Abstract
In mammals, adipose tissue, composed of BAT and WAT, collaborates in energy partitioning and performs metabolic regulatory functions. It is the most flexible tissue in the body, because it is remodeled in size and shape by modifications in adipocyte cell size and/or number, depending on developmental status and energy fluxes. Although numerous reviews have focused on the differentiation program of both brown and white adipocytes as well as on the pathophysiological role of white adipose tissues, the importance of mitochondrial activity in the differentiation or the dedifferentiation programs of adipose cells and in systemic metabolic alterations has not been extensively reviewed previously. Here, we address the crucial role of mitochondrial functions during adipogenesis and in mature adipocytes and discuss the cellular responses of white adipocytes to mitochondrial activity impairment. In addition, we discuss the increase in scientific knowledge regarding mitochondrial functions in the last 10 years and the recent suspicion of mitochondrial dysfunction in several 21st century epidemics (ie, obesity and diabetes), as well as in lipodystrophy found in HIV-treated patients, which can contribute to the development of new therapeutic strategies targeting adipocyte mitochondria.
Adipocytes and, more generally, the adipose tissues are major actors in both obesity and the emergence of a cluster of associated diseases such as insulin resistance and type 2 diabetes mellitus (T2DM), cardiovascular diseases, hypertension, dyslipidemia, and even some cancers. Obesity and diabetes are now recognized as worldwide epidemics,1 with 1.6 billion people being overweight, of which 400 million are obese (body mass index ≥30) (World Health Organization, Geneva 2006).
Attention for adipocytes has increased ever since it has been found that these differentiated cells are not only able to store and release triglycerides (TGs) but also have an important endocrine activity. Indeed, adipocytes secrete “adipokines” (specific hormones and proinflammatory cytokines) to communicate systemically with other cell types and thus, importantly, contribute to the regulation of energy homeostasis.2 Adipose tissue is present in different interacting depots in the body. In addition to white adipose tissue (WAT), brown adipose tissue (BAT) can also be distinguished.3 Although BAT originates from the myogenic lineage,4 it shares many features of WAT that are discussed in this review. Because WAT is by far the largest depot in humans and, as a metabolically active, lipid storage and endocrine organ, its proper functioning is essential for health maintenance and is of primary importance for pharmaceutical and food industries.
A better understanding of the mechanisms involved in adipocyte differentiation, dedifferentiation (defined as the acquisition of a more primitive phenotype and gain of cell proliferative ability)5 and even trans-differentiation (a process related to reversion of one cell phenotype into another, ie, from white to brown adipocytes,6,7 which is still poorly experimentally documented), is required to unravel mechanisms underlying obesity and its symptomatic cohort of associated pathologies. This understanding may be used to develop new, original, and more effective therapeutic approaches that directly target intracellular pathways in adipocytes. Although the adipocyte differentiation program,8 as well as the activity/function and dys/malfunction of the endoplasmic reticulum (which play an important role in the adipocyte physiology) have been recently reviewed,9 the role of mitochondrial activity or dysfunction during preadipocyte differentiation and its consequences in mature adipocytes has hardly been addressed. Subcutaneous and visceral WATs have a different metabolic activity, depending on their anatomical position and mitochondrial content: epididymal (in the visceral depot) adipocytes are richer in mitochondria than inguinal (s.c.) adipocytes.10 In addition, mitochondria play a key role in physiological processes and are involved in the pathology of many diseases.11 In compiling knowledge on mitochondria in the context of adipose tissue, we hope to stimulate thoughts in regards to the impact of mitochondrial activity in adipocyte biology, the effects of mitochondrial dysfunction/stress on adipocytes, and the subsequent alterations of systemic metabolic functions.
Mitochondria in Cell Function
Mitochondria are usually described as the “powerhouse unit” of the cell, because they contain the molecular machinery that governs many distinct metabolic pathways by which chemical energy (coming from carbohydrates, lipids, and proteins) is converted into ATP. Indeed, it is in this organelle that pyruvate oxidation, fatty acid β-oxidation, the tricarboxylic acid (TCA) cycle, and oxidative phosphorylation (OXPHOS) take place.12 The essential role of mitochondria in bioenergetic aspects of the cell is supported by the dynamics of this organelle, which is controlled by fusion and fission events.13 In addition, eukaryotic cells have the ability to initiate adaptative responses to different environmental stimuli, such as modifications in energy demands, cell growth, cell death/stress or cell differentiation, by altering the number of mitochondria (enhanced or reduced mitochondrial biogenesis), changing their morphology, or remodeling the organization and distribution of mitochondria within the cell.14
Mitochondrial Biogenesis in Adipogenesis
It is thus understandable that the “mitochondrion” (a word referring to the network and the ultrastructure of the organelle) is also dramatically affected during adipocyte differentiation. Indeed, undifferentiated adipoblasts undergo numerous and radical events, and the acquisition of the adipocyte phenotype is characterized by chronological and sequential changes in the activity of several transcription factors such as cAMP responsive element-binding protein (CREB), CCAAT/enhancer-binding protein (C/EBP) family members, and peroxisome proliferator-activated receptor γ (PPARγ), which control the expression of numerous genes encoding proteins and effectors involved in TG accumulation and other characteristics of differentiated adipocytes.15 The activity of the different transcription factors is sequentially turned on, and their transcriptional activation usually requires the participation of PPARγ coactivator 1 (PGC-1) and related proteins, major coactivators of nuclear receptors that regulate several components of energy metabolism involved in both adipogenesis and mitochondrial biogenesis.16 The fact that the transcription factors PPARγ, C/EBPα, CREB, and estrogen-related receptor α (ERRα)17 and the gene expression coactivator PGC-1α16 are induced in the control of both adipogenesis and mitochondrial biogenesis is a strong argument that supports coordination between the biogenesis of the organelle and energetic balance (Figure 1).
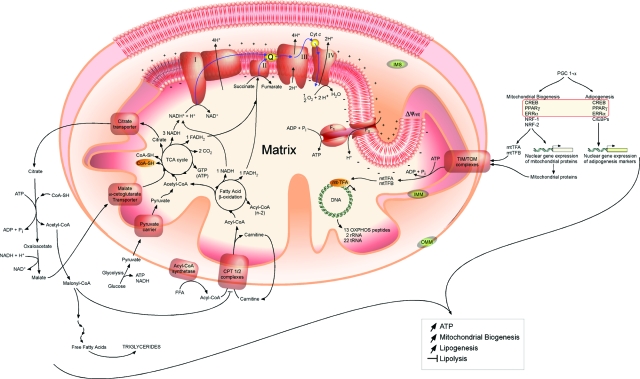
Figure 1.
Main mitochondrial functions in adipocytes. Pyruvate derived from glucose by glycolysis in the cytosol is converted, after uptake, into acetyl-CoA in the matrix. Acetyl groups pass out of the mitochondrion as citrate; in the cytosol, acetyl-CoA is released for fatty acid synthesis eventually esterified TGs. Oxaloacetate is reduced to malate, which returns to the mitochondrial matrix and is converted to oxaloacetate, a TCA cycle intermediate. Alternatively, free fatty acids are taken by the carnitine-palmitoyl-transferase-1 (CPT-1) complexes into the mitochondrial matrix and are oxidized to yield acetyl residues in the form of acetyl-CoA in a process called fatty acid β-oxidation. The acetyl groups are oxidized to CO2 via the TCA cycle. Electrons derived from oxido-reduction reactions are finally accepted by O2. The energy is retrieved as an electrochemical proton gradient used as the driving force for ATP synthesis. Besides, the coactivator PGC1-α contributes to both mitochondrial biogenesis in adipocytes and adipogenesis itself by activating specific transcription factors involved in the expression of nuclear genes encoding mitochondrial proteins and/or adipogenic markers. Both mitochondrial proteins and transcription factors such as mitochondrial transcription factors A and B (mtTFA and mtTFB) are imported into mitochondria by translocase outer membrane/translocase inner membrane (TOM/TIM) complexes: mtTFA and mtTFB being specifically involved in mtDNA replication. Increased mitochondrial biogenesis goes along with both an enhance ATP production and lipogenesis, whereas lipolysis is inhibited during adipocyte differentiation. OMM, outer mitochondrial membrane; IMS, intermembrane space; IMM, inner mitochondrial membrane.
In addition, a huge increase in the expression and/or abundance of numerous mitochondrial proteins is detectable in vitro in differentiating 3T3-L1 adipocytes within 4 days after induction of the differentiation program, and the enhanced biogenesis of the organelle is sustained up to 10 days postdifferentiation. The de novo mitochondrial biogenesis found during 3T3-L1 adipogenesis is accompanied by the remodeling of mitochondrion, ie, qualitative changes in mitochondrial composition as pyuvate carboxylase, aconitase, and enzymes involved in fatty acid metabolism, such as acyl-CoA synthetase and various forms of acyl-CoA dehydrogenase, are only expressed in adipocyte mitochondria.18 Besides, the increase in the basal rate of oxygen consumption in adipocytes compared with preadipocytes is a clear manifestation of an increased mitochondrial biogenesis during the adipogenic process.18,19,20,21,22
Moreover, mitochondrial biogenesis during adipogenesis is thought to be a necessary adjustment, because the adipocyte differentiation program requires large amount of ATP when cells become fully metabolically active. More specifically, although biogenesis of mitochondria is stimulated during the differentiation program, ATP content decreases as a negative balance between production and consumption by high ATP-consuming processes such as lipogenesis.18 Furthermore, the connection between mitochondrial biogenesis, organelle function and adipocyte differentiation is best supported by treatment of adipocytes with rosiglitazone, a potent PPARγ agonist that causes significant alterations in mitochondrial density and morphology, suggesting that nucleus-encoded mitochondrial genes may be under the control of the adipogenic transcription factor PPARγ.22
Mitochondria in Lipogenesis and Lipolysis
The mitochondria might play a critical role in lipogenesis by providing key intermediates for the synthesis of TGs. More particularly, adipocytes must generate glycerol 3-phosphate at a sufficient rate to sustain TG synthesis; this generation is covered by a glyceroneogenic pathway and mitochondrial anaplerosis.23,24 In addition, the generation of acetyl-CoA for fatty acid activation and synthesis before their esterification into TGs also requires an abundant mitochondrial population. Indeed, whereas the activation of long-chain fatty acids is shared with the endoplasmic reticulum, the mitochondrial matrix is the only place where medium-chain fatty acid activation occurs. Moreover, the outer mitochondrial membrane is also a site for phospholipid synthesis.25
Besides its role in lipogenesis, mitochondria of WAT also seem to be involved in the regulation of lipolysis. Indeed, in numerous cell types including adipocytes, fatty acids resulting from lipolysis are oxidized by the fatty acid β-oxidation cycle into the mitochondrial matrix compartment. This fatty acid oxidation constitutes an important source of energy for ATP production when energy needs increase. On the other hand, it has been long known that a decrease in intracellular ATP in white adipocytes induced by uncouplers or inhibitors of the mitochondrial respiratory chain can inhibit the lipolysis stimulated by catecholamines.26 Furthermore, lipolysis is now accepted to be a metabolic pathway that depends on the energy status of adipocytes as the activation of AMP-activated protein kinase, a central intracellular molecular sensor of energetic stress, can decrease the lipolysis stimulated by agonists of β-adrenoreceptors.27 These data sets clearly show a direct link between lipolysis and the functional state of mitochondrial OXPHOS system in white adipocytes.
Taken together, these data support the thesis that a reorganization of the mitochondrial population, its morphology, and abundance occurs during adipogenesis and is necessary to cover energy needs and lipid metabolism during the differentiation program. Consequently, because of numerous and key functions played by mitochondria during adipogenesis, impaired mitochondrial activity within preadipocytes and/or mature adipocytes could alter the physiology of WAT and thus might be reflected at the system level by affecting the molecular communication between adipocytes and other tissues such as muscle, liver, and brain.28
The Impact of Mitochondrial Dysfunction
Mitochondrial dysfunction could result in acute cellular or systemic disruption, leading to the development of pathologies. Since mitochondrial proteins are encoded by both the mitochondrial DNA (mtDNA) and the nuclear DNA, mitochondrial diseases may thus result from mutations in both nuclear and mitochondrial genomes.29 It is well established that the mitochondrial genome displays a very high mutation rate (10 to 20 times higher than nuclear genome) because of the proximity of sites of reactive oxygen species (ROS) production, a histone-free packaging of DNA in nucleoids, and a less active and lower diversity in DNA repair enzymes.30
The major tissues affected by mitochondrial dysfunction are tissues with a high energy demand such as the brain, heart, muscles, and endocrine glands.31 In the past few years, it has been shown that reduced mitochondrial density and oxidative metabolism in various tissues is an early event in the complications that are associated with obesity,32,33,34,35 a phenomenon observed in both humans and rodents. Besides mitochondrial involvement in energy state deficiency-associated diseases, the malfunction of the organelle might also play a major role in pathologies that show modifications of lipid metabolism and/or energy partitioning.
Indeed, a clear link between mitochondrial dysfunction and type I diabetes has been established; patients with mitochondrial diabetes often harbor mutations or deletions in mtDNA of pancreatic β-cells that lead to a defective insulin secretion, cell apoptosis, and eventually, a decrease in β-cell mass.36 A strong argument supporting a crucial role of mitochondrial dysfunction in T2DM in vivo is the fact that insulin resistance is often observed in elderly people with reduced OXPHOS activity as well as in obese individuals with increased risk for T2DM, which is supposed to be caused by high plasma free fatty acid concentrations.37 Indeed, in adipocytes as in skeletal muscle, mitochondrial activity impairment is usually associated with reduced fatty acid β-oxidation, leading to an increase in cytosolic free fatty acid that alters glucose uptake.28,36 Central obesity accompanied by diabetes and hypertriglyceridemia with insulin resistance are also common features found in patients with nonalcoholic steatohepatitis, who suffer from mitochondrial injury characterized by increased lipid peroxidation, alterations in the mitochondrial ultrastructure, depletion in mtDNA, and low OXPHOS activity.38
Moreover, impaired mitochondrial activity has been reported for HIV-treated patients with highly active antiretroviral therapy (HAART) leading to lipodystrophy (ectopic fat storage). These metabolic complications induced by HAART are brought together in lipodystrophy syndrome, which is associated with peripheral lipoatrophy and an increase in the amount of visceral WAT and often accompanied by glucose homeostasis abnormalities and insulin resistance.39 A similar phenotype is also observed in old age. Of interest, engineered mice carrying a proof-reading-deficient version of POLγA, the nucleus-encoded catalytic subunit of mtDNA polymerase, develop a mtDNA mutator phenotype associated with reduced lifespan and premature onset of aging-related phenotypes, such as reduced s.c. fat and increased lipid accumulation in nonlipid tissues.40
Mitochondrial Dysfunction in Preadipocytes
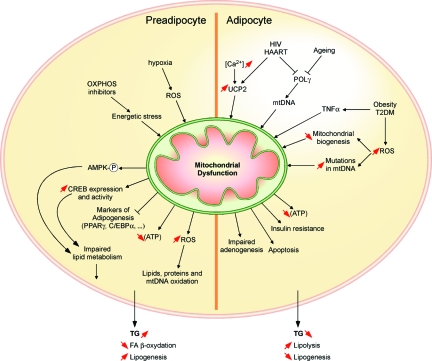
Interestingly, CREB, an ubiquitous transcription factor involved in numerous cellular functions such as cell survival, proliferation, and differentiation as well as glucose and lipid metabolism,41,42 is a gene expression regulator that is activated in response to impaired mitochondrial activity in different cell lines such as L929, 143B, and PC12 cells.43,44,45 In 3T3-L1 preadipocytes, mitochondrial OXPHOS inhibitors as well as mitochondrial protein synthesis inhibitors impair respiration, leading to TG accumulation.46 Surprisingly, mitochondrial uncouplers such as FCCP (carbonyl cyanide p-trifluoromethoxy phenylhydrazone) do not induce TG accumulation in these cells, suggesting that different signaling pathways or second messengers are activated, depending on the type of mitochondrial alterations. Although TGs accumulate in preadipocytes treated with OXPHOS inhibitors, a process that might be induced by free fatty acid (re)esterification into TGs in the cytosol of cells that display impaired mitochondrial activity, they maintain a fibroblast phenotype and do not acquire adipogenic markers46,47 (Figure 2).
Figure 2.
Comparative effects of mitochondrial dysfunction in preadipocytes and in adipocytes. In preadipocytes, mitochondrial dysfunction induced by different factors such as hypoxia or mitochondrial respiration impairment (ie, using OXPHOS inhibitors) leads to impaired lipid metabolism and/or oxidation of lipids, proteins, and mtDNA, which trigger the accumulation of TGs in the cytosol of preadipocytes, a process mediated through a decrease in fatty acid β-oxidation and an increase in lipogenesis. Conversely, in adipocytes, mitochondrial dysfunction induced by factors such as HIV, HAART, aging, obesity, or T2DM leads to a decrease in ATP production, the development of insulin resistance, apoptosis, or impairment of adipogenesis. A moderate increase in cytosolic calcium concentration ([Ca2+]) results in the stimulation of lipogenesis and exerting an inhibitory effect on lipolysis accompanied by UCP-2 overexpression. All these effects lead to a decrease in triglyceride content mediated by a stimulation of lipolysis and a decrease in lipogenesis. POLγ, polymerase γ.
In addition, a role for CREB in TG accumulation has been demonstrated in both preadipocytes submitted to mitochondrial OXPHOS inhibitors as well as in the 3T3-L1 adipogenesis process.47,48 Specifically, one CREB-target gene, glycerol-3-phosphate dehydrogenase, mitochondrial (GPDmit), has been identified in the control of TG synthesis and/or storage as GPD−/− mice display a reduction in adiposity and body weight.49 Although these studies show a response to a mitochondrial dysfunction in preadipocytes, further studies would be needed to fully address the specificity of the response to mitochondrial dysfunction.
Mitochondrial Dysfunction in Adipocyte Differentiation
During preadipocyte differentiation, the TCA cycle generates reducing equivalents such as NADH and flavin-adenine dinucleotide, which feed the mitochondrial respiratory chain, and achieves the complete oxidation of mitochondrial acetyl-CoA, a crucial metabolite generated from glucose, fatty acids, and ketogenic amino acids catabolism. Specific inhibitors of mitochondrial di- and tri-carboxylate carriers of TCA intermediates also inhibit fat accumulation in 3T3-L1 preadipocytes. Therefore, as expected, the citrate export from mitochondria is essential at an early differentiation stage for effective adipogenesis.50
Mitochondrial ROS generated by the respiratory chain, and thus indirectly associated with the status of mitochondrial activity, are at low concentrations considered as secondary messengers, playing a role in cell signaling inside and outside mitochondria.18 However, at high concentrations, ROS have been reported to exert many detrimental effects on adipoblast proliferation and differentiation.51,52 Particularly, an increase in ROS production induced by inhibitors of complex I, complex III, and F0-F1 ATP synthase (such as rotenone, antimycin A, and oligomycin, respectively) has been demonstrated to inhibit the proliferation of 3T3-L1 preadipocytes without inducing necrosis or apoptosis52 and to prevent 3T3-F442A preadipocyte differentiation.51 Moreover, 3T3-F442A preadipocytes submitted to hypoxia demonstrate a hypoxia-dependent inhibition of adipocyte differentiation mediated by hypoxia-inducible ROS generation and hypoxia-inducible factor-1α-independent CHOP10/GADD153 induction.51 In three related articles,53,54,55 it was shown that mitochondria integrate oxygen sensing, ROS production, and hypoxia-inducible factor signaling. Together, mitochondrial ROS, by modulating the number of the white preadipocyte pool and by inhibiting adipogenesis, might influence and limit the development of adipose tissue.
A large body of evidence supports the importance of the mitochondrial activity status in lipid metabolism. Consequently, it is tempting to target mitochondrial dysfunction in adipocytes to control adipose tissue function. Both in vitro and in vivo models have been developed to study how mitochondrial alterations can affect lipid metabolism in adipocytes and to determine their impact on other tissues.
Mitochondrial Dysfunction in Glucose and Lipid Metabolism
It is now well accepted that adipocytes act as integrators and regulators of food intake and energy expenditure by both endocrine and nonendocrine mechanisms.8 Adiponectin, a hormone exclusively synthesized and secreted by adipocytes, improves insulin action and sensitivity. Interestingly, in obese db/db mice, both adiponectin expression and mitochondrial content are reduced, and these effects can be reverted by rosiglitazone, a PPARγ agonist with antidiabetic action.56 In murine adipocytes, it has also been reported that the stimulation of mitochondrial biogenesis mediated by the overexpression of nuclear respiratory factor-1 also leads to enhance adiponectin synthesis. Moreover, mitochondrial dysfunction increases endoplasmic reticulum stress and reduces adiponectin transcription by a pathway depending on the activation of c-Jun-NH2-terminal kinases and of activating transcription factor-3,56 which may explain the lower plasma adiponectin concentration found in obese patients.
Experimental evidence tends to incriminate the malfunction of adipose mitochondria in obesity and T2DM. Indeed, the abundance of the mitochondrial population is lower (approximately 50% less) in white adipocytes derived from epididymal fat pads of ob/ob mice when compared with related fat cells from age-matched C57BL/6J mice.22 Moreover, several pieces of evidence link the effects of the PPARγ agonist rosiglitazone to mitochondrial modifications in white adipocytes of obese mice.22 Interestingly, rosiglitazone triggers mitochondrial biogenesis in white adipocytes from ob/ob mice, a process accompanied with remodeling of mitochondria shape and size. Furthermore, the abundance of numerous gene transcripts (about 50%) encoding mitochondrial proteins is decreased with the onset of obesity, as revealed by whole transcriptome studies on white adipocytes from ob/ob mice, whereas half of those genes were found to be up-regulated after a treatment with rosiglitazone.22 These modifications in nuclear gene expression encoding mitochondrial proteins do have a functional impact, because white adipocytes from ob/ob mice treated with rosiglitazone display enhanced oxygen consumption and increased palmitate oxidation.22
The expression of genes encoding mitochondrial proteins has also been systematically analyzed using microarray technology in adipocytes of two different mouse models for obesity and type 2 diabetes: the genetic model db/db mice and the dietary high-fat fed C57BL/6 (HFD) mice.57 The expression of genes involved in mitochondrial ATP production or energy uncoupling as well as those genes encoding mitochondrial ribosomal proteins, outer and inner membrane translocases, and mitochondrial heat-shock proteins were found to be down-regulated in HFD and db/db mice when compared with standard-fat diet-fed control and db/+ mice, respectively. The expression of nuclear receptors ERRα and PPARα is also suppressed in HFD and db/db mice. The transcription of PGC-1β58 is suppressed in the inguinal fat in both HFD and db/db mice, whereas PGC-1α was found to be only suppressed in db/db mice and not influenced by diet.57 Interestingly, as with rosiglitazone-treated ob/ob mice, half of the down-regulated genes encoding mitochondrial proteins in db/db mice could be induced by rosiglitazone treatment. This reaction was accompanied by an increase in mitochondrial mass and modifications in mitochondrial structure.57 In conclusion, mitochondrial biogenesis seems to be highly compromised in adipose tissue from HFD and db/db mice models, a process that can be improved by rosiglitazone.
Another thiazolidinedione, pioglitazone, has also been reported to stimulate mitochondrial biogenesis through PGC-1α and to increase fatty acid β-oxidation in s.c. fat cells from diabetic patients.59 The expression of PGC-1α is also reduced in the adipose tissue of morbidly human obese individuals, arguing for a role of PGC-1α in obesity.35 Finally, a major role for these coactivators in adipogenesis and biogenesis of mitochondria is supported by the fact that a deficiency of both PGC-1α and PGC-1β causes a total loss of differentiation-linked mitochondrial biogenesis and mitochondrial respiration.60
A systemic oxidative stress has been reported in both human obese individuals and diabetic obese KKAy mice. Indeed, increased ROS production has been found in adipose tissue of three mouse models of obesity: KKAy, diet-induced obesity (DIO), and db/db mice, and associated with the overexpression of NADPH oxidase and repression of antioxidative enzymes such as superoxide dismutase 2, glutathione peroxidise, and catalase.61 These observations suggest that the oxidative stress in obese individuals could be the result of stronger ROS production in the mitochondria of fat cells. Indeed, oxidative stress in murine 3T3-L1 adipocytes down-regulates the expression of PPARγ and adiponectin expression/secretion but up-regulates the expression of proinflammatory adipokines such as plasminogen activator inhibitor-1, IL-6, and monocyte chemotactic protein-1, suggesting that treatment with antioxidants or inhibitors of ROS production might restore the dysregulation of adipokine balance observed in obesity.61
Moreover, endothelial nitric oxide synthase expression is down-regulated; this process is accompanied by a slower rate of mitochondrial biogenesis in metabolically active tissues such as WAT, BAT, and muscle in three animal models of obesity: ob/ob mice, fa/fa rats, and DIO mice.62 Surprisingly, the genetic deletion of tumor necrosis factor α (TNFα) receptor-1 restored endothelial nitric oxide synthase expression and mitochondrial biogenesis and function in fat tissue of obese mice.62 Cultured white and brown adipocytes as well as muscle satellite cells of mice treated with TNFα also exhibit a reduction in endothelial nitric oxide synthase expression and mitochondrial biogenesis. Together, these data imply that TNFα inhibits endothelial nitric oxide synthase expression and impairs mitochondrial biogenesis and function in metabolically active tissues of obese rodents.62 Besides, TNFα is a proinflammatory cytokine that is highly expressed and secreted in adipose tissue from obese type 2 diabetics,63 a condition associated with decreased expression of the OXPHOS genes in visceral adipose tissues. Interestingly, TNFα treatment also resulted in down-regulation of OXPHOS gene expression in preadipocytes of healthy individuals.64 Altogether, these data suggest an important role for TNFα in impaired OXPHOS of visceral adipose tissue during the development of type 2 diabetes.
Genetic Models of Obesity Resistance
Clues to the molecular mechanisms that may lead to an increase in fat accumulation and obesity in adipocytes have been obtained with the C/EBPα-null mice.65 These mice are lean and exhibit markedly reduced fat storage in WAT and do not develop hyperlipidemia or fatty liver,65 a process associated with a specific enhancement of mitochondrial biogenesis in white fat cells.57,66
A role in energy homeostasis and adipogenesis has also been suggested for receptor-interacting protein 140, which regulates of transcriptional activity of both ligand-activated and orphan nuclear receptors.67 In 3T3-L1 adipocytes, receptor-interacting protein 140 down-regulates the expression of a cluster of genes involved in glucose uptake, glycolysis, TCA cycle, fatty acid β-oxidation, mitochondrial biogenesis, and OXPHOS.20,68 The positive action of this protein on metabolism is clearly supported by receptor-interacting protein 140-null mice, which are lean, exhibit resistance to high-fat DIO, and have glucose tolerance and relatively normal insulin sensitivity.19
The capacity of uncoupling proteins (UCPs) to regulate basal metabolic rate has provided options for obesity treatment. To determine whether enhanced energy dissipation in WAT could reduce obesity, transgenic mice have been generated in which the UCP-1 gene is controlled by the fat-specific aP2 promoter allowing increased expression in both BAT and WAT.69 These transgenic mice exhibit partial resistance to age-related obesity, induced genetically or by a high-fat diet, as reflected by a lower accumulation of TG in all fat depots, except in gonadal fat.69,70 However, ubiquitously expressed UCP-2 and muscle-expressed UCP-3 do not appear to play a major role in thermogenesis and mitochondrial uncoupling, because mice with genetic ablation of these UCP isoforms display normal response to cold, normal basal proton conductance and have normal body weight.71 Nevertheless, UCPs collectively are regarded as playing an important role in mitochondrial function, mainly through regulation of heat and/or ROS production.72
Several models of obesity resistance induced by transgenic modifications in adipose tissue or muscle exhibit the same behavior, indicating a strong systemic defense against weight loss in lean organisms. More specifically, RIIβ cAMP-dependent protein kinase (PKA) knockout mice appear healthy but have markedly diminished WAT despite normal food intake and are protected against DIO and fatty livers.73 Heterozygous PPARγ-deficient mice are protected from the development of insulin resistance under a high-fat diet because of adipocyte hypertrophy and overexpression and high secretion of leptin,74 an adipokine that controls food intake and energy expenditure and has many effects on the regulation of preadipocyte proliferation, thermogenesis, and lipolysis.74 Transgenic mice overexpressing the β1-adrenergic receptor in adipose tissue are also partially resistant to DIO because of the stimulation of lipolysis and the accumulation of brown fat cells.75 Similarly, transgenic mice that overexpress of the transcription factor FOXC2 in WAT are lean and resistant to DIO. This is due, in part, to an increased lipolysis in response to an increase in catecholamine-induced cAMP production and a lower threshold for protein kinase A activation. These processes involve both an increase in the expression of β-adrenergic receptors and a decrease in the expression of cAMP-specific phosphodiesterases.76,77
HIV Treatment-Dependent Lipodystrophy
As a key organelle in adipocyte differentiation, impairment of mitochondrial activity can explain, at least partially, adipose tissue perturbations in HAART treatment-associated lipodystrophy syndrome patients.78 Moreover, increased ROS production has been reported in adipose tissue of HAART treatment-associated lipodystrophy syndrome patients.79 Prevention of adiponectin release by chronic oxidative stress is consistent with the low adiponectin levels found in HAART treatment-associated lipodystrophy syndrome patients.78,79,80,81 Interestingly, the nucleoside and nucleotide reverse transcriptase inhibitor drugs such as stavudine and zidovudine that cause mtDNA depletion, also decrease lipid content, mitochondrial activity, and adipocyte survival in murine adipose cell types, 3T3-F442A and 3T3-L1.82 In addition, treatment of adipocytes with uridine, which averts mitochondrial dysfunction, prevents nucleoside and nucleotide reverse transcriptase inhibitor-induced impairment in adipocyte differentiation83 and improves lipodystrophy, ie, increase s.c. fat mass in lipoatrophic HIV-infected patients during unchanged HAART.84 Interestingly, toxicity of nucleoside and nucleotide reverse transcriptase inhibitor antiretroviral drugs has been reported to have opposite effects in adipose cells depending on the oxygen availability, suggesting that lipodystrophy phenotype in HAART treatment-associated lipodystrophy syndrome patients might depend on the metabolic status of the targeted adipose tissue.85
Adipocytes as Drug Targets against Obesity
The growing understanding of the relation between fat mass and different physiological and pathophysiological processes makes adipocytes a potential pharmacological drug target for treatment of obesity and diabetes.86,87,88 Possible new therapies may target proliferation and/or differentiation of preadipocytes, induction of dedifferentiation and apoptosis of adipocytes, vascularization of adipose tissue, regulation of lipid metabolism, control of adipokines release, mitochondrial energy dissipation, and the production of ROS by adipocytes.87 As this review focuses specifically on the role of mitochondrial function and dysfunction in adipocyte pathophysiology, we will limit our discussion to potential therapies that target adipocyte mitochondria (Table 1).
Table 1.
Future Potential Therapeutic Strategies to Treat Obesity by Targeting Mitochondria in White Adipocytes
| Strategies | Therapeutic target area or putative drugs | Advantages | Disadvantages | References |
|---|---|---|---|---|
| To increase energy expenditure in white adipocytes | OXPHOS uncoupling molecules (ie, FCCP, DNP, constitutive over-expression of UCP1) | Triglyceride content decreased | Insulin sensitivity impaired | 21, 91 |
| Lipolysis increased | 92, 94 | |||
| Metabolic rate increased | Fatty acid release increased | |||
| To induce a reduction of white adipocyte number | Apoptosis inducers (ie, FAT-ATTAC mouse, Ajoene) | Abundance of adipose tissue reduced | Abnormal fat accumulation (ie, muscle, liver) | 108, 110 |
| Glucose intolerance | ||||
| Insulin secretion decreased | ||||
| Circulating adipokines level decreased | ||||
| To induce white adipocyte transdifferentiation into brown-like adipocytes | Ectopic expression of PGC-1α | Lipid oxidation increased | Not known | 112,113,114,115 |
| Overexpression of leptin | ||||
| Treatment with trans-retinoic acid | Lipogenic enzymes down-regulated | |||
| Body fat decreased | ||||
| To increase mitochondrial oxidative capacity | Bioactive food components (ie, polyunsaturated fatty acid, polyphenols such as resveratrol) | Lipid oxidation increased | Not known | 117,118,119,120 |
| 122,123,124,125,126,127 | ||||
| Body fat decreased | ||||
| Mitochondrial biogenesis increased | ||||
| Synthetic mimetic directed at SIRT1 activation (ie, SRT-1720, SRT-501) | ||||
| Lifespan increased | ||||
| Insulin sensitivity improved |
Therapeutic Approaches to Treat Obesity
Mitochondrial Uncoupling and UCPs as Targets
Current therapeutic approaches for obesity predominantly aim to reduce energy intake. Two widely approved and commonly used drugs are Sibutramine, acting on satiety centers in the brain by inhibiting serotonin and noradrenaline reuptake, and Orlistat, which inhibits fat digestion in the gut by reducing the efficiency of intestinal absorption.89
However, several studies have demonstrated that any treatment for obesity other than reducing energy intake has to increase energy expenditure to elevate resting metabolic rate.90 Because mitochondria are fundamental in mediating effects of energy dissipation, the goal is to modify the uncoupling of mitochondrial OXPHOS. Strategies to dissipate energy as heat and to decrease ATP production through increased proton leak have thus been proposed.90,91
In the 1930s, the artificial uncoupler Dinitrophenol was used for this purpose, with weight losses of as much as 3 kg per week and a 40% average increase in metabolic rate.91 However, despite the significant reduction in body weight in the absence of dietary restriction, the U.S. Food and Drug Administration, due to numerous side effects observed, discontinued the use of Dinitrophenol. However, it has recently been shown that mild mitochondrial uncoupling, induced by the protonophore FCCP, is able to reduce the intracellular TG content of lipid droplets in differentiated adipocytes through a down-regulation of several energy and carbon flux requiring processes. This decrease is accompanied by an enhanced lipolysis and down-regulation of lipid synthesis as well as the significant decrease in the transcriptional activity of adipogenic transcription factors such as PPARγ and C/EBPs.92
Alternatively, uncoupling proteins have attracted attention as functional targets. These proteins are implicated in adaptative thermogenesis, fatty acid oxidation, aging, prevention of ROS formation, and body weight regulation.93 Even though UCP-1 is expressed exclusively in brown fat mitochondria and acts as thermogenic regulator, in vitro studies have demonstrated that constitutively overexpression of UCP-1 in both BAT and WAT of transgenic aP2-Ucp1 mice94 and 3T3-L1 preadipocytes during adipocyte differentiation21 induced reduced accumulation of TGs. In addition, recent studies 95,96 confirmed the presence of BAT in human adults. On the basis of these observations, these authors also present interesting data showing that cold exposition could stimulate the activity of BAT to burn a high quantity of TGs. Cool temperatures exposition might thus also be used to limit fat accumulation, but the efficiency of lower temperature seems to be highly dependent on age, gender, and leanness/obesity status.95,96
Although UCP-2 and UCP-3 appear to be mainly involved in the limitation of ROS production rather than in physiological uncoupling and thermogenesis, the expression of these proteins is controlled by numerous physiological signals, such as fatty acids, thyroid and β-adrenergetic hormones, leptin, and modulators of PPARs, suggesting an important role for these molecules in metabolism and making them new targets for pharmacological strategies.97
Transgenic mice that overexpress UCP-3 in skeletal muscle showed a decrease in adiposity, a reduction in cholesterolemia, a higher insulin sensitivity, and a lower blood glucose level accompanied by a higher metabolic rate, despite higher food intake than their wild-type counterparts.98 However, this positive effect is still debated, as it seems to be due to the artificially high levels and supraphysiological expression of UCP-3.99 Indeed, UCP-2 and UCP-3 proteins are not highly expressed in mammalian tissues. Nevertheless, it was subsequently shown that proton leak and the expression of UCP-3 (but not UCP-2) correlate with lower weight when comparing diet-resistant and diet-responsive overweight women.100
Mitochondrial uncoupling thus seems an effective way to increase resting metabolic rate, thermogenesis, and/or regulate lipid metabolism, leading to an important reduction in body weight and related syndromes. However, further research is still needed to have a full array of actions of UCPs, necessary to consider them for beneficial pharmacological targeting.
Selective Induction of Adipocyte Apoptosis
Significant alteration of adipose tissue mass is dependent on the average volume and the number of adipocytes.101 It is interesting to speculate that a decrease in TGs could be caused by a reduction in adipocyte number (a process that most likely involves the apoptosis of adipocytes) or possible adipocyte dedifferentiation.102,103,104 Because of the presence of numerous effectors of the prosurvival phosphatidylinositol 3-kinase pathway, such as very high Akt/protein kinase B expression, and/or the high abundance of the antiapoptotic factors, such as Bcl-2 and neuronal apoptosis-inhibitory protein during adipogenesis,105,106 adipocytes have a remarkable resistance to induced apoptosis.104,107 Nevertheless, targeted and moderate induction of cell death in adipocytes seems to be an attractive approach in obesity treatment, because reducing the number of adipocytes can assure an irreversible effect of fat loss. In this field, the most elegant model is the inducible “fatless” model, the FAT-ATTAC mouse, with cell fat apoptosis triggered by activation of caspase 8. This mouse that develops identically to wild-type littermates can undergo apoptosis of adipocytes at any developmental stage by administration of an FK1012 analog leading to the dimerization of a membrane-bound, adipocyte-specific caspase 8-FKBP fusion protein. The level of adipose tissue is fastly and markedly reduced within 2 weeks of dimerizer administration, but treated-FAT-ATTAC mice display near-knockout levels of circulating adipokines, are glucose-intolerant, have decreased basal and endotoxin-stimulated systemic inflammation, secrete less insulin in response to glucose compared with the wild-type, and show increased food intake independent of the effects of leptin.108
Few studies have been performed in the field of adipocyte apoptosis, but apoptotic events can be observed in vivo and in vitro. For example, in adipose tissue of patients with tumor cachexia or in preadipocytes and adipocytes treated in vitro with a high concentration of TNFα, apoptotic markers such as Bcl-2 and caspase 1 have been found.109 A study aiming at targeted adipocyte apoptosis was performed using ajoene, an organosulfur compound from garlic.110 This compound can influence the regulation of fat cell number through the induction of hydrogen peroxide generation, activation of mitogen-activated protein kinases, degradation of poly(ADP-ribose) polymerase-1, translocation of apoptosis-inducing factor, and fragmentation of DNA leading to apoptotic cell death.
Control of Fat Mass by Conversion of White Adipocytes into Brown-Like Adipocytes
Although it shares many features with WAT, BAT is specialized in adaptative thermogenesis and major differences that affect mitochondria exist between these two types of adipocytes.97 Fatty acid oxidation enzymes and respiratory chain components are highly expressed in brown adipocytes, contributing to a high oxidative capacity enhanced by the large number of mitochondria, but the most distinguishing feature is the expression of UCP-1, which allows the dissipation of the proton electrochemical gradient generated by the respiratory chain as heat.111 Molecular pathways able to modulate adaptive thermogenesis should thus provide a plausible and safe way to increase energy expenditure. Since BAT is present in rodents, hibernators, and newborns, as well as in adult humans (although in lower quantities), one alternative to attempt this goal could be to stimulate the conversion of white adipocytes into brown-like adipocytes.
Indeed, treatment of animals with all trans-retinoic acid, which targets the retinoic acid receptor, was shown to reduce obesity, to increase UCP-1 expression in WAT, and to modulate other features of WAT to BAT conversion.112 Two other recent studies have showed positive results dealing with trans-differentiation of white adipocytes.114,115 First, it was demonstrated that ectopic expression of PGC-1α in human white adipocytes induces the expression of brown adipocyte gene marker encoding UCP-1, respiratory chain proteins, and fatty acid oxidation enzymes and increases energy balance through increased utilization of fat.113,114 Second, adenovirus-induced leptin overexpression in adipocytes of normal rats induced the expression of PGC-1α, UCP1, and UCP2 and represses genes encoding lipogenic enzymes such as malonyl-CoA, acetyl-CoA carboxylase, fatty acid synthase, stearoyl-CoA desaturase 1, and glycerol-3-phosphate acyl transferase.115 In response to leptin, an activating phosphorylation of AMP-activated protein kinase that inhibits Acetyl-CoA Carboxylase leading to an increase in fatty oxidation and a rapid depletion of body fat was reported in these animals. This potential ability to transform white adipocytes into mitochondria-rich fat-burning cells has opened a novel therapeutic strategy to regulate fat mass and fight obesity.
Increase in Mitochondrial Oxidative Capacity by Bioactive Food Components
In obesity, metabolic tissues, including WAT, display reduced mitochondrial density and diminished oxidative capacity.32,33,34,35,116 Recent evidence suggests that different categories of bioactive food components, polyunsaturated fatty acids and polyphenols, have the potential to prevent and even reverse this process. Partial replacement of the plant ω-3 polyunsaturated fatty acid α linoleic acid, at an equal energy density, by the long chain marine ω-3 polyunsaturated fatty acids eicosapentaenoic acid and docosahexaenoic acid showed increased mitochondrial density, reduced WAT mass, and increased fatty acid oxidation,117 which most likely explains the mechanism behind the beneficial of these fatty acids in rodents and humans.118 Another class of bioactive food components that may function to increase mitochondrial biogenesis and oxidative capacity, also in WAT, are polyphenols. The polyphenol resveratrol can activate SIRT1, a deacetylase that has PGC-1α and a number of transcription factors involved in mitochondrial biogenesis (PPARγ, ERRα, and nuclear respiratory factor-1) as targets. Indeed, in two independent mouse studies, dietary resveratrol, compared with the same high-fat diet without resveratrol, was shown to deacetylate PGC-1α, reduce WAT mass, increase mitochondrial density, and improve mitochondrial oxidative capacity.119,120 These changes were accompanied by induction of ERRα and nuclear respiratory factor-1 and were associated with increased lifespan, improved metabolic biomarkers (insulin, glucose, and insulin growth factor-1), and improved endurance.119,120 The beneficial effect of resveratrol may be strengthened by its ability to inhibit TNFα-induced changes of plasminogen activator inhibitor-1, IL-6, and adiponectin in 3T3-L1 adipocytes.121 The protective effect of resveratrol has initiated a search for synthetic mimetics specifically directed at SIRT1 activation. Indeed, one such a mimetic, SRT1720, was able to protect against DIO as well as genetic obesity by enhancing mitochondrial oxidative capacity in metabolic tissues.122,123 Although the cellular and molecular effects of resveratrol and its mimetics were primarily examined in liver, BAT, and muscle, functional effects were seen in WAT.124 Another polyphenol with similar beneficial physiological effects, cyanidin-3-O-β-d-glucoside, clearly modulated WAT, affecting AMP-activated protein kinase phosphorylation and PPAR-γ, adiponectin, plasminogen activator inhibitor-1, and IL-6 expression.125 Several other polyphenols were shown to beneficially affect energy metabolism, including quercetin and epigallocathechin-3-gallate.126,127 Although the effects of the different polyphenols may operate via various, partly overlapping, molecular mechanisms, they all seem to impinge on mitochondria.126,127
Conclusions
In the past decade, mitochondria have been extensively studied. Increased evidence demonstrates the major role of mitochondria in adipocyte differentiation and in adipocyte homeostasis. During adipogenesis, an enhanced mitochondrial biogenesis associated with increased mitochondrial activity covers energy needs and contributes to glucose/lipid metabolism. Furthermore, as mature adipocytes are fully metabolically active cells that require large amount of ATP to regulate the intracellular TG balance (ie, fatty acid synthesis, fatty acid β-oxidation, and lipolysis), highly active mitochondria are crucial for adipocyte function. Nutritional, pharmacological, and genetic impairments of adipose mitochondrial function lead to the dysregulation of homeostasis of this endocrinological important organ. These alterations cause a vast array of metabolic diseases such as insulin resistance, T2DM, and cardiovascular diseases.
Strategies to fight obesity and associated diseases have a large spectrum of potential targets such as regulation of lipid metabolism, mitochondrial energy dissipation, adipocyte ROS production, adipokines control, induction of dedifferentiation and apoptosis, vascularization, and inhibition of proliferation and differentiation of adipocytes. All of these mechanisms can be modulated by mitochondrial activity status. Therefore, strategies that regulate mitochondrial biogenesis and functions may have therapeutic potential for the treatment of important pathophysiological conditions related to glucose/lipid metabolism.
Acknowledgments
We thank Michel Savels for help with the figure layout and graphics.
Footnotes
Address reprint requests to Thierry Arnould, Laboratory of Biochemistry and Cell Biology, University of Namur (F.U.N.D.P.), 61 rue de Bruxelles, 5000 Namur, Belgium. E-mail: thierry.arnould@fundp.ac.be.
Supported by an “Action de Recherches Concertées” (no. 326: Gouvernement de la Communauté Française), the Fonds de la Recherche Fondamentale Collective (convention n° 2.4650.06)-Fonds National de la Recherche Scientifique, European Union Mitochondria-Food Cost Action (FA 0602), and Interuniversity Attraction Pole (Phase VI, 06/02), Belgian science policy, federal government.
A.D. and S.T. contributed equally to the work.
J.K. and T.A. are chairman and member of EU COST-ACTION (FA0602-MITO-FOOD), respectively.
A.D. is a Fonds National de la Recherche Scientifique Research Fellow and S.T. is recipient of a doctoral fellowship from the Coopération Universitaire au Développement.
References
- Smyth S, Heron A. Diabetes and obesity: the twin epidemics. Nat Med. 2006;12:75–80. doi: 10.1038/nm0106-75. [DOI] [PubMed] [Google Scholar]
- Ahima RS. Adipose tissue as an endocrine organ. Obesity. 2006;14(Suppl 5):242S–249S. doi: 10.1038/oby.2006.317. [DOI] [PubMed] [Google Scholar]
- Rossmeisl M, Barbatelli G, Flachs P, Brauner P, Zingaretti MC, Marelli M, Janovska P, Horakova M, Syrovy I, Cinti S, Kopecky J. Expression of the uncoupling protein 1 from the aP2 gene promoter stimulates mitochondrial biogenesis in unilocular adipocytes in vivo. Eur J Biochem. 2002;269:19–28. doi: 10.1046/j.0014-2956.2002.02627.x. [DOI] [PubMed] [Google Scholar]
- Seale P, Bjork B, Yang W, Kajimura S, Chin S, Kuang S, Scime A, Devarakonda S, Conroe HM, Erdjument-Bromage H, Tempst P, Rudnicki MA, Beier DR, Spiegelman BM. PRDM16 controls a brown fat/skeletal muscle switch. Nature. 2008;454:961–967. doi: 10.1038/nature07182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsumoto T, Kano K, Kondo D, Fukuda N, Iribe Y, Tanaka N, Matsubara Y, Sakuma T, Satomi A, Otaki M, Ryu J, Mugishima H. Mature adipocyte-derived dedifferentiated fat cells exhibit multilineage potential. J Cell Physiol. 2008;215:210–222. doi: 10.1002/jcp.21304. [DOI] [PubMed] [Google Scholar]
- Cinti S. Adipocyte differentiation and transdifferentiation: plasticity of the adipose organ. J Endocrinol Invest. 2002;25:823–835. doi: 10.1007/BF03344046. [DOI] [PubMed] [Google Scholar]
- Morroni M, Giordano A, Zingaretti MC, Boiani R, De Matteis R, Kahn BB, Nisoli E, Tonello C, Pisoschi C, Luchetti MM, Marelli M, Cinti S. Reversible transdifferentiation of secretory epithelial cells into adipocytes in the mammary gland. Proc Natl Acad Sci USA. 2004;101:16801–16806. doi: 10.1073/pnas.0407647101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen ED, Spiegelman BM. Adipocytes as regulators of energy balance and glucose homeostasis. Nature. 2006;444:847–853. doi: 10.1038/nature05483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregor MG, Hotamisligil GS. Thematic review series: Adipocyte Biology Adipocyte stress: the endoplasmic reticulum and metabolic disease. J Lipid Res. 2007;48:1905–1914. doi: 10.1194/jlr.R700007-JLR200. [DOI] [PubMed] [Google Scholar]
- Deveaud C, Beauvoit B, Salin B, Schaeffer J, Rigoulet M. Regional differences in oxidative capacity of rat white adipose tissue are linked to the mitochondrial content of mature adipocytes. Mol Cell Biochem. 2004;267:157–166. doi: 10.1023/b:mcbi.0000049374.52989.9b. [DOI] [PubMed] [Google Scholar]
- Duchen MR. Mitochondria in health and disease: perspectives on a new mitochondrial biology. Mol Aspects Med. 2004;25:365–451. doi: 10.1016/j.mam.2004.03.001. [DOI] [PubMed] [Google Scholar]
- Goldenthal MJ, Marin-Garcia J. Mitochondrial signaling pathways: a receiver/integrator organelle. Mol Cell Biochem. 2004;262:1–16. doi: 10.1023/b:mcbi.0000038228.85494.3b. [DOI] [PubMed] [Google Scholar]
- Detmer SA, Chan DC. Functions and dysfunctions of mitochondrial dynamics. Nat Rev Mol Cell Biol. 2007;8:870–879. doi: 10.1038/nrm2275. [DOI] [PubMed] [Google Scholar]
- Li P, Zhu Z, Lu Y, Granneman JG. Metabolic and cellular plasticity in white adipose tissue II: role of peroxisome proliferator-activated receptor α. Am J Physiol Endocrinol Metab. 2005;289:E617–E626. doi: 10.1152/ajpendo.00010.2005. [DOI] [PubMed] [Google Scholar]
- Rosen ED, Spiegelman BM. Molecular regulation of adipogenesis. Annu Rev Cell Dev Biol. 2000;16:145–171. doi: 10.1146/annurev.cellbio.16.1.145. [DOI] [PubMed] [Google Scholar]
- Spiegelman BM, Puigserver P, Wu Z. Regulation of adipogenesis and energy balance by PPARγ and PGC-1. Int J Obes Relat Metab Disord. 2000;24(Suppl 4):S8–S10. doi: 10.1038/sj.ijo.0801492. [DOI] [PubMed] [Google Scholar]
- Ijichi N, Ikeda K, Horie-Inoue K, Yagi K, Okazaki Y, Inoue S. Estrogen-related receptor α modulates the expression of adipogenesis-related genes during adipocyte differentiation. Biochem Biophys Res Commun. 2007;358:813–818. doi: 10.1016/j.bbrc.2007.04.209. [DOI] [PubMed] [Google Scholar]
- Wilson-Fritch L, Burkart A, Bell G, Mendelson K, Leszyk J, Nicoloro S, Czech M, Corvera S. Mitochondrial biogenesis and remodeling during adipogenesis and in response to the insulin sensitizer rosiglitazone. Mol Cell Biol. 2003;23:1085–1094. doi: 10.1128/MCB.23.3.1085-1094.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonardsson G, Steel JH, Christian M, Pocock V, Milligan S, Bell J, So PW, Medina-Gomez G, Vidal-Puig A, White R, Parker MG. Nuclear receptor corepressor RIP140 regulates fat accumulation. Proc Natl Acad Sci USA. 2004;101:8437–8442. doi: 10.1073/pnas.0401013101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powelka AM, Seth A, Virbasius JV, Kiskinis E, Nicoloro SM, Guilherme A, Tang X, Straubhaar J, Cherniack AD, Parker MG, Czech MP. Suppression of oxidative metabolism and mitochondrial biogenesis by the transcriptional corepressor RIP140 in mouse adipocytes. J Clin Invest. 2006;116:125–136. doi: 10.1172/JCI26040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Si Y, Palani S, Jayaraman A, Lee K. Effects of forced uncoupling protein 1 expression in 3T3-L1 cells on mitochondrial function and lipid metabolism. J Lipid Res. 2007;48:826–836. doi: 10.1194/jlr.M600343-JLR200. [DOI] [PubMed] [Google Scholar]
- Wilson-Fritch L, Nicoloro S, Chouinard M, Lazar MA, Chui PC, Leszyk J, Straubhaar J, Czech MP, Corvera S. Mitochondrial remodeling in adipose tissue associated with obesity and treatment with rosiglitazone. J Clin Invest. 2004;114:1281–1289. doi: 10.1172/JCI21752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franckhauser S, Munoz S, Pujol A, Casellas A, Riu E, Otaegui P, Su B, Bosch F. Increased fatty acid re-esterification by PEPCK overexpression in adipose tissue leads to obesity without insulin resistance. Diabetes. 2002;51:624–630. doi: 10.2337/diabetes.51.3.624. [DOI] [PubMed] [Google Scholar]
- Olswang Y, Cohen H, Papo O, Cassuto H, Croniger CM, Hakimi P, Tilghman SM, Hanson RW, Reshef L. A mutation in the peroxisome proliferator-activated receptor γ-binding site in the gene for the cytosolic form of phosphoenolpyruvate carboxykinase reduces adipose tissue size and fat content in mice. Proc Natl Acad Sci USA. 2002;99:625–630. doi: 10.1073/pnas.022616299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bremer J, Bjerve KS, Borrebaek B, Christiansen R. The glycerophosphateacyltransferases and their function in the metabolism of fatty acids. Mol Cell Biochem. 1976;12:113–125. doi: 10.1007/BF01731557. [DOI] [PubMed] [Google Scholar]
- Fassina G, Dorigo P, Gaion RM. Equilibrium between metabolic pathways producing energy: a key factor in regulating lipolysis. Pharmacol Res Commun. 1974;6:1–21. doi: 10.1016/s0031-6989(74)80010-x. [DOI] [PubMed] [Google Scholar]
- Daval M, Diot-Dupuy F, Bazin R, Hainault I, Viollet B, Vaulont S, Hajduch E, Ferre P, Foufelle F. Anti-lipolytic action of AMP-activated protein kinase in rodent adipocytes. J Biol Chem. 2005;280:25250–25257. doi: 10.1074/jbc.M414222200. [DOI] [PubMed] [Google Scholar]
- Maasen JA. Mitochondria, body fat and type 2 diabetes: what is the connection? Minerva Med. 2008;99:241–251. [PubMed] [Google Scholar]
- Wallace DC. Mitochondrial diseases in man and mouse. Science. 1999;283:1482–1488. doi: 10.1126/science.283.5407.1482. [DOI] [PubMed] [Google Scholar]
- Kujoth GC, Bradshaw PC, Haroon S, Prolla TA. The role of mitochondrial DNA mutations in mammalian aging. PLoS Genet. 2007;3:e24. doi: 10.1371/journal.pgen.0030024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan DC. Mitochondria: dynamic organelles in disease, aging, and development. Cell. 2006;125:1241–1252. doi: 10.1016/j.cell.2006.06.010. [DOI] [PubMed] [Google Scholar]
- Crunkhorn S, Dearie F, Mantzoros C, Gami H, da Silva WS, Espinoza D, Faucette R, Barry K, Bianco AC, Patti ME. Peroxisome proliferator activator receptor γ coactivator-1 expression is reduced in obesity: potential pathogenic role of saturated fatty acids and p38 mitogen-activated protein kinase activation. J Biol Chem. 2007;282:15439–15450. doi: 10.1074/jbc.M611214200. [DOI] [PubMed] [Google Scholar]
- Heilbronn LK, Gan SK, Turner N, Campbell LV, Chisholm DJ. Markers of mitochondrial biogenesis and metabolism are lower in overweight and obese insulin-resistant subjects. J Clin Endocrinol Metab. 2007;92:1467–1473. doi: 10.1210/jc.2006-2210. [DOI] [PubMed] [Google Scholar]
- Mootha VK, Lindgren CM, Eriksson KF, Subramanian A, Sihag S, Lehar J, Puigserver P, Carlsson E, Ridderstrale M, Laurila E, Houstis N, Daly MJ, Patterson N, Mesirov JP, Golub TR, Tamayo P, Spiegelman B, Lander ES, Hirschhorn JN, Altshuler D, Groop LC. PGC-1α-responsive genes involved in oxidative phosphorylation are coordinately down-regulated in human diabetes. Nat Genet. 2003;34:267–273. doi: 10.1038/ng1180. [DOI] [PubMed] [Google Scholar]
- Semple RK, Crowley VC, Sewter CP, Laudes M, Christodoulides C, Considine RV, Vidal-Puig A, O'Rahilly S. Expression of the thermogenic nuclear hormone receptor coactivator PGC-1α is reduced in the adipose tissue of morbidly obese subjects. Int J Obes Relat Metab Disord. 2004;28:176–179. doi: 10.1038/sj.ijo.0802482. [DOI] [PubMed] [Google Scholar]
- Lowell BB, Shulman GI. Mitochondrial dysfunction and type 2 diabetes. Science. 2005;307:384–387. doi: 10.1126/science.1104343. [DOI] [PubMed] [Google Scholar]
- Petersen KF, Befroy D, Dufour S, Dziura J, Ariyan C, Rothman DL, DiPietro L, Cline GW, Shulman GI. Mitochondrial dysfunction in the elderly: possible role in insulin resistance. Science. 2003;300:1140–1142. doi: 10.1126/science.1082889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pessayre D, Fromenty B, Mansouri A. Mitochondrial injury in steatohepatitis. Eur J Gastroenterol Hepatol. 2004;16:1095–1105. doi: 10.1097/00042737-200411000-00003. [DOI] [PubMed] [Google Scholar]
- Falutz J. Therapy insight: body-shape changes and metabolic complications associated with HIV and highly active antiretroviral therapy. Nat Clin Pract Endocrinol Metab. 2007;3:651–661. doi: 10.1038/ncpendmet0587. [DOI] [PubMed] [Google Scholar]
- Trifunovic A, Wredenberg A, Falkenberg M, Spelbrink JN, Rovio AT, Bruder CE, Bohlooly YM, Gidlof S, Oldfors A, Wibom R, Tornell J, Jacobs HT, Larsson NG. Premature ageing in mice expressing defective mitochondrial DNA polymerase. Nature. 2004;429:417–423. doi: 10.1038/nature02517. [DOI] [PubMed] [Google Scholar]
- Reusch JE, Klemm DJ. Inhibition of cAMP-response element-binding protein activity decreases protein kinase B/Akt expression in 3T3-L1 adipocytes and induces apoptosis. J Biol Chem. 2002;277:1426–1432. doi: 10.1074/jbc.M107923200. [DOI] [PubMed] [Google Scholar]
- Zhou XY, Shibusawa N, Naik K, Porras D, Temple K, Ou H, Kaihara K, Roe MW, Brady MJ, Wondisford FE. Insulin regulation of hepatic gluconeogenesis through phosphorylation of CREB-binding protein. Nat Med. 2004;10:633–637. doi: 10.1038/nm1050. [DOI] [PubMed] [Google Scholar]
- Arnould T, Vankoningsloo S, Renard P, Houbion A, Ninane N, Demazy C, Remacle J, Raes M. CREB activation induced by mitochondrial dysfunction is a new signaling pathway that impairs cell proliferation. EMBO J. 2002;21:53–63. doi: 10.1093/emboj/21.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beitner-Johnson D, Millhorn DE. Hypoxia induces phosphorylation of the cyclic AMP response element-binding protein by a novel signaling mechanism. J Biol Chem. 1998;273:19834–19839. doi: 10.1074/jbc.273.31.19834. [DOI] [PubMed] [Google Scholar]
- Beitner-Johnson D, Rust RT, Hsieh T, Millhorn DE. Regulation of CREB by moderate hypoxia in PC12 cells. Adv Exp Med Biol. 2000;475:143–152. doi: 10.1007/0-306-46825-5_14. [DOI] [PubMed] [Google Scholar]
- Vankoningsloo S, Piens M, Lecocq C, Gilson A, De Pauw A, Renard P, Demazy C, Houbion A, Raes M, Arnould T. Mitochondrial dysfunction induces triglyceride accumulation in 3T3-L1 cells: role of fatty acid β-oxidation and glucose. J Lipid Res. 2005;46:1133–1149. doi: 10.1194/jlr.M400464-JLR200. [DOI] [PubMed] [Google Scholar]
- Vankoningsloo S, De Pauw A, Houbion A, Tejerina S, Demazy C, de Longueville F, Bertholet V, Renard P, Remacle J, Holvoet P, Raes M, Arnould T. CREB activation induced by mitochondrial dysfunction triggers triglyceride accumulation in 3T3-L1 preadipocytes. J Cell Sci. 2006;119:1266–1282. doi: 10.1242/jcs.02848. [DOI] [PubMed] [Google Scholar]
- MacDougald OA, Lane MD. Transcriptional regulation of gene expression during adipocyte differentiation. Annu Rev Biochem. 1995;64:345–373. doi: 10.1146/annurev.bi.64.070195.002021. [DOI] [PubMed] [Google Scholar]
- Brown LJ, Koza RA, Everett C, Reitman ML, Marshall L, Fahien LA, Kozak LP, MacDonald MJ. Normal thyroid thermogenesis but reduced viability and adiposity in mice lacking the mitochondrial glycerol phosphate dehydrogenase. J Biol Chem. 2002;277:32892–32898. doi: 10.1074/jbc.M202408200. [DOI] [PubMed] [Google Scholar]
- Kajimoto K, Terada H, Baba Y, Shinohara Y. Essential role of citrate export from mitochondria at early differentiation stage of 3T3-L1 cells for their effective differentiation into fat cells, as revealed by studies using specific inhibitors of mitochondrial di- and tricarboxylate carriers. Mol Genet Metab. 2005;85:46–53. doi: 10.1016/j.ymgme.2005.01.006. [DOI] [PubMed] [Google Scholar]
- Carriere A, Carmona MC, Fernandez Y, Rigoulet M, Wenger RH, Penicaud L, Casteilla L. Mitochondrial reactive oxygen species control the transcription factor CHOP-10/GADD153 and adipocyte differentiation: a mechanism for hypoxia-dependent effect. J Biol Chem. 2004;279:40462–40469. doi: 10.1074/jbc.M407258200. [DOI] [PubMed] [Google Scholar]
- Carriere A, Fernandez Y, Rigoulet M, Penicaud L, Casteilla L. Inhibition of preadipocyte proliferation by mitochondrial reactive oxygen species. FEBS Lett. 2003;550:163–167. doi: 10.1016/s0014-5793(03)00862-7. [DOI] [PubMed] [Google Scholar]
- Brunelle JK, Bell EL, Quesada NM, Vercauteren K, Tiranti V, Zeviani M, Scarpulla RC, Chandel NS. Oxygen sensing requires mitochondrial ROS but not oxidative phosphorylation. Cell Metab. 2005;1:409–414. doi: 10.1016/j.cmet.2005.05.002. [DOI] [PubMed] [Google Scholar]
- Guzy RD, Hoyos B, Robin E, Chen H, Liu L, Mansfield KD, Simon MC, Hammerling U, Schumacker PT. Mitochondrial complex III is required for hypoxia-induced ROS production and cellular oxygen sensing. Cell Metab. 2005;1:401–408. doi: 10.1016/j.cmet.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Mansfield KD, Guzy RD, Pan Y, Young RM, Cash TP, Schumacker PT, Simon MC. Mitochondrial dysfunction resulting from loss of cytochrome c impairs cellular oxygen sensing and hypoxic HIF-α activation. Cell Metab. 2005;1:393–399. doi: 10.1016/j.cmet.2005.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh EH, Park JY, Park HS, Jeon MJ, Ryu JW, Kim M, Kim SY, Kim MS, Kim SW, Park IS, Youn JH, Lee KU. Essential role of mitochondrial function in adiponectin synthesis in adipocytes. Diabetes. 2007;56:2973–2981.. doi: 10.2337/db07-0510. [DOI] [PubMed] [Google Scholar]
- Rong JX, Qiu Y, Hansen MK, Zhu L, Zhang V, Xie M, Okamoto Y, Mattie MD, Higashiyama H, Asano S, Strum JC, Ryan TE. Adipose mitochondrial biogenesis is suppressed in db/db and high-fat diet-fed mice and improved by rosiglitazone. Diabetes. 2007;56:1751–1760. doi: 10.2337/db06-1135. [DOI] [PubMed] [Google Scholar]
- Spiegelman BM. Transcriptional control of mitochondrial energy metabolism through the PGC1 coactivators. Novartis Found Symp. 2007;287:60–63. discussion 63–69. [PubMed] [Google Scholar]
- Bogacka I, Xie H, Bray GA, Smith SR. Pioglitazone induces mitochondrial biogenesis in human subcutaneous adipose tissue in vivo. Diabetes. 2005;54:1392–1399. doi: 10.2337/diabetes.54.5.1392. [DOI] [PubMed] [Google Scholar]
- Uldry M, Yang W, St-Pierre J, Lin J, Seale P, Spiegelman BM. Complementary action of the PGC-1 coactivators in mitochondrial biogenesis and brown fat differentiation. Cell Metab. 2006;3:333–341. doi: 10.1016/j.cmet.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Furukawa S, Fujita T, Shimabukuro M, Iwaki M, Yamada Y, Nakajima Y, Nakayama O, Makishima M, Matsuda M, Shimomura I. Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest. 2004;114:1752–1761. doi: 10.1172/JCI21625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valerio A, Cardile A, Cozzi V, Bracale R, Tedesco L, Pisconti A, Palomba L, Cantoni O, Clementi E, Moncada S, Carruba MO, Nisoli E. TNF-α down-regulates eNOS expression and mitochondrial biogenesis in fat and muscle of obese rodents. J Clin Invest. 2006;116:2791–2798. doi: 10.1172/JCI28570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cawthorn WP, Sethi JK. TNF-α and adipocyte biology. FEBS Lett. 2008;582:117–131. doi: 10.1016/j.febslet.2007.11.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlman I, Forsgren M, Sjogren A, Nordstrom EA, Kaaman M, Naslund E, Attersand A, Arner P. Down-regulation of electron transport chain genes in visceral adipose tissue in type 2 diabetes independent of obesity and possibly involving tumor necrosis factor-α. Diabetes. 2006;55:1792–1799. doi: 10.2337/db05-1421. [DOI] [PubMed] [Google Scholar]
- Chen SS, Chen JF, Johnson PF, Muppala V, Lee YH. C/EBPβ, when expressed from the C/ebpα gene locus, can functionally replace C/EBPα in liver but not in adipose tissue. Mol Cell Biol. 2000;20:7292–7299. doi: 10.1128/mcb.20.19.7292-7299.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu CH, Lin WD, Huang SY, Lee YH. Effect of a C/EBP gene replacement on mitochondrial biogenesis in fat cells. Genes Dev. 2004;18:1970–1975. doi: 10.1101/gad.1213104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farooqui M, Franco PJ, Thompson J, Kagechika H, Chandraratna RA, Banaszak L, Wei LN. Effects of retinoid ligands on RIP140: molecular interaction with retinoid receptors and biological activity. Biochemistry. 2003;42:971–979. doi: 10.1021/bi020497k. [DOI] [PubMed] [Google Scholar]
- Christian M, White R, Parker MG. Metabolic regulation by the nuclear receptor corepressor RIP140. Trends Endocrinol Metab. 2006;17:243–250. doi: 10.1016/j.tem.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Kopecky J, Clarke G, Enerback S, Spiegelman B, Kozak LP. Expression of the mitochondrial uncoupling protein gene from the aP2 gene promoter prevents genetic obesity. J Clin Invest. 1995;96:2914–2923. doi: 10.1172/JCI118363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopecky J, Hodny Z, Rossmeisl M, Syrovy I, Kozak LP. Reduction of dietary obesity in aP2-Ucp transgenic mice: physiology and adipose tissue distribution. Am J Physiol. 1996;270:E768–E775. doi: 10.1152/ajpendo.1996.270.5.E768. [DOI] [PubMed] [Google Scholar]
- Arsenijevic D, Onuma H, Pecqueur C, Raimbault S, Manning BS, Miroux B, Couplan E, Alves-Guerra MC, Goubern M, Surwit R, Bouillaud F, Richard D, Collins S, Ricquier D. Disruption of the uncoupling protein-2 gene in mice reveals a role in immunity and reactive oxygen species production. Nat Genet. 2000;26:435–439. doi: 10.1038/82565. [DOI] [PubMed] [Google Scholar]
- Lee KU, Lee IK, Han J, Song DK, Kim YM, Song HS, Kim HS, Lee WJ, Koh EH, Song KH, Han SM, Kim MS, Park IS, Park JY. Effects of recombinant adenovirus-mediated uncoupling protein 2 overexpression on endothelial function and apoptosis. Circ Res. 2005;96:1200–1207. doi: 10.1161/01.RES.0000170075.73039.5b. [DOI] [PubMed] [Google Scholar]
- Cummings DE, Brandon EP, Planas JV, Motamed K, Idzerda RL, McKnight GS. Genetically lean mice result from targeted disruption of the RII β subunit of protein kinase A. Nature. 1996;382:622–626. doi: 10.1038/382622a0. [DOI] [PubMed] [Google Scholar]
- Kubota N, Terauchi Y, Miki H, Tamemoto H, Yamauchi T, Komeda K, Satoh S, Nakano R, Ishii C, Sugiyama T, Eto K, Tsubamoto Y, Okuno A, Murakami K, Sekihara H, Hasegawa G, Naito M, Toyoshima Y, Tanaka S, Shiota K, Kitamura T, Fujita T, Ezaki O, Aizawa S, Kadowaki T. PPARγ mediates high-fat diet-induced adipocyte hypertrophy and insulin resistance. Mol Cell. 1999;4:597–609. doi: 10.1016/s1097-2765(00)80210-5. [DOI] [PubMed] [Google Scholar]
- Soloveva V, Graves RA, Rasenick MM, Spiegelman BM, Ross SR. Transgenic mice overexpressing the β1-adrenergic receptor in adipose tissue are resistant to obesity. Mol Endocrinol. 1997;11:27–38. doi: 10.1210/mend.11.1.9870. [DOI] [PubMed] [Google Scholar]
- Di Gregorio GB, Westergren R, Enerback S, Lu T, Kern PA. Expression of FOXC2 in adipose and muscle and its association with whole body insulin sensitivity. Am J Physiol Endocrinol Metab. 2004;287:E799–E803. doi: 10.1152/ajpendo.00155.2004. [DOI] [PubMed] [Google Scholar]
- Gronning LM, Baillie GS, Cederberg A, Lynch MJ, Houslay MD, Enerback S, Tasken K. Reduced PDE4 expression and activity contributes to enhanced catecholamine-induced cAMP accumulation in adipocytes from FOXC2 transgenic mice. FEBS Lett. 2006;580:4126–4130. doi: 10.1016/j.febslet.2006.06.058. [DOI] [PubMed] [Google Scholar]
- Villarroya F, Domingo P, Giralt M. Lipodystrophy in HIV 1-infected patients: lessons for obesity research. Int J Obes. 2007;31:1763–1776. doi: 10.1038/sj.ijo.0803698. [DOI] [PubMed] [Google Scholar]
- Giralt M, Domingo P, Guallar JP, Rodriguez de la Concepcion ML, Alegre M, Domingo JC, Villarroya F. HIV-1 infection alters gene expression in adipose tissue, which contributes to HIV-1/HAART-associated lipodystrophy. Antivir Ther. 2006;11:729–740. [PubMed] [Google Scholar]
- El Hadri K, Glorian M, Monsempes C, Dieudonne MN, Pecquery R, Giudicelli Y, Andreani M, Dugail I, Feve B. In vitro suppression of the lipogenic pathway by the nonnucleoside reverse transcriptase inhibitor efavirenz in 3T3 and human preadipocytes or adipocytes. J Biol Chem. 2004;279:15130–15141. doi: 10.1074/jbc.M312875200. [DOI] [PubMed] [Google Scholar]
- Villarroya F, Domingo P, Giralt M. Lipodystrophy associated with highly active antiretroviral therapy for HIV infection: the adipocyte as a target of antiretroviral-induced mitochondrial toxicity. Trends Pharmacol Sci. 2005;26:88–93. doi: 10.1016/j.tips.2004.12.005. [DOI] [PubMed] [Google Scholar]
- Caron M, Auclair M, Lagathu C, Lombes A, Walker UA, Kornprobst M, Capeau J. The HIV-1 nucleoside reverse transcriptase inhibitors stavudine and zidovudine alter adipocyte functions in vitro. AIDS. 2004;18:2127–2136. doi: 10.1097/00002030-200411050-00004. [DOI] [PubMed] [Google Scholar]
- Walker UA, Auclair M, Lebrecht D, Kornprobst M, Capeau J, Caron M. Uridine abrogates the adverse effects of antiretroviral pyrimidine analogues on adipose cell functions. Antivir Ther. 2006;11:25–34. [PubMed] [Google Scholar]
- Sutinen J, Walker UA, Sevastianova K, Klinker H, Hakkinen AM, Ristola M, Yki-Jarvinen H. Uridine supplementation for the treatment of antiretroviral therapy-associated lipoatrophy: a randomized, double-blind, placebo-controlled trial. Antivir Ther. 2007;12:97–105. [PubMed] [Google Scholar]
- Yun Z, Maecker HL, Johnson RS, Giaccia AJ. Inhibition of PPARγ2 gene expression by the HIF-1-regulated gene DEC1/Stra13: a mechanism for regulation of adipogenesis by hypoxia. Dev Cell. 2002;2:331–341. doi: 10.1016/s1534-5807(02)00131-4. [DOI] [PubMed] [Google Scholar]
- Guilherme A, Virbasius JV, Puri V, Czech MP. Adipocyte dysfunctions linking obesity to insulin resistance and type 2 diabetes. Nat Rev Mol Cell Biol. 2008;9:367–377. doi: 10.1038/nrm2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nawrocki AR, Scherer PE. Keynote review: the adipocyte as a drug discovery target. Drug Discov Today. 2005;10:1219–1230. doi: 10.1016/S1359-6446(05)03569-5. [DOI] [PubMed] [Google Scholar]
- Pilch PF, Bergenhem N. Pharmacological targeting of adipocytes/fat metabolism for treatment of obesity and diabetes. Mol Pharmacol. 2006;70:779–785. doi: 10.1124/mol.106.026104. [DOI] [PubMed] [Google Scholar]
- Hvizdos KM, Markham A. Orlistat: a review of its use in the management of obesity. Drugs. 1999;58:743–760. doi: 10.2165/00003495-199958040-00015. [DOI] [PubMed] [Google Scholar]
- Clapham JC, Arch JR. Thermogenic and metabolic antiobesity drugs: rationale and opportunities. Diabetes Obes Metab. 2007;9:259–275. doi: 10.1111/j.1463-1326.2006.00608.x. [DOI] [PubMed] [Google Scholar]
- Harper JA, Dickinson K, Brand MD. Mitochondrial uncoupling as a target for drug development for the treatment of obesity. Obes Rev. 2001;2:255–265. doi: 10.1046/j.1467-789x.2001.00043.x. [DOI] [PubMed] [Google Scholar]
- Tejerina S, De Pauw A, Vankoningsloo S, Houbion A, Renard P, De Longueville F, Raes M, Arnould T. Mild mitochondrial uncoupling induces 3T3-L1 adipocyte dedifferentiation by a PPARγ-independent mechanism, whereas TNFα-induced de-differentiation is PPARγ dependent. J Cell Sci. 2009;122:145–155. doi: 10.1242/jcs.027508. [DOI] [PubMed] [Google Scholar]
- Krauss S, Zhang CY, Lowell BB. The mitochondrial uncoupling-protein homologues. Nat Rev Mol Cell Biol. 2005;6:248–261. doi: 10.1038/nrm1592. [DOI] [PubMed] [Google Scholar]
- Rossmeisl M, Syrovy I, Baumruk F, Flachs P, Janovska P, Kopecky J. Decreased fatty acid synthesis due to mitochondrial uncoupling in adipose tissue. FASEB J. 2000;14:1793–1800. doi: 10.1096/fj.99-0965com. [DOI] [PubMed] [Google Scholar]
- van Marken Lichtenbelt WD, Vanhommerig JW, Smulders NM, Drossaerts JM, Kemerink GJ, Bouvy ND, Schrauwen P, Teule GJ. Cold-activated brown adipose tissue in healthy men. N Engl J Med. 2009;360:1500–1508. doi: 10.1056/NEJMoa0808718. [DOI] [PubMed] [Google Scholar]
- Virtanen KA, Lidell ME, Orava J, Heglind M, Westergren R, Niemi T, Taittonen M, Laine J, Savisto NJ, Enerback S, Nuutila P. Functional brown adipose tissue in healthy adults. N Engl J Med. 2009;360:1518–1525. doi: 10.1056/NEJMoa0808949. [DOI] [PubMed] [Google Scholar]
- Nubel T, Ricquier D. Respiration under control of uncoupling proteins: clinical perspective. Horm Res. 2006;65:300–310. doi: 10.1159/000092847. [DOI] [PubMed] [Google Scholar]
- Clapham JC, Arch JR, Chapman H, Haynes A, Lister C, Moore GB, Piercy V, Carter SA, Lehner I, Smith SA, Beeley LJ, Godden RJ, Herrity N, Skehel M, Changani KK, Hockings PD, Reid DG, Squires SM, Hatcher J, Trail B, Latcham J, Rastan S, Harper AJ, Cadenas S, Buckingham JA, Brand MD, Abuin A. Mice overexpressing human uncoupling protein-3 in skeletal muscle are hyperphagic and lean. Nature. 2000;406:415–418. doi: 10.1038/35019082. [DOI] [PubMed] [Google Scholar]
- Cadenas S, Echtay KS, Harper JA, Jekabsons MB, Buckingham JA, Grau E, Abuin A, Chapman H, Clapham JC, Brand MD. The basal proton conductance of skeletal muscle mitochondria from transgenic mice overexpressing or lacking uncoupling protein-3. J Biol Chem. 2002;277:2773–2778. doi: 10.1074/jbc.M109736200. [DOI] [PubMed] [Google Scholar]
- Harper ME, Dent R, Monemdjou S, Bezaire V, Van Wyck L, Wells G, Kavaslar GN, Gauthier A, Tesson F, McPherson R. Decreased mitochondrial proton leak and reduced expression of uncoupling protein 3 in skeletal muscle of obese diet-resistant women. Diabetes. 2002;51:2459–2466. doi: 10.2337/diabetes.51.8.2459. [DOI] [PubMed] [Google Scholar]
- Hirsch J, Han PW. Cellularity of rat adipose tissue: effects of growth, starvation, and obesity. J Lipid Res. 1969;10:77–82. [PubMed] [Google Scholar]
- Gullicksen PS, Della-Fera MA, Baile CA. Leptin-induced adipose apoptosis: implications for body weight regulation. Apoptosis. 2003;8:327–335. doi: 10.1023/a:1024112716024. [DOI] [PubMed] [Google Scholar]
- Prins JB, O'Rahilly S. Regulation of adipose cell number in man. Clin Sci. 1997;92:3–11. doi: 10.1042/cs0920003. [DOI] [PubMed] [Google Scholar]
- Sorisky A, Magun R, Gagnon AM. Adipose cell apoptosis: death in the energy depot. Int J Obes Relat Metab Disord. 2000;24(Suppl 4):S3–S7. doi: 10.1038/sj.ijo.0801491. [DOI] [PubMed] [Google Scholar]
- Magun R, Gagnon A, Yaraghi Z, Sorisky A. Expression and regulation of neuronal apoptosis inhibitory protein during adipocyte differentiation. Diabetes. 1998;47:1948–1952. doi: 10.2337/diabetes.47.12.1948. [DOI] [PubMed] [Google Scholar]
- Xu J, Liao K. Protein kinase B/AKT 1 plays a pivotal role in insulin-like growth factor-1 receptor signaling induced 3T3-L1 adipocyte differentiation. J Biol Chem. 2004;279:35914–35922. doi: 10.1074/jbc.M402297200. [DOI] [PubMed] [Google Scholar]
- Nisoli E, Cardile A, Bulbarelli A, Tedesco L, Bracale R, Cozzi V, Morroni M, Cinti S, Valerio A, Carruba MO. White adipocytes are less prone to apoptotic stimuli than brown adipocytes in rodent. Cell Death Differ. 2006;13:2154–2156. doi: 10.1038/sj.cdd.4401956. [DOI] [PubMed] [Google Scholar]
- Pajvani UB, Trujillo ME, Combs TP, Iyengar P, Jelicks L, Roth KA, Kitsis RN, Scherer PE. Fat apoptosis through targeted activation of caspase 8: a new mouse model of inducible and reversible lipoatrophy. Nat Med. 2005;11:797–803. doi: 10.1038/nm1262. [DOI] [PubMed] [Google Scholar]
- Warne JP. Tumour necrosis factor α: a key regulator of adipose tissue mass. J Endocrinol. 2003;177:351–355. doi: 10.1677/joe.0.1770351. [DOI] [PubMed] [Google Scholar]
- Yang JY, Della-Fera MA, Nelson-Dooley C, Baile CA. Molecular mechanisms of apoptosis induced by ajoene in 3T3-L1 adipocytes. Obesity. 2006;14:388–397. doi: 10.1038/oby.2006.52. [DOI] [PubMed] [Google Scholar]
- Hansen JB, Kristiansen K. Regulatory circuits controlling white versus brown adipocyte differentiation. Biochem J. 2006;398:153–168. doi: 10.1042/BJ20060402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercader J, Ribot J, Murano I, Felipe F, Cinti S, Bonet ML, Palou A. Remodeling of white adipose tissue after retinoic acid administration in mice. Endocrinology. 2006;147:5325–5332. doi: 10.1210/en.2006-0760. [DOI] [PubMed] [Google Scholar]
- Tiraby C, Langin D. Conversion from white to brown adipocytes: a strategy for the control of fat mass? Trends Endocrinol Metab. 2003;14:439–441. doi: 10.1016/j.tem.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Tiraby C, Tavernier G, Lefort C, Larrouy D, Bouillaud F, Ricquier D, Langin D. Acquirement of brown fat cell features by human white adipocytes. J Biol Chem. 2003;278:33370–33376. doi: 10.1074/jbc.M305235200. [DOI] [PubMed] [Google Scholar]
- Orci L, Cook WS, Ravazzola M, Wang MY, Park BH, Montesano R, Unger RH. Rapid transformation of white adipocytes into fat-oxidizing machines. Proc Natl Acad Sci USA. 2004;101:2058–2063. doi: 10.1073/pnas.0308258100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keijer J, van Schothorst EM. Adipose tissue failure and mitochondria as a possible target for improvement by bioactive food components. Curr Opin Lipidol. 2008;19:4–10. doi: 10.1097/MOL.0b013e3282f39f95. [DOI] [PubMed] [Google Scholar]
- Flachs P, Horakova O, Brauner P, Rossmeisl M, Pecina P, Franssen-van Hal N, Ruzickova J, Sponarova J, Drahota Z, Vlcek C, Keijer J, Houstek J, Kopecky J. Polyunsaturated fatty acids of marine origin up-regulate mitochondrial biogenesis and induce β-oxidation in white fat. Diabetologia. 2005;48:2365–2375. doi: 10.1007/s00125-005-1944-7. [DOI] [PubMed] [Google Scholar]
- Nettleton JA, Katz R. n-3 Long-chain polyunsaturated fatty acids in type 2 diabetes: a review. J Am Diet Assoc. 2005;105:428–440. doi: 10.1016/j.jada.2004.11.029. [DOI] [PubMed] [Google Scholar]
- Baur JA, Pearson KJ, Price NL, Jamieson HA, Lerin C, Kalra A, Prabhu VV, Allard JS, Lopez-Lluch G, Lewis K, Pistell PJ, Poosala S, Becker KG, Boss O, Gwinn D, Wang M, Ramaswamy S, Fishbein KW, Spencer RG, Lakatta EG, Le Couteur D, Shaw RJ, Navas P, Puigserver P, Ingram DK, de Cabo R, Sinclair DA. Resveratrol improves health and survival of mice on a high-calorie diet. Nature. 2006;444:337–342. doi: 10.1038/nature05354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagouge M, Argmann C, Gerhart-Hines Z, Meziane H, Lerin C, Daussin F, Messadeq N, Milne J, Lambert P, Elliott P, Geny B, Laakso M, Puigserver P, Auwerx J. Resveratrol improves mitochondrial function and protects against metabolic disease by activating SIRT1 and PGC-1α. Cell. 2006;127:1109–1122. doi: 10.1016/j.cell.2006.11.013. [DOI] [PubMed] [Google Scholar]
- Ahn J, Lee H, Kim S, Ha T. Resveratrol inhibits TNF-α-induced changes of adipokines in 3T3-L1 adipocytes. Biochem Biophys Res Commun. 2007;364:972–977. doi: 10.1016/j.bbrc.2007.10.109. [DOI] [PubMed] [Google Scholar]
- Feige JN, Lagouge M, Canto C, Strehle A, Houten SM, Milne JC, Lambert PD, Mataki C, Elliott PJ, Auwerx J. Specific SIRT1 activation mimics low energy levels and protects against diet-induced metabolic disorders by enhancing fat oxidation. Cell Metab. 2008;8:347–358. doi: 10.1016/j.cmet.2008.08.017. [DOI] [PubMed] [Google Scholar]
- Milne JC, Lambert PD, Schenk S, Carney DP, Smith JJ, Gagne DJ, Jin L, Boss O, Perni RB, Vu CB, Bemis JE, Xie R, Disch JS, Ng PY, Nunes JJ, Lynch AV, Yang H, Galonek H, Israelian K, Choy W, Iffland A, Lavu S, Medvedik O, Sinclair DA, Olefsky JM, Jirousek MR, Elliott PJ, Westphal CH. Small molecule activators of SIRT1 as therapeutics for the treatment of type 2 diabetes. Nature. 2007;450:712–716. doi: 10.1038/nature06261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott PJ, Jirousek M. Sirtuins: novel targets for metabolic disease. Curr Opin Investig Drugs. 2008;9:371–378. [PubMed] [Google Scholar]
- Tsuda T. Regulation of adipocyte function by anthocyanins: possibility of preventing the metabolic syndrome. J Agric Food Chem. 2008;56:642–646. doi: 10.1021/jf073113b. [DOI] [PubMed] [Google Scholar]
- Boschmann M, Thielecke F. The effects of epigallocatechin-3-gallate on thermogenesis and fat oxidation in obese men: a pilot study. J Am Coll Nutr. 2007;26:389S–395S. doi: 10.1080/07315724.2007.10719627. [DOI] [PubMed] [Google Scholar]
- de Boer VC, van Schothorst EM, Dihal AA, van der Woude H, Arts IC, Rietjens IM, Hollman PC, Keijer J. Chronic quercetin exposure affects fatty acid catabolism in rat lung. Cell Mol Life Sci. 2006;63:2847–2858. doi: 10.1007/s00018-006-6316-z. [DOI] [PMC free article] [PubMed] [Google Scholar]