Abstract
Regional variation in health care use may stem, in part, from the fact that patients in high-utilization regions demand and receive more-intensive care. We examine the association between patients’ care-seeking preferences and use of services, using a national survey of Medicare patients. Patients’ preferences, in addition to health and socio-demographic characteristics, are associated with differences in individuals’ use of office visits. However, we find that patients’ preferences for seeking primary and specialty medical care do not play a significant role in explaining regional variation in health care use.
Health care use varies widely across the United States.1 Medicare beneficiaries in some regions receive much more intensive health care, including more office visits, greater use of specialists, more tests, and more hospital-based care than beneficiaries in other areas of the country. Not surprisingly, Medicare spending per beneficiary in 2005 (adjusted for age, race, sex, health status, and price) ranged from $5,358 in Salem, Oregon, to more than $14,000 in Miami, Florida.2 What is surprising is that patients’ health and demographic differences do not appear to account for much of the variation. 3 Given that regions with higher utilization rates have a greater supply of specialists, hospital and intensive care unit (ICU) beds, and other technologies than regions with lower rates, some have argued that the supply of medical resources, not medical necessity, accounts for variation in use among the Medicare population.4
Much of the work on regional variation has focused on either the demand-side factors of health status and sociodemographic characteristics, or the supply-side factors of supplier-induced demand and practice-style variations. 5 However, as noted by John Bertko, understanding variations in use also requires measuring the role of patients’ preferences for care.6 If patients in some regions of the country prefer to see more specialists, to be treated in an intensive care unit (ICU), and to undergo more diagnostic testing, then specialists and hospital beds have tended to migrate toward regions where patients demand the most intensive care, and providers’ practice rates in these areas may simply be a response to high levels of patient demand.7
Patients’ preferences for care seeking and their expectations about health care services may stem both from a desire for information or psychosocial support and from more specific expectations for particular tests or treatments. 8 Such expectations and preferences have been shown to affect utilization both directly and indirectly through doctor-patient communication and patients’ compliance and satisfaction, but it is unclear whether patients’ care-seeking preferences vary regionally or contribute to regional variation in utilization.9 Although the importance of patients’ preferences to high-quality care is widely recognized, only a few studies have looked at the relationship between those preferences and regional variations in utilization.10 A positive association between patients’ preferences and regional utilization levels could be both cause and effect of system characteristics. That is, not only might differences in patients’ preferences lead to higher utilization patterns, but also, since patients in high-utilization regions encounter a system much more likely to provide tests and specialty care, it would not be surprising for such patients to come to prefer high levels of tests and visits. Cross-sectional data cannot tease apart this chicken-and-egg problem, but a better understanding of the role of patients’ preferences in utilization may help to better evaluate the potential impact of policy recommendations that target patients’ utilization behavior versus provider-side actions.
In this paper we use survey data from a national sample of elderly Medicare beneficiaries in the United States to examine whether and how patients’ care-seeking preferences are associated with their use of physician visits, and to what extent differences in preferences can account for regional utilization patterns. We also explore whether patients’ perceptions of unmet need vary across regions.
Study Data And Methods
Data
The national random survey of patients’ preferences for care in general and under specific conditions (n = 2,515, 65 percent response rate) is part of a larger project funded by the National Institute on Aging (NIA) to understand the causes and consequences of regional variation in Medicare utilization patterns. The Center for Survey Research (CSR) at the University of Massachusetts, Boston, implemented the dual-mode survey (telephone followed by a mailed questionnaire to all for whom a telephone number could not be obtained or who had not responded by telephone) between June and December 2005 from a national random sample of 4,000 community-dwelling Medicare beneficiaries obtained from the Centers for Medicare and Medicaid Services (CMS). A more complete description of the survey development and implementation is available elsewhere.11
Individual utilization
Respondents’ utilization is based on actual outpatient physician visits as billed for in the Medicare claims data, averaged over a two-year billing period (2004–2005). Because claims data for beneficiaries with Medicare managed care are typically incomplete, we dropped the 481 respondents with managed care from the analyses reported below. (Retaining managed care beneficiaries in the analyses, with or without an indicator variable for managed care status, does not change the results reported.)
Care-seeking preferences
To learn about patients’ primary care-seeking preferences, two clinical vignettes were used: whether the respondent would seek medical care because of new chest pain when walking up stairs, or because of a residual cough that remained after the flu (the exact wordings are shown in online Appendix Exhibit 1).12 We chose these clinical scenarios because most patients have experience with these symptoms or could easily imagine them, and because the need for immediate evaluation is uncertain. For each of the vignettes, respondents were asked whether they would want to see a doctor right away or wait, whether they would want a test or not (even if their doctor said they did not need one), and finally, whether they would want to see a specialist or not. We created three preference items based on “yes” responses to the questions in both of the vignettes: preference for seeing a doctor right away, in which respondents indicated they would want a doctor visit right away for both chest pain and cough; preference for tests; and preference for specialist visits, measured in the same way.13 Finally, respondents were asked their preference for primary versus specialty providers: did they think it was better to have one general physician to provide primary care or to have several specialist physicians?14 We coded the variable as 1 if respondents preferred a specialist as their primary provider, and as 0 otherwise. Summary statistics for all variables are shown in Exhibit 1.
EXHIBIT 1.
Characteristics Of A Sample Of Elderly Medicare Beneficiaries, 2005
| Characteristic | Total |
|---|---|
| Percent female | 57.8% |
| Age (years) | |
| 65–74 | 49.4 |
| 75–84 | 40.8 |
| 85+ | 9.8 |
| Race/ethnicity | |
| Non-Hispanic white | 85.7 |
| Nonwhite or Hispanic | 14.3 |
| Education | |
| Less than high school | 20.3 |
| High school | 59.2 |
| Some college or more | 20.5 |
| Financial concern | |
| Finances important or very important for medical care decisions | 51.4 |
| Health | |
| Excellent or very good | 30.8 |
| Good | 40.3 |
| Fair or poor | 28.9 |
| Preferences | |
| Preference for seeing the doctor right away | 17.4 |
| Preference for tests | 45.5 |
| Preference for specialty visit | 26.1 |
| Preference for specialist as primary doctor | 21.9 |
| Number of outpatient visits: pooled years 2004–05 | 7.5 (6.5) |
SOURCE: Causes and Consequences of Health Care Intensity Patient Survey, national random sample of elderly Medicare beneficiaries.
NOTES: N = 1,936. Standard deviation is in parentheses.
Patients’ characteristics
The survey collected extensive information about beneficiaries’ attributes. Age was categorized in three groups: 65–74 (suppressed category in analyses below), 75–84, or 85 and older. Self-reported race and ethnicity were limited to non-Hispanic white (suppressed category), and nonwhite or Hispanic. We categorized education into less than a high school education, completion of high school (suppressed category), or some college or greater. Respondents were coded as having financial concerns if they indicated that financial issues were “very important” or “important” in deciding whether to obtain medical care. Respondents’ self-reported health status was collapsed from five to three groups: poor or fair health, good health, and very good or excellent health (the suppressed category).
Unmet desire for care
Respondents were deemed to have unmet medical need in the past twelve months if they answered “yes” to either of two questions: were there any tests or treatments they wanted but didn’t get, and did they want but not get to see a specialist?15
Regional visit rate
The regional visit rate is the outpatient visit rate per Medicare beneficiary—adjusted for age, sex, and race—in a Hospital Referral Region (HRR) in 2003, calculated from a 5 percent sample of Medicare Part B claims. Similar to variation in overall Medicare spending noted above, the estimates of outpatient visit rates from the 5 percent sample varies threefold across HRRs, from as low as 3.6 visits per beneficiary to as high as 10.5 visits. Survey respondents were assigned to the corresponding HRRs based on their ZIP codes of residence. We then categorized the HRR outpatient visit rate into five quintiles: low (mean rate of 4.9 visits per beneficiary); low moderate (mean rate of 5.7 visits); moderate (mean rate of 6.3 visits); high moderate (mean rate of 6.8 visits); and high (mean rate of 8.1 visits).
First, we looked at variations in patients’ preferences by individual demographic and health characteristics. Second, we estimated multivariate ordinary least squares (OLS) regressions of respondents’ number of outpatient visits on patients’ preferences, controlling for age, sex, race/ethnicity, education, financial concerns, and health status. Finally, we compared patients’ preferences across HRR visit-rate quintiles. We also compared respondents’ perceptions of unmet medical need across quintiles.
Results are displayed according to quintile, but all reported tests for trend were based on logisitic regression in which the independent variable was the outpatient visit rate in the respondent’s HRR of residence (expressed as a continuous variable), and the dependent variable was the respondent’s preference response. We performed multivariable logistic regression for each of the four preferences plus perception of unmet need, with HRR visit rate as the exposure (expressed as a continuous variable), adjusting for age, sex, race/ethnicity, education, financial strain, and health status. All regressions used the Huber/White/sandwich estimator of variance to adjust standard errors for clustering of respondents within HRRs.
Study Results
Sample characteristics
Data were available for 1,955 respondents for all variables used in the analyses. The mean age of respondents was 75.6 (standard deviation: 6.6); 57.8 percent were women, 85.7 percent were non- Hispanic white, and 14.3 percent were non-white or Hispanic (Exhibit 1). One-fifth of respondents had not completed high school, and more than half had a high school diploma. More than half reported that financial issues were important or very important in deciding whether to obtain medical care; 31 percent were in very good or excellent health.
Patients’ preferences and characteristics
Men and women did not differ significantly in preferences for seeing a doctor right away or for tests, but men were more likely than women to state a preference for specialty visits and for having specialists rather than one generalist as their primary providers (Exhibit 2). However, only a little more than one quarter of men expressed such preferences. There was little variation in preferences across age groups, except that respondents age eighty-five or older were somewhat more likely than younger respondents to want to see a doctor right away instead of waiting to see if symptoms resolved on their own.
EXHIBIT 2.
Patients’ Preferences For Care, By Individual Characteristics, 2005
| Characteristic | Prefer to see doctor right away |
Preference for tests |
Preference for specialty visits |
Prefer specialist as primary provider |
|---|---|---|---|---|
| Sex | ||||
| Male | 17% | 46% | 29% | 26% |
| Female | 18 | 46 | 24*** | 19*** |
| Age (years) | ||||
| 65–74 | 16 | 48 | 28 | 22 |
| 75–84 | 19 | 44 | 25 | 23 |
| 85+ | 22** | 43 | 25 | 18 |
| Race | ||||
| Nonwhite | 26 | 53 | 36 | 29 |
| White or Hispanic | 16*** | 44*** | 24*** | 21*** |
| Education | ||||
| Less than high school | 24 | 50 | 32 | 22 |
| High school graduate | 16 | 47 | 26 | 22 |
| At least some college or higher | 14*** | 39*** | 22*** | 23 |
| Financial strain | ||||
| Finances important when seeking medical care |
19 | 46 | 27 | 22 |
| Finances not important when seeking medical care |
16 | 45 | 24 | 22 |
| Health status | ||||
| Excellent or very good | 15 | 47 | 27 | 21 |
| Good | 18 | 46 | 24 | 22 |
| Fair or poor | 20 | 43 | 27 | 24 |
SOURCE: Causes and Consequences of Health Care Intensity Patient Survey, national random sample of elderly Medicare beneficiaries, 2005.
NOTE: Statistical significance is denoted as ANOVA F statistic of difference between groups.
p < 0.05
p < 0.01
There are strong and consistent differences in stated preferences by race/ethnicity. We found that nonwhites were more likely than whites to express preferences for visits right away, for tests and specialty care, and for specialists rather than one generalist primary care doctor. Elsewhere, we found similar racial differences in stated preferences for care, as have other researchers, which may result in part from poor physician-patient communication or concerns that the health care system is withholding care from minority patients.16
Patients’ preferences for care seeking also vary by education. Respondents with less than a high school education were more likely than more educated respondents to prefer visits right away, tests, and specialty visits. Respondents for whom financial matters are important or very important when making medical decisions were more likely than those for whom finances are not important to want visits right away, but these groups did not differ in other stated preferences for care seeking. Finally, there were no strong differences in preferences for care across health status groups, except that those who were in fair or poor health were somewhat more likely than those in the other health status categories to want to see a doctor right away when experiencing an unresolved cough or new chest pain.
Preferences and utilization
Exhibit 3 shows the results of OLS regressions (using five models, described below) of respondents’ number of outpatient visits on their characteristics and preferences. As shown in model 1, women had significantly more medical visits than men had in 2005, as did respondents older than age seventy-four, those with less than a high school diploma, and those with good or fair-poor health status.
EXHIBIT 3.
Regression Coefficients Of Medicare Beneficiaries’ Outpatient Visits On Patients’ Characteristics And Stated Preferences For Care, 2005
| Outpatient utilization | |||||
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
| Constant | 4.1***(0.35) | 4.0***(0.36) | 3.9***(0.37) | 4.0***(0.38) | 3.8***(0.38) |
| Female | 1.2***(0.30) | 1.2***(0.30) | 1.2***(0.30) | 1.2***(0.30) | 1.3***(0.29) |
| 75–84 years | 2.0***(0.30) | 2.1***(0.30) | 2.0***(0.30) | 2.0***(0.30) | 2.0***(0.30) |
| 85+ years | 1.5***(0.56) | 1.5***(0.56) | 1.6***(0.56) | 1.5***(0.56) | 1.6***(0.56) |
| Nonwhite race | −0.11 (0.42) | −0.19 (0.43) | −0.13 (0.42) | −0.12 (0.42) | −0.25 (0.42) |
| Less than high school | −0.48 (0.38) | −0.52 (0.38) | −0.49 (0.38) | −0.48 (0.38) | −0.47 (0.38) |
| College degree or higher | 0.65*(0.37) | 0.67*(0.37) | 0.67*(0.37) | 0.66*(0.37) | 0.64*(0.37) |
| Financial concerns | −0.21 (0.30) | −0.22 (0.30) | −0.21 (0.30) | −0.21 (0.30) | −0.21 (0.30) |
| Good health | 1.8***(0.31) | 1.8***(0.31) | 1.8***(0.31) | 1.8***(0.31) | 1.8***(0.31) |
| Poor or fair health | 3.9***(0.39) | 3.9***(0.39) | 3.9***(0.39) | 3.9***(0.39) | 3.9***(0.39) |
| Preference for seeing doctor right away (model 2) |
– | 0.79**(.39) | – | – | – |
| Preference for tests (model 3) | – | – | 0.25 (.28) | – | – |
| Preference for specialty visits (model 4) |
– | – | – | 0.08 (0.33) | – |
| Preference for specialist as primary provider (model 5) |
– | – | – | – | 1.4***(.38) |
| Adjusted R2 | 0.087 | 0.089 | 0.088 | 0.087 | 0.095 |
SOURCE: Causes and Consequences of Health Care Intensity Patient Survey, national random sample of elderly Medicare beneficiaries, 2005.
NOTES: N = 1,955. The regression coefficient indicates the net effect of the independent variables listed in column 1 on the number of outpatient visits, holding the remaining variables constant. For example, in model 1, female respondents had 1.2 more visits than male respondents, holding all else equal. Robust standard errors are in parentheses.
p < 0.10
p < 0.05
p < 0.01
Models 2–5 introduce the measures of stated preference for seeing a doctor right away, for tests, for specialist visits, and for having specialists for primary care. When patients’ health status and sociodemographic characteristics were controlled for, respondents’ stated preference for seeing a doctor right away was associated with significantly more outpatient visits (close to one additional visit annually). Similarly, a stated preference for specialists instead of one generalist as a primary provider was significantly associated with more than one additional visit per year. Preferences for tests or specialist visits were not significantly associated with visits. Including all variables in the model simultaneously produced the same results (results not shown). These findings indicate that even after patients’ health status and sociodemographic characteristics are controlled for, some individual preferences for care seeking influence utilization; those who preferred care right away and from specialists experienced higher utilization rates.
Preferences and regional variation
After patients’ demographic characteristics and health status were adjusted for (Exhibit 4), patients in the lowest quintile of outpatient visit rates were less likely than those in the higher quintiles to express a preference for seeing a doctor right away when experiencing an unresolved cough or new chest pain.17 Similarly, patients in the lowest quintile were also less likely than those in upper quintiles to prefer having multiple specialists rather than one generalist physician as their primary provider. There were no differences in preferences for tests or specialty visits across quintiles. These findings show that preferences vary across quintiles consistent with regional utilization patterns for two of the four preferences tested; however, it should be noted that the differences across quintiles are quite small.
EXHIBIT 4.
Percentage Of Elderly Medicare Beneficiary Respondents Reporting Various Preferences, By Quintiles Of Hospital Referral Region (HRR) Visit Rates, 2005
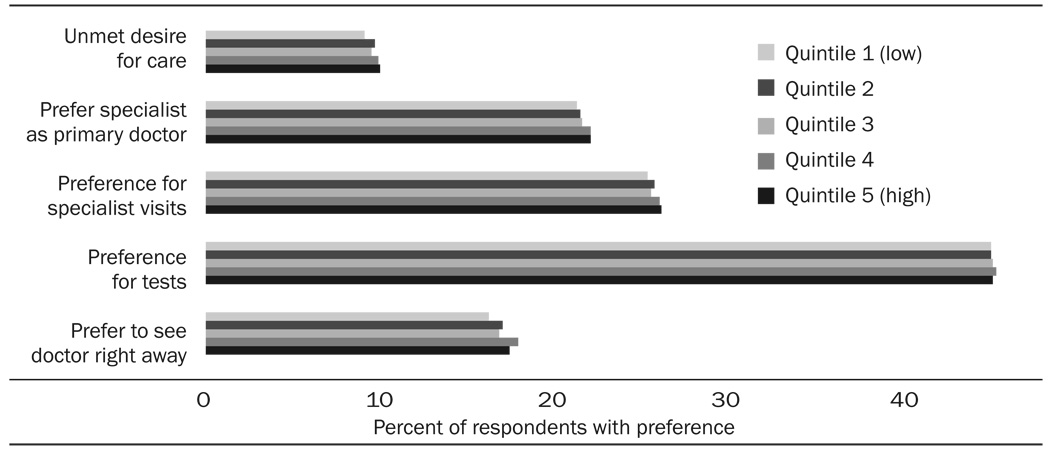 |
SOURCE: Causes and Consequences of Health Care Intensity Patient Survey, national random sample of elderly Medicare beneficiaries, 2005.
NOTES: Complete preference wordings are explained in the text. Adjusted for age, sex, nonwhite race, education, financial strain, and self-reported health status.
It could be the case that regardless of stated preferences for care, patients in the lower quintiles wanted more visits in the previous year than they received, on average. To test this hypothesis, we analyzed whether more patients in the lowest quintile had any unmet desire for care compared to those in higher quintiles. As shown in Exhibit 4, we found the opposite. That is, significantly more patients in the highest quintile of outpatient visits said that they had unmet desire for care, with and without adjustment for sociodemographic and health characteristics, although as above, the difference between the highest and lowest quintiles was less than 1 percent.
Discussion
More than thirty years ago, medical sociologists found that apparent health need, symptoms, or pain had little explanatory power for whether patients actually seek care.18 Factors such as socioeconomic and insurance status, having a regular source of care, and even patients’ social network characteristics influence both if and when they seek care.19 More recently, patient-centered care, designed to reflect patients’ preferences, has been identified as a key component of high-quality care.20 Given medical uncertainty for a variety of conditions, patients’ values and preferences should play a key role in treatment choices, yet physicians’ decisions do not always reflect their patients’ treatment preferences.21
Variation in preferences versus variation in use
This paper shows that at the individual level, there is considerable variation among elderly Medicare beneficiaries in preferences for seeking medical care. In addition, we found that some preferences are predictive of actual physician visits, even after health status and demographic factors were controlled for. Given this variation, it seems reasonable to expect that differences in patient demand may be responsible for at least some of the regional variation in utilization across the United States. However, although patients’ preferences are associated with utilization at the individual level, the distribution of preferences across regions appears quite similar, leading us to conclude that patients’ preferences have only a minor influence on aggregate regional usage patterns. Yet even these small differences in care-seeking preferences may provide some insight into how demand and supply interact to produce very different rates of utilization across regions. Patients in regions with high utilization encounter a health care system that is much more likely to provide tests and specialist visits. By being only slightly more likely to want to see a doctor sooner in an illness episode, patients in such regions enter a health care system that puts them on a trajectory of medical tests and specialist visits that they might not prefer and might not choose if they could.
Consistency with other studies
Our findings are consistent with the related studies by Amber Barnato and colleagues on patients’ preferences for end-of-life care, and Jack Fowler and colleagues on patient satisfaction across spending regions; both found little relation between patients’ preferences and the overall care they received.22
We expected initially that care-seeking preferences could evolve over time across regions. Patients in high-utilization regions encounter a health care system that is much more likely to provide tests and specialist visits, and so it would make sense for such patients to expect tests and referrals to specialists; indeed, they might suspect that they were being undertreated if they were not referred for subsequent testing and additional appointments. And although we did observe a greater preference for specialists rather than one generalist as a primary provider in high-visit-rate regions (consistent with this hypothesis), it is surprising that other measures of preferences, particularly for tests and for specialist visits, exhibited little association with normal patterns of care.
Limitations
This study has several important limitations. One is the use of hypothetical scenarios to ask about stated, not revealed, preferences. It is possible that in the event of an actual illness, people in regions with higher (or lower) visit rates might behave differently than they indicated in response to a hypothetical scenario. The particular survey items used here were intentionally oversimplified to gain insight into broad preferences, rather than to anticipate particular treatment choices for specific medical conditions. In addition, some caution is warranted in thinking about stated preferences as predictive of action, particularly in the context of health care.23 However, the finding that stated preferences were associated with actual utilization behavior at the individual level provides some support for the view that at least some stated preferences do translate into actual behavior.
Overall, the results of this survey suggest that observed regional variations in use and spending are attributable only weakly, if at all, to differences in preferences for care among residents of those regions. Policies aimed at changing individual patients’ use of health care are unlikely to have a major effect on regional differences in utilization that indicate high levels of unwarranted care. Regional variations in utilization caused by differences in informed patients’ preferences, based on shared decision- making tools that help patients and their providers identify how patients value potential clinical outcomes, could, in the long term, represent a success of patient-centered care initiatives.24 However, at this stage, it appears that more of the variation in use is the consequence of health care system characteristics than it is of patients’ preferences.
Acknowledgments
Funding was provided by National Institute on Aging (NIA) Grant no. P01 AG19783. The authors are grateful to F. Jack Fowler for valuable guidance in the design of the survey.
Contributor Information
Denise L. Anthony, Email: danthony@dartmouth.edu, Sociology at Dartmouth College in Hanover, New Hampshire.
M. Brooke Herndon, General Internal Medicine at Dartmouth Medical School.
Patricia M. Gallagher, The University of Massachusetts, Boston, Survey Research Center.
Amber E. Barnato, Medicine and Clinical and Translational Science at the University of Pittsburgh School of Medicine.
Julie P.W. Bynum, General Internal Medicine at Dartmouth Medical School.
Daniel J. Gottlieb, The Dartmouth Institute for Health Policy and Clinical Practice, Dartmouth Medical School, in Lebanon, New Hampshire.
Elliott S. Fisher, The Dartmouth Institute for Health Policy and Clinical Practice, Dartmouth Medical School, in Lebanon, New Hampshire.
Jonathan S. Skinner, The John Sloan Dickey Third Century Professor of Economics, Dartmouth College
NOTES
- 1.Wennberg JE, et al. [(accessed 24 February 2009)];Tracking the Care of Patients with Severe Chronic Illness: The Dartmouth Atlas of Health Care. 2008 http://www.dartmouthatlas.org/atlases/2008_Chronic_Care_Atlas.pdf. [PubMed]
- 2.Ibid.
- 3.See, for example, Welch WP et al. Geographic Variation in Expenditures for Physicians’ Services in the United States. New England Journal of Medicine. 1993;328(no 9):621–627. doi: 10.1056/NEJM199303043280906. Fisher ES, et al. Hospital Readmission Rates for Cohorts of Medicare Beneficiaries in Boston and New Haven. New England Journal of Medicine. 1994;331(no 15):989–995. doi: 10.1056/NEJM199410133311506. Gatsonis CA, et al. Variations in the Utilization of Coronary Angiography for Elderly Patients with an Acute Myocardial Infarction: An Analysis Using Hierarchical Logistic Regression. Medical Care. 1995;33(no 6):625–642. doi: 10.1097/00005650-199506000-00005. and McClellan M. Uncertainty, Health-Care Technologies, and Health-Care Choices. American Economic Review. 1995;85(no 2):38–44.
- 4.Wennberg JE, Fisher ES, Skinner JS. Geography and the Debate over Medicare Reform. Health Affairs. 2004;23:w96–w114. doi: 10.1377/hlthaff.w2.96. (published online 13 February 2002; 10.1377/hlthaff.w4.96) [DOI] [PubMed] [Google Scholar]; Fisher ES, et al. The Implications of Regional Variations in Medicare Spending, Part 1: The Content, Quality, and Accessibility of Care. Annals of Internal Medicine. 2003;138(no 4):273–287. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]; Fisher ES, et al. The Implications of Regional Variations in Medicare Spending, Part 2: Health Outcomes and Satisfaction with Care. Annals of Internal Medicine. 2003;138(no 4):288–298. doi: 10.7326/0003-4819-138-4-200302180-00007. [DOI] [PubMed] [Google Scholar]
- 5.See, for example, McLaughlin CG, et al. Small-Area Variation in Hospital Discharge Rates: Do Socioeconomic Variables Matter? Medical Care. 1989;27(no 5):507–521. doi: 10.1097/00005650-198905000-00006. Shwartz M, et al. Do Variations in Disease Prevalence Limit the Usefulness of Population-Based Hospitalization Rates for Studying Variations in Hospital Admissions? Medical Care. 2005;43(no 1):4–11. and Folland S, Stano M. Small Area Variations: A Critical Review of Propositions, Methods, and Evidence. Medical Care Review. 1990;47(no 4):419–465. doi: 10.1177/107755879004700403. See also the references in Notes 3 and 4
- 6.Bertko JM. Variation in Use of Medical Care Services: Higher Risk or Higher Consumption? Health Affairs. 2003;22:w363–w365. doi: 10.1377/hlthaff.w3.363. (published online 13 August 2003; 10.1377/hlthaff.w3.363) [DOI] [PubMed] [Google Scholar]
- 7. Fuchs VR. Floridian Exceptionalism. Health Affairs. 2003;22:w357–w362. doi: 10.1377/hlthaff.w3.357. (published online 13 August 2003; 10.1377/hlthaff.w3.357) Newhouse JP, et al. Does the Geographical Distribution of Physicians Reflect Market Failure. Bell Journal of Economics. 1982;13(no 2):493–505. and Sirovich BE, et al. Variation in the Tendency of Primary Care Physicians to Intervene. Archives of Internal Medicine. 2005;165(no 19):2252–2256. doi: 10.1001/archinte.165.19.2252.
- 8. Kravitz RL. Patients’ Expectations for Medical Care: An Expanded Formulation Based on Review of the Literature. Medical Care Research and Review. 1996;53(no 1):3–27. doi: 10.1177/107755879605300101. Kravitz RL. Measuring Patients’ Expectations and Requests. Annals of Internal Medicine. 2001;134(no 9):881–888. doi: 10.7326/0003-4819-134-9_part_2-200105011-00012. Part 2. Peck BM et al. Measuring Patient Expectations: Does the Instrument Affect Satisfaction or Expectations. Medical Care. 2001;39(no 1):100–108. doi: 10.1097/00005650-200101000-00011. Fiscella K, Franks P, Clancy CM. Skepticism toward Medical Care and Health Care Utilization. Medical Care. 1998;36(no 2):180–189. doi: 10.1097/00005650-199802000-00007. and Schwartz LM et al. Enthusiasm for Cancer Screening in the United States. Journal of the American Medical Association. 2004;291(no 1):71–78. doi: 10.1001/jama.291.1.71.
- 9. Fiscella, et al. Skepticism to ward Medical Care Jackson JL, Kroenke K. The Effect of Unmet Expectations among Adults Presenting with Physical Symptoms. Annals of Internal Medicine. 2001;134(no 9):889–897. doi: 10.7326/0003-4819-134-9_part_2-200105011-00013. Part 2. and Lewis CL, et al. Patient Preferences for Care by General Internists and Specialists in the Ambulatory Setting. Journal of General Internal Medicine. 2000;15(no 2):75–83. doi: 10.1046/j.1525-1497.2000.05089.x.
- 10. Blumenthal D. Quality of Care: What Is It? New England Journal of Medicine. 1996;335(no 12):891–894. doi: 10.1056/NEJM199609193351213. Crossing the Quality Chasm: A New Health System for the Twenty-first Century. National Academies Press: Washington; 2001. Institute of Medicine. Barnato AE, et al. Are Regional Variations in End-of-Life Care Intensity Explained by Patient Preferences? A Study of the U.S. Medicare Population. Medical Care. 2007;45(no 5):386–393. doi: 10.1097/01.mlr.0000255248.79308.41. Fowler FJ, Jr, et al. Relationship between Regional Per Capita Medicare Expenditures and Patient Perceptions of Quality of Care. Journal of the American Medical Association. 2008;299(no 20):2406–2412. doi: 10.1001/jama.299.20.2406. and Pritchard RS, et al. Influence of Patient Preferences and Local Health System Characteristics on the Place of Death. Journal of the American Geriatrics Society. 1998;46(no 10):1242–1250. doi: 10.1111/j.1532-5415.1998.tb04540.x.
- 11.Barnato, et al. Are Regional Variations? [Google Scholar]; Fowler, et al. Relationship. [(accessed 24 March 2009)]; The patient survey data set is available at http://www.intensity.dartmouth.edu/?q=node/15.
- 12.Appendix Exhibit 1 is available online at http://content.healthaffairs.org/cgi/content/full/28/3/864/DC1
- 13.Using Principal Component Analysis to analyze the six preference questions reduced these three variables to two factors (with rotation): preference for doctor visits right away, and preference for specialty care and tests. Substituting these two factors for the three preference variables in the subsequent linear regression analyses yielded substantively identical results.
- 14.The exact wording is in online Appendix Exhibit 1, as in Note 12.
- 15.Ibid.
- 16. Barnato AE, et al. Racial and Ethnic Differences in Preferences for End-of-Life Treatment. Journal of General InternalMedicine. doi: 10.1007/s11606-009-0952-6. (forthcoming) Stein R. At the End of Life, a Racial Divide. Washington Post. 2007 March 12; Crawley L, et al. Palliative and End-of-Life Care in the African American Community. Journal of the American Medical Association. 2000;284(no 19):2518–2521. doi: 10.1001/jama.284.19.2518. and Stepanikova I, et al. Patients’ Race, Ethnicity, Language, and Trust in a Physician. Journal of Health and Social Behavior. 2006;47(no 4):390–405. doi: 10.1177/002214650604700406.
- 17.A graph of unadjusted results is available in Appendix Exhibit 2, online as in Note 12
- 18.Zola IK. Pathways to the Doctor—From Person to Patient. Social Science and Medicine. 1973;7(no 9):677–689. doi: 10.1016/0037-7856(73)90002-4. [DOI] [PubMed] [Google Scholar]
- 19.Buchmueller TC, et al. The Effect of Health Insurance on Medical Care Utilization and Implications for Insurance Expansion: A Review of the Literature. Medical Care Research and Review. 2005;62(no 1):3–30. doi: 10.1177/1077558704271718. [DOI] [PubMed] [Google Scholar]; Pescosolido BA. Beyond Rational Choice: The Social Dynamics of How People Seek Help. American Journal of Sociology. 1992;97(no 4):1096–1138. [Google Scholar]; Katz JN. Patient Preferences and Health Disparities. Journal of the American Medical Association. 2001;286(no 12):1506–1509. doi: 10.1001/jama.286.12.1506. [DOI] [PubMed] [Google Scholar]; Phillips KA et al. Understanding the Context of Healthcare Utilization: Assessing Environmental and Provider-Related Variables in the Behavioral Model of Utilization. Health Services Research. 1998;33(no 3):571–596. Part 1. [PMC free article] [PubMed] [Google Scholar]
- 20.Blumenthal Quality of Care [Google Scholar]; IOM Crossing the Quality Chasm [Google Scholar]
- 21.See, for example, Coppola KM, et al. Accuracy of Primary Care and Hospital-Based Physicians' Predictions of Elderly Outpatients Treatment Preferences With and Without Advance Directives. Archives of Internal Medicine. 2001;161(no 3):431–440. doi: 10.1001/archinte.161.3.431. Jackson, Kroenke The Effect of Unmet Expectations O’Connor AM, Llewellyn-Thomas HA, Flood AB. Modifying Unwarranted Variations in Health Care: Shared Decision Making Using Patient Decision Aids. Health Affairs. 2004;23:VAR-63–VAR-72. doi: 10.1377/hlthaff.var.63. (published online 7 October 2004; 10.1377/hlthaff.var.63) and Varma S, Wendler D. Medical Decision Making for Patients without Surrogates. Archives of Internal Medicine. 2007;167(no 16):1711–1715. doi: 10.1001/archinte.167.16.1711.
- 22.Barnato, et al. Are Regional Variations? [Google Scholar]; Fowler, et al. Relationship [Google Scholar]
- 23. Phillips KA, Johnson FR, Maddala T. Measuring What People Value: A Comparison of ‘Attitude’ and ‘Preference’ Surveys. Health Services Research. 2002;37(no 6):1659–1679. doi: 10.1111/1475-6773.01116. Fried TR, et al. Prospective Study of Health Status Preferences and Changes in Preferences over Time in Older Adults. Archives of Internal Medicine. 2006;166(no 8):890–895. doi: 10.1001/archinte.166.8.890. Sevdalis N, Harvey N. Predicting Preferences: A Neglected Aspect of Shared Decision-Making. Health Expectations. 2006;9(no 3):245–251. doi: 10.1111/j.1369-7625.2006.00391.x. and Vick S, Scott A. Agency in Health Care: Examining Patients’ Preferences for Attributes of the Doctor-Patient Relationship. Journal of Health Economics. 1998;17(no 5):587–605. doi: 10.1016/s0167-6296(97)00035-0.
- 24. Barry MJ, et al. Patient Reactions to a Program Designed to Facilitate Patient Participation in Treatment Decisions for Benign Prostatic Hyperplasia. Medical Care. 1995;33(no 8):771–782. doi: 10.1097/00005650-199508000-00003. Deyo RA, et al. Involving Patients in Clinical Decisions: Impact of an Interactive Video Program on Use of Back Surgery. Medical Care. 2000;38(no 9):959–969. doi: 10.1097/00005650-200009000-00009. and O’Connor, et al. Modifying Unwarranted Variations


