Abstract
Although hepatocellular carcinoma (HCC) is a common tumor, direct invasion of the gastrointestinal tract by HCC is uncommon. Recently, we encountered two cases of HCC with direct invasion to the colon. The first patient was a 79-year-old man who underwent transarterial chemo-embolization (TACE) for HCC 1.5 years prior to admission to our hospital. Computed tomography (CT) showed a 7.5-cm liver tumor directly invading the transverse colon. Partial resection of the liver and transverse colon was performed. The patient survived 6 mo after surgery, but died of recurrent HCC. The second patient was a 69-year-old man who underwent TACE and ablation for HCC 2 years and 7 months prior to being admitted to our hospital for melena and abdominal distension. CT revealed a 6-cm liver tumor with direct invasion to the colon. The patient underwent partial resection of the liver and right hemicolectomy. The patient recovered from the surgery. But, unfortunately, he died of liver failure due to liver cirrhosis one month later. Although the prognosis of HCC that has invaded the colon is generally poor due to the advanced stage of the disease, surgical resection may be a favorable treatment option in patients with a good general condition.
Keywords: Hepatocellular carcinoma, Colon, Hepatoma
INTRODUCTION
Hepatocellular carcinoma (HCC) is one of the most common tumors worldwide[1]. Direct invasion to the gastrointestinal (GI) tract by HCC is uncommon, with a reported incidence of 0.5%-2% among clinical HCC cases[2,3]. GI bleeding or stenosis due to HCC invasion is very uncommon. In such cases, the best treatment remains controversial[4].
Due to improved instruments, techniques, and perioperative management, surgical resection is now safely performed in patients with advanced HCC. Therefore, it is also possible to resect HCC with direct invasion to the GI tract. Here, we present two cases of HCC with direct invasion to the colon that were treated by surgical resection.
CASE REPORT
Case 1
A 79-year-old man with chronic hepatitis C has been followed up since 1983. In August 1998, computed tomography (CT) revealed a 4-cm tumor in the caudate lobe of the liver, which was diagnosed as HCC. The lesion was treated by transarterial chemo-embolization (TACE). In February 2000, the patient suffered from epigastralgia, and was admitted to our hospital. CT revealed that the liver tumor increased to 7.5 cm in diameter and directly invaded the transverse colon (Figure 1). Liver function tests revealed no abnormalities. The serum α-fetoprotein (AFP) level was 331 ng/mL, and the protein induced by vitamin K absence or antagonist 2 (PIVKA-2) level was within normal range. HCC invading the transverse colon was diagnosed and partial resection of the liver and transverse colon was performed. In the resected specimen, a 96 mm × 58 mm liver tumor invading the transverse colon was found (Figure 2). Histopathologic examination of the specimen also showed poorly-differentiated HCC with direct invasion to the colon. The postoperative course was uneventful, and the patient was discharged on postoperative day 21. He survived symptom free for 6 mo and died of recurrent HCC.
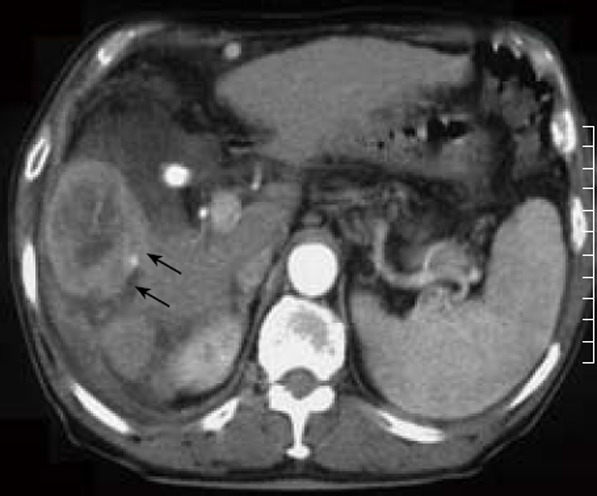
Figure 1.

Computed tomography images showing a 7.5-cm liver tumor (arrows) arising from the caudate lobe in case 1(A), which appears to invade the transverse colon directly (arrows) (B).
Figure 2.

Macroscopic appearance of the surgical specimen in case 1. The liver tumor invades the colon (arrows).
Case 2
A 69-year-old man has been treated since 2000 for liver cirrhosis due to hepatitis C. In July 2004, CT revealed a 4-cm tumor in segment 6 of the liver, which was diagnosed as HCC. The lesion was treated by radiofrequency ablation (RFA) and TACE. In February 2007, the patient suffered from melena and abdominal distension and was admitted to our hospital. CT revealed that the tumor increased to 6 cm in diameter and directly invaded the diaphragm and the hepatic flexure of the colon (Figure 3). The ascending colon was dilated due to stenosis of the colon. Colonoscopic examination revealed a hemorrhagic and lobulated tumor in the hepatic flexure of the colon (Figure 4). Laboratory tests revealed 2.9 g/dL serum albumin, 1.9 mg/dL serum total bilirubin, 52.1% prothrombin activity, and 17.3% indocyanine green retention rate at 15 minutes, 15 ng/mL serum AFP, and 370 AU/mL PIVKA-2. HCC invading the hepatic flexure of the colon was diagnosed, and partial resection of the liver, right hemicolectomy and partial excision of the diaphragm were performed. In the resected specimen, a 65 mm × 47 mm liver tumor, which invaded the hepatic flexure of the colon, was found (Figure 5). Histopathologic examination of the specimen also showed moderately differentiated HCC with direct invasion to the colon and diaphragm. The patient recovered from the operation, and had no evidence of HCC recurrence, but unfortunately, he died of liver failure due to liver cirrhosis 1 mo later.
Figure 3.
Computed tomography images showing a 6-cm liver tumor invades the colon and diaphragm (arrows) in case 2.
Figure 4.
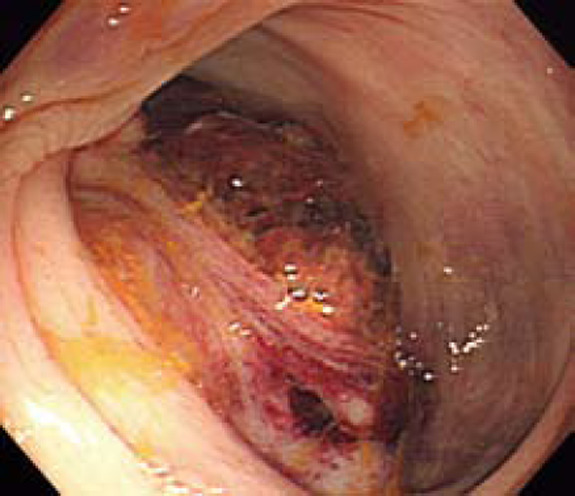
Colonoscopic view showing a hemorrhagic and lobulated tumor with a smooth surface is seen in the ascending colon in case 2.
Figure 5.
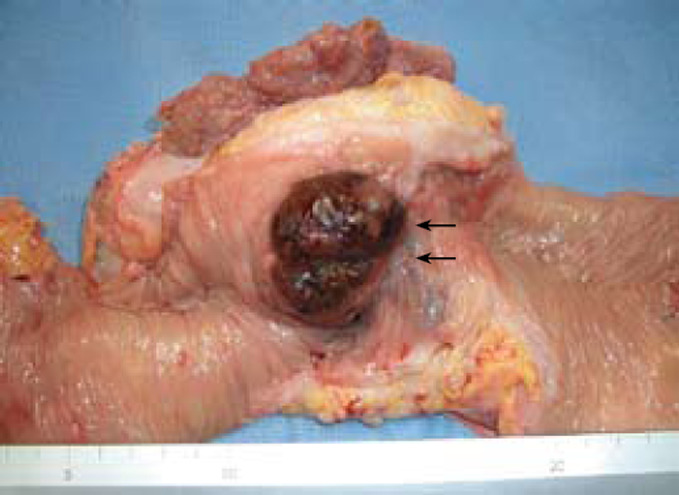
Macroscopic appearance of the surgical specimen in case 2. The liver tumor invades the colon (arrows).
DISCUSSION
HCC, one of the most common malignant tumors worldwide, is responsible for more than 250 000 deaths annually[1]. In some autopsy series, extrahepatic metastasis to the lung, lymphnodes, bone, heart, or adrenal glands has been found in 30%-75% of advanced HCC cases[5]. HCC with direct invasion to other organs can occur, with the most frequent sites being the diaphragm and gallbladder[6]. HCC only rarely invades the GI tract, the reported incidence is 0.5%-2% of clinical HCC cases and 4% of autopsy cases[2,3,7]. GI bleeding or stenosis due to HCC invasion is very uncommon[8]. The most frequently invaded GI tract sites are the duodenum and stomach[2] and invasion into the colon is very rare. To date, only eight cases of invasion to the colon by HCC have been reported in the English literature (Table 1)[2,3,9–11]. Among the 10 patients (including our two cases), the most frequent symptom was bloody stool (8 of 10 patients, 80%). Seven patients (70%) underwent transarterial embolization (TAE) or TACE for HCC prior to development of invasion. Surgical resection or supportive care was almost selected in almost all cases. However, the outcomes were very poor, and the median survival was only 2.5 mo.
Table 1.
Reported cases with invasion to the colon by HCC
| Authors | Age (yr)/Sex | Viral infection | Symptom | Endoscopic shape | Tumor size (mm) | Previous treatment for HCC | Treatment | Prognosis |
| Hashimoto M[8] (1996) | 72/F | HCV | Melena | Ulcerated | 45 | TAE (7 times) | Operation | 4 mo alive |
| Chen CY[9] (1997) | 71/M | Negative | Bloody stool | Lobulated | 200 | - | - | 6 mo dead |
| Lin CP[2] (2000) | 59/M | HCV | Bloody stool | Polypoid | 80 | TAE (3 times) | - | 1.2 mo dead |
| Lin CP[2] (2000) | 67/M | HBV | Stool OB (+) | Not observed | 150 | Operation TAE | - | 1.5 mo dead |
| Lin CP[2] (2000) | 69/M | HBV | Stool OB (+) | Not observed | 200 | - | - | 1.2 mo dead |
| Lin CP[2] (2000) | 63/M | Negative | Bloody stool | Not observed | 200 | - | - | 4.0 mo dead |
| Strivastava DN[10] (2000) | 32/M | HBV | Bloody stool | Not observed | n.d. | TAE | TAE | 0.7 mo dead |
| Zech CJ[11] (2006) | 57/M | HBV HCV | Abdominal pain | Not observed | n.d. | TACE (6 times) | Operation | ND |
| Our case | 79/M | HCV | Epigastralgia | Not observed | 75 | TACE | Operation | 6.0 mo dead |
| Our case | 69/M | HCV | Melena | Lobulated | 55 | RFA TACE | Operation | 1.0 mo dead |
HBV: Hepatitis B virus; HCV: Hepatitis C virus; Stool OB (+): Stool positive for occult blood; TAE: Transarterial embolization; TACE: Transarterial chemoembolization; ND: Not described.
GI tract invasion by HCC sometimes occurs after TAE or TACE[8]. TAE and TACE can induce exophytic growth of the HCC due to an inflammatory reaction and change in the extrahepatic blood supply. As a result, HCC may invade adjacent organs such as the diaphragm, stomach, duodenum, and colon.
TAE or TACE is not an effective treatment for GI invasion by HCC. RFA is difficult to perform in patients with GI tract invasion because of the risk of GI tract perforation. Fujii et al[12] reported that the median survival time of patients with GI tract invasion treated by surgical resection, nonsurgically, or by supportive therapies is 9.7 mo, 3.0 mo and 1.2 mo, respectively. Therefore, surgical resection may be the most effective treatment for GI tract invasion by HCC. In addition, surgical techniques including liver resection and perioperative management have recently improved. Surgical resection is probably the best treatment option for HCC invading the GI tract if the patient’s general condition including liver function is good.
In conclusion, although the prognosis of colonic invasion of HCC is generally poor due to the advanced stage of the disease, surgical resection may be a favorable treatment option in patients with a good general condition.
Peer reviewer: Fritz von Weizsäcker, Professor, Department of Medicine Schlosspark-Klinik, Humboldt University, Heubnerweg 2, Berlin D-14059, Germany
S- Editor Zhong XY L- Editor Wang XL E- Editor Zhang WB
References
- 1.Ramsey WH, Wu GY. Hepatocellular carcinoma: update on diagnosis and treatment. Dig Dis. 1995;13:81–91. doi: 10.1159/000171490. [DOI] [PubMed] [Google Scholar]
- 2.Lin CP, Cheng JS, Lai KH, Lo GH, Hsu PI, Chan HH, Hsu JH, Wang YY, Pan HB, Tseng HH. Gastrointestinal metastasis in hepatocellular carcinoma: radiological and endoscopic studies of 11 cases. J Gastroenterol Hepatol. 2000;15:536–541. doi: 10.1046/j.1440-1746.2000.02152.x. [DOI] [PubMed] [Google Scholar]
- 3.Chen LT, Chen CY, Jan CM, Wang WM, Lan TS, Hsieh MY, Liu GC. Gastrointestinal tract involvement in hepatocellular carcinoma: clinical, radiological and endoscopic studies. Endoscopy. 1990;22:118–123. doi: 10.1055/s-2007-1012815. [DOI] [PubMed] [Google Scholar]
- 4.Tung WY, Chau GY, Loong CC, Wu JC, Tsay SH, King KL, Huang SM, Chiu JH, Wu CW, Lui WY. Surgical resection of primary hepatocellular carcinoma extending to adjacent organ(s) Eur J Surg Oncol. 1996;22:516–520. doi: 10.1016/s0748-7983(96)93056-5. [DOI] [PubMed] [Google Scholar]
- 5.Anthony PP. Primary carcinoma of the liver: a study of 282 cases in Ugandan Africans. J Pathol. 1973;110:37–48. doi: 10.1002/path.1711100105. [DOI] [PubMed] [Google Scholar]
- 6.Edmondson HA, Steiner PE. Primary carcinoma of the liver: a study of 100 cases among 48,900 necropsies. Cancer. 1954;7:462–503. doi: 10.1002/1097-0142(195405)7:3<462::aid-cncr2820070308>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 7.Nakashima T, Okuda K, Kojiro M, Jimi A, Yamaguchi R, Sakamoto K, Ikari T. Pathology of hepatocellular carcinoma in Japan. 232 Consecutive cases autopsied in ten years. Cancer. 1983;51:863–877. doi: 10.1002/1097-0142(19830301)51:5<863::aid-cncr2820510520>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 8.Hashimoto M, Watanabe G, Matsuda M, Yamamoto T, Tsutsumi K, Tsurumaru M. Case report: gastrointestinal bleeding from a hepatocellular carcinoma invading the transverse colon. J Gastroenterol Hepatol. 1996;11:765–767. doi: 10.1111/j.1440-1746.1996.tb00328.x. [DOI] [PubMed] [Google Scholar]
- 9.Chen CY, Lu CL, Pan CC, Chiang JH, Chang FY, Lee SD. Lower gastrointestinal bleeding from a hepatocellular carcinoma invading the colon. J Clin Gastroenterol. 1997;25:373–375. doi: 10.1097/00004836-199707000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Srivastava DN, Gandhi D, Julka PK, Tandon RK. Gastrointestinal hemorrhage in hepatocellular carcinoma: management with transheptic arterioembolization. Abdom Imaging. 2000;25:380–384. doi: 10.1007/s002610000056. [DOI] [PubMed] [Google Scholar]
- 11.Zech CJ, Bilzer M, Mueller-Lisse UG, Steitz HO, Haraida S, Reiser MF. Perforation of the colon: a rare complication of hepatocellular carcinoma. Acta Radiol. 2006;47:538–542. doi: 10.1080/02841850600635947. [DOI] [PubMed] [Google Scholar]
- 12.Fujii K, Nagino M, Kamiya J, Uesaka K, Sano T, Yuasa N, Oda K, Nimura Y. Complete resection of hepatocellular carcinoma with direct invasion to the stomach remnant. J Hepatobiliary Pancreat Surg. 2004;11:441–444. doi: 10.1007/s00534-004-0926-3. [DOI] [PubMed] [Google Scholar]


