Abstract
Multicentric Castleman disease (MCD) is a rare lymphoproliferative disorder. Although MCD pathogenesis is unclear, studies have suggested that human herpesvirus 8 (HHV-8) may be associated with the disorder. Recent reports have identified MCD cases without viral infection. A 43-year-old woman presented to our hospital for fever and myalgia of 6 months' duration. The complete blood count revealed an elevated leukocyte count (15.1×103/µL) and a decreased hemoglobin level of 10.0 g/dL. The C-reactive protein level was elevated at 276.5 mg/L. Thoracic computed tomography (CT) scans revealed bilateral axillary lymphadenopathy. There was no evidence of HHV-8, human immunodeficiency virus (HIV), or Mycobacterium infection. Histologic evaluation of a lymph node biopsy from the left axilla yielded a diagnosis of MCD. Cyclophosphamide, adriamycin, vincristine, and prednisone (CHOP) were administered for a total of 4 cycles. The patient's fever and lymphadenopathy resolved after the course of chemotherapy. She has been in complete remission for 24 months at this writing. As previously reported, this case report suggests that MCD can develop without viral infection. CHOP chemotherapy may be an effective treatment option for newly diagnosed MCD patients.
Keywords: Chemotherapy, Human herpes virus 8, Multicentric Castleman disease
Introduction
Castleman disease (CD) is a rare lymphoproliferative disorder diagnosed by clinical, histopathologic, and laboratory criteria. The disease was first described as a pathologic entity in 1954 and was defined in 1956 (1). The two primary clinical presentations are unicentric (UCD) and multicentric CD (MCD). The disease is confined to a single lymph node with UCD, while MCD typically presents with lymphoid hyperplasia at multiple sites, including the peripheral lymph nodes, bone marrow, and multiple organs. Pathology is associated with systemic signs and constitutional symptoms. CD is classified into three histological subtypes: 1) hyaline-vascular CD, 2) plasma cell CD, and 3) mixed variant CD. Hyaline-vascular CD is characterized by numerous germinal follicles in the lymph nodes with thick-walled blood vessels and a concentrically expanded follicular mantle zone. These result in a characteristic onion peel appearance. Plasma cell CD is characterized by large, hyperplastic follicles with intervening sheets of plasma cells (2), and results in fever, sweats, fatigue, anemia, polyclonal hypergammaglobulinemia, and bone marrow plasmacytosis. Hyaline-vascular CD is identified in approximately 90% of patients with unicentric CD (3). Conversely, most MCD cases are of the plasma cell predominance type. Mixed CD forms also exist with both hyaline-vascular and plasma cell elements.
Immunologic pathogenic processes have been implicated in MCD, and viral infections may be involved in disease pathogenesis. Recent reports have identified CD cases without viral infection (4,5). This case report describes a multicentric Castleman disease patient without HHV-8 and HIV infection. The patient was successfully treated with combined chemotherapy.
Case Report
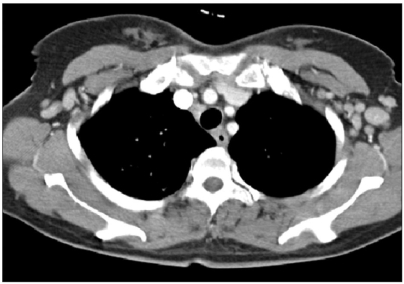
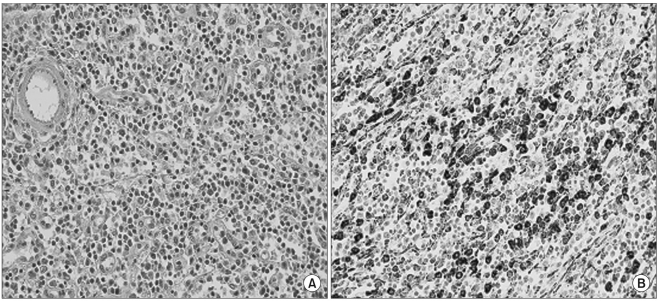
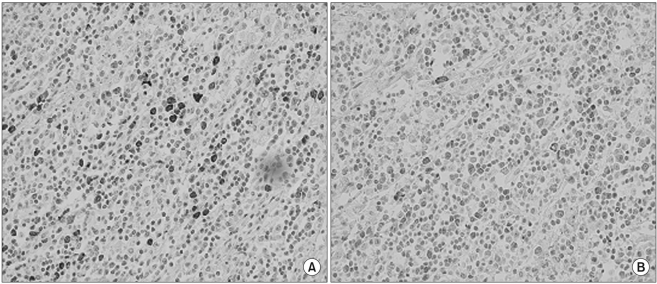
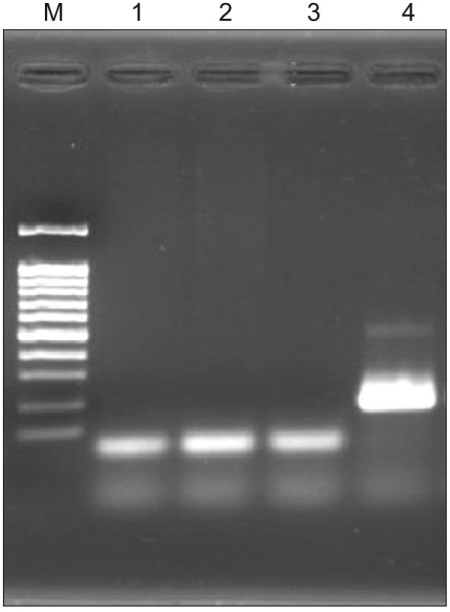
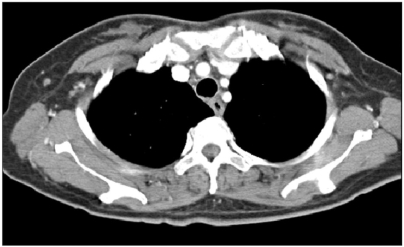
A 43-year-old female patient presented to our hospital in January 2005 for evaluation of 6 months' duration of fever (38℃) and myalgia. The complete blood count revealed an elevated leukocyte count of 15.1×103/µL (85.4% neutrophils and 7.7% lymphocytes), a decreased hemoglobin level (of 10.0 g/dL), and a platelet count of 395×103/µL. The C-reactive protein level was elevated at 276.5 mg/L (normal value <6 mg/L). Chest CT scan revealed bilateral axillary lymphadenopathy (Fig. 1). Concentrated urine protein electrophoresis revealed polyclonal hypergammaglobuminemia (15.8 mg/dL). Plasma cell MCD was diagnosed by histologic evaluation of a left axillary lymph node biopsy (Fig. 2, 3). There was no evidence of bone marrow involvement. The patient tested negative for HHV-8, HIV, Mycoplasma, Salmonella, Legionella, and Mycobacterium infections (Fig. 4). CHOP chemotherapy consisted of intravenous (IV) cyclophosphamide (750 mg/m2 on day 1), IV adriamycin (50 mg/m2 on day 1), IV vincristine (1.4 mg/m2 on day 1), and oral prednisone (100 mg for 5 days) was administered every 3 weeks for 4 cycles. The patient's fever subsided and her lymphadenopathy resolved after the initial course of treatment (Fig. 5). At this writing, the patient has been in complete remission for 24 months.
Fig. 1.
Chest CT scan on admission revealed bilateral axillary lymphadenopathy.
Fig. 2.
Left axillary lymph node biopsy. (A) Heavy infiltration of plasma cells and occasional eosinophils in the medullary cords and interfollicular areas (H & E, ×400). (B) Plasma cells were strongly reactive for Vs38, and some cells were large and multinucleated (Vs38 Immunohistochemical stain, ×400).
Fig. 3.
Left axillary lymph node biopsy. (A) Lambda immunohistochemical stain, ×400. (B) Kappa immunohistochemical stain, ×400. Plasma cells were polyclonal and both lambda and kappa positive.
Fig. 4.
HHV-8 nested polymerase chain reaction. Lane M=100 bp ladder, Lane 1=blood, Lane 2=tissue, Lane 3=distilled water (negative control), Lane 4=BCBL-1 (positive control). HHV-8, human herpesvirus 8.
Fig. 5.
Chest CT scan after treatment with resolution of bilateral axillary lymphadenopathy.
Discussion
Multicentric CD was clinico-pathologically defined in 1983 (6). CD is a lymphoproliferative disorder characterized by both systemic lymphadenopathy and polyclonal hypergammaglobulinemia with possible constitutional symptoms. However, the etiology of CD is poorly understood. Various immunopathologic processes have been suggested and the best therapeutic options are not well-established.
HHV-8 is a gamma herpesvirus that was initially identified in Kaposi sarcoma patients. It is frequently present in acquired immunodeficiency syndrome (AIDS)-associated Kaposi sarcoma (7). HHV-8 DNA is frequently detected in the peripheral blood of HIV-positive patients with MCD (8). However, HHV-8 DNA is detected in 41% of HIV-negative MCD patients, and HHV-8 is associated with MCD etiology. HHV-8 has a viral homologue of human interleukin (IL)-6 in its genomic DNA, and this has been suggested that HHV-8 infection may be related to excessive IL-6 production. IL-6 overproduction in HHV-8-infected lymphocytes has been postulated as a pathogenic MCD cause. Increased serum IL-6 was reported in many MCD patients, and IL-6 may have linked plasma cell proliferation and vessels in CD (9). There are multiple etiologies for the promotion of IL-6 overproduction. In addition, increases in cytokines including IL-1 and tumor necrosis factor (TNF)-β are possibly associated with CD. Vascular endothelial growth factor (VEGF) levels in the sera and supernatants of cultured lymph nodes from CD patients were higher than in normal controls (10). This suggested that VEGF may be involved in CD pathogenesis. The immune stimulus for HHV-8 negative MCD is not established.
The standard treatment option for CD remains uncertain. However, treatment options include surgical excision, cytoreductive chemotherapy, and radiation therapy. Patients with unicentric disease can be cured by surgery, although radiotherapy is another option for poor surgical candidates. MCD patients must undergo comprehensive laboratory testing, including a complete blood count, C-reactive protein levels, liver function tests, anti-nuclear antibody titers, rheumatoid factor levels, HIV screening, IL-6 levels, HHV-8 testing, and CD20 levels. Several antiviral medications (ganciclovir, valganciclovir, foscarnet, and cidofovir) have resulted in mixed responses for the inhibition of HHV-8 replication in HHV-8-associated MCD patients (11). Recent reports have suggested that rituximab may serve as an option for CD20-expressing MCD patients (4,12). Rituximab is a monoclonal antibody against CD20, and is primarily used to treat non-Hodgkins lymphoma patients. Other immune modulator treatment modalities include steroids, interferon-α, all-trans retinoic acid, and thalidomide, none of which have resulted in consistent disease control (13). Chemotherapy is the first treatment option in most progressive or symptomatic patients. Both single and multiple agent combination chemotherapy have been effectively used in MCD treatment. Chlorambucil, cyclophosphamide, vinblastine, and etoposide have demonstrated efficacy and are well-tolerated in some patient (14,15). Cytoreductive combination chemotherapies, including CHOP or CVP (cyclophosphamide, vincristine, and prednisone), have been effectively used in immunocompetent non-Hodgkins lymphoma patients (14). These may be suitable for MCD patients. These treatments may be associated with marked toxicity in HIV-positive patients, so patients must be carefully selected and closely monitored for infection.
In conclusion, our case suggests that MCD can develop without evidence of a viral infection. CHOP chemotherapy may be an effective first-line therapy for newly diagnosed MCD patients.
References
- 1.Castleman B, Iverson L, Menendez VP. Localized mediastinal lymphnode hyperplasia re sembling thymoma. Cancer. 1956;9:822–830. doi: 10.1002/1097-0142(195607/08)9:4<822::aid-cncr2820090430>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 2.Ruco LP, Gearing AJ, Pigott R, Pomponi D, Burgio VL, Cafolla A, et al. Expression of ICAM-1, VCAM-1 and ELAM-1 in angiofollicular lymph node hyperplasia (Castleman's disease): evidence for dysplasia of follicular dendritic reticulum cells. Histopathology. 1991;19:523–528. doi: 10.1111/j.1365-2559.1991.tb01500.x. [DOI] [PubMed] [Google Scholar]
- 3.Keller AR, Hochholzer L, Castleman B. Hyaline-vascular and plasma-cell types of giant lymph node hyperplasia of the mediastinum and other locations. Cancer. 1972;29:670–683. doi: 10.1002/1097-0142(197203)29:3<670::aid-cncr2820290321>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 4.Gholam D, Vantelon JM, Al-Jijakli A, Bourhis JH. A case of multicentric Castleman's disease associated with advanced systemic amyloidosis treated with chemotherapy and anti-CD20 monoclonal antibody. Ann Hematol. 2003;82:766–768. doi: 10.1007/s00277-003-0718-x. [DOI] [PubMed] [Google Scholar]
- 5.Ide M, Kawachi Y, Izumi Y, Kasagi K, Ogino T. Long-term remission in HIV-negative patients with multicentric Castleman's disease using rituximab. Eur J Haematol. 2006;76:119–123. doi: 10.1111/j.1600-0609.2005.00570.x. [DOI] [PubMed] [Google Scholar]
- 6.Frizzera G, Banks PM, Massarelli G, Rosai J. A systemic lymphoproliferative disorder with morphologic features of Castleman's disease. Pathological findings in 15 patients. Am J Surg Pathol. 1983;7:211–231. doi: 10.1097/00000478-198304000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Chang Y, Cesarman E, Pessin MS, Lee F, Culpepper J, Knowles DM, et al. Identification of herpesvirus-like DNA sequences in AIDS-associated Kaposi's sarcoma. Science. 1994;266:1865–1869. doi: 10.1126/science.7997879. [DOI] [PubMed] [Google Scholar]
- 8.Soulier J, Grollet L, Oksenhendler E, Cacoub P, Cazals-Hatem D, Babinet P, et al. Kaposi's sarcoma-associated herpesvirus-like DNA sequences in multicentric Castleman's disease. Blood. 1995;86:1276–1280. [PubMed] [Google Scholar]
- 9.Aoki Y, Jaffe ES, Chang Y, Jones K, Teruya-Feldstein J, Moore PS, et al. Angiogenesis and hematopoiesis induced by Kaposi's sarcoma-associated herpesvirus-encoded interleukin-6. Blood. 1999;93:4034–4043. [PubMed] [Google Scholar]
- 10.Nishi J, Maruyama I. Increased expression of vascular endothelial growth factor (VEGF) in Castleman's disease: proposed pathomechanism of vascular proliferation in the affected lymph node. Leuk Lymphoma. 2000;38:387–394. doi: 10.3109/10428190009087030. [DOI] [PubMed] [Google Scholar]
- 11.Berezne A, Agbalika F, Oksenhendler E. Failure of cidofovir in HIV-associated multicentric Castleman disease. Blood. 2004;103:4368–4369. doi: 10.1182/blood-2004-01-0158. [DOI] [PubMed] [Google Scholar]
- 12.Marcelin AG, Aaron L, Mateus C, Gyan E, Gorin I, Viard JP, et al. Rituximab therapy for HIV-associated Castleman disease. Blood. 2003;102:2786–2788. doi: 10.1182/blood-2003-03-0951. [DOI] [PubMed] [Google Scholar]
- 13.Rieu P, Droz D, Gessain A, Grunfeld JP, Hermine O. Retinoic acid for treatment of multicentric Castleman's disease. Lancet. 1999;354:1262–1263. doi: 10.1016/S0140-6736(99)03957-4. [DOI] [PubMed] [Google Scholar]
- 14.Frizzera G, Peterson BA, Bayrd ED, Goldman A. A systemic lymphoproliferative disorder with morphologic features of Castleman's disease: clinical findings and clinicopathologic correlations in 15 patients. J Clin Oncol. 1985;3:1202–1216. doi: 10.1200/JCO.1985.3.9.1202. [DOI] [PubMed] [Google Scholar]
- 15.Scott D, Cabral L, Harrington WJ., Jr Treatment of HIV-associated multicentric Castleman's disease with oral etoposide. Am J Hematol. 2001;66:148–150. doi: 10.1002/1096-8652(200102)66:2<148::AID-AJH1034>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]