Abstract
Purpose
To examine the association between severity of visual field loss (VFL) and self-reported health-related quality of life (HRQOL) in a population-based sample.
Design
Population-based cross-sectional study.
Methods
Participants in the Los Angeles Latino Eye Study underwent a comprehensive ophthalmic examination including visual field testing using the Humphrey Automated Field Analyzer II (SITA Standard 24-2). Mean Deviation (MD) scores were used to determine severity of VFL both as a continuous variable and stratified by severity: no VFL (MD≥ − 2 decibels [dB]), mild VFL (6dB<MD<−2dB), moderate/severe VFL (MD<−6dB). HRQOL was assessed by the Medical Outcomes Study 12-Item Short-Form Health Survey (SF-12) and the National Eye Institute Visual Function Questionnaire (NEI-VFQ-25). Linear regression analyses and analysis of covariance were used to assess the relationship between HRQOL scores and VFL.
Results
Of the 5,213 participants included in this study, 18% had unilateral mild, 1.5% unilateral moderate/severe, 19% bilateral mild, and 6.5% bilateral moderate/severe VFL. Worse NEI-VFQ-25 and SF-12 HRQOL scores were associated with VFL in a linear manner. 4–5 dB differences in VFL were associated with a 5-point difference in the NEI-VFQ composite and most subscale scores. Persons with VFL had the greatest difficulty with driving activities, dependency, mental health, distance vision and peripheral vision.
Conclusion
HRQOL is diminished even in persons with relatively mild VFL based on MD scores. Prevention and management of persons with VFL may be important in preventing or reducing poor HRQOL related to difficulties in driving, distance and peripheral vision activities and a sense of dependency.
Introduction
The number of people at risk for age-related eye diseases and vision loss associated with these diseases is expected to increase in the next several decades as the U.S. population ages.1 Visual impairment is assessed by several measures including visual acuity (VA) and peripheral visual field. Worse VA has been associated with a decreased ability to complete daily activities 2, 3, increased falls 4, increased risk of car accidents 4, and increased mortality.5 Less is known about the impact of peripheral visual field loss (VFL) on the ability of people to perform normal, daily activities, however there is evidence that VFL, independent of VA, is associated with diminished mobility, diminished ability to complete activities such as reading or watching television 6, and with an increased risk of falling and/or injury.3, 6, 7 Several studies have described the impact of VFL on vision-related daily functioning and well-being or health-related quality of life (HRQOL) in glaucoma (a disease that is associated with both VA and VF loss) patients.8–10 However, these studies are based on selected clinic-based groups of persons and the impact of VFL on HRQOL among a general, population-based sample has not been well described.
We examined the association between severity of VFL and HRQOL in adults participating in The Los Angeles Latino Eye Study (LALES), a population-based prevalence study of eye disease in adult Latinos residing in Los Angeles, California. The study was designed to examine how severity of VFL impacts general and vision-targeted HRQOL. We also examined the types of daily activities that are most impacted by VFL and compared these results to previous findings of daily activities impacted by VA associated visual impairment.
METHODS
Data for this analysis were collected as part of LALES, a population-based prevalence study of eye disease in Latinos living in Los Angeles, CA aged 40 years and older. Details of the study design and data collected have been described previously.11 Briefly, a census of all residential households in 6 census tracts in La Puente, CA was completed to identify individuals eligible to be included in the study. Eligibility includes men and women aged 40 years and older, who are Latinos (self-described), and residing in any of the 6 census tracts. Eligible participants were given a verbal and written description of the study and invited to participate in both a home interview and a clinic examination between February 2000 and May 2003. Demographic and socioeconomic characteristics of participants were similar to those of the Latino population in the U.S. 11. All study procedures adhered to the principles outlined in the Declaration of Helsinki for research involving human subjects. Institutional review board (IRB)/ethics committee approval was obtained from the Los Angeles County/University of Southern California Medical Center Institutional Review Board.
Socio-demographic and Clinical Data
A brief home interview was completed after informed consent was obtained including information on demographics, history of ocular and medical conditions, access to health care, health insurance coverage for eye care, and degree of acculturation.12 Operational definitions for these variables were similar to those described in the Hispanic Health and Nutrition Examination Survey.13,14 Twelve self-reported medical conditions were measured using a systematic co-morbidity summation score including: diabetes mellitus, arthritis, stroke or brain hemorrhage, high blood pressure, angina, heart attack, heart failure, asthma, skin cancer, other cancers, back problems, and deafness or hearing problems.15–17 Acculturation was measured using the short-form Cuellar Acculturation Scale,14 with scale scores ranging from 1 to 5 (5 representing the highest level of acculturation). 14
Visual Field Loss Assessment and Definitions
Visual field testing was completed to assess a participant’s ability to detect objects in the periphery of their visual environment. Visual field testing was performed separately in each eye using the Humphrey Field Analyzer II (Swedish Interactive Thresholding Algorithm Standard 24-2 program) (Carl Zeiss Meditec, Dublin, CA). Visual field testing was repeated for any abnormal results; results of the second test were recorded and qualitatively confirmed as visual field loss by two ophthalmologists. Severity of visual field loss was analyzed using two approaches: (i) as a continuous variable using mean deviation (MD) in decibels (dB) as a measure of severity and (ii) stratified by bilaterality and level of visual field loss into five categories: no VFL (MD>−2 dB in both eyes), unilateral mild VFL(−6 dB ≤MD≤ −2 dB in the worse eye), unilateral moderate/severe VFL(MD<−6 dB in one eye, MD>−2 dB in the other eye), bilateral mild VFL(−6 dB≤MD≤ −2 dB in both eyes; or −6 dB ≤MD≤ −2 dB in one eye, MD<−6 dB in the other eye), and bilateral moderate/severe VFL(MD<−6 dB in the both eyes). The severity classification is based on previous work by Cello, Nelson-Quigg and Johnson.18
Visual Acuity Assessment
The procedure used to measure presenting distance visual acuity in LALES has been described previously.19–21 Presenting distance visual acuity for each LALES participant was measured with the presenting correction (if any) at 4 m using modified Early Treatment Diabetic Retinopathy Study distance charts trans-illuminated with the chart illuminator (Precision Vision, La Salle, III). Presenting visual acuity was scored as the total number of letters read correctly and converted to a logarithm of the minimum angle of resolution (logMAR) score.
Health Related Quality of Life (HRQOL) Measures
SF-12
General HRQOL was measured using the Medical Outcomes Study 12-Item Short-Form Health Survey (SF-12, version 1). 22 Data from the SF-12 was used to calculate the standard U.S. norm-based SF-12 Physical Component Summary (PCS) and Mental Component Summary (MCS) scores.23 Higher PCS and MCS scores represent better HRQOL. 23
NEI-VFQ-25
Vision-targeted HRQOL was assessed by the NEI-VFQ-25.24,25 The NEIVFQ-25 was designed to measure the dimensions of self-reported vision-targeted health status that are important for person who have chronic eye diseases.24 The survey measures the influence of visual disability and visual symptoms on generic health domains such as emotional well-being and social functioning, in addition to task-oriented domains related to daily visual functioning.24,25 The survey is composed of 12 vision-targeted scales: general vision, near and distance vision activities, ocular pain, vision-related social function, vision-related role function, vision-related mental health, vision-related dependency, driving difficulties, color vision, and peripheral vision. The VFQ-25 also includes a general health item similar to one of the SF-12 items. Each subscale consisted of a minimum of 1 and a maximum of 4 items. The standard algorithm was used to calculate the scale scores, which have a possible range from 0 to 100. Higher score represents better visual functioning and well-being. Eleven of the 12 scale scores (excluding the general health item) were averaged to yield a composite score.24
Interviewers administered the questionnaires (before the clinical examination) in either English or Spanish according to participant preference at the LALES Local Eye Examination Center.
Statistical Analyses
Analysis of variance was used to compare continuous demographic characteristics by severity of unilateral and bilateral VFL with means and standard deviations presented for age (years), acculturation scores, and number of comorbidities. Tukey pairwise comparisons were used to identify significant differences across subgroups of VFL severity. Categorical variables [unemployed (yes/no), income ≤ $20,000 (yes/no), education (< high school, high school graduate and < high school, high school graduate, college training or higher), health insurance (yes/no), vision insurance (yes/no), visual acuity loss (none, unilateral mild, unilateral moderate/severe, bilateral mild one eye and moderate/severe second eye, bilateral moderate/severe both eyes)] are presented as frequencies and percents; differences across subgroups were compared using chi-square tests. Bonferroni-adjusted pairwise comparisons were conducted at the 0.05 level for the categorical variables.
Actual and predicted mean NEI-VFQ-25 composite scores were plotted against MD for the worse eye and MD for the better eye. The plotted figures show means for each unit of MD (in decibels) from 0 to −30dB. Predicted mean MCS, PCS and the NEI-VFQ-25 composite and subscale scores were calculated for each MD value of visual field loss, adjusting for age, gender, education, employment status, income, acculturation, health insurance, vision insurance, number of co-morbidities, and visual acuity. The plot of predicted QOL scores and visual field loss scores allows a more accurate evaluation of the independent relationship between these two variables. To examine possible nonlinear relationships between HRQOL measures and VFL in the better and worse seeing eyes, an iterative, locally weighted, least squares method was used to generate lines of best fit (LOWESS fit line).26
Analysis of covariance was used to compare SF-12 PCS and MCS and the NEI-VFQ-25 subscale and composite scores by five severity categories of VFL (none, unilateral mild, unilateral moderate/severe, bilateral mild, bilateral moderate/severe). Models were adjusted for age, gender, education, employment status, income, acculturation, health insurance, vision insurance, number of co-morbidities, and visual acuity.27
Due to the skewed score distribution toward the higher scores, a logarithmic transformation was performed to normalize the distribution using the formula tSCORE = ln(101-SCORE), in which tSCORE and SCORE are the transformed and untransformed values of the NEI-VFQ-25 scales, respectively. If significant differences were present, Tukey multiple comparison28,29 tests for adjusting the overall significance level were used to identify significant pairwise differences in the logarithmically transformed scale and composite scores. For ease of interpretation, however, results are reported in the original untransformed scale.
Effect size is a group of indices used to measure the magnitude of impact of one variable on an outcome variable. The magnitude of the effect size is independent of sample sizes. To measure the impact of the magnitude of VFL on HRQOL, a covariate adjusted effect size (ES) was calculated as the difference in the covariate adjusted mean scores (between each severity level of VFL and no VFL) divided by the standard deviation of the scores for the no VFL group.30 The standard deviation for the no VFL group was used, rather than the traditional pooled standard deviation corresponding to the subgroups associated with each pairwise comparison, in order to provide a “common denominator” for all pairwise comparisons. Effect sizes of 0.20–0.49 are considered small, 0.50–0.79 as moderate, and 0.80 or greater as large.31,32
All analyses were conducted using SAS software 9.1 (SAS Institute, Inc., Cary, NC) at the 0.05 significance level.
RESULTS
Description of Study Cohort
Of the 7,789 participants who were eligible for LALES, 1,432 were excluded from the study because they did not complete the ophthalmic examination; the overall participation rate for the clinical examination among eligible residents was 82%. Of the 6,357 that completed the ophthalmic exam, 1,144 (15%) were excluded from the current analysis because they were missing SF-12, NEI-VFQ-25, covariate data, or did not complete visual field testing resulting in 5,213 participants in the HRQOL analysis. The mean age of the LALES participants in this analysis was 55 years (range 40 – 98). Of the 5,213 included in the analysis 3,081 (59%) were females, 1,762 (34%) had a high school education or higher, and 2,660 (51%) had insurance that covered vision care. Included participants were similar to excluded individuals with the exception of gender (59% participants were female vs. 54% non-participants; p<0.005), employment status (48% of participants currently employed vs. 53% of non participants; p<0.004), and self-reported annual income (45% of participants below $20,000 annually vs. 40% of non participants; p<0.0006).
The characteristics of the LALES population by severity of VFL are shown in Table 1. In the LALES population, severity of VFL increased with increasing age of the participants (trend p<0.0001); participants with bilateral moderate or severe VFL were significantly older (63.5 years) than participants without VFL (52.4 years) (Table 1). Participants with bilateral moderate or severe VFL also were more likely to be female (68% vs. 56%), have more co-morbidities (2.5 vs. 1.3), have finished their high school education (77% vs. 61%), and were more likely to be unemployed (82% vs. 42%) than participants without VFL (all p-values<0.05 by Tukey tests). We also noted that participants with bilateral moderate or severe VFL were significantly more likely to have visual acuity loss than participants with bilateral mild, unilateral mild, or no VFL (p<0.0001). The prevalence of any visual field loss varies depending on the definition. If, the prevalence of VFL is defined as MD≤ −2 dB in the ‘better seeing eye’ the prevalence of visual field loss was 25% (1,305/5,213).
Table 1.
Socio-demographic and Clinical Characteristics of participants in the Los Angeles Latino Eye Study stratified by various categories of severity of Visual Field Loss (N= 5,213)
| Visual Field Loss |
||||||
|---|---|---|---|---|---|---|
| Unilateral |
Bilateral |
|||||
| Socio-demographic and Clinical Characteristics* | No Visual Field Loss (N=2,886) | Mild (N=945) | Moderate/Severe (N=77) | Mild (N=965) | Moderate/Severe (N=340) | P-value† |
| Age (years) | 52.4 (9.0)a | 55.5(10.7)b | 60.0 (10.8)c | 58.9(11.9)c | 63.5(12.9)d | <0.0001 |
| Acculturation Score‡ | 1.9(0.9)a | 1.7(0.8)a,b | 1.8(0.9)a,b | 1.7(0.8)b | 1.7(0.9)b | <0.0001 |
| Co-morbidities§ | 1.3 (1.4)a | 1.6(1.5)b,c | 1.7 (1.5)b | 1.9 (1.7)b | 2.5(1.9)c | <0.0001 |
| Gender: Female | 1,606 (55.6)a | 580 (61.4)b | 42 (54.5)a,b | 622 (64.5)b,c | 231 (67.9)c | <0.0001 |
| Unemployed | 1,221 (42.3)a | 521 (55.1)b | 54(70.1)c | 633 (65.6)c | 280 (82.4)d | <0.0001 |
| Income≤$20,000 | 1,199 (41.5)a | 445 (47.1)b | 40 (51.9)a,b,c | 523 (54.2)c | 191 (56.2)c | <0.01 |
| Education<12 years | 1,131 (39.2)a | 299 (31.6)b | 18 (23.4)b,c | 237 (24.6)c | 77 (22.6)c | <0.0001 |
| Health Insurance: Yes | 1,881 (65.2)a | 622 (65.8)a,b | 51 (66.2)a,b | 579 (60.0)b | 235 (69.1)a | <0.0001 |
| Vision Insurance: Yes | 1,470 (50.9) | 495 (52.4) | 39 (50.6) | 474 (49.1) | 182 (53.5) | 0.56 |
| Visual Acuity Loss: None¶ | 2,585 (89.6)a | 747 (79.0)b | 30 (39.0)c | 666 (69.0)d | 147 (43.2)c | <0.0001 |
Data are presented as mean ± standard deviation (SD) for continuous variables (age, acculturation score, and co-morbidities); categorical variables are presented as frequency counts with percents (%) of individuals in severity of visual field loss category.
P-values based on ANOVA for continuous variables and chi-square tests for categorical variables (with Bonferroni-adjusted pairwise comparisons).
Acculturation was measured using the short-form Cuellar Acculturation Scale.
Number of self-reported co-morbidities (diabetes, arthritis, stroke/brain hemorrhage, high blood pressure, angina, heart attack, heart failure, asthma, skin cancer, other cancer, back problems, hearing problems and other major health problems).
Visual Acuity Loss was defined as presenting visual acuity 20/40 or worse.
Relationship Between HRQOL and Severity of VFL
In our study, there was a decrement in HRQOL associated with mild visual field loss. SF-12 and NEI-VFQ-25 scores were significantly lower in persons with greater VFL (more negative MD values). Plots of adjusted mean NEI-VFQ-25 composite scores show an approximate linear relationship with MD of the better seeing eye (Figure 1). The same plot for the worse seeing eye shows a similar pattern with a smaller β coefficient (Figure 2). Plots of all NEI-VFQ-25 subscales (data not shown) indicate a linear pattern with MD, with the exception of the general health subscale which declines from 0 to −10 dB and then reaches a threshold and remains flat for more extreme values of MD. Plots of adjusted mean SF-12 Physical composite scores show an approximate linear relationship with MD of the better seeing eye from 0 to −30 dB (Figure 3) with significantly smaller β coefficients than those for the NEI-VFQ scores. The same plot of the worse seeing eye shows a similar linear pattern with a flattening of the plot at MD values of −20 dB and worse (Figure 4). Table 2 shows the model β coefficients for the adjusted mean NEI-VFQ-25 composite, subscale, and SF-12 component scores by MD for the better and worse seeing eye. As expected, the β coefficients for the SF-12 scores are significantly smaller than those for the NEI-VFQ scores. The largest β coefficients were noted for driving difficulties (β =1.6), vision related dependency (β =1.4), and vision related mental health (β =1.2). β coefficients were consistently larger for the better seeing eye.
Figure 1.
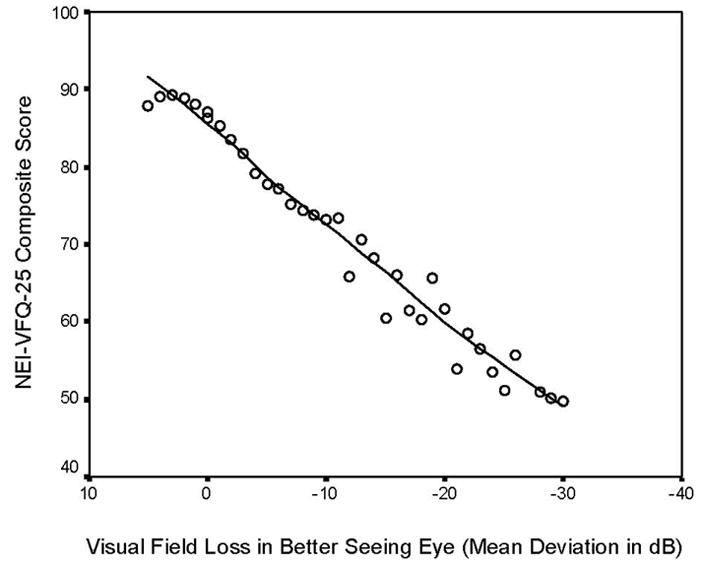
Linear regression plot of NEI-VFQ-25 composite scores and visual field loss (Mean Deviation scores in decibels) in better seeing eye. The NEI- VFQ-25 composite scores are adjusted for co-variates including age, gender, education, employment status, income, acculturation, co-morbidities, health insurance, vision insurance, and visual acuity impairment. The mean deviation-specific data of all persons by each unit of mean deviation of visual field loss were plotted to show the independent relationship of visual field loss with vision-specific quality of life.
Figure 2.
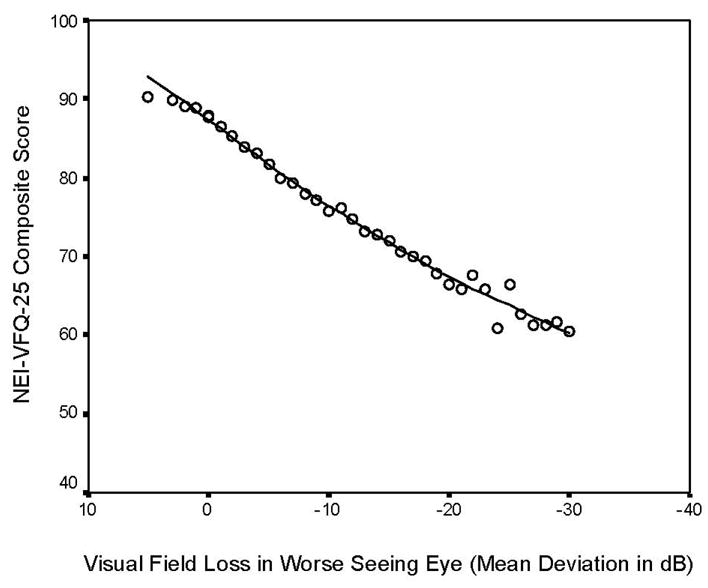
Linear regression plot of NEI-VFQ-25 composite scores and visual field loss (Mean Deviation scores in decibels) in worse seeing eye. The NEI- VFQ-25 composite scores are adjusted for co-variates including age, gender, education, employment status, income, acculturation, co-morbidities, health insurance, vision insurance, and visual acuity impairment. The mean deviation-specific data of all persons by each unit of mean deviation of visual field loss were plotted to show the independent relationship of visual field loss with vision-specific quality of life.
Figure 3.
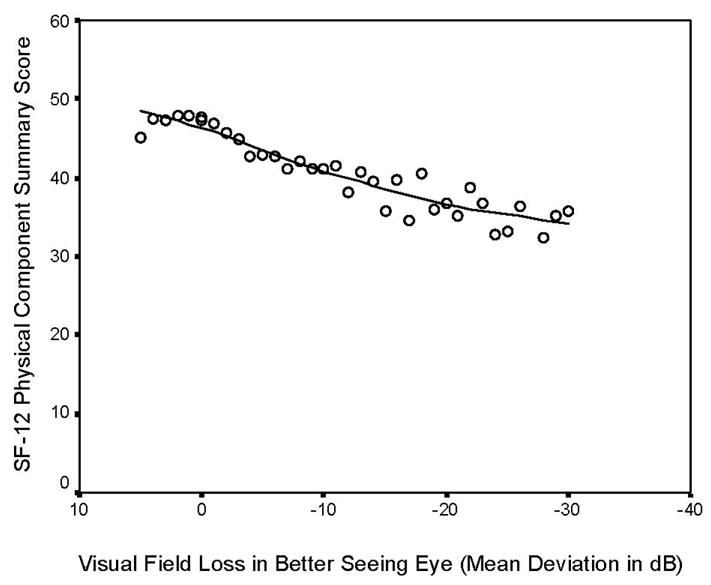
Linear regression plot of SF-12 Physical Composite Scores and visual field loss (Mean Deviation scores in decibels) in better seeing eye. The SF-12 Physical Composite scores are adjusted for co-variates including age, gender, education, employment status, income, acculturation, comorbidities, health insurance, vision insurance, and visual acuity impairment. The mean deviation-specific data of all persons by each unit of mean deviation of visual field loss were plotted to show the independent relationship of visual field loss with generic health-related quality of life.
Figure 4.
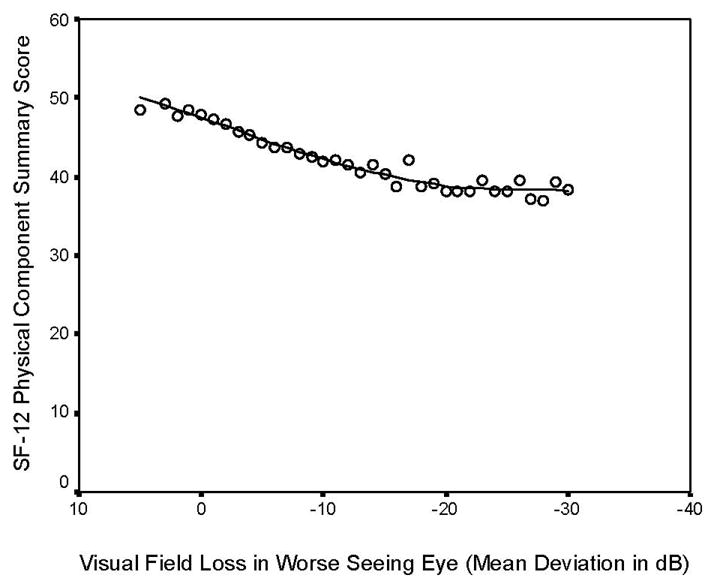
Linear regression plot of SF-12 Physical Composite scores and visual field loss (Mean Deviation scores in decibels) in worse seeing eye. The SF-12 Physical Composite scores are adjusted for co-variates including age, gender, education, employment status, income, acculturation, comorbidities, health insurance, vision insurance, and visual acuity impairment. The mean deviation-specific data of all persons by each unit of mean deviation of visual field loss were plotted to show the independent relationship of visual field loss with generic health-related quality of life.
Table 2.
Linear regression β coefficients for the association between Visual field loss (Mean Deviation Score in decibels) and Health Related Quality of Life (adjusted NEI-VFQ – 25 and SF-12 scores) in Los Angeles Latino Eye Study participants, stratified by visual field loss in the better and worse seeing eye.
| VFL in Better Seeing Eye |
VFL in Worse Seeing Eye |
|||
|---|---|---|---|---|
| Health Related Quality of Life measures | βcoefficient (95% CI) | P-value | β coefficient (95% CI) | P-value |
| SF-12 | ||||
| MCS | 0.21 (0.13, 0.29) | <.0001 | 0.11 (0.05, 0.17) | 0.0003 |
| PCS | 0.23 (0.16, 0.29) | <.0001 | 0.17 (0.12, 0.22) | <.0001 |
| NEI-VFQ-25 | ||||
| General Health | 0.42 (0.26, 0.59) | <.0001 | 0.32 (0.19, 0.44) | <.0001 |
| Color Vision | 0.67 (0.56, 0.79) | <.0001 | 0.38 (0.30, 0.47) | <.0001 |
| Driving Difficulties|| | 1.56 (1.38, 1.74) | <.0001 | 1.09 (0.95, 1.23) | <.0001 |
| Distance Vision | 1.02 (0.89, 1.16) | <.0001 | 0.71 (0.61, 0.81) | <.0001 |
| Near Vision | 0.97 (0.82, 1.12) | <.0001 | 0.71 (0.59, 0.82) | <.0001 |
| Vision Related Dependency | 1.42 (1.27, 1.56) | <.0001 | 0.97 (0.86, 1.08) | <.0001 |
| General Vision | 0.51 (0.38, 0.63) | <0001 | 0.41 (0.32, 0.50) | <.0001 |
| Vision Related Mental Health | 1.20 (1.04, 1.37) | <.0001 | 0.92 (0.80, 1.04) | <.0001 |
| Ocular Pain | 0.70 (0.55, 0.86) | <.0001 | 0.51 (0.40, 0.63) | <.0001 |
| Peripheral Vision | 0.92 (0.76, 1.07) | <.0001 | 0.79 (0.67, 0.90) | <.0001 |
| Vision Related Role Function | 1.02 (0.87, 1.18) | <.0001 | 0.77 (0.66, 0.89) | <0001 |
| Vision Related Social Function | 0.78 (0.67, 0.88) | <.0001 | 0.50 (0.42, 0.58) | <.0001 |
| Composite¶ | 0.94 (0.85, 1.04) | <.0001 | 0.69 (0.61,0.76) | <.0001 |
Note: data are presented as coefficient (95% CI). Abbreviations: SF-12, Medical Outcomes Study 12-Item Short-Form Health Survey, MCS, Mental Component Summary; PCS, Physical Component Summary; NEI-VFQ-25, National Eye Institute Visual Function Questionnaire 25-Item. VFL: Visual field loss. The SF-12 and NEI-VFQ-25 scores were adjusted for: age, gender, education, employment status, income, acculturation, co-morbidities, health insurance, vision insurance, and visual acuity impairment.
Scores could be generated for only 3,762 of the participants who reported that they were currently driving or had driven in the past.
Composite score is an un-weighted mean of the 12 subscale scores (except general health).
Table 3 summarizes our findings for HRQOL when VFL is stratified by severity of VFL. While, poorer HRQOL scores were found in persons categorized as having mild unilateral VFL, the largest decrement in HRQOL was found in persons with bilateral moderate/severe VFL. Mean scores were statistically significantly different for a majority of the sub-scale comparisons of unilateral mild, bilateral mild, bilateral moderate/severe, and no VFL (all p-values<0.05). Score differences were smaller (<5) when participants had less severe levels of VFL (bilateral mild, unilateral moderate/severe, unilateral mild) when compared to participants without VFL. Bilateral moderate/severe VFL had the greatest impact on vision-targeted HRQOL on all subscales (all p-values<0.01). Score differences typically did not reach statistical significance when comparing unilateral moderate/severe to no VFL due to the small number of individuals in the unilateral moderate/severe category, with the exception of distance vision and peripheral vision. The greatest score differences were noted for vision related dependency, driving difficulties, vision related mental health and distance and peripheral vision activities. One exception was a large score difference (9) for the peripheral vision subscale between individuals with unilateral moderate/severe VFL versus no VFL.
Table 3.
Analysis of Covariance assessing the relationship between health-related quality of life measures and various categories of severity of visual field loss in the Los Angeles Latino Eye Study (N= 5,213)
| Health Related Quality of Life Measures | Visual Field Loss category* |
|||||
|---|---|---|---|---|---|---|
| Unilateral |
Bilateral |
|||||
| Adjusted Mean Scores (SE)† | No Visual Field Loss (N=2,886) | Mild (N=945) | Moderate/Severe (N=77) | Mild‡ (N=965) | Moderate/Severe (N=340) | p-value§ |
| SF12 | ||||||
| MCS | 50.4 (0.4)a | 49.4 (0.5)b | 51.4(1.2)a,b | 49.8 (0.4)a,b | 47.6 (0.6)c | <0.0001 |
| PCS | 46.7 (0.3)a | 46.2 (0.4)a | 46.0(1.0)a,b | 45.1(0.4)b | 43.0 (0.5)c | <0.0001 |
| NEI-VFQ-25 | ||||||
| General Health | 47.7 (0.8)a,b | 47.5(1.0)a | 48.8 (2.5)a,b,c | 45.2 (0.9)b,c | 41.4(1.2)c | 0.01 |
| Color Vision | 92.9 (0.6)a | 92.7 (0.7)a | 91.5 (1.7)a,b | 90.6 (0.6)b | 85.9 (0.9)c | <0.0001 |
| Driving Difficulties|| | 76.9 (0.8)a | 75.5 (0.9)b | 73.4 (2.4)a,b,c | 73.4 (0.9)c | 59.8(1.3)d | <0.0001 |
| Distance Vision | 80.7 (0.6)a | 79.1 (0.8)b | 75.9 (2.0)b,c,d | 77.0 (0.7)c | 68.4(1.0)d | <0.0001 |
| Near Vision | 75.5 (0.7)a | 74.2 (0.9)b | 72.2 (2.2)a,b,c | 72.5 (0.8)b | 63.8(1.1)c | <0.0001 |
| Vision Related Dependency | 84.9 (0.7)a | 84.0 (0.8)b,c | 83.8 (2.2)a,b,c | 82.0 (0.8)c | 66.7 (1.1)d | <0.0001 |
| General Vision | 64.4 (0.6)a | 63.4 (0.7)a,b | 60.5(1.8)a,b | 62.0 (0.7)b,c | 57.9 (0.9)c | 0.002 |
| Vision Related Mental Health | 71.7 (0.8)a | 70.5 (0.9)b | 71.2 (2.4)a,b,c | 67.2 (0.9)c | 55.0(1.2)d | <0.0001 |
| Ocular Pain | 77.3 (0.8)a | 76.2 (0.9)a,b | 72.7 (2.3)a,b,c | 74.2 (0.9)b | 68.0(1.2)c | <0.0001 |
| Peripheral Vision | 84.8 (0.7)a | 83.1 (0.9)b | 75.7 (2.3)c,d,e | 81.0 (0.8)d | 72.2 (1.2)e | <0.0001 |
| Vision Related Role Function | 84.4 (0.8)a | 83.3 (0.9)a | 81.5(2.3)a,b,c | 81.4 (0.9)b | 70.6(1.2)c | <0.0001 |
| Vision Related Social Function | 89.8 (0.5)a | 89.0 (0.6)a | 89.0(1.6)a,b | 87.4 (0.6)b | 81.2 (0.8)c | <0.0001 |
| Composite¶ | 80.5 (0.5)a | 79.4 (0.6)b | 77.3(1.4)b,c | 77.3 (0.5)c | 68.6 (0.7)d | <0.0001 |
Abbreviations: SF-12, Medical Outcomes Study 12-Item Short-Form Health Survey, MCS, Mental Component Summary; PCS, Physical Component Summary; NEI-VFQ-25, National Eye Institute Visual Function Questionnaire 25-ltem.
Visual field loss was classified as none (mean deviation (MD)>−2), unilateral mild VFL (−6≤MD≤−2 in the worse eye), unilateral moderate/severe VFL (MD<−6 in one eye, MD>−2 in the other eye), bilateral mild VFL (−6≤MD≤−2 in both eyes, or −6≤MD≤−2 in one eye, MD<−6 in the other eye), bilateral moderate/severe VFL (MD<−6 in the both eyes).
Shown in the table are the adjusted mean (standard error) of SF-12 and NEI-VFQ-25 scores. The covariates for adjustment are: age, gender, education, employment status, income, acculturation, co-morbidities, health insurance, vision insurance, and visual acuity impairment.
This category also included one eye with mild VFL and the other eye with moderate/severe VFL.
Analysis of covariance was used to compare logarithmically transformed adjusted mean scores across the different levels of unilateral and bilateral visual field loss. For each row, means with different letters (a–e) across the visual field loss categories are statistically significantly different from one another using Tukey multiple comparison procedure (P<0.05). P-value in the last column is corresponding to the ANCOVA test of significance for the visual field loss groups. ANCOVA revealed significant differences for all scales across the visual field loss categories.
Scores could be generated for only 3,762 of the participants who reported that they were currently driving or had driven in the past.
Composite score is an un-weighted mean of the 12 subscale scores (except general health).
Smaller differences were present in SF-12 MCS and PCS across various strata of VFL severity. The magnitude of the difference in these SF-12 measures achieved statistical significance when comparing participants with bilateral moderate/severe visual field loss to participants without VFL (Table 3).
HRQOL Effect Size Estimates
Small effect sizes were present when comparing individuals with unilateral mild VFL (largest ES≤ 0.12) to those with no VFL. These effect sizes increased in increasing severity of VFL (Figure 3). When comparing HRQOL scores for unilateral moderate/severe VFL to no VFL, small effect sizes were present for four subscales (driving difficulties, vision related mental health, distance vision, and vision related social function) and a moderate effect (ES=0.52) was noted for the peripheral vision subscale. Effects sizes were greatest when comparing participants with bilateral moderate/severe VFL to participants with no VFL. Bilateral moderate/severe VFL had the greatest impact on the NEI-VFQ-25 driving difficulty subscale (ES=1.23), followed by vision specific dependency (ES=1.18) and vision related mental health (ES=0.88) (Figure 3). Effect sizes were large (ES>0.8) for 3 subscales and moderate (ES≥ 0.5) for 7 other subscales (color vision, distance vision, near vision, ocular pain, peripheral vision, vision related role function and vision related social function).
DISCUSSION
In the current analysis, we found that mild VFL in either the better or worse seeing eye (as assessed by Mean Deviation scores using the 24-2 SITA Standard test on the HFA II) is associated with significantly lower self-reported NEI-VFQ-25 scores whether VFL was analyzed as a continuous measure or by categories of severity. Lower NEI-VFQ-25 composite and subscale scores were observed in persons with small losses in MD compared to persons with no VFL (MD>−2 dB in both eyes) and the QOL scores continued to decrease in an approximately linear pattern with greater severity of VFL. If we assume that a difference of 5 points or more in any NEI-VFQ subscale corresponds to a clinically meaningful difference (this difference in QOL scores corresponds to a 2 line difference in visual acuity)28 then our study suggests that a VFL of 4–5 dB in the better or worse seeing eye corresponds to a clinically meaningful difference in vision-related quality of life. Large differences in effect size were observed for individuals with bilateral moderate/severe VFL compared to no VFL (score difference >5 points or ES >0.8), and smaller effects were observed in individuals with more modest loss (unilateral moderate/severe VFL or bilateral mild VFL); one exception was a large score difference for the peripheral vision subscale for moderate/severe VFL, regardless if the loss was unilateral or bilateral.
The data from our population-based study appear to be consistent with previous studies designed to assess the impact of VFL on daily function and HRQOL. Ramrattan et al. have noted in the Rotterdam Eye Study that the greatest impact of VFL on daily activities occurs in those individuals who have bilateral VFL 6. Furthermore, in an evaluation of the relationship between VFL and HRQOL in 147 glaucoma patients and 44 reference normal persons from 5 tertiary care glaucoma practices, Gutierrez et al. reported a linear association between VFL and NEI-VFQ, suggesting that vision-targeted QOL begins to decline with mild VFL and that the impact of VFL on QOL increases with severity of VFL8.
In our study, the largest β coefficients and the largest differences in NEI-VFQ-25 vision-targeted subscales were present for driving difficulties, vision specific dependency, and vision specific mental health, indicating that VFL has substantial impact on mobility and ability of individuals to function independently. The smallest effect sizes were noted for the SF-12 MCS and SF-12 PCS and for the NEI-VFQ-25 general health subscale, suggesting that general health questions were less sensitive to the impact of VFL than those questions focused on vision-specific daily tasks (e.g. driving, dependency on others).
Two previous studies reported associations between glaucomatous VFL and HRQOL sub-scale scores from the 51-item National Eye Institute-Visual Functioning Questionnaire (NEI-VFQ). Gutierrez et al. noted a statistically significant negative correlation between NEI-VFQ and VFL scores (Advanced Glaucoma Intervention Study - AGIS Scores) among a clinic-based sample of 147 glaucoma patients for 7 of 11 NEI-VFQ subscales, including driving difficulties, difficulties with general vision, distance vision, dependency due to vision, difficulty with near vision, and visual limitations with social functioning, and role limitations due to vision.8 Consistent with our data, they also noted a linear decrease between NEI-VFQ and AGIS VFL scores for either the better or worse eye8. In a second study, Parrish and coworkers studied a clinic-based sample of 147 glaucoma patients from a single center and noted a moderate correlation (r2>30%) between peripheral vision, distance activities, vision-specific dependency and visual field loss using the NEI-VFQ, but only a modest correlation (10%< r2 <30%) with driving difficulties and vision-specific mental health10.
Several studies have investigated the association between VFL and questions concerning completion of daily activities such as the ability to read or watch television, issues of mobility including walking or driving, and frequency of falls. In the Rotterdam Study, a population-based study of chronic disease in 6,250 persons living in the Netherlands, Ramrattan et al. 6 examined the association between VFL and disability for 8 daily activities (dressing, rising, reaching, hygiene, eating, walking, gripping, and activity). Individuals with bilateral VFL were more likely to use a walking aid, be involved in frequent falls, and to indicate they didn’t find enjoyment in reading or watching television than individuals with no VFL. 6 In the Blue Mountains Eye Study, a population-based longitudinal study of eye disease in Australian adults, participants with decreased visual field were more likely to report two or more falls in the previous 12 months (RR=3.8; 95%CI 1.0–1.2) 7 and more likely to have a history of ankle fracture (RR 2.7; 95%CI 1.1–6.2). 33 Nelson and colleagues noted when using a 58-item visual disability questionnaire in 47 clinic-based glaucoma patients, that those with VFL experienced problems with dark adaptation, glare disability, activities related to functional peripheral vision and outdoor mobility tasks 2. In another study of 79 glaucoma patients using the Impact of Vision Impairment questionnaire, Noe and co workers determined that more than 25% of patients experienced moderate to severe restriction of mobility activities due to visual field loss34. Similarly, Mills noted in a clinic-based sample of 607 glaucoma patients from 15 clinics that there was a weak but significant relationship between the Visual Activities Questionnaire scale scores and visual field scores.9 Finally, McGwin and colleagues found that patients with glaucoma who have moderate or severe VFL in the central 24 degree radius of the worse seeing eye were more likely to be involved in a motor vehicle collision35. Findings from these studies and LALES suggest that persons with VFL experience significant decrements in HRQOL. Particularly, with regard to driving and motor vehicle collisions, our data suggest that persons with VFL begin to experience difficulty with driving activities even with mild VFL and, based on the data from McGwin et al35, these driving difficulties translate to overt collisions once VFL is moderate to severe.
Using a criteria of MD <−2 dB in the better eye we classified 25% of our LALES population as having VFL. The prevalence of VFL in two other population-based samples of Whites 40 years and older from the Netherlands and Australia ranges from approximately 3% to 17% 6,36 with the highest frequencies present in older age groups. The prevalence of VFL in LALES is higher than previously reported in the literature however the methods to determine and categorize individuals as having VFL differed for each of the three studies. It also may be reasonable to expect a high prevalence of VFL in LALES due to a higher prevalence of vision threatening diseases such as glaucoma and diabetic retinopathy in Latinos.
We observed that NEI-VFQ-25 composite scores were lower in persons with even small losses in visual field as measured by MD scores. Predicted means were calculated to be certain that patterns of HRQOL scores by MD were not impacted by differences in age or other covariates. A similar pattern was observed for the better and worse seeing eyes. However, the β coefficients (slopes) were larger for the better seeing eye compared to the worse seeing eye, indicating that loss of VFL in the better seeing eye has greater impact on HRQOL than does VFL in the worse seeing eye. The composite HRQOL scores continue to decline through approximately −30 dB for the better seeing eye, but begin to level off for the worse seeing eye. The greater loss in HRQOL associated with VFL in the better seeing eye suggests that HRQOL is driven by vision of the better seeing eye and that individuals may compensate for VFL in the worse eye with the better seeing eye. This compensatory binocular mechanism has been noted previously20 and should be considered when counseling patients with VFL.
We have previously reported the impact of visual acuity (VA) on vision-targeted HRQOL37. Similar to our findings on VFL, we noted loss in HRQOL beginning with mild levels of impairment in VA. The largest differences in NEI-VFQ-25 scores were observed when comparing individuals with bilateral moderate/severe VA impairment to individuals without impairment. However, participants with unilateral or bilateral VA impairment had significantly lower mean NEI-VFQ-25 scores (p<0.05) for most scales at any level of severity when compared to participants with VFL (data not shown). These data suggest that while both VA and VFL have significant impact on HRQOL, loss in central vision has a greater impact on HRQOL compared to VFL. This observation should also be considered and communicated to patients when discussing the impact of vision threatening eye disease on HRQOL.
A limitation of our current analysis is that we evaluated VFL based on visual field in each eye separately, rather than using a binocular visual field measure. One concern with this approach is that the area of vision loss in one eye does not necessarily overlap with the area of vision loss in the second, therefore the visual field of one eye (particularly the worse seeing eye) does not always provide an accurate description of a person’s binocular visual field 38. Another potential limitation of our study is that the models were adjusted for VA, but we did not have the data to adjust for other measures of visual function, such as contrast sensitivity, glare sensitivity, and stereoacuity; however the current assessment of visual disability by the United States Social Security Administration is based exclusively on VA and VF 38. Our conclusions are limited by the use of prevalent data; the analysis of longitudinal data that is currently being collected for LALES will allow us to examine how changes in VF for individuals over time affects HRQOL. Finally, our population-based sample of Latinos in Southern California may not be representative of the larger US population or Latinos in other parts of the United States and results obtained from this sample may not be representative of QOL issues among patients with VFL due to a single type of disease (e.g. glaucoma). However, given that similar relationships were noted in clinic-based samples of glaucoma patients from different racial/ethnic groups, it is likely that the relationship between VFL and HRQOL will be similar in persons of other racial/ethnic groups.
Findings from this study may help both patients with VFL and clinicians to be better informed about the impact of VFL on HRQOL. This assessment may help physicians and patients to weigh the risks and benefits of intervention for specific conditions considering not only the severity of VFL but also the potential impact of VFL on the patients HRQOL. These assessments may also contribute to healthcare policy and health resource allocation in terms of the potential value of an intervention (or lack of intervention) in disease management. It is likely that as more longitudinal data is collected on the impact of various interventions on vision related HRQOL, physician will need to carefully consider the impact of their management strategy, especially in diseases with progressive VFL such as optic neuropathies (Glaucoma) and retinal degenerations (Retinitis Pigmentosa).
Age-related diseases and associated vision loss will be of growing concern in the U.S. and the world over the next several decades as the proportion of adults in the oldest age groups continue to increase. While the largest differences in NEI-VFQ-25 scores were detectable for participants with bilateral, moderate/severe VFL, loss of HRQOL began with small changes in VFL as measured by MD - suggesting that early eye care management and disease prevention are critical for maintaining HRQOL. The largest impact of VFL on HRQOL scores were noted for driving difficulties and vision-specific dependency, which indicates that VFL could have a large impact on the mobility of our aging population and the ability of a growing number of older adults to live independent lives. Finally, the prevention of peripheral vision loss may help people to maintain their independence and is likely to decrease the burden of eye disease in our aging population.
Figure 5.
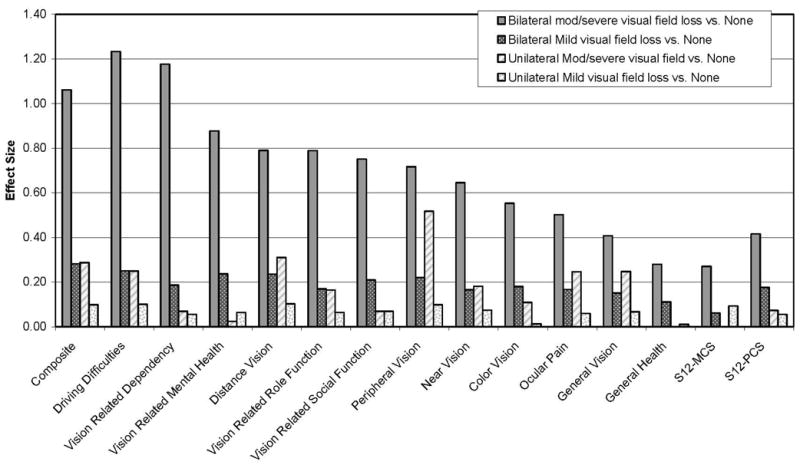
Comparison of Effect Sizes between the No Visual Field Loss Subgroup with Subgroups with Different Severity Levels of Visual Field Loss. The level of visual field loss was stratified into five categories: no VFL (MD>−2 dB in both eyes), unilateral mild VFL(−6 dB≤MD≤ −2 dB in the worse eye), unilateral moderate/severe VFL(MD<−6 dB in one eye, MD>−2 dB in the other eye), bilateral mild VFL(−6 dB≤MD≤ −2 dB in both eyes; or −6 dB ≤MD≤ −2 dB in one eye, MD<−6 dB in the other eye), and bilateral moderate/severe VFL(MD<−6 dB in the both eyes). The effect size was calculated as the difference in the adjusted mean scores (between each of the severity level of visual field loss and no visual field loss) divided by the standard deviation for the no visual field loss group. Subscales are clustered in decreasing order of effect sizes for the bilateral moderate/severe visual field loss vs. none groups, for the National Eye Institute Visual Function Questionnaire (NEI-VFQ-25) vision-related subscales, and the Medical Outcomes Study 12-ltem Short-Form Health Survey (SF-12) general health subscale scores. Effect sizes below 0.20 represent “no significant effect”. An effect size of 0.20~0.49 is considered small effect, 0.50~0.79 as medium effect, and 0.80+ as a large effect.
Acknowledgments
A. Funding/Support: Grants EY-11753 and EY-03040 from the National Eye Institute and the National Center on Minority Health and Health Disparities, National Institutes of Health, Bethesda, Maryland, and an unrestricted grant from Research to Prevent Blindness, New York, NY. Rohit Varma is a Research to Prevent Blindness Sybil B. Harrington Scholar. Ron D. Hays, Ph.D., was also supported by the UCLA/DREW Project EXPORT, National Institutes of Health, National Center on Minority Health & Health Disparities, (P20-MD00148-01) and the UCLA Center for Health Improvement in Minority Elders/Resource Centers for Minority Aging Research, National Institutes of Health, National Institute of Aging, (AG-02-004).
B. Financial Disclosures. The authors have no proprietary or commercial interest in any materials discussed in the manuscript.
C. Contributions: design and conduct of the study (RV, SA); collection, management, analysis, and interpretation of the data (RMC, RV, SA, JW, RH); and preparation, review, or approval of the manuscript (RMC, RV, SA, JW, RH).
D. Acknowledgements: The Los Angeles Latino Eye Study Group, University of Southern California, Los Angeles, CA.-Rohit Varma, MD, MPH; Sylvia H. Paz, MS; Stanley P. Azen, PhD; Lupe Cisneros, COA; Elizabeth Corona; Carolina Cuestas, OD; Denise R. Globe, PhD; Sora Hahn, MD; Mei-Ying Lai, MS; George Martinez; Susan Preston-Martin, PhD; Ronald E. Smith, MD; LaVina Tetrow, Mina Torres, MS; Natalia Uribe, OD; Jennifer Wong, MPH; Joanne Wu, MPH; Myrna Zuniga.
Battelle Survey Research Center, St. Louis, MO- Sonia Chico, BS; Lisa John, MSW; Michael Preciado, BA; Karen Tucker, MA.
Ocular Epidemiology Grading Center, University of Wisconsin, Madison, WI Ronald Klein, MD, MPH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Friedman DS, Congdon N, Kempen J, Tielsch JM. Vision Problems in the U.S., Prevalence of Adult Vision Impairment and Age-Related Eye Disease in America. Bethesda, MD: National Eye Institute; 2002. p. 1. [Google Scholar]
- 2.Nelson P, Aspinall P, O’Brien C. Patients’ perception of visual impairment in glaucoma: a pilot study. Br J Ophthalmol. 1999;83:546–52. doi: 10.1136/bjo.83.5.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sherwood MB, Garcia-Siekavizza A, Meltzer MI, Hebert A, Burns AF, McGorray S. Glaucoma’s impact on quality of life and its relation to clinical indicators. A pilot study Ophthalmology. 1998;105:561–6. doi: 10.1016/S0161-6420(98)93043-3. [DOI] [PubMed] [Google Scholar]
- 4.Klein BE, Klein R, Lee KE, Cruickshanks KJ. Performance-based and self-assessed measures of visual function as related to history of falls, hip fractures, and measured gait time. The Beaver Dam Eye Study. Ophthalmology. 1998;105:160–4. doi: 10.1016/s0161-6420(98)91911-x. [DOI] [PubMed] [Google Scholar]
- 5.McCarty CA, Nanjan MB, Taylor HR. Vision impairment predicts 5 year mortality. Br J Ophthalmol. 2001;85:322–6. doi: 10.1136/bjo.85.3.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramrattan RS, Wolfs RC, Panda-Jonas S, et al. Prevalence and causes of visual field loss in the elderly and associations with impairment in daily functioning: the Rotterdam Study. Arch Ophthalmol. 2001;119:1788–94. doi: 10.1001/archopht.119.12.1788. [DOI] [PubMed] [Google Scholar]
- 7.Ivers R, Cumming R, Mitchell P, Attebo K. Visual impairment and falls in older adults: the Blue Mountains Eye Study. J Am Geriatr Soc. 1998;46:58–64. doi: 10.1111/j.1532-5415.1998.tb01014.x. [DOI] [PubMed] [Google Scholar]
- 8.Gutierrez P, Wilson MR, Johnson C, et al. Influence of glaucomatous visual field loss on health-related quality of life. Arch Ophthalmol. 1997;115:777–84. doi: 10.1001/archopht.1997.01100150779014. [DOI] [PubMed] [Google Scholar]
- 9.Mills RP. Correlation of quality of life with clinical symptoms and signs at the time of glaucoma diagnosis. Trans Am Ophthalmol Soc. 1998;96:753–812. [PMC free article] [PubMed] [Google Scholar]
- 10.Parrish RK, 2nd, Gedde SJ, Scott IU, et al. Visual function and quality of life among patients with glaucoma. Arch Ophthalmol. 1997;115:1447–55. doi: 10.1001/archopht.1997.01100160617016. [DOI] [PubMed] [Google Scholar]
- 11.Varma R, Paz SH, Azen SP, et al. The Los Angeles Latino Eye Study: design, methods, and baseline data. Ophthalmology. 2004;111:1121–31. doi: 10.1016/j.ophtha.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 12.Globe DR, Schoua-Glusberg A, Paz S, et al. Using focus groups to develop a culturally sensitive methodology for epidemiological surveys in a Latino population: findings from the Los Angeles Latino Eye Study (LALES) Ethn Dis. 2002;12:259–66. [PubMed] [Google Scholar]
- 13.Solis JM, Marks G, Garcia M, Shelton D. Acculturation, access to care, and use of preventive services by Hispanics: findings from HHANES 1982–84. Am J Public Health. 1990;80 (Suppl):11–9. doi: 10.2105/ajph.80.suppl.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marks G, Garcia M, Solis JM. Health risk behaviors of Hispanics in the United States: findings from HHANES, 1982–84. Am J Public Health. 1990;80 (Suppl):20–6. doi: 10.2105/ajph.80.suppl.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brody BL, Gamst AC, Williams RA, et al. Depression, visual acuity, comorbidity, and disability associated with age-related macular degeneration. Ophthalmology. 2001;108:1893–900. doi: 10.1016/s0161-6420(01)00754-0. discussion 1900-1. [DOI] [PubMed] [Google Scholar]
- 16.Globe DR, Varma R, Torres M, Wu J, Klein R, Azen SP. Self-reported comorbidities and visual function in a population-based study: the Los Angeles Latino Eye Study. Arch Ophthalmol. 2005;123:815–21. doi: 10.1001/archopht.123.6.815. [DOI] [PubMed] [Google Scholar]
- 17.Linn BS, Linn MW, Gurel L. Cumulative illness rating scale. J Am Geriatr Soc. 1968;16:622–6. doi: 10.1111/j.1532-5415.1968.tb02103.x. [DOI] [PubMed] [Google Scholar]
- 18.Cello KE, Nelson-Quigg JM, Johnson CA. Frequency doubling technology perimetry for detection of glaucomatous visual field loss. Am J Ophthalmol. 2000;129:314–22. doi: 10.1016/s0002-9394(99)00414-6. [DOI] [PubMed] [Google Scholar]
- 19.Azen SP, Varma R, Preston-Martin S, Ying-Lai M, Globe D, Hahn S. Binocular visual acuity summation and inhibition in an ocular epidemiological study: the Los Angeles Latino Eye Study. Invest Ophthalmol Vis Sci. 2002;43:1742–8. [PubMed] [Google Scholar]
- 20.Varma R, Fraser-Bell S, Tan S, Klein R, Azen SP. Prevalence of age-related macular degeneration in Latinos: the Los Angeles Latino eye study. Ophthalmology. 2004;111:1288–97. doi: 10.1016/j.ophtha.2004.01.023. [DOI] [PubMed] [Google Scholar]
- 21.Varma R, Torres M, Pena F, Klein R, Azen SP. Prevalence of diabetic retinopathy in adult Latinos: the Los Angeles Latino eye study. Ophthalmology. 2004;111:1298–306. doi: 10.1016/j.ophtha.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 22.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Ware JE, Kosinski M, Keller SD. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales. 2. Boston, MA: The Health Institute, New England Medical Center; 1995. [Google Scholar]
- 24.Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD. Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2001;119:1050–8. doi: 10.1001/archopht.119.7.1050. [DOI] [PubMed] [Google Scholar]
- 25.Mangione CM, Lee PP, Pitts J, Gutierrez P, Berry S, Hays RD. Psychometric properties of the National Eye Institute Visual Function Questionnaire (NEI-VFQ). NEI-VFQ Field Test Investigators. Arch Ophthalmol. 1998;116:1496–504. doi: 10.1001/archopht.116.11.1496. [DOI] [PubMed] [Google Scholar]
- 26.Cleveland W, Grosse E. Computational Methods for Local Regression. Statistics and Computing. 1991;1:47–62. [Google Scholar]
- 27.Globe DR, Wu J, Azen SP, Varma R. The impact of visual impairment on self-reported visual functioning in Latinos: The Los Angeles Latino Eye Study. Ophthalmology. 2004;111:1141–9. doi: 10.1016/j.ophtha.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 28.Hsu JC, Nelson B. Multiple Comparisons in the General Linear Model. Journal of Computational and Graphical Statistics. 1998;7:23–41. [Google Scholar]
- 29.Hsu JC. Multiple Comparisons: Theory and Methods. London: Chapman & Hall; 1996. [Google Scholar]
- 30.Rosenthal R. Parametric measures of effect size. In: Cooper H, Hedges LV, editors. The handbook of research synthesis. New York: Russell Sage Foundation; 1994. [Google Scholar]
- 31.Lindblad AS, Clemons TE. Responsiveness of the National Eye Institute Visual Function Questionnaire to progression to advanced age-related macular degeneration, vision loss, and lens opacity: AREDS Report no. 14. Arch Ophthalmol. 2005;123:1207–14. doi: 10.1001/archopht.123.9.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 33.Ivers RQ, Cumming RG, Mitchell P, Peduto AJ. Risk factors for fractures of the wrist, shoulder and ankle: the Blue Mountains Eye Study. Osteoporos Int. 2002;13:513–8. doi: 10.1007/s001980200063. [DOI] [PubMed] [Google Scholar]
- 34.Noe G, Ferraro J, Lamoureux E, Rait J, Keeffe JE. Associations between glaucomatous visual field loss and participation in activities of daily living. Clin Experiment Ophthalmol. 2003;31:482–6. doi: 10.1046/j.1442-9071.2003.00712.x. [DOI] [PubMed] [Google Scholar]
- 35.McGwin G, Jr, Xie A, Mays A, et al. Visual field defects and the risk of motor vehicle collisions among patients with glaucoma. Invest Ophthalmol Vis Sci. 2005;46:4437–41. doi: 10.1167/iovs.05-0750. [DOI] [PubMed] [Google Scholar]
- 36.Taylor HR, Livingston PM, Stanislavsky YL, McCarty CA. Visual impairment in Australia: distance visual acuity, near vision, and visual field findings of the Melbourne Visual Impairment Project. Am J Ophthalmol. 1997;123:328–37. doi: 10.1016/s0002-9394(14)70128-x. [DOI] [PubMed] [Google Scholar]
- 37.Varma R, Wu J, Chong K, Azen SP, Hays RD. Impact of severity and bilaterality of visual impairment on health-related quality of life. Ophthalmology. 2006;113:1846–53. doi: 10.1016/j.ophtha.2006.04.028. [DOI] [PubMed] [Google Scholar]
- 38.Lennie P, Van Hemel S, editors. Visual impairments: Determining eligibility for social security benefits. Washington, DC: National Academy Press; 2002. pp. 111–25. [PubMed] [Google Scholar]


