Abstract
Background: Rotational knee movement after reconstruction of the anterior cruciate ligament has been difficult to quantify. The purpose of this study was to identify in vivo whether a more horizontal placement of the femoral tunnel (in the ten o'clock position rather than in the eleven o'clock position) can restore rotational kinematics, during highly demanding dynamic activities, in a knee in which a bone-patellar tendon-bone graft had been used to reconstruct the anterior cruciate ligament.
Methods: We evaluated ten patients in whom a bone-patellar tendon-bone graft had been used to reconstruct the anterior cruciate ligament with the femoral tunnel in the eleven o'clock position, ten patients who had had the same procedure with the femoral tunnel in the ten o'clock position, and ten healthy controls. Kinematic data were collected while the subjects (1) descended from a stairway, made foot contact, and then pivoted 90° on the landing lower limb and (2) jumped from a platform, landed with both feet on the ground, and pivoted 90° on the right or left lower limb. The dependent variable that we examined was tibial rotation during pivoting.
Results: The results demonstrated that reconstruction of the anterior cruciate ligament with the femoral tunnel in either the ten or the eleven o'clock position successfully restored anterior tibial translation. However, both techniques resulted in tibial rotation values, during the dynamic activities evaluated, that were significantly larger than those in the intact contralateral lower limbs and those in the healthy controls. Tibial rotation did not differ significantly between the two reconstruction groups or between the healthy controls and the intact contralateral lower limbs. However, we noticed that positioning the tunnel at ten o'clock resulted in slightly decreased rotation values that may have clinical relevance but not statistical significance.
Conclusions: Regardless of which of the two tested positions was utilized to fix the graft to the femur, reconstruction of the anterior cruciate ligament did not restore normal tibial rotation during dynamic activities.
Level of Evidence: Therapeutic Level II. See Instructions to Authors for a complete description of levels of evidence.
Anterior-posterior tibiofemoral translation remains the primary objective criterion for judging whether normal knee mechanics have been restored after a reconstruction of the anterior cruciate ligament. This parameter is measured clinically with the Lachman test or the anterior drawer test1. However, rotational knee movement after injury and reconstruction of the anterior cruciate ligament is difficult to quantify2-7. The only clinical test for examining rotation is the pivot-shift test, which is a subjective static measurement that can mask small rotational differences between the intact and the reconstructed knee. Thus, various researchers have assessed dynamic knee movement during activities of daily living in order to quantify rotation following reconstruction of the anterior cruciate ligament2-7. Such assessments are crucial because it has been reported recently that abnormal rotational movements of knees treated with reconstruction of the anterior cruciate ligament are related to the initiation of chondral degeneration8-10.
In vivo studies with three-dimensional motion analysis from our laboratory4-6 have demonstrated abnormal rotational knee movement during highly demanding activities after reconstruction of the anterior cruciate ligament. Our results have been verified by both in vitro and in vivo studies from other laboratories2,7,11-14. Furthermore, authors of in vitro studies have examined the possible causes of this phenomenon and have investigated the effects, on rotational knee kinematics, of the configuration and placement of the graft used to reconstruct the anterior cruciate ligament. It has been demonstrated that currently used methods for reconstruction of the anterior cruciate ligament are insufficient for controlling combined rotatory and valgus loads12,14. This finding has been attributed to the commonly used surgical technique of placing the graft in the femoral bone tunnel at the so-called eleven o'clock position in the right knee (and the one o'clock position in the left knee). This placement replicates the anatomy of the anteromedial bundle, but not the posterolateral bundle, of the anterior cruciate ligament. The posterolateral bundle originates more laterally and is important for knee stabilization against rotational loads15. Thus, it has been proposed that a more horizontal placement of the graft can address abnormal rotational knee movement after a reconstruction of the anterior cruciate ligament. However, this proposition has not been tested in in vivo studies that can identify how knee rotational kinematics are affected, to our knowledge.
The purpose of this study was to investigate in vivo the effect, on tibial rotation, of two different positions for the femoral tunnel in patients in whom the anterior cruciate ligament was reconstructed with a bone-patellar tendon-bone graft. We hypothesized that more horizontal placement of the graft (in the ten o'clock position) would be better than the standard eleven o'clock position for addressing abnormal rotational knee movement after a reconstruction of the anterior cruciate ligament.
Materials and Methods
Subjects
Twenty patients who required a reconstruction of the anterior cruciate ligament with a bone-patellar tendon-bone graft volunteered to participate in this prospective cohort study. Ten healthy subjects, matched with the treatment group in terms of sex, age, height, and weight, formed the control group; the mean age (and standard deviation) in that group was 29 ± 5 years, the mean weight was 76 ± 7 kg, and the mean height was 1.76 ± 0.09 m. The subjects scheduled for reconstruction of the anterior cruciate ligament were randomly assigned to two groups. In Group A, which consisted of ten patients (mean age, 30 ± 7 years; mean weight, 80 ± 11 kg; mean height, 1.79 ± 0.1 m), the femoral tunnel was placed more laterally—i.e., in the ten o'clock position in a right knee (or a two o'clock position in a left knee). In Group B, which consisted of ten patients (mean age, 28 ± 4 years; mean weight, 75 ± 6 kg; mean height, 1.79 ± 0.05 m), the femoral tunnel was placed more vertically—i.e., in the eleven o'clock position in a right knee (or a one o'clock position in a left knee). The tunnel positions were assessed intraoperatively with use of Kirschner wires and confirmed postoperatively with use of magnetic resonance imaging (Figs. 1-A and 1-B).
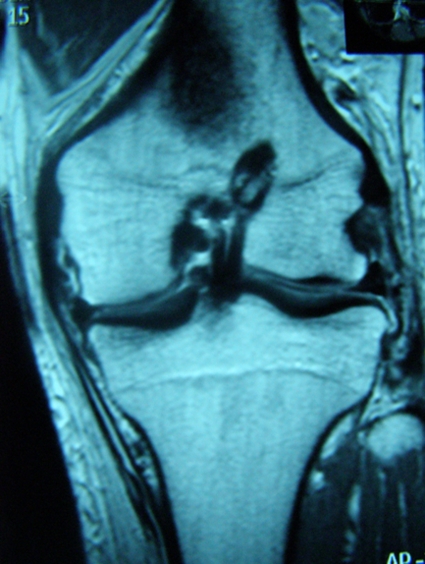
Fig. 1-A Fig. 1-A.
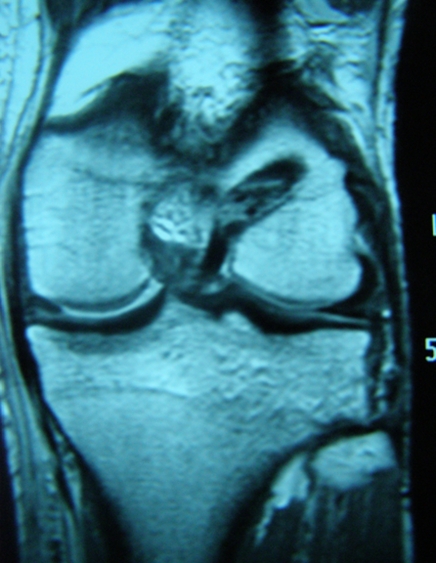
Figs. 1-A and 1-B Postoperative magnetic resonance imaging scans showing the two different positions for the femoral tunnel used in this study. Fig. 1-A The femoral tunnel was drilled at the one o'clock position (corresponding to the eleven o'clock position in a right knee). Fig. 1-B The femoral tunnel was drilled more laterally, at the two o'clock position (corresponding to the ten o'clock position in a right knee).
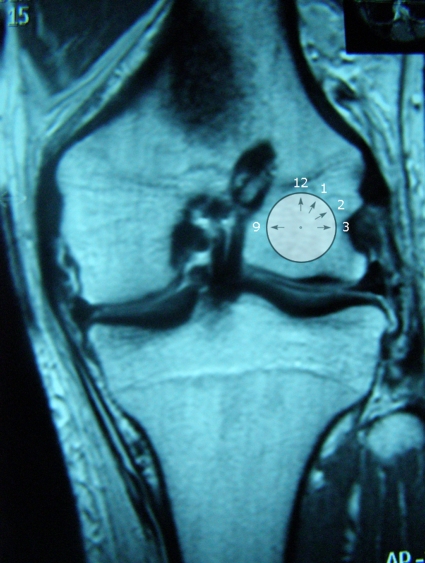
We used the system of the scientific committee of the European Society of Sports Traumatology, Knee Surgery and Arthroscopy16 to classify the position of the femoral tunnel on tunnel-view radiographs and on magnetic resonance imaging scans. According to that system, the femoral origin of the anterior cruciate ligament is identified in the frontal plane by drawing a circle around the intercondylar notch in a clockwise fashion (Fig. 2). The twelve o'clock position is located at the apex of the notch at the posterior wall, and all other positions are referenced from the twelve o'clock point according to the numbers on the face of a clock. Due to variations in notch sizes between knees and differences in femoral dimensions, the o'clock system has become a useful and accepted tool for consistently describing the position of the femoral tunnel. The authors of several scientific studies have used this classification to clarify the tunnel position17-19.
Fig. 2.
A magnetic resonance imaging scan indicating the “hours” according to the classification system of the scientific committee of the European Society of Sports Traumatology, Knee Surgery and Arthroscopy. The twelve o'clock position is located at the apex of the intercondylar notch at the posterior wall, while all other positions are referenced from the twelve o'clock point according to the numbers on the face of a clock.
Surgical Technique
All of the subjects were operated on by the senior author (A.D.G.). The drilling of the femoral tunnel was performed arthroscopically, through the anteromedial portal. With the knee in 90° of flexion, the posterior margin of the notch was clearly identified in order to ascertain the over-the-top position. This anatomical landmark was used to define the orientation in the femur and where the tunnel should be drilled. After marking the eleven o'clock position, we identified a point 7 to 10 mm (depending on the size of the knee) more laterally and always 5 mm beyond the cartilage border as the ten o'clock position. Then we slowly flexed the knee 120° to achieve good visualization to perform the drilling. The tibial tunnel was drilled in the center of the anterior cruciate ligament footprint, with the knee in 90° of flexion. The center of the tibial tunnel in the intra-articular space was slightly medial to the center of the intercondylar region on a line joining the inner edge of the anterior horn of the lateral meniscus and the medial tibial spine. With the knee joint in hyperextension and in the dorsal drawer position, we checked that this point was at least 5 mm dorsal to the roof of the intercondylar notch, to avoid impingement of the graft. We fixed the graft with bioabsorbable interference screws in both the femur and the tibia. After it was fixed in the femur, the graft was pulled manually from the tibial edge to place it under maximal tension. With the knee held in 25° to 30° of flexion20 and the graft held in tension as described, the graft was fixed in the tibial tunnel with the second interference screw.
Follow-up Evaluation
The patients were evaluated at an average of two years after the reconstruction of the anterior cruciate ligament. Both groups were allowed to return to sports-related activities at six months after the reconstruction, provided that they had regained full functional strength and stability. At that time, strength was determined with the Biodex isokinetic dynamometer (System 3; Biodex Medical Systems, Shirley, New York), which demonstrated acceptable symmetry of quadriceps and hamstrings strength. At the time of data collection, all patients had resumed their activities of daily living and sports activities. During the clinical evaluation, Tegner and Lysholm scores were obtained21 and anterior tibial translation was evaluated with use of the KT-1000 knee arthrometer (MEDmetric, San Diego, California) in both reconstruction groups and the healthy controls22.
Data Collection
An eight-camera optoelectronic system (Vicon-Peak Performance Technologies, Englewood, Colorado) sampling at 50 Hz was used to capture the movements of fifteen reflective markers placed on selected osseous landmarks of the lower limbs and the pelvis with use of the model described by Davis et al.23. The subjects were asked to perform two different activities: (1) descending from stairs and subsequent pivoting, and (2) landing from a 40-cm-high platform and subsequent pivoting. The stairway was constructed according to the description provided by Andriacchi et al.24, and the platform was designed according to the description provided by James et al.25.
It was important, to enable us to better analyze our kinematic data, to obtain a simultaneous recording of the signal describing the key events of the patient's gait cycle. Therefore, inline foot switches (Noraxon, Scottsdale, Arizona), with two sensors on each, were placed on the plantar surface of the shoes in the toe and heel positions. The foot-switch signals were collected with use of a Noraxon eight-channel telemetric system, which allowed the subjects to walk free of cables. Foot-switch data collection was time-synchronized with the kinematic data through the Vicon-Peak Performance Technologies digital transceiver. The signals provided by the foot switches were used to determine the exact time of the start and end of the pivoting period that was under evaluation.
During the first activity, the subjects descended the stairway at their own pace. The descending period was concluded on initial foot contact with the ground. After foot contact, the subjects pivoted (externally rotated) 90° on the landing (ipsilateral) lower limb and walked away. While pivoting, the contralateral lower limb swung around the body (as it was coming down from the stairway) and the trunk was oriented perpendicular to the stairway. During the second activity, the subjects folded their arms across their chest and then jumped from the platform and landed with both feet on the ground. After foot contact, the subjects pivoted (externally rotated) 90° on the right or left lower limb and walked away, as in the first activity. The pivoting period was identified as beginning with the initial contact of the ipsilateral foot with the ground and ending with touch-down of the contralateral lower limb. Each subject performed each activity with both lower limbs (i.e., using each as the pivoting limb) for six trials.
Data Analysis
Marker identification and angular displacement calculations were conducted with use of Vicon Motus (version 9.0; Vicon-Peak Performance Technologies) and MATLAB (version 7; The MathWorks, Natick, Massachusetts) software. Anthropometric measurements were combined with three-dimensional marker data from the anatomical position trial to provide positions of the joint centers and define anatomical axes of the joint rotations23. On the basis of our hypothesis, we identified the dependent variable to be examined in the present study as the range of motion of tibial rotation during the pivoting period of the two examined tasks. The selection of the range of motion as the dependent variable eliminated possible errors reported in the literature26,27 by investigators who used absolute (i.e., maximum) measures.
Statistical Analysis
One-way analysis of variance was performed on the group means to identify whether there were differences in the dependent variable between the limbs in which the anterior cruciate ligament graft had been fixed at the ten o'clock position (Group A) and the limbs in which it had been fixed at the eleven o'clock position (Group B) as well as between those groups and the control healthy lower limbs. This analysis was performed on the data obtained during both activities: (1) descending stairs and pivoting and (2) landing and pivoting. Post hoc analysis was performed if significant differences were identified with use of independent t tests. In addition, and as part of our post hoc analysis, paired t tests were performed within the two reconstruction groups to compare the treated and intact lower limbs. Similarly, independent t tests were conducted to compare the intact lower limbs of the two reconstruction groups and the limbs of the healthy controls. The level of significance was adjusted on the basis of the number of analyses of variance performed and was set at α = 0.025 (0.05 divided by two).
Ethical Considerations
This clinical trial was registered in the Current Controlled Trials public registry and was assigned the ISRCTN (International Standard Randomised Controlled Trial Number) 59873081. All subjects gave their consent for participation, according to the university institutional review board procedures. The original consent form was maintained in the investigators' files, and a copy was given to the subject at the time of consent. All subjects' physicians were in agreement with the testing protocol.
Source of Funding
This study was supported by a Hellenic Association of Orthopaedic Surgery and Traumatology (HAOST-EEXOT) research grant.
Results
Clinical
All subjects in both anterior cruciate ligament-reconstruction groups were satisfied with the outcome of the surgery and had resumed their preinjury level of sports participation. Negative Lachman, anterior drawer, and pivot-shift tests indicated that knee joint stability had been regained clinically in all subjects. The subjects in whom the femoral tunnel had been placed at ten o'clock (Group A) had a median Lysholm score of 94 points (range, 88 to 100 points) and a median Tegner score of 7 points (6, 7, or 8 points) at the time of examination, and the subjects in whom the femoral tunnel had been placed at eleven o'clock (Group B) had a median Lysholm score of 95 points (range, 92 to 100 points) and a median Tegner score of 7 points (6, 7, or 8 points). The healthy controls had a median Lysholm score of 99 points (range, 97 to 100 points) and a median Tegner score of 8 points (range, 7 to 9 points).
Testing with the KT-1000 arthrometer revealed that the mean difference in anterior tibial translation between the reconstructed and intact sides in Group A was 1.8 mm (range, 0.3 to 2.3 mm) with application of a 134-N load and 2.2 mm (range, 0.6 to 2.8 mm) with a maximum manual force. The values for Group B were 1.5 mm (range, 1 to 2 mm) and 1.7 mm (range, 1 to 2 mm), respectively.
Kinematics
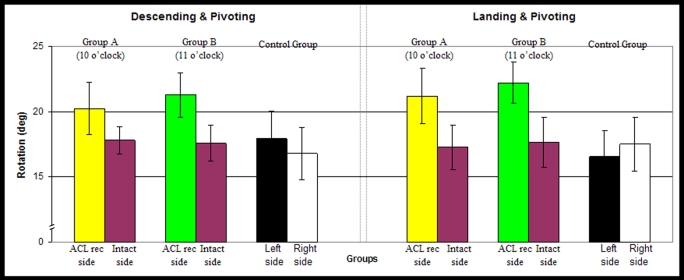
One-way analysis of variance showed a significant difference in the dependent variable among the three groups during the task involving descending stairs and pivoting (F = 8.948; p = 0.001) and during the landing-and-pivoting task (F = 6.918; p = 0.003) (Fig. 3).
Fig. 3.
Bar graphs demonstrating the group means and standard deviations in degrees for the maximum range of tibial rotation during the pivoting period of two activities: (1) descending and pivoting and (2) landing and pivoting. ACL rec = reconstruction of the anterior cruciate ligament.
The post hoc comparisons revealed significant differences, during both activities, between the control group and the subjects in whom the femoral tunnel for the anterior cruciate ligament reconstruction had been placed in the ten o'clock position (Group A) (p = 0.003 for descending and pivoting and p = 0.02 for landing and pivoting) as well as between the control group and the subjects in whom the femoral tunnel had been placed in the eleven o'clock position (Group B) (p = 0.008 for descending and pivoting and p = 0.001 for landing and pivoting). The post hoc analysis showed no significant differences between the two anterior cruciate ligament-reconstruction groups (p = 0.360 for descending and pivoting and p = 0.426 for landing and pivoting). No significant differences were found, during either activity, between the knees in the control group and the intact contralateral knees in the reconstruction groups (Group A: p = 0.086 for descending and pivoting and p = 0.707 for landing and pivoting; Group B: p = 0.094 for descending and pivoting and p = 0.57 for landing and pivoting) (Fig. 3). Significant differences were found between the intact and treated sides in both reconstruction groups and during both activities (Group A: p = 0.002 for descending and pivoting and p = 0.004 for landing and pivoting; Group B: p = 0.001 for descending and pivoting and p = 0.0002 for landing and pivoting) (Fig. 3).
Discussion
We evaluated in vivo the rotational kinematics of knees in which the anterior cruciate ligament had been reconstructed with a bone-patellar tendon-bone graft after random assignment to one of two groups defined according to the position of the graft tunnel in the femur. We investigated the knee rotational kinematics during two high-demand activities that place both anteriorly directed and rotational loads on the knee joint. As has been done in previous studies4-6, we studied tasks that increased demands on the knee to uncover rotational differences resulting from the reconstruction. We hypothesized that a more horizontal placement of the graft (at the ten o'clock rather than the standard eleven o'clock position) can better address abnormal rotational knee movement after a reconstruction of the anterior cruciate ligament. This hypothesis was based on the proposition that such placement better replicates the anatomy of the natural anterior cruciate ligament. However, the experimental results refuted our hypothesis. We did note that the ten o'clock position resulted in slightly decreased tibial rotation values, which may have clinical relevance but not statistical significance.
Interestingly, the results of the commonly used clinical pivot-shift test were normal for all of our patients. At the same time, the in vivo kinematic evaluation demonstrated abnormally increased rotational values. This contradiction may be due to the subjective nature of the pivot-shift test and its low sensitivity. Considering that the in vivo investigation showed a difference in tibial rotation of <5° between the groups and between the sides, it is possible that this difference was masked during the pivot-shift test by intraobserver and intrasubject variability. An alternative explanation is that the rotational load applied to the knee joint during the pivot-shift test is considerably less than the load applied to the knee joint during the investigated dynamic movements. It should be emphasized that the increased rotation that was found in the subjects treated with the anterior cruciate ligament reconstruction does not mean that the knees were unstable during the performance of the activities. It means that, compared with the intact contralateral knees and the healthy control knees, the reconstructed knees had an abnormal movement pattern in the transverse plane during the performance of these activities.
Correct selection of the femoral tunnel position is a critical step in the surgical procedure. Authors of previous studies have investigated the performances of several different femoral tunnel positions. Hefzy et al.28 described positions producing the best graft isometry and reported that no femoral positions resulted in complete isometry. Zavras et al.29 found that femoral tunnel positions located closest to the Blumensaat line (the twelve o'clock position) resulted in the most isometry. However, studies of the natural anterior cruciate ligament have shown that it has a complex anatomical structure and does not obey the rules of isometry. A femoral tunnel oriented at eleven o'clock in the intercondylar notch has been considered the standard and has been accepted as the correct tunnel location for all individuals17,18. This assumption was based on the fact that the femoral bone tunnel at this position best replicated the origin of the anteromedial bundle. However, the anterior cruciate ligament does not function as a simple band of fibers with constant tension as the knee moves. Its two bundles exhibit different tension patterns and are susceptible to different forces30. When the knee is extended, the posterolateral bundle is tight and the anteromedial bundle is moderately lax. As the knee is flexed, the femoral attachment of the anterior cruciate ligament assumes a more horizontal orientation, causing the anteromedial bundle to tighten and the posterolateral bundle to loosen30. Thus, it seems that this structural complexity of the anterior cruciate ligament cannot be restored by a reconstruction performed with the femoral tunnel in the standard eleven o'clock position. Recent in vitro studies have shown that an anterior cruciate ligament graft placed in this position is insufficient to limit more complex rotatory loads that include valgus and axial tibial torques12,14. Therefore, it has been proposed that a more horizontal placement of the graft (in the ten o'clock position), which increases the frontal plane obliquity of the graft, can better replicate the movement of the natural anterior cruciate ligament and improve rotational stability as the function of the posterolateral bundle is also taken into consideration. However, in our study, both of the anterior cruciate ligament-reconstruction groups had significantly greater tibial rotation during dynamic activities than did the healthy controls or the intact contralateral lower limbs. No significant differences were found between the two reconstruction groups, which demonstrates that a more horizontal placement of the femoral tunnel (at the ten o'clock position) cannot fully restore normal tibial rotation. Our results are supported by an in vitro investigation by Loh et al.19, who found that neither femoral tunnel position completely restored the kinematics and the in situ forces to the levels found in the intact knee.
We believe that our results emphasize the three-dimensional nature of the anterior cruciate ligament. A more horizontal drilling of the femoral tunnel is related to the positioning of the graft with respect to the frontal plane. However, the graft also has to be fixed to the tibia. It is possible that the position in which the tibial tunnel is drilled affects rotational results, in terms of the final three-dimensional obliquity of the graft within the knee. While there is general agreement regarding the placement of the tibial tunnel during a reconstruction of the anterior cruciate ligament31,32, current surgical techniques utilizing uniform grafts cannot reproduce the natural proximal or distal insertions of the anterior cruciate ligament. In vitro studies have shown that, in the sagittal plane, the tibial insertion site is nearly twice as wide as the midsubstance of the ligament33,34. This wide anterior insertion results in the twisting of the anterior cruciate ligament fibers, and this configuration seems to allow full extension of the knee without impingement on the femoral notch35. Because of differences in the shapes and sizes of the grafts, selection of the location for the tibial tunnel in the sagittal plane is a challenging decision for the surgeon. Placement of the tunnel at the center of the tibial footprint of the anterior cruciate ligament will probably reproduce the original obliquity of the anterior cruciate ligament in the sagittal plane, but the position will be too anterior in relation to the intercondylar roof. Thus, there will be a high risk of impingement of the graft on the roof. The alternative is to place the tibial tunnel slightly more posterior, with the graft centered and aligned with the bulk of the fibers of the anterior cruciate ligament36,37. This type of reconstruction (i.e., more vertical positioning of the graft) may result in a functional graft that will not impinge on the roof, but it will not reproduce the actual anatomy of the native anterior cruciate ligament. Two recent magnetic resonance imaging studies have shown that contemporary anterior cruciate ligament grafts are more vertical than the native anterior cruciate ligament38,39. Therefore, we propose that a reconstruction of the anterior cruciate ligament should be performed with consideration of the three-dimensional positioning of the ligament within the knee. We believe that a reconstruction of the anterior cruciate ligament that combines more horizontal femoral positioning with improvements in the tibial drilling can better reproduce the actual anatomy of the native anterior cruciate ligament.
It is worth mentioning that the slightly decreased tibial rotation values seen with the ten o'clock positioning of the femoral tunnel in the present study may have clinical relevance. A difference of only 1° to 2° in the decrease in tibial rotation due to this technique may not produce statistically significant results, since the actual differences between the values for reconstructed and native ligaments are of a magnitude of 5° to 6° (Fig. 3). However, excessive tibial rotation has been linked to the eventual development of osteoarthritis at the knee40. Since degeneration of the knee is an accumulative overuse effect, it is possible that even such a small change in tibial rotation can have a longitudinal impact in terms of a delay in the development of pathological changes in the knee. This hypothesis is currently under investigation in our laboratory.
Limitations of the present study include the known drawbacks of gait analysis26,27. We tried to address these limitations with more careful experimentation procedures. We minimized the interoperator error by having the same clinician (S.R.) place all of the markers and obtain all of the anthropometric measurements. The absolute three-dimensional marker reconstruction error of the system was very low (maximum standard deviation, 0.303 mm; calibration space, approximately 8 m3). We recorded data during an additional trial in the anatomical position for each subject, and that was used as a reference for the calculation of the anatomical angles (standing calibration). We also incorporated two different control conditions (the intact contralateral lower limb in both patient groups and a separate healthy control group) to ensure the existence of differences in our dependent variable. In addition, we used inline foot switches in order to have a precise recording of the exact time frame of the pivoting movement and to define the exact key events of the patient's gait cycle.
Since the same instrumentation was used for all subjects, the level of measurement noise would be consistent for all subjects; thus, any differences that were observed can be attributed to changes within the system itself. Each subject performed each activity with both lower limbs (i.e., use of each as the pivoting limb) for six trials in order to decrease within-subject variability, and we avoided references to maxima and minima of motion as range-of-motion values are more scientifically justifiable. We strongly believe that the incorporation of all of the above precautions strengthened the conclusions drawn from the gait analysis. Furthermore, gait analysis is widely accepted and is considered to be a well-established and reliable method41,42. Finally, all of the effect sizes of our significant comparisons were found to be >0.8. Such effect sizes are considered to be “large” according to Cohen43.
Experimental in vitro models cannot duplicate the variety of physiologic scenarios encountered throughout the spectrum of life's everyday activities. Therefore, the in vivo assessment of the subtle biomechanical nature of the knee joint is critical to our understanding of the short-term and long-term implications of reconstructive surgery. In conclusion, we found that tibial rotation during dynamic activities was not restored by reconstruction of the anterior cruciate ligament regardless of which of two tested positions was utilized to fix the graft to the femur. 
Disclosure: In support of their research for or preparation of this work, one or more of the authors received, in any one year, outside funding or grants of less than $10,000 from the Hellenic Association of Orthopaedic Surgery and Traumatology (HAOST-EEXOT). Neither they nor a member of their immediate families received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity. No commercial entity paid or directed, or agreed to pay or direct, any benefits to any research fund, foundation, division, center, clinical practice, or other charitable or nonprofit organization with which the authors, or a member of their immediate families, are affiliated or associated.
Investigation performed at the Orthopaedic Sports Medicine Center, Ioannina, Greece
References
- 1.Draganich LF, Vahey JW. An in vitro study of anterior cruciate ligament strain induced by quadriceps and hamstrings forces. J Orthop Res. 1990;8:57-63. [DOI] [PubMed] [Google Scholar]
- 2.Brandsson S, Karlsson J, Sward L, Kartus J, Eriksson BI, Kärrholm J. Kinematics and laxity of the knee joint after anterior cruciate ligament reconstruction: pre- and postoperative radiostereometric studies. Am J Sports Med. 2002;30:361-7. [DOI] [PubMed] [Google Scholar]
- 3.Bush-Joseph CA, Hurwitz DE, Patel RR, Bahrani Y, Garretson R, Bach BR Jr, Andriacchi TP. Dynamic function after anterior cruciate ligament reconstruction with autologous patellar tendon. Am J Sports Med. 2001;29:36-41. [DOI] [PubMed] [Google Scholar]
- 4.Georgoulis AD, Papadonikolakis A, Papageorgiou CD, Mitsou A, Stergiou N. Three-dimensional tibiofemoral kinematics of the anterior cruciate ligament-deficient and reconstructed knee during walking. Am J Sports Med. 2003;31:75-9. [DOI] [PubMed] [Google Scholar]
- 5.Ristanis S, Giakas G, Papageorgiou CD, Moraiti T, Stergiou N, Georgoulis AD. The effects of anterior cruciate ligament reconstruction on tibial rotation during pivoting after descending stairs. Knee Surg Sports Traumatol Arthrosc. 2003;11:360-5. [DOI] [PubMed] [Google Scholar]
- 6.Ristanis S, Stergiou N, Patras K, Vasiliadis HS, Giakas G, Georgoulis AD. Excessive tibial rotation during high-demand activities is not restored by anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:1323-9. [DOI] [PubMed] [Google Scholar]
- 7.Tashman S, Collon D, Anderson K, Kolowich P, Anderst W. Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:975-83. [DOI] [PubMed] [Google Scholar]
- 8.Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50:3145-52. [DOI] [PubMed] [Google Scholar]
- 9.Asano H, Muneta T, Ikeda H, Yagishita K, Kurihara Y, Sekiya I. Arthroscopic evaluation of the articular cartilage after anterior cruciate ligament reconstruction: a short-term prospective study of 105 patients. Arthroscopy. 2004;20:474-81. [DOI] [PubMed] [Google Scholar]
- 10.Jomha NM, Borton DC, Clingeleffer AJ, Pinczewski LA. Long-term osteoarthritic changes in anterior cruciate ligament reconstructed knees. Clin Orthop Relat Res. 1999;358:188-93. [PubMed] [Google Scholar]
- 11.Logan MC, Williams A, Lavelle J, Gedroyc W, Freeman M. Tibiofemoral kinematics following successful anterior cruciate ligament reconstruction using dynamic multiple resonance imaging. Am J Sports Med. 2004;32:984-92. [DOI] [PubMed] [Google Scholar]
- 12.Scopp JM, Jasper LE, Belkoff SM, Moorman CT 3rd. The effect of oblique femoral tunnel placement on rotational constraint of the knee reconstructed using patellar tendon autografts. Arthroscopy. 2004;20:294-9. [DOI] [PubMed] [Google Scholar]
- 13.Yoo JD, Papannagari R, Park SE, DeFrate LE, Gill TJ, Li G. The effect of anterior cruciate ligament reconstruction on knee joint kinematics under simulated muscle loads. Am J Sports Med. 2005;33:240-6. [DOI] [PubMed] [Google Scholar]
- 14.Kanamori A, Zeminski J, Rudy TW, Li G, Fu FH, Woo SL. The effect of axial tibial torque on the function of the anterior cruciate ligament: a biomechanical study of a simulated pivot shift test. Arthroscopy. 2002;18:394-8. [DOI] [PubMed] [Google Scholar]
- 15.Gabriel MT, Wong EK, Woo SL, Yagi M, Debski RE. Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res. 2004;22:85-9. [DOI] [PubMed] [Google Scholar]
- 16.Amis AA, Beynnon B, Blankevoort L, Chambat P, Christel P, Durselen L, Friederich N, Grood E, Hertel P, Jakob RP, Muller W, O'Brien M, O'Connor J. Proceedings of the ESSKA scientific workshop on reconstruction of the anterior and posterior cruciate ligaments. Knee Surg Sports Traumatol Arthrosc. 1994;2:124-32. [DOI] [PubMed] [Google Scholar]
- 17.Fu FH, Bennett CH, Ma CB, Menetrey J, Lattermann C. Current trends in anterior cruciate ligament reconstruction. Part II. Operative procedures and clinical correlations. Am J Sports Med. 2000;28:124-30. [DOI] [PubMed] [Google Scholar]
- 18.Good L, Odensten M, Gillquist J. Sagittal knee stability after anterior cruciate ligament reconstruction with patellar tendon strip. A two-year follow-up study. Am J Sports Med. 1994;22:518-23. [DOI] [PubMed] [Google Scholar]
- 19.Loh JC, Fukuda Y, Tsuda E, Steadman RJ, Fu FH, Woo SL. Knee stability and graft function following anterior cruciate ligament reconstruction: comparison between 11 o'clock and 10 o'clock femoral tunnel placement. Arthroscopy. 2003;19:297-304. [DOI] [PubMed] [Google Scholar]
- 20.Höher J, Kanamori A, Zeminski J, Fu FH, Woo SL. The position of the tibia during graft fixation affects knee kinematics and graft forces for anterior cruciate ligament reconstruction. Am J Sports Med. 2001;29:771-6. [DOI] [PubMed] [Google Scholar]
- 21.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43-9. [PubMed] [Google Scholar]
- 22.Steiner ME, Brown C, Zarins B, Brownstein B, Koval PS, Stone P. Measurement of anterior-posterior displacement of the knee. A comparison of the results with instrumented devices and with clinical examination. J Bone Joint Surg Am. 1990;72:1307-15. [PubMed] [Google Scholar]
- 23.Davis RB 3rd, Õunpuu S, Tyburski D, Gage JR. A gait analysis data collection and reduction technique. Hum Mov Sci. 1991;10:575-87. [Google Scholar]
- 24.Andriacchi TP, Andersson GB, Fermier RW, Stern D, Galante JO. A study of lower-limb mechanics during stair-climbing. J Bone Joint Surg Am. 1980;62:749-57. [PubMed] [Google Scholar]
- 25.James CR, Bates BT, Dufek JS. Classification and comparison of biomechanical response strategies for accommodating landing impact. J Appl Biomech. 2003;19:106-18. [DOI] [PubMed] [Google Scholar]
- 26.Cappozzo A, Catani F, Leardini A, Benedetti MG, Croce UD. Position and orientation in space of bones during movement: experimental artifacts. Clin Biomech (Bristol, Avon). 1996;11:90-100. [DOI] [PubMed] [Google Scholar]
- 27.Reinschmidt C, van den Bogert AJ, Nigg BM, Lundberg A, Murphy N. Effect of skin movement on the analysis of skeletal knee joint motion during running. J Biomech. 1997;30:729-32. [DOI] [PubMed] [Google Scholar]
- 28.Hefzy MS, Grood ES, Noyes FR. Factors affecting the region of most isometric femoral attachments. Part II: the anterior cruciate ligament. Am J Sports Med. 1989;17:208-16. [DOI] [PubMed] [Google Scholar]
- 29.Zavras TD, Race A, Bull AM, Amis AA. A comparative study of “isometric” points for anterior cruciate ligament graft attachment. Knee Surg Sports Traumatol Arthrosc. 2001;9:28-33. [DOI] [PubMed] [Google Scholar]
- 30.Amis AA, Dawkins GP. Functional anatomy of the anterior cruciate ligament. Fibre bundle actions related to ligament replacements and injuries. J Bone Joint Surg Br. 1991;73:260-7. [DOI] [PubMed] [Google Scholar]
- 31.Jackson DW, Gasser SI. Tibial tunnel placement in ACL reconstruction. Arthroscopy. 1994;10:124-31. [DOI] [PubMed] [Google Scholar]
- 32.Canale ST, editor. Campbell's operative orthopaedics. 10th ed. Philadelphia: Mosby; 2003.
- 33.Harner CD, Baek GH, Vogrin TM, Carlin GJ, Kashiwaguchi S, Woo SL. Quantitative analysis of human cruciate ligament insertions. Arthroscopy. 1999;15:741-9. [DOI] [PubMed] [Google Scholar]
- 34.Odensten M, Gillquist J. Functional anatomy of the anterior cruciate ligament and a rationale for reconstruction. J Bone Joint Surg Am. 1985;67:257-62. [PubMed] [Google Scholar]
- 35.Sidles JA, Larson RV, Garbini JL, Downey DJ, Matsen FA 3rd. Ligament length relationships in the moving knee. J Orthop Res. 1988;6:593-610. [DOI] [PubMed] [Google Scholar]
- 36.Howell SM, Clark JA. Tibial tunnel placement in anterior cruciate ligament reconstructions and graft impingement. Clin Orthop Relat Res. 1992;283:187-95. [PubMed] [Google Scholar]
- 37.Morgan CD, Kalman VR, Grawl DM. Definitive landmarks for reproducible tibial tunnel placement in anterior cruciate ligament reconstruction. Arthroscopy. 1995;11:275-88. [DOI] [PubMed] [Google Scholar]
- 38.Ahn JH, Lee SH, Yoo JC, Ha HC. Measurement of the graft angles for the anterior cruciate ligament reconstruction with transtibial technique using postoperative magnetic resonance imaging in comparative study. Knee Surg Sports Traumatol Arthrosc. 2007;15:1293-300. [DOI] [PubMed] [Google Scholar]
- 39.Ayerza MA, Muscolo DL, Costa-Paz M, Makino A, Rondon L. Comparison of sagittal obliquity of the reconstructed anterior cruciate ligament with native anterior cruciate ligament using magnetic resonance imaging. Arthroscopy. 2003;19:257-61. [DOI] [PubMed] [Google Scholar]
- 40.Stergiou N, Ristanis S, Moraiti C, Georgoulis AD. Tibial rotation in anterior cruciate ligament (ACL)-deficient and ACL-reconstructed knees: a theoretical proposition for the development of osteoarthritis. Sports Med. 2007;37:601-13. [DOI] [PubMed] [Google Scholar]
- 41.Chambers HG, Sutherland DH. A practical guide to gait analysis. J Am Acad Orthop Surg. 2002;10:222-31. [DOI] [PubMed] [Google Scholar]
- 42.Gage JR. Gait analysis. An essential tool in the treatment of cerebral palsy. Clin Orthop Relat Res. 1993;288:126-34. [PubMed] [Google Scholar]
- 43.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum; 1988.