ABSTRACT
This article reports on the presence of an anatomic feature of the extracranial skull base that may result in internal carotid artery injury if secure and complete pterygomaxillary separation is not achieved before maxillary downfracture in the Le Fort I osteotomy. The extracranial skull base of 129 adult skulls and 10 pediatric skulls was examined in the region near the foramen lacerum. This region was inspected for the presence or absence of a bony protrusion that projected posteriorly from the base of the sphenoid, lying inferior to the foramen lacerum. The bony protrusion was present bilaterally in 71% of the adult skulls and 60% of the pediatric skulls. The protrusion was a bony “spike” that pointed posteriorly and was located inferior to the foramen lacerum on the extracranial skull base. Due to its size, shape, and location, the bony protrusion described in this study poses considerable risk to the internal carotid artery if the protrusion is displaced superiorly through the foramen lacerum. In the Le Fort I osteotomy, secure and complete pterygomaxillary separation is crucial to avoid injury to the internal carotid artery during maxillary downfracture.
Keywords: Le Fort I osteotomy, internal carotid artery, anterior skull base, foramen lacerum, pterygomaxillary separation, maxillary downfracture
The Le Fort I maxillary osteotomy is one of several surgical approaches to the central skull base and is used for access to numerous skull base tumors and lesions.1 One primary advantage of this approach is wide operative exposure, allowing access to craniocervical lesions from the sphenoid to the fourth cervical vertebra between the carotids.1 The Le Fort I osteotomy is also routinely used in the management of dentofacial anomalies.2 The comprehensive technical aspects of the exposure have been well described in the literature.1,3,4,5
Injuries to the internal carotid artery during the Le Fort I osteotomy have been reported in the literature.6,7,8,9,10,11,12,13,14 Although rare, these complications can have severe consequences. The purpose of this study is to examine the anatomy of the extracranial skull base and the potential mechanisms by which internal carotid artery injury may occur during the Le Fort I osteotomy. Specifically, we describe the presence of a bony protrusion on the extracranial surface of the sphenoid, inferior to the foramen lacerum. This protrusion has the potential to be displaced superiorly through the foramen lacerum, posing considerable risk to the internal carotid artery. The presence of this bony protrusion highlights the importance of secure and complete pterygomaxillary separation before maxillary downfracture to reduce the risk of vascular complications involving the internal carotid artery during the Le Fort I osteotomy.
MATERIALS AND METHODS
Demographic Data
A total of 129 adult and 10 pediatric cadaveric skulls were obtained for inspection at the Cleveland Museum of Natural History. Of the adult skulls, 63 were female and 66 were male. Of the pediatric skulls, 8 were female and 2 were male. The average age of the adult skulls was 49 years, with a median of 48 years and a range of 18 to 85 years. The average age of the pediatric skulls was 14 years, with a median of 14 years and a range of 10 to 16 years.
Skull Base Examination
The region surrounding the foramen lacerum on the extracranial skull base was examined bilaterally on all 139 skulls. The presence or absence of a bony protrusion inferior to the foramen lacerum was determined. Protrusions were counted as present if the base of the sphenoid protruded posteriorly, resulting in a projection of bone inferior to the foramen lacerum. As a result, the bony protrusions influenced the shape of the foramen lacerum when viewed from the extracranial skull base and were visible from the intracranial skull base when looking inferiorly through the foramen lacerum.
Because no consistent landmark existed among the skulls, the size of the protrusions was estimated using trigonometry. The protrusions approximated the shape of a triangle, with the apex projecting inferior to the foramen lacerum. Fine-needle digital calipers were used to measure the dimensions of a triangle, with the three points being the apex of the protrusion and the two points of attachment to the body of the sphenoid (Fig. 1). The height of the triangle was then calculated and used to estimate the anterior-posterior distance of the protrusion. When the foramen lacerum was free of any bony protrusion from the base of the sphenoid, no measurements were taken and protrusion was determined to be absent. A single author (SYK) conducted examination and measurements of the skull base.
Figure 1.
The length of the protrusion was estimated using trigonometry. The apex of the protrusion and the two points of attachment to the body of the sphenoid formed the three points of the triangle (shown in gray). The height of the triangle (shown in black) was calculated and used to estimate the anterior-posterior distance of the protrusion.
RESULTS
The bony protrusion was present in 91 of 129 (71%) adult skulls and 6 of 10 (60%) pediatric skulls (Table 1). This protrusion formed a “spike” on the extracranial surface of the skull base where the posterior portion of the medial pterygoid plate joined the base of the sphenoid (Figs. 2–4). The apex of the “spike” pointed posteriorly and protruded inferior to the foramen lacerum. Figure 2 shows the bilateral protrusions on the extracranial skull base. Figure 3 is a close-up view of the protrusion, highlighting the pointed nature of the apex. Figure 4 is a view of the intracranial skull base, where the protrusion is clearly visible through the foramen lacerum.
Table 1.
Summary of the Skull Base Examination
| Total Number with Protrusion | Percent of Population with Protrusion | Length of Protrusion (mm), Right | Standard Deviation (mm), Right | Length of Protrusion (mm), Left | Standard Deviation (mm), Left | |
|---|---|---|---|---|---|---|
| Adult | 91 | 71 | 3.20 | 1.05 | 3.36 | 1.09 |
| Pediatric | 6 | 60 | 2.50 | 0.739 | 2.94 | 1.05 |
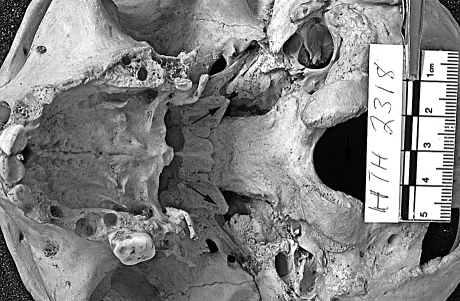
Figure 2.
Examples of the bony protrusions (arrows) are shown on the extracranial skull base, projecting inferior to the foramen lacerum.
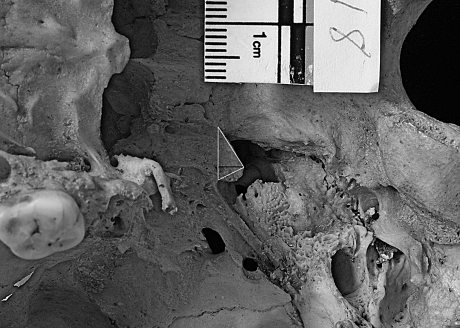
Figure 3.
An example of the bony protrusion (arrow) is shown on the left side of the extracranial skull base, clearly showing the pointed nature of the protrusion.
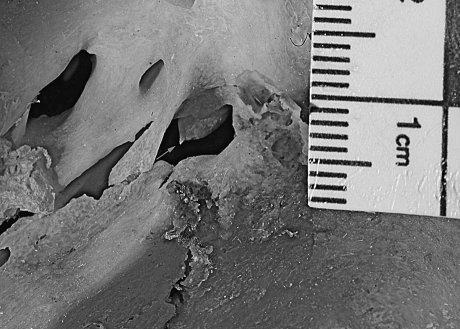
Figure 4.
An example of the bony protrusion (arrow) is shown from the viewpoint of the intracranial skull base and is clearly visible through the foramen lacerum.
In cases where protrusion was not present, the foramen lacerum was absent of bony projections that altered the contour of the foramen. Figure 5 shows an example of a skull where bony protrusions were absent. The shape of the protrusion was maintained but was further anterior on the skull base and did not project inferior to the foramen lacerum.
Figure 5.
An example of a skull in which no bony protrusion was present. The shape of the protrusion was maintained (small arrow) at the base of the sphenoid, but did not extend into the region of the foramen lacerum (large arrow).
The protrusion was present in both sexes and at all ages. In the adult population, the protrusion was found in 76% of women and 65% of men. The age of the skulls with the protrusion ranged from 10 to 83 years. In all cases where the protrusion was present, it was present bilaterally. In adult skulls with the protrusion, the average anterior-posterior length was 3.20 mm on the right and 3.36 mm on the left. In the pediatric skulls with the protrusion, the average anterior-posterior length was 2.50 mm on the right and 2.94 mm on the left. These data are summarized in Table 1.
DISCUSSION
Complications specifically related to the Le Fort I osteotomy include traction injury to the infraorbital nerve; injury to dental roots; lacrimal duct disruption; avascular necrosis of the soft tissue lining, bone, and teeth; postoperative malocclusion; oronasal fistula; and velopharyngeal dysfunction.1 Although relatively rare, there are multiple reports of internal carotid artery injury following the Le Fort I osteotomy. Previous reports of carotid-cavernous sinus fistula6,7,8,9 and internal carotid artery dissection,10 aneurysm,11,12 thrombosis,13 and laceration14 following the Le Fort I osteotomy all exist, mostly in the oral and maxillofacial surgery literature.
The report by Newhouse et al (1982)11 is of particular relevance to this study. The authors described a case of a 32-year-old woman that suffered profuse arterial hemorrhage from the right posterior region following downfracture of the maxilla. Angiography revealed a traumatic arteriovenous fistula involving the right internal carotid artery and the internal jugular vein at the skull base. Upon repair of the fistula, the surgeons noted that the right pterygoid plates were completely separated from the sphenoid base and the maxilla. It was speculated that during pterygomaxillary dysjunction, the right pterygoid complex was detached, resulting in a sharp bony edge. During downfracture, this bony edge may have been forced posteriorly, lacerating the internal carotid artery.
The bony protrusion described in this study presents a similar mechanism by which the internal carotid artery may be injured during the Le Fort I osteotomy. The size, shape, and location of the protrusion make its presence a danger in the event that it is displaced superiorly, injuring the internal carotid artery in its course superior to the foramen lacerum.
The protrusion likely poses the greatest risk during pterygomaxillary separation and maxillary downfracture. If the skull base is fractured during pterygomaxillary separation, the protrusion may be displaced superiorly through the foramen lacerum. Additionally, if pterygomaxillary separation is incomplete, when force is delivered to the maxilla during downfracture, the downward force may also transfer to the body of the sphenoid and the pterygoid plates. As a result, the protrusion may be forced superiorly through the foramen lacerum during downfracture. Difficulty during downfracture of the maxilla was encountered in two of the previously reported cases of internal carotid artery injury,6,9 which may have been due to an incomplete pterygomaxillary osteotomy. The presence of the bony protrusion described in this study highlights the importance of achieving secure and complete pterygomaxillary separation before maxillary downfracture.
CONCLUSION
Although complications involving the internal carotid artery during the Le Fort I osteotomy are rare, they may have devastating consequences and should be avoided at all costs. The presence of a bony protrusion from the base of the sphenoid that projects inferior to the foramen lacerum necessitates extreme care during pterygomaxillary separation and maxillary downfracture. Surgeons should ensure that pterygomaxillary separation is complete before maxillary downfracture to ensure that the protrusion is not displaced superiorly through the foramen lacerum during this maneuver.
ACKNOWLEDGMENTS
The authors would like to thank the Cleveland Museum of Natural History for providing access to the skulls described in this study. The authors also thank Thomas Gest and Lyman Jellema for their assistance with the study.
REFERENCES
- Roy S, Patel P K, Tomita T. The LeFort I transmaxillary approach to skull base tumors. Clin Plast Surg. 2007;34(3):575–583. doi: 10.1016/j.cps.2007.05.013. [DOI] [PubMed] [Google Scholar]
- Cruz A A, dos Santos A C. Blindness after Le Fort I osteotomy: a possible complication associated with pterygomaxillary separation. J Craniomaxillofac Surg. 2006;34(4):210–216. doi: 10.1016/j.jcms.2006.01.001. [DOI] [PubMed] [Google Scholar]
- Belmont J R. The Le Fort I osteotomy approach for nasopharyngeal and nasal fossa tumors. Arch Otolaryngol Head Neck Surg. 1988;114(7):751–754. doi: 10.1001/archotol.1988.01860190055022. [DOI] [PubMed] [Google Scholar]
- Brown D H. The Le Fort I maxillary osteotomy approach to surgery of the skull base. J Otolaryngol. 1989;18(6):289–292. [PubMed] [Google Scholar]
- Sasaki C T, Lowlicht R A, Astrachan D I, Friedman C D, Goodwin W J, Morales M. Le Fort I osteotomy approach to the skull base. Laryngoscope. 1990;100(10 Pt 1):1073–1076. doi: 10.1288/00005537-199010000-00009. [DOI] [PubMed] [Google Scholar]
- Bendor-Samuel R, Chen Y R, Chen P K. Unusual complications of the Le Fort I osteotomy. Plast Reconstr Surg. 1995;96(6):1289–1296. discussion 1297. [PubMed] [Google Scholar]
- Brady S C, Courtemanche A D, Steinbok P. Carotid artery thrombosis after elective mandibular and maxillary osteotomies. Ann Plast Surg. 1981;6(2):121–126. [PubMed] [Google Scholar]
- Hes J, de Man K. Carotid-cavernous sinus fistula following maxillofacial trauma and orthognathic surgery. Int J Oral Maxillofac Surg. 1988;17(5):295–297. doi: 10.1016/s0901-5027(88)80006-7. [DOI] [PubMed] [Google Scholar]
- Lanigan D T, Tubman D E. Carotid-cavernous sinus fistula following Le Fort I osteotomy. J Oral Maxillofac Surg. 1987;45(11):969–975. doi: 10.1016/0278-2391(87)90452-6. [DOI] [PubMed] [Google Scholar]
- Lo L J, Hung K F, Chen Y R. Blindness as a complication of Le Fort I osteotomy for maxillary distraction. Plast Reconstr Surg. 2002;109(2):688–698. discussion 699–700. doi: 10.1097/00006534-200202000-00041. [DOI] [PubMed] [Google Scholar]
- Newhouse R F, Schow S R, Kraut R A, Price J C. Life-threatening hemorrhage from a Le Fort I osteotomy. J Oral Maxillofac Surg. 1982;40(2):117–119. doi: 10.1016/s0278-2391(82)80039-6. [DOI] [PubMed] [Google Scholar]
- Singhal A, Golomb M, Mochida G, et al. Another case of internal carotid artery dissection after mandibular osteotomy. J Oral Maxillofac Surg. 1998;56(1):115–116. doi: 10.1016/s0278-2391(98)90945-4. [DOI] [PubMed] [Google Scholar]
- Suzuki H, Saito E, Hashimoto K. Dissecting aneurysm of the internal carotid artery after a mandibular osteotomy. J Oral Maxillofac Surg. 1997;55(7):747–750. doi: 10.1016/s0278-2391(97)90591-7. [DOI] [PubMed] [Google Scholar]
- Habal M B. A carotid cavernous sinus fistula after maxillary osteotomy. Plast Reconstr Surg. 1986;77(6):981–987. [PubMed] [Google Scholar]