0.001 |
| Intraortic balloon counterpulsation | 44.7 | 21.7 | <.001 |
90-05 only
86-05 only
91-05 only
95-05 only
Discussion
The results of our population-based observational study provide insights into changing trends in the magnitude, management, and hospital outcomes of patients with cardiogenic shock complicating AMI as well as to the characteristics of patients likely to develop, as well as survive, cardiogenic shock.
Incidence Rates of Cardiogenic Shock
The incidence rates of cardiogenic shock after AMI have ranged from 5 to 15 percent in previously published studies. This relatively wide range reflects the varying definitions of AMI and cardiogenic shock utilized, use of representative as opposed to more highly selected patient samples, time periods under study, and use of therapeutic options that may reduce the risk of cardiogenic shock. The overall incidence rates of cardiogenic shock observed in the current study fall within this range.
The relatively few studies that have examined changing trends in the incidence rates of cardiogenic shock after AMI have yielded conflicting results. In the National Hospital Discharge Survey, declines in the frequency of cardiogenic shock were observed between 1979 and the early 2000's, in concert with increasing utilization rates of PCI (12). In contrast, findings from the National Registry of Myocardial Infarction showed either stable, or slightly increasing, incidence rates of cardiogenic shock over the 10 year period beginning in 1995 in patients hospitalized with ST-segment elevation MI (5).
The results of our study suggest that patients hospitalized with AMI in the 2000's were less likely to develop cardiogenic shock than greater Worcester residents hospitalized with AMI during earlier study years. This finding is all the more impressive given the considerable aging of our patient population and increasing prevalence of serious comorbidities including diabetes, heart failure, and prior stroke (17).
While we cannot ascertain the reasons behind these encouraging trends, there are a number of likely contributory factors. We have previously documented progressive declines since the mid-1970s in the hospital death rates of greater Worcester residents hospitalized with AMI at all area medical centers (15-17). Patients presenting with AMI in recent study years were more likely to have had prior MIs or present with a non-Q wave MI than during early study years. This may explain some of the changes in the incidence rates of cardiogenic shock that were found in the present study as well as in our earlier investigations.
Early revascularization, particularly via percutaneous intervention in patients with ST-segment elevation AMI, has been shown to decrease infarct size, hemodynamic compromise, and improve patient survival. Due to our data collection methods, we were unable to examine the association between the increased use of coronary reperfusion and revascularization strategies and the risk of developing, or dying after, cardiogenic shock. Nevertheless, our data and the findings from other recent investigations shows a significant increase in the utilization of primary PCI over the past decade for the treatment of patients hospitalized with AMI. Significant resources in our community (as in others) have been spent attempting to improve the timeliness with which revascularization is performed in these patients. While gains in “time from hospital presentation to balloon initiation” appear promising, efforts to decrease the extent of delay from symptom onset to hospital presentation remain frustrated. Indeed, the average duration of prehospital delay in patients presenting with cardiogenic shock during our most recent study years was nearly 4 hours.
Other possible reasons for the observed decline in the incidence rates of cardiogenic shock may include increased monitoring efforts, particularly of patient populations at increased risk for developing shock, use of increasingly effective cardiac medications for the secondary prevention of recurrent events, and careful attention to the maintenance of desirable hemodynamic parameters in patients with AMI.
Factors Associated With Cardiogenic Shock
Efforts to decrease the risk of developing cardiogenic shock in patients with AMI should focus on identifying patients who are at high risk for this serious complication and instructing them to seek care immediately after the onset of acute coronary symptoms so that appropriate monitoring, risk stratification, and intervention can be undertaken. Aggressive intervention may result in improved survival rates among patients in whom cardiogenic shock has developed (9,11,18). In the present study, patients who developed cardiogenic shock were older, more likely to be women, present with prior cardiovascular disease, or experience various physiologic findings than patients without shock.
Hospital Case-Fatality Rates After Cardiogenic Shock
Patients in whom cardiogenic shock developed continue to have a markedly higher risk of dying in the hospital than patients who did not develop cardiogenic shock. However, the hospital prognosis for greater Worcester residents hospitalized with cardiogenic shock has improved considerably during the most recent years under investigation. Between the mid-1970's and late 1980's slightly more than three quarters of patients who developed cardiogenic shock died during hospitalization; in contrast, approximately 2 out of every 5 patients who developed shock between 2001 and 2005 died. Much of this decline occurred coincident with the increasingly effective management of patients with AMI with cardiac medications and coronary intervention approaches. This improvement in hospital survival may be due to the increasingly aggressive intervention strategies used, or to changes in the natural history of shock, with fewer cases that subsequently result in death identified early in the course of the illness.
A number of nonrandomized studies suggest that PCI improves short-term survival in patients with cardiogenic shock, with survival contingent on the successful establishment of coronary reperfusion (19,20). Uncontrolled studies of coronary artery bypass grafting show that this revascularization approach improves short-term survival among patients with cardiogenic shock when they are treated soon after shock has developed (21). We were unable, however, to assess the role of these interventional procedures since we could not determine whether shock preceded, or came after, the utilization of these treatment strategies or determine other reasons why certain patients received these therapeutic regimens whereas others did not.
Analyses from the GUSTO-1 trial suggest that the use of a more aggressive revascularization strategy in patients with cardiogenic shock, after initial treatment with a thrombolytic regimen, is associated with a reduction in short-term mortality after AMI (11). Findings from the SHOCK trial suggest benefits on 1 year survival with emergency revascularization and use of intra-aortic counterpulsation (18,22). In the National Registry of Myocardial Infarction, there was a marked increase in the use of PCI in patients hospitalized for AMI at more than 650 medical centers between 1995 and 2004 and the increased utilization of this treatment strategy was associated with a marked decline in short-term mortality associated with cardiogenic shock (5).
In current guidelines, AMI complicated by cardiogenic shock is listed as a class IA indication for PCI and a class IA indication for CABG surgery if the patient has suitable coronary anatomy (14). In the National Hospital Discharge Survey (12), and the National Registry of Myocardial Infarction (5), mortality rates from cardiogenic shock declined to <50% during the most recent years under investigation of these studies. In the Global Registry of Acute Coronary Events (GRACE) project, improvements in the management of patients with an acute coronary syndrome were accompanied by reductions in the magnitude and mortality associated with cardiogenic shock between 1999 and 2006 (23).
Conclusions
Cardiogenic shock continues to develop at a relatively high rate, though apparently declining, after AMI. The hospital death rate among patients with this complication remains high, but continues to decline over time. While the results of the SHOCK trial are encouraging, it is unclear to what extent the broader pool of patients who develop cardiogenic shock are currently managed with an aggressive coronary revascularization or reperfusion approach. It remains to be seen whether current efforts aimed at reducing extent of pre-hospital delay and “door-to-balloon” times may lead to further declines in the incidence and case-fatality rates of cardiogenic shock after AMI. It remains important to examine contemporary trends in the magnitude and short-term outcomes associated with cardiogenic shock and develop a risk prognostication index for purposes of identifying patients most likely to develop this compromised hemodynamic state.
Acknowledgments
We wish to express our appreciation to all persons involved in the review of data for this project during the years under study.
Sources of Funding: Grant support for this project was provided by the National Heart, Lung, and Blood Institute (RO1 HL35434).
Footnotes
Conflict of Interest Disclosures: There are no conflicts of interest to report by any of the authors.
Short Commentary/Clinical Summary: The results of this population-based epidemiologic study demonstrate that cardiogenic shock remains a relatively frequent complication of acute myocardial infarction (AMI), affecting approximately 1 in every 15 patients hospitalized with AMI. While the incidence rates of cardiogenic shock have remained relatively stable over the past 30 years (1975-2005) in our investigation of residents of a large New England metropolitan area hospitalized at all area medical centers with AMI, encouraging improvements in the hospital survival of these high risk patients have occurred, coincident with the increasingly aggressive management of patients who developed cardiogenic shock. Our findings also provide insights into the characteristics of patients who died after an episode of cardiogenic shock to whom targeted surveillance as well as therapeutic efforts might be directed.
References
- 1.Killip T. Cardiogenic shock complicating myocardial infarction. J Am Coll Cardiol. 1989;14:47–48. [Google Scholar]
- 2.Hands ME, Rutherford JD, Muller JE, Davies G, Stone PH, Parker C, Braunwald E. The in-hospital development of cardiogenic shock after myocardial infarction: incidence, predictors of occurrence, outcome and prognostic factors: the MILIS Study Group. J Am Coll Cardiol. 1989;14:40–46. doi: 10.1016/0735-1097(89)90051-x. [DOI] [PubMed] [Google Scholar]
- 3.Domanski MJ, Topol EJ. Cardiogenic shock: current understandings and future research directions. Am J Cardiol. 1994;74:724–726. doi: 10.1016/0002-9149(94)90318-2. [DOI] [PubMed] [Google Scholar]
- 4.Califf RM, Bengston JR. Cardiogenic shock. N Engl J Med. 1994;330:1724–30. doi: 10.1056/NEJM199406163302406. [DOI] [PubMed] [Google Scholar]
- 5.Babaev A, Frederick PD, Pasta DJ, Every N, Sichrovsky T, Hochman JS NRMI investigators. Trends in management and outcomes of patients with acute myocardial infarction complicated by cardiogenic shock. JAMA. 2005;294:448–454. doi: 10.1001/jama.294.4.448. [DOI] [PubMed] [Google Scholar]
- 6.Goldberg RJ, Gore JM, Alpert JS, Osganian V, de Groot J, Bade J, Chen Z, Frid D, Dalen JE. Cardiogenic shock after acute myocardial infarction: incidence and mortality from a community-wide perspective, 1975 to 1988. N Engl J Med. 1991;325:1117–1122. doi: 10.1056/NEJM199110173251601. [DOI] [PubMed] [Google Scholar]
- 7.Goldberg RJ, Samad NA, Yarzebski J, Gurwitz J, Bigelow C, Gore JM. Temporal trends (1975-1997) in the incidence and hospital death rates of cardiogenic shock complicating acute myocardial infarction (Worcester Heart Attack Study) N Engl J Med. 1999;340:1162–1168. doi: 10.1056/NEJM199904153401504. [DOI] [PubMed] [Google Scholar]
- 8.Leor J, Goldbourt U, Reicher-Reiss H, Kaplinsky E, Behar S. Cardiogenic shock complicating acute myocardial infarction in patients without heart failure on admission: incidence, risk factors, and outcome. Am J Med. 1993;94:265–273. doi: 10.1016/0002-9343(93)90058-w. [DOI] [PubMed] [Google Scholar]
- 9.Hochman JS, Boland J, Sleeper LA, Porway M, Brinker J, Col J, Jacobs A, Slater J, Miller D, Wasserman H. Current spectrum of cardiogenic shock and effect of early revascularization on mortality: results of an international registry. Circulation. 1995;91:873–881. doi: 10.1161/01.cir.91.3.873. [DOI] [PubMed] [Google Scholar]
- 10.Holmes DR, Jr, Califf RM, Van de Werf F, Berger PB, Bates ER, Simoons ML, White HD, Thompson TD, Topol EJ. Difference in countries' use of resources and clinical outcome for patients with cardiogenic shock after myocardial infarction: results from the GUSTO trial. Lancet. 1997;349:75–78. doi: 10.1016/s0140-6736(96)03031-0. [DOI] [PubMed] [Google Scholar]
- 11.Berger PB, Holmes DR, Jr, Stebbins AL, Bates ER, Califf RM, Topol EJ. Impact of an aggressive invasive catheterization and revascularization strategy on mortality in patients with cardiogenic shock in the Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries (GUSTO-I) trial: an observational study. Circulation. 1997;96:122–127. doi: 10.1161/01.cir.96.1.122. [DOI] [PubMed] [Google Scholar]
- 12.Fang J, Mensah GA, Alderman MH, Croft JB. Trends in acute myocardial infarction complicated by cardiogenic shock, 1979-2003, United States. Am Heart J. 2006;152:1035–1041. doi: 10.1016/j.ahj.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 13.Urban P, Stauffer JC, Bleed D, Khatchatrian N, Amann W, Bertel O, van den Brand M, Danchin N, Kaufmann U, Meier B, Machecourt J, Pfisterer M. A randomized evaluation of early revascularization to treat shock complicating acute myocardial infarction. The (Swiss) Multicenter Trial of Angioplasty for Shock-(S)MASH. Eur Heart J. 1999;20:1030–1038. doi: 10.1053/euhj.1998.1353. [DOI] [PubMed] [Google Scholar]
- 14.Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC, Jr, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK. American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction—executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2004;110:588–636. doi: 10.1161/01.CIR.0000134791.68010.FA. [DOI] [PubMed] [Google Scholar]
- 15.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Recent changes in attack and survival rates of acute myocardial infarction (1975 through 1981): the Worcester Heart Attack Study. JAMA. 1986;255:2774–2779. [PubMed] [Google Scholar]
- 16.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. A two-decades (1975-1995) long experience in the incidence, in-hospital and long-term case-fatality rates of acute myocardial infarction: A community-wide perspective. J Am Coll Cardiol. 1999;33:1533–1539. doi: 10.1016/s0735-1097(99)00040-6. [DOI] [PubMed] [Google Scholar]
- 17.Goldberg RJ, Spencer FA, Yarzebski J, Lessard D, Gore JM, Alpert JS, Dalen JE. A 25-year perspective into the changing landscape of patients hospitalized with acute myocardial infarction (the Worcester Heart Attack Study) Am J Cardiol. 2004;94:1373–1378. doi: 10.1016/j.amjcard.2004.07.142. [DOI] [PubMed] [Google Scholar]
- 18.Hochman JS, Sleeper LA, Webb JG, Sanborn TA, White HD, Talley JD, Buller CE, Jacobs AK, Slater JN, Col J, McKinlay SM, LeJemtel TH, Picard MH, Menegus MA, Boland J, Dzavik V, Thompson CR, Wong SC, Steingart R, Forman R, Aylward PE, Godfrey E, Desvigne-Nickens P SHOCK Investigators. Early revascularization in acute myocardial infarction complicated by cardiogenic shock. N Engl J Med. 1999;341:625–634. doi: 10.1056/NEJM199908263410901. [DOI] [PubMed] [Google Scholar]
- 19.Gacioch GM, Ellis SG, Lee L, Bates ER, Kirsh M, Walton JA, Topol EJ. Cardiogenic shock complicating acute myocardial infarction: the use of coronary angioplasty and the integration of the new support devices into patient management. J Am Coll Cardiol. 1992;19:647–653. doi: 10.1016/s0735-1097(10)80286-4. [DOI] [PubMed] [Google Scholar]
- 20.O'Neill WW. Angioplasty therapy of cardiogenic shock: are randomized trials necessary? J Am Coll Cardiol. 1992;19:915–917. doi: 10.1016/0735-1097(92)90270-w. [DOI] [PubMed] [Google Scholar]
- 21.Bolooki H. Emergency cardiac procedures in patients in cardiogenic shock due to complications of coronary artery disease. Circulation. 1989;79 I:I-137–148. [PubMed] [Google Scholar]
- 22.Hochman JS, Sleeper LA, Webb JG, Dzavik V, Buller CE, Aylward P, Col J, White HD. Early revascularization and long-term survival in cardiogenic shock complicating acute myocardial infarction. JAMA. 2006;295:2511–2515. doi: 10.1001/jama.295.21.2511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fox KA, Steg PG, Eagle KA, Goodman SG, Anderson FA, Jr, Granger CB, Flather MD, Budaj A, Quill A, Gore JM. Decline in rates of death and heart failure in acute coronary syndromes, 1999-2006. JAMA. 2007;297:1892–1900. doi: 10.1001/jama.297.17.1892. [DOI] [PubMed] [Google Scholar]