Abstract
Rationale: Although there is a growing belief that physicians should routinely provide a recommendation to surrogates during deliberations about withdrawing life support, there is a paucity of empirical data on surrogates' perspectives on this topic.
Objectives: To understand the attitudes of surrogate decision-makers toward receiving a physician's recommendation during deliberations about whether to limit life support for an incapacitated patient.
Methods: We conducted a prospective, mixed methods study among 169 surrogate decision-makers for critically ill patients. Surrogates sequentially viewed two videos of simulated physician–surrogate discussions about whether to limit life support, which varied only by whether the physician gave a recommendation.
Measurements and Main Results: The main quantitative outcome was whether surrogates preferred to receive a physicians' recommendation. Surrogates also participated in an in-depth, semistructured interview to explore the reasons for their preference. Fifty-six percent (95/169) of surrogates preferred to receive a recommendation, 42% (70/169) preferred not to receive a recommendation, and 2% (4/169) felt that both approaches were equally acceptable. We identified four main themes that explained surrogates' preferences, including surrogates' perceptions of physicians' appropriate role in life or death decisions and their perceptions of the positive or negative consequences of a recommendation on the physician–surrogate relationship, on the decision-making process, and on long-term regret for the family.
Conclusions: There is no consensus among surrogates about whether physicians should routinely provide a recommendation regarding life support decisions for incapacitated patients. These findings suggest that physicians should ask surrogates whether they wish to receive a recommendation regarding life support decisions and should be flexible in their approach to decision-making.
Keywords: surrogate decision-making, physician recommendations, empirical ethics
AT A GLANCE COMMENTARY
Scientific Knowledge on the Subject
Multiple pulmonary and critical care professional societies recently recommended that physicians should routinely provide recommendations to surrogates about whether to limit life support.
What This Study Adds to the Field
The current study reveals that there is no consensus among surrogates about whether physicians' recommendations are desired for value-sensitive decisions about withdrawing life support. These empirical findings suggest that recent professional society guidelines may not be in line with the diverse perspectives of families in intensive care units.
Surrogate decision-making is a difficult task for family members of incapacitated patients (1–4). In intensive care units (ICUs), surrogate decision-making is the norm because critical illness and neuroactive medications often impair patients' cognition (5). Although roughly 500,000 Americans die yearly after decisions by surrogates to limit life support, there is a paucity of research about how to improve surrogate decision-making (6). There is, however, substantial evidence that the emotional needs of surrogate decision-makers are incompletely met (7), that communication between physicians and surrogates is inadequate (8–11), and that many surrogates feel ill-prepared to carry out their role (4, 12).
A particularly controversial aspect of surrogate decision-making is whether physicians should provide recommendations during deliberations about limiting life support. Many physicians are reluctant to do so, believing it is outside their professional role to make these value-based judgments (13). However, there has been a recent call for “shared decision-making” about life support in ICUs, including a recent consensus conference statement from four major European and American critical care societies (14). Under this model, physicians and surrogates share information with each other about the medical situation and the patient's values, deliberate together, and ultimately both are moral participants in making these difficult decisions (15). A physician's recommendation is one component of the larger process of shared decision-making. Despite the importance of the topic, little is known about surrogates' attitudes toward receiving recommendations from physicians about whether to withdraw life support. The absence of these data poses a barrier to designing empirically derived interventions to improve surrogate decision-making.
We conducted a prospective study using quantitative and qualitative methods to examine surrogates' attitudes toward receiving a physician's recommendation to limit life support for an incapacitated, critically ill patient.
METHODS
We conducted a prospective, mixed methods study using video recordings of a simulated ICU family conference to elicit surrogates' views about physicians' recommendations for value-laden life-support decisions. Between July 2007 and April 2008, we enrolled subjects from four ICUs at the University of California, San Francisco Medical Center. The ICUs included two medical-surgical ICUs, a neurological ICU, and a cardiac ICU. Eligible subjects were the surrogates of any critically ill patient who were at least 18 years old and who spoke English well enough not to require the use of an interpreter. We excluded family members and friends who visited the patient in the hospital but were not centrally involved in surrogate decision-making. The Institutional Review Board at the University of California, San Francisco Medical Center approved all study procedures. A study coordinator screened for subjects daily by identifying family members present in the waiting room of each ICU or at the patient's bedside. To ensure that surrogates' work schedules or other factors did not result in a biased sample, the coordinator screened surrogates at different times of the day, including early and late in the day when many surrogates who work come to the hospital, and followed a systematic protocol to identify surrogate decision-makers for each patient. Before approaching a potential subject, the study coordinator contacted the attending physician for permission to do so. All participants provided written consent.
Development and Content of the Video
The videos were developed through extensive collaboration with experts in bioethics, critical care medicine, palliative care medicine, and sociology. We sought to create an ICU family conference that addressed a common “type” of life support decision: a patient with a small chance of short-term survival but a high likelihood of substantial functional impairment, including ventilator dependence. Similarly, we sought to create the most common conditions of knowledge about the patient's values: a patient who lacks an advance directive but who has previously spoken informally with family about treatment preferences. The interaction followed the conceptual model of decision-making described by Charles and colleagues (15). We “created” a physician who was empathic and adhered to recent evidence about quality communication in ICUs (11, 16–22). The video was divided into two segments. In the first segment, the physician explained the medical scenario, expressed empathy, explained principles of surrogate decision-making, discussed the patient's prognosis, asked a series of questions to elicit information about the patient's values, and explained the treatment options (Appendixes I and II in the online supplement). This portion of the video ended with the surrogate asking who should make the decision about whether to withdraw life support. We created two endings to the video, which varied only by whether the physician provided a recommendation. The two endings were similar in length, proportion of physician speech, and emotional support from the physician (Table 1). To minimize the chance that nonverbal cues resulted in subtle differences in the two video endings, we used the same video clips except for the portions of speech in which the physician provided (or did not provide) a recommendation.
TABLE 1.
TRANSCRIPTS OF TWO ENDINGS TO AN ICU FAMILY CONFERENCE
| Ending A: Physician Does Not Provide a Recommendation |
| MD: Well, this is a decision that you should make, Ms. Smith. I mean, my job is to give you all the information about the various choices so that you can make an informed decision. You should use the information to make the decision that you think your father would make, if he could speak for himself. |
| Daughter: Okay, uhm, what would you do if you had to make this decision? |
| MD: Well, it's a very individual decision, and it's not my role to make a recommendation for you. I can help you understand the various options, but you need to decide what your father would want in this situation. |
| Daughter: This is definitely the hardest decision I've ever had to make. He was so independent. I just don't think he would want this. |
| MD: You're right; it is a tough decision for you. Again, remember though, that the most important thing is for you to make the choice that your father would have made if he could speak for himself. Or make the choice that's most consistent with his values. We rely on you to make this decision, and it should be right for him. |
| Daughter: Well, I don't think dad would want to continue like this. But, I'm not ready to make this decision yet. I think I need some more time to think about it. Is that OK? |
| MD: Sure, you don't have to decide right now. I'll be available to talk with you about it if you want anytime. |
| Daughter: Okay, thank you. |
| Ending B: Physician Provides a Recommendation |
| MD: Well Ms. Smith, this is a decision we should make together. My job is not only to give you all the information about the various choices, but also help you decide which is most consistent with what your father would have wanted. |
| Daughter: Yeah. So, what would you do if you had to make this decision? |
| MD: Well, it's a very individual decision. Based on what you've told me so far, it sounds like your father was someone who really valued his independence and would not want to end up in a nursing home. Does that sound right to you? |
| Daughter: Yeah, I think it does. I mean, I don't think he would have wanted all this but it's just such a hard decision. I don't think he would have wanted this… he's so independent. |
| MD: Yes, this is a very tough decision. But, based on what you've said about your father as a person, I really think that he wouldn't want to continue with treatment if it meant ending up in a nursing home. I know this is hard to hear, but I would recommend that we focus on keeping him comfortable and recognize that trying to get him well enough to go to a nursing home is not what he would have wanted. [SHORT PAUSE] What do you think about what I've said? |
| Daughter: I don't think, I don't think dad would want to continue like this. But, I'm not ready to make this decision yet. I think I need some more time to think about it. OK? |
| MD: Sure, we don't have to decide right now. I'll be available to talk with you about it if you want anytime. |
| Daughter: Okay, thank you. |
Data Collection
Before viewing the video, surrogates completed a questionnaire addressing their demographic characteristics in a private room adjacent to the ICU. Surrogates then read a brief introductory statement about the hypothethical patient's clinical course before the family meeting depicted in the video (Appendix I). Next, they viewed the first segment of the video, then viewed the two endings sequentially. We randomized the order in which surrogates viewed the endings. After viewing the video, surrogates were asked which ending they preferred. Then, using techniques of cognitive interviewing, we asked surrogates to explain their choice. These interviews were audiotaped and transcribed. The main data for this project were the binary outcome of which ending the surrogate preferred, as well as the surrogates' qualitative explanations for their choice.
Qualitative Data Coding
The audiotaped interviews were transcribed verbatim by a medical transcriptionist. We used constant comparative methods to inductively develop a framework to describe participants' attitudes about receiving a physician's recommendation. Constant comparative methods are a general methodology for inductively analyzing systematically gathered qualitative data. The method is most useful when existing conceptual frameworks for the topics under study are inadequate (23–25).
To develop the preliminary coding scheme, four investigators independently coded a subset of transcripts line by line. We identified recurrent themes relating to surrogates' attitudes about physicians' recommendations. As themes and concepts accumulated, we refined distinctions between concepts and then grouped similar concepts into conceptual categories. These categories were developed further by comparing across transcripts. All investigators collaborated on developing the preliminary framework and, through a series of investigator meetings, arrived at consensus on the final coding framework. We modified the framework iteratively over the study period as interviews yielded new insights.
Reliability of the Coding
Using the final coding framework, two investigators independently coded all interviews by listening to the audiotapes and reading the transcripts. Both coders were blinded to the demographic characteristics of the subjects and to one another's coding. To assess intercoder reliability, we calculated a kappa statistic on a random sample of 20% of interviews. The average kappa statistic for identifying individual themes within an interview was 0.82 (range, 0.71–0.89). A kappa value greater than 0.8 represents excellent interrater reliability (26). All discrepancies between coders were reviewed and resolved through dialogue between the coders, involving coauthors as needed.
Validity of the Findings
We used two techniques to ensure the validity of our findings (27, 28). First, we used a multidisciplinary approach in developing the coding framework. Areas of investigator expertise included critical care medicine, bioethics, doctor–patient communication, and ethnic studies. A multidisciplinary approach minimizes the chance that individual bias threatens the validity of the findings. Second, we presented the preliminary conceptual framework to a sample of study subjects for confirmation and/or modification, a process known as member checking (28). These insights were incorporated into the final organizing framework for the data.
RESULTS
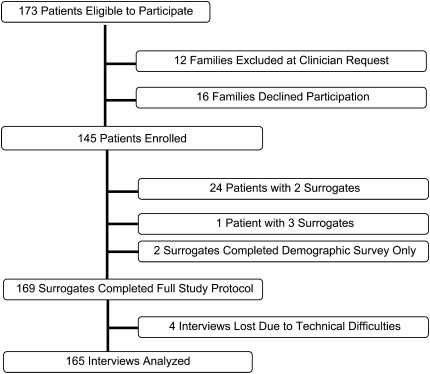
Among 173 eligible patients, 12 (7%) were not enrolled at the request of the attending physician, and 16 (9%) surrogates declined to participate after learning about the study. The overall enrollment rate was 84% (Figure 1). In some cases, a family indicated that more than one individual would be involved in surrogate decision-making; therefore, for 24 patients, two surrogates were enrolled, and for one patient three surrogates were enrolled (n = 171 surrogates). Of the 171 surrogates enrolled, two participants completed demographic information only. A total of 169 surrogates completed the full study protocol of viewing the videos and completing both demographic and postvideo questionnaires. Four interviews could not be analyzed due to technical problems with audiorecording; therefore, 165 interviews were included in the qualitative analyses.
Figure 1.
Flow diagram describing the enrollment of surrogates.
The demographic characteristics of the patients and surrogate decision-makers who participated in the study are shown in Table 2 and Table 3, respectively. The sample was diverse in terms of gender, race, ethnicity, religious affiliation, and level of education.
TABLE 2.
DEMOGRAPHIC CHARACTERISTICS OF PATIENTS
| Patient Characteristics | Enrolled (N = 145) |
|---|---|
| Male, n (%) | 73 (50) |
| Age, mean (SD) | 58 (15.6) |
| Race*, n (%) | |
| White | 100 (69) |
| Hispanic | 23 (16) |
| Multiethnic | 18 (12) |
| Asian/Pacific Islander | 13 (9) |
| Black | 8 (6) |
| Native American | 1 (1) |
| Admission diagnosis, n (%) | |
| Neurological failure | 57 (39) |
| Cardiac failure or shock (including sepsis) | 19 (13) |
| Hepatic failure | 12 (8) |
| Trauma | 11 (8) |
| Metastatic cancer | 11 (8) |
| Respiratory failure | 10 (7) |
| Gastrointestinal failure | 9 (6) |
| Renal failure | 6 (4) |
| Missing data/not available | 10 (7) |
Sums are greater than n = 145 Enrolled Patients because some individuals identified with more than one race/ethnicity.
TABLE 3.
DEMOGRAPHIC CHARACTERISTICS OF SURROGATE DECISION-MAKERS (N = 169)
| Characteristics of Surrogate Decision-Makers | n (%) | |
|---|---|---|
| Gender | ||
| Female | 94 (56) | |
| Race/ethnicity* | ||
| White | 116 (69) | |
| Hispanic | 28 (17) | |
| Multiethnic | 20 (12) | |
| Asian/Pacific Islander | 15 (9) | |
| African-American | 9 (5) | |
| No response/Did not know | 5 (3) | |
| Native American | 3 (2) | |
| Relationship to patient | ||
| Spouse/partner | 66 (39) | |
| Child | 45 (27) | |
| Parent | 23 (13) | |
| Sibling | 20 (12) | |
| Other | 13 (8) | |
| Friend | 2 (1) | |
| Level of education | ||
| Some college or all college | 85 (50) | |
| Graduate or professional school | 43 (25) | |
| Some high school (incl. diploma or GED) | 40 (24) | |
| No response | 1 (1) | |
| Primary language | ||
| English | 153 (91) | |
| Spanish | 9 (5) | |
| Other† | 7 (4) | |
| Religious preference | ||
| Protestant | 59 (35) | |
| Catholic | 41 (24) | |
| None/agnostic/atheist | 38 (22) | |
| No response | 13 (8) | |
| Other Christian (Latter Day Saints/Mormons, Jehovah's Witness) | 6 (4) | |
| Buddhist | 4 (2) | |
| Jewish | 3 (2) | |
| Other (including Wiccan) | 2 (1) | |
| Hindu | 2 (1) | |
| Islam | 1 (1) | |
| Importance of religion/spiritual beliefs in everyday life | ||
| Very important | 77 (45) | |
| Fairly important | 37 (22) | |
| Not too important | 33 (20) | |
| Declined response | 17 (10) | |
| Not at all important | 5 (3) | |
Sums are greater than n = 169 family members because some individuals identified with more than one race/ethnicity.
Includes Cantonese, Korean, Russian, Asian Indian, and “unspecified.”
Overall, 56% (95/169) of surrogates preferred to receive a recommendation from the physician about whether to limit life support, 42% (70/169) preferred to not receive a recommendation, and 2% (4/169) felt both approaches were acceptable. We found no correlation between surrogates' demographic characteristics and their preference for receiving a recommendation.
Four main themes explained surrogates' preferences. These included surrogates' beliefs about what role is appropriate for physicians and surrogates in life or death decisions, their perceptions of the consequences of a recommendation on the physician-surrogate relationship, their beliefs about the decision-making process, and and their beliefs about long-term regret for the family.
The Appropriate Roles of the Physician and the Surrogate
Among the surrogates who preferred to receive a physician's recommendation, 51% (48/95) expressed that providing such a recommendation is a central part of the physicians' role. The 50-year-old brother of a patient with a mitral valve rupture explained, “[The doctor is] really leaning on my appreciation of the patient…but I'm also leaning on the doctor, with his background and experience.” Some surrogates expressed that a physician's unwillingness to offer a recommendation amounted to a “denial of responsibility to help in the process.”
In contrast, 79% of surrogates who preferred that the physician refrain from giving a recommendation expressed that doing so was beyond the appropriate role for physicians. For these surrogates, “it didn't seem appropriate” for a physician to lead surrogates toward a particular choice. One 59-year-old man said that a recommendation was not welcome because “I don't want to be led…into terminating my mom's life. I'll decide.” In addition, some believed that a physician could not know enough about a patient's life or values to make a meaningful recommendation. The surrogate of a man with liver failure put it this way: “The simple fact is a doctor cannot give you that kind of information…in no way do I believe that he can, at any point in time, assume in any way that he knows…he knows anything about the person, except for the medical condition and the outcome.”
A few surrogates objected to the provision of a recommendation in the video because the physician had never directly spoken to the patient and had no prior knowledge of the patient. As one surrogate explained, the surrogate “would be the one who would really have the information towards what the patient's desires would be, not the doctor.”
Several surrogates expressed a belief that physicians should enforce the family's responsibility to decide. For example, one surrogate expressed a belief that even if a surrogate asks for a recommendation, the physician should say “I am here to explain your options, but you need to make that decision for yourself.” Another wanted the physician “to put it back on [the surrogate], so that [the doctor] had no part in the decision-making.”
Consequences of a Recommendation on Emotional Experience and Physician–Family Relationship
The vast majority of surrogates (92% [87/95]) who preferred to receive a physician's recommendation mentioned at least one positive consequence the recommendation would have on the physician-surrogate relationship, the decision making process, or the families' long-term psychological well being. For some, receiving a recommendation “took some pressure off” families and meant that “the burden of the final decision isn't completely on the surrogate.” For others, a physician who offers a recommendation seems more “engaged,” “intelligent,” “concerned,” “communicative,” and “human.” One explained that by offering a recommendation, the “doctor gave 'em his mind,” whereas not offering a recommendation meant “the doctor didn't give her anything.” A few felt that by offering a recommendation, a physician seemed “more trustworthy.”
Conversely, 37% (26/70) of surrogates who did not want a recommendation believed that a recommendation would result in significant negative consequences on the physician–surrogate relationship or the surrogate's emotional experience. For example, one surrogate stated that a recommendation might make the process more difficult because “dealing with the recommendation…actually may have been harder,” particularly if the surrogate disagreed with the physician. One 62-year-old woman felt that a recommendation “diminished respect” for the family's intelligence and knowledge. Also, a few surrogates worried that families might “blame” the physician in the future if they later felt that limiting life support was the wrong decision.
Consequences of a Recommendation on the Decision-making Process
Forty-seven percent (45/95) of surrogates who preferred to receive a physician's recommendation felt that a recommendation would improve the quality of the decision-making process and lead to better substantive decisions. Some surrogates expressed that a recommendation would help them deliberate and come to the best, most informed decision through hearing the “perspective of someone with medical experience.” Said one surrogate, “the doctor is the expert on the end of life…and I think it's sensible to get an expert's opinion.” Others felt that although a recommendation was helpful, it was not binding: “His opinion would matter, since he was a doctor. But as far as making the decision though, I'd imagine it would lie with the family.”
Other surrogates appreciated the “emotional distance” of physicians, who could provide an objective, less “emotionally conflicted” view of the situation. These surrogates felt that a recommendation improved deliberation by providing “structure” for the process and also gave surrogates the “emotional permission” to consider limiting life support. The son of a woman with heart failure felt a recommendation served “just to assure you that it's not a bad thing to decide to…take him off a breather.” Also, several surrogates in this group believed that if physicians did not provide a recommendation, families may be unable to make the decision they knew to be correct for the patient.
In contrast, for surrogates who preferred that physicians not provide a recommendation, a prevalent concern was that a recommendation could hinder or impair the family's ability to come to the best decision. One surrogate stated that a recommendation did not give “the chance…for the family member to think.” The son of a 77-year-old woman with meningococcemia said, of the vignette in which the recommendation was offered: “I was kind of surprised that the daughter had the emotional strength…to say, ‘I don't feel comfortable making this decision right now.’ The more natural flow, I think, would've been for the daughter to have made the decision, whether she was comfortable with it or not.”
The surrogate of an elderly man with an aortic aneurysm explained that due to the authority of the physician, “Sometimes we don't listen to what we really feel. We'll just take their decision.”
Consequences of Recommendation for a Family's Future and Psychological Well-being
Five percent of surrogates (5/95) who preferred to receive a physician's recommendation believed that the potential for regret over a life support decision might be lessened if the physician offers a recommendation as part of the decision-making process. One surrogate put it bluntly: “[The doctor] helped me, showed in my mind, I'm not the one who's killin' her…and I would, in the long run, feel lots better.”
Conversely, 11% (8/70) of surrogates who did not want to receive a recommendation worried that families who followed a physician's recommendation to limit life support might regret the decision in the future, particularly if they felt that they were improperly influenced. One surrogate explained, “If you have someone swaying you…sometimes you'll make a decision based on what someone else is feeling and what they're saying. And then later, you have regrets.”
Other Findings
Several surrogates emphasized that the timing of giving a recommendation to limit life support is critically important. The spouse of a man with cirrhosis suggested: “Don't offer an opinion, give her a chance to assess what's really happening. Let it sink in and give her a couple o' days to just really figure out what's going on. And then come back and talk to her more.” A few surrogates who did not wish to receive the physicians' recommendation articulated that, if the doctor had a longstanding relationship with the patient, then a recommendation might be appropriate.
DISCUSSION
We found substantial variability in surrogates' preferences for receiving a physician's recommendation for value-laden decisions about withdrawing life support. The main qualitative explanations for this variability were differing interpretations of role responsibilities for physicians and surrogates and differing beliefs about the positive or negative consequences of a recommendation from physicians. These empirical findings suggest that recent professional society guidelines advocating that physicians should routinely provide recommendations during deliberations about withdrawing life support may not be in line with the diverse perspectives of families (14).
The finding that a relatively large proportion of surrogates do not wish to receive a physician's recommendation differs from a prior study conducted in ICUs by Heyland and colleagues (29). They found that less than 1% of surrogates wished to make medical decisions without advice from physicians. Several key methodological differences may explain this difference. First, Heyland and colleagues asked surrogates about ICU decision-making in general. Without clarifying the extent to which they were asking about largely biomedical decisions (i.e., which antibiotic should be used to treat a pneumonia) versus value-based decisions (i.e., whether chronic ventilator dependence is worse than death), it is difficult to know whether their data apply to the value-based life support decisions we studied. We purposefully create a life-support decision in which the decision hinges largely on patients' values rather than medical facts (i.e., reasonable patients differ in their preferences about whether to continue life support). We chose this approach because in our experience, most decisions about whether to limit life support in ICUs hinge on patients' values about the acceptability of aggressive treatment when the likely outcome is living with severe disabilities or prolonged dependence on life support. In addition, we speculate that our use of a video allowed surrogates to see and hear the physician–surrogate interaction (rather than read about it), which may have helped surrogates more accurately imagine how they would feel about receiving or not receiving a recommendation from physicians.
What are the normative ethical implications of our empirical findings? If one accepts—as we do—that physicians have an ethical obligation to respond to surrogates' individual needs for information and advice, then our data suggest that recent professional society recommendations are insufficient because they advocate a single approach to decision-making. Instead, we propose that the emphasis should be shifted away from teaching a single model of decision-making toward training physicians to be flexible in their approach. This requires that physicians develop skills to recognize and respond to the unique needs of surrogates facing value-laden life support decisions. A more recent document on end of life care in ICUs supports this approach (30).
An important consideration regarding our findings is that surrogates' preferences are but one piece of the ethical argument for what role physicians should play in decision-making for incapacitated patients. We believe that physicians' strongest ethical obligation is to ensure that decisions are made in accordance with patients' values. Therefore, in circumstances in which surrogates do not want a recommendation from physicians but appear to be unable or unwilling to act in accord with the patient's values, we believe the physician has a duty to make a recommendation and take other steps to ensure that decisions reflect the patient's values and preferences.
This study has several strengths. The sample size is large and diverse for a mixed methods study. The integration of quantitative and qualitative methods allows us to not only quantify surrogates' preferences regarding a physician's recommendation but also to understand the reasons for their preferences. The resulting data illustrate the complex considerations in a much richer way than is possible with quantitative data alone. The use of video to help surrogates see the differences in physicians' potential roles is a novel methodological advance in the study of surrogate decision making. We took a number of steps to ensure that the two video vignettes were identical except for the presence or absence of a recommendation, including review by a panel of leading ethicists, intensivists, and palliative care physicians. The use of an inductive approach to data analysis allowed us to create a framework that emerged from the data, which is especially important in a hypothesis generating study such as this. The multidisciplinary group of investigators enhances the validity of the coding framework. The use of member checking near the end of the study allowed us to refine our coding framework based on the feedback of study participants.
This study also has several limitations. We used video recordings to illustrate two different approaches to the physician's role in surrogate decision-making. Although we believe this is an improvement over prior questionnaire-based efforts, it is possible that surrogates' stated preferences could differ in actual clinical situations. The study was conducted in one region of the United States and therefore may not be generalizable to areas in which there are different cultural perspectives on the physician–family relationship. Because we did not gather detailed information about the patients' clinical condition, we do not know how closely the scenario in the video compared with the surrogates' actual experiences in the ICU and therefore could not assess whether their ICU experiences affected their reactions to the videos. However, a large number of surrogates commented that the videos were realistic, compelling, and for some, emotionally moving. We cannot exclude the possibility that surrogates' responses reflected their attitudes about withdrawing life support in their loved ones' current situation rather than their attitudes about the scenario depicted in the video. We reviewed all transcripts looking for evidence of this type of “transference” and found none. Nonetheless, the possibility remains that the effect was subconscious. In the medical encounter we developed, the physician and patient did not have a pre-existing relationship. Although this is the norm in intensive care units, these results may not apply to situations in which the physician and patient have had a longitudinal relationship. Finally, we studied only one “type” of life support decision: a patient with a small chance of survival and high likelihood of functional impairment who has made some prior statements about his treatment preferences. Although this is a very common situation in ICUs, future studies should address the extent to which surrogate's preferences for a recommendation differ by the medical condition and prognosis, the nature of the clinical decision (e.g., withholding versus withdrawing life support), the demographic characteristics of family members and physicians, and the clarity of the information about the patient's values.
This study contributes new empirical data to the ethical debate on whether physicians should routinely provide recommendations to surrogates during the process of making value-laden life support decisions in ICUs. Our findings reveal that surrogates' views are heterogeneous, with a substantial minority preferring not to receive a recommendation from physicians. To best meet surrogates' needs, we recommend that physicians ask surrogates whether they would like to hear the physician's recommendation and view the recommendation as a starting point for shared deliberations about how to act for the good of the patient.
Supplementary Material
Supported by a Greenwall Foundation Faculty Scholars Award and National Institutes of Health (NIH) grant KL2 RR024130 from the National Center for Research Resources (NCRR), a component of the NIH Roadmap for Medical Research (D.B.W.); by the Greenwall Foundation (B.L.); and by the UCSF School of Medicine Student Research Grant (C.A.B.).
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Originally Published in Press as DOI: 10.1164/rccm.200811-1776OC on June 4, 2009
Conflict of Interest Statement: D.B.W. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. L.R.E. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. C.A.B. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. J.M.L. received more than $100,001 as an expert witness for multiple law firms. B.L. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
References
- 1.Braun UK, Beyth RJ, Ford ME, McCullough LB. Voices of African American, Caucasian, and Hispanic surrogates on the burdens of end-of-life decision making. J Gen Intern Med 2008;23:267–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vig EK, Starks H, Taylor JS, Hopley EK, Fryer-Edwards K. Surviving surrogate decision-making: what helps and hampers the experience of making medical decisions for others. J Gen Intern Med 2007;22:1274–1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tilden VP, Tolle SW, Garland MJ, Nelson CA. Decisions about life-sustaining treatment: impact of physicians' behaviors on the family. Arch Intern Med 1995;155:633–638. [PubMed] [Google Scholar]
- 4.Tilden VP, Tolle SW, Nelson CA, Fields J. Family decision-making to withdraw life-sustaining treatments from hospitalized patients. Nurs Res 2001;50:105–115. [DOI] [PubMed] [Google Scholar]
- 5.Prendergast TJ, Claessens MT, Luce JM. A national survey of end-of-life care for critically ill patients. Am J Respir Crit Care Med 1998;158:1163–1167. [DOI] [PubMed] [Google Scholar]
- 6.Angus DC, Barnato AE, Linde-Zwirble WT, Weissfeld LA, Watson RS, Rickert T, Rubenfeld GD. Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med 2004;32:638–643. [DOI] [PubMed] [Google Scholar]
- 7.Kirchhoff KT, Walker L, Hutton A, Spuhler V, Cole BV, Clemmer T. The vortex: families' experiences with death in the intensive care unit. Am J Crit Care 2002;11:200–209. [PubMed] [Google Scholar]
- 8.Azoulay E, Chevret S, Leleu G, Pochard F, Barboteu M, Adrie C, Canoui P, Le Gall JR, Schlemmer B. Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med 2000;28:3044–3049. [DOI] [PubMed] [Google Scholar]
- 9.White DB, Braddock CH III, Bereknyei S, Curtis JR. Toward shared decision making at the end of life in intensive care units: opportunities for improvement. Arch Intern Med 2007;167:461–467. [DOI] [PubMed] [Google Scholar]
- 10.White DB, Engelberg RA, Wenrich MD, Lo B, Curtis JR. The language of prognostication in intensive care units. Med Decis Making (In press). [DOI] [PMC free article] [PubMed]
- 11.White DB, Engelberg RA, Wenrich MD, Lo B, Curtis JR. Prognostication during physician-family discussions about limiting life support in intensive care units. Crit Care Med 2007;35:442–448. [DOI] [PubMed] [Google Scholar]
- 12.Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, Adrie C, Annane D, Bleichner G, Bollaert PE, Darmon M, et al. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med 2005;171:987–994. [DOI] [PubMed] [Google Scholar]
- 13.Johnston SC, Pfeifer MP. Patient and physician roles in end-of-life decision making. J Gen Intern Med 1998;13:43–45. [DOI] [PubMed] [Google Scholar]
- 14.Thompson BT, Cox PN, Antonelli M, Carlet JM, Cassell J, Hill NS, Hinds CJ, Pimentel JM, Reinhart K, Thijs LG. Challenges in end-of-life care in the ICU: statement of the 5th International Consensus Conference in Critical Care: Brussels, Belgium, April 2003: executive summary. Crit Care Med 2004;32:1781–1784. [DOI] [PubMed] [Google Scholar]
- 15.Charles C, Whelan T, Gafni A. What do we mean by partnership in making decisions about treatment? BMJ 1999;319:780–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Curtis JR, Engelberg RA, Wenrich MD, Nielsen EL, Shannon SE, Treece PD, Tonelli MR, Patrick DL, Robins LS, McGrath BB, et al. Studying communication about end-of-life care during the ICU family conference: development of a framework. J Crit Care 2002;17:147–160. [DOI] [PubMed] [Google Scholar]
- 17.Curtis JR, Engelberg RA, Wenrich MD, Shannon SE, Treece PD, Rubenfeld GD. Missed opportunities during family conferences about end-of-life care in the intensive care unit. Am J Respir Crit Care Med 2005;171:844–849. [DOI] [PubMed] [Google Scholar]
- 18.Curtis JR, Patrick DL, Shannon SE, Treece PD, Engelberg RA, Rubenfeld GD. The family conference as a focus to improve communication about end-of-life care in the intensive care unit: opportunities for improvement. Crit Care Med 2001;29(2, Suppl):N26–N33. [DOI] [PubMed] [Google Scholar]
- 19.Curtis JR, Wenrich MD, Carline JD, Shannon SE, Ambrozy DM, Ramsey PG. Understanding physicians' skills at providing end-of-life care perspectives of patients, families, and health care workers. J Gen Intern Med 2001;16:41–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stapleton RD, Engelberg RA, Wenrich MD, Goss CH, Curtis JR. Clinician statements and family satisfaction with family conferences in the intensive care unit. Crit Care Med 2006;34:1679–1685. [DOI] [PubMed] [Google Scholar]
- 21.White DB, Curtis JR. Establishing an evidence base for physician-family communication and shared decision making in the intensive care unit. Crit Care Med 2006;34:2500–2501. [DOI] [PubMed] [Google Scholar]
- 22.Lautrette A, Darmon M, Megarbane B, Joly LM, Chevret S, Adrie C, Barnoud D, Bleichner G, Bruel C, Choukroun G, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med 2007;356:469–478. [DOI] [PubMed] [Google Scholar]
- 23.Strauss AL, Corbin J. basics of qualitative research: techniques and procedures for developing grounded theory. Thousand Oaks, CA: Sage Publications; 1998.
- 24.Glaser BG, Strauss AL. Discovery of Grounded Theory. Chicago, IL: Adline Publishing Company; 1967.
- 25.Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis. Thousand Oaks, CA: Sage Publications; 2006.
- 26.Sackett DL, Haynes RB, Guyatt GH, Tugwell P. Clinical epidemiology: a basic science for clinical medicine, 2nd ed. Boston, MA: Little, Brown and Company; 1991.
- 27.Patton MQ. Enhancing the quality and credibility of qualitative analysis. Health Serv Res 1999;34:1189–1208. [PMC free article] [PubMed] [Google Scholar]
- 28.Giacomini MK, Cook DJ. Users' guides to the medical literature: XXIII. Qualitative research in health care A. Are the results of the study valid? Evidence-Based Medicine Working Group. JAMA 2000;284:357–362. [DOI] [PubMed] [Google Scholar]
- 29.Heyland DK, Cook DJ, Rocker GM, Dodek PM, Kutsogiannis DJ, Peters S, Tranmer JE, O'Callaghan CJ. Decision-making in the ICU: perspectives of the substitute decision-maker. Intensive Care Med 2003;29:75–82. [DOI] [PubMed] [Google Scholar]
- 30.Truog RD, Campbell ML, Curtis JR, Haas CE, Luce JM, Rubenfeld GD, Rushton CH, Kaufman DC, American Academy of Critical Care Medicine. Recommendations for end-of-life care in the intensive care unit: a consensus statement by the American College [corrected] of Critical Care Medicine. Crit Care Med 2008;36:953–963. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.