Abstract
OBJECTIVE
Cystic fibrosis (CF)-related diabetes (CFRD) diagnosis and management have considerably changed since diabetes was first shown to be associated with a poor prognosis in subjects with CF. Current trends in CFRD prevalence, incidence, and mortality were determined from a comprehensive clinical database.
RESEARCH DESIGN AND METHODS
Data were reviewed from 872 CF patients followed at the University of Minnesota during three consecutive intervals: 1992–1997, 1998–2002, and 2003–2008.
RESULTS
CFRD is currently present in 2% of children, 19% of adolescents, and 40–50% of adults. Incidence and prevalence are higher in female subjects aged 30–39 years; otherwise, there are no sex differences. In younger individuals, CFRD without fasting hyperglycemia predominates, but fasting hyperglycemia prevalence rises with age. CFRD mortality has significantly decreased over time. From 1992–1997 to 2003–2008, mortality rate in female subjects dropped by >50% from 6.9 to 3.2 deaths per 100 patient-years and in male subjects from 6.5 to 3.8 deaths per 100 patient-years. There is no longer a sex difference in mortality. Diabetes was previously diagnosed as a perimorbid event in nearly 20% of patients, but of 61 patients diagnosed with diabetes during 2003–2008, only 2 died. Lung function but not nutritional status is still worse in CF patients with diabetes compared with those without diabetes. Nutritional status and pulmonary status are similar between patients without fasting hyperglycemia and those with fasting hyperglycemia.
CONCLUSIONS
Previously noted sex differences in mortality have disappeared, and the gap in mortality between CF patients with and without diabetes has considerably narrowed. We believe that early diagnosis and aggressive treatment have played a major role in improving survival in these patients.
Diabetes is the most common comorbidity in subjects with cystic fibrosis (CF). Of particular concern is the fact that the additional diagnosis of diabetes has been associated with significantly greater mortality, especially in women. In 1988, we reported that compared with >60% of the nondiabetic CF population, <25% of individuals with diabetes survived until age 30 years (1). We subsequently published data examining mortality at the University of Minnesota Cystic Fibrosis Center during the 15-year period between 1987 and 2002 and reached the startling conclusion that diabetes reduced survival in women by >16 years (2). Unlike the general population, patients with CF-related diabetes (CFRD) are not at risk for atherosclerotic cardiovascular disease (3); as in other individuals with CF, death occurs from chronic inflammatory lung disease. In several studies, pulmonary function and nutritional status have been shown to be intimately linked and to be worse in patients with CFRD compared with CF patients without diabetes (4–8). It has been postulated that this is a consequence of the protein catabolic effects of insulin deficiency combined with the proinflammatory effects of hyperglycemia.
Since 1987, experimental studies and careful clinical data collection have progressively increased our understanding of CFRD, and it is managed much differently today than even 5 years ago. With routine annual oral glucose tolerance test (OGTT) outpatient screening and careful inpatient glucose monitoring, patients are not likely to experience long periods of undiagnosed diabetes. We are much better able to accurately report prevalence and incidence of CFRD, particularly in the older age-groups, because CF patients are living longer. Early institution of intensive basal-bolus insulin therapy has become routine in the last 5 years. Thus, patients are diagnosed earlier and treated more aggressively than ever before. The current database review was undertaken to determine whether modern diabetes screening and management have influenced prevalence, incidence, and mortality figures.
RESEARCH DESIGN AND METHODS
Clinical information was reviewed from a total of 872 patients followed at the University of Minnesota Cystic Fibrosis Center from 1 January 1992 through 15 September 2008. CF patients are routinely seen at quarterly intervals, and patient data are recorded in the Minnesota Cystic Fibrosis Database. The information collected includes demographic and anthropometric data, pulmonary function tests, other laboratory tests, data on medication use, and clinical characteristics. All patients followed at this center gave informed consent permitting their records to be reviewed for research purposes.
CFRD diagnosis and management
CFRD is diagnosed by standard criteria including persistent random glucose levels >200 mg/dl (11.1 mmol/l) and persistent fasting glucose levels >126 mg/dl (7.0 mmol/l) or by OGTT. Routine annual OGTT screening has been recommended at the University of Minnesota since the early 1990s for patients aged ≥6 years (1.75 g/kg glucose [maximum 75g]). OGTTs are performed when patients are in their usual baseline state of health. Subjects are classified based on standards adopted by the 1998 CFRD consensus guidelines (9). Patients with a fasting glucose ≥126 mg/dl (7.0 mmol/l) have CFRD with fasting hyperglycemia, while those with a fasting glucose <126 mg/dl (7.0 mmol/l) and a 2-h glucose ≥200 mg/dl (11.1 mmol/l) have CFRD without fasting hyperglycemia.
Diabetes management follows a uniform protocol that includes the involvement of an endocrinologist, a diabetes nurse educator, and a dietitian. Prior to 2003, the most common insulin regimen for patients with fasting hyperglycemia was a single injection of NPH insulin at bedtime and three to four injections of regular insulin (before 2000) or four to six injections of rapid-acting insulin (after 2000) with meals. Patients without fasting hyperglycemia were seldom treated with insulin. Since 2003, basal-bolus insulin therapy has been standard for CFRD with fasting hyperglycemia, using either an insulin pump or multiple daily injections including basal insulin. Patients without fasting hyperglycemia have been encouraged to use premeal rapid-acting insulin. Hospitalized patients are now routinely treated with insulin if they are hyperglycemic; the need for persistent insulin is then reevaluated once they are clinically well.
Database review
In order to examine temporal changes, the data were examined for three consecutive intervals: 1 January 1992 through 31 December 1997, 1 January 1998 through 31 December 2002, and 1 January 2003 through 15 September 2008. All patients seen in a clinic during an interval were included in calculations for that interval. Date of diabetes diagnosis was the earlier date for either starting insulin based on clinical criteria or an OGTT result diagnostic of diabetes. Percent predicted forced expiratory volume in 1 s (FEV1) was the last recorded value before 15 September 2008.
Analytic methods
Prevalence percents and counts were compared between groups with logistic regression. Incidence and mortality rates were calculated as d/m, where d is the total number of events during a time interval and m is the total time at risk of the event during the interval from all individuals. Under a Poisson model, the SE of the rate is √d/m. Incidence and mortality rates were compared between groups with Poisson regression. All analyses were performed with SAS (version 9.2; SAS Institute, Cary, NC).
RESULTS
CFRD prevalence
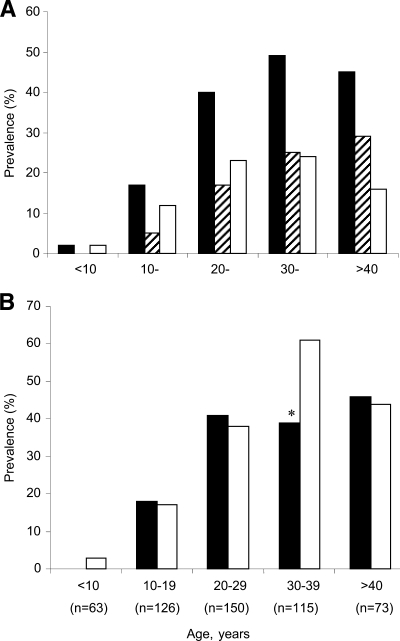
In September 2008, there were 527 pediatric and adult patients actively followed at the University of Minnesota Cystic Fibrosis Center. Of these, 33% had diabetes—the figure similar to the 30% at the end of 2002 but showing a significant increase from the 20% of patients known to have diabetes at the end of 1997 (Table 1). In all three periods, the prevalence of diabetes rose steadily with age through the 30–39 age decade and after the age of 40 years remained at 45–50% (Fig. 1A). In younger individuals, CFRD without fasting hyperglycemia predominated; however, the prevalence of fasting hyperglycemia rose steadily with age so that the percentage of CFRD patients with and without fasting hyperglycemia was approximately equal for individuals in their 30s, and after the age of 40 years, CFRD with fasting hyperglycemia predominated. In 2008, female subjects had significantly higher diabetes prevalence in the 30–39 age decade than male subjects, but otherwise no sex differences in prevalence were present (Fig. 1B).
Table 1.
Mortality rates and CFRD prevalence and incidence for consecutive time intervals
| 1992−1997 | 1998−2002 | 2003−2008 | |
|---|---|---|---|
| Patients seen in a clinic during the interval | 752 | 702 | 647 |
| Female subjects (%) | 53 | 53 | 53 |
| CFRD prevalence at the end of the interval (%) | 20 ± 2a | 30 ± 2b | 33 ± 2b |
| CFRD incidence per 100 person-years | 3.0 ± 0.3a | 4.0 ± 0.4b | 2.7 ± 0.3a |
| CFRD mortality rate per 100 person-years | 6.7 ± 1.3a | 5.4 ± 0.9a | 3.5 ± 0.6b |
| Patients diagnosed with CFRD during the interval/those who were diagnosed and died within the same interval | 108/18a | 102/12a | 61/2b |
| Total CF population mortality rate per 100 person-years | 1.2 ± 0.2 | 1.6 ± 0.2 | 1.8 ± 0.2 |
| Non-CFRD mortality rate per 100 person-years | 0.5 ± 0.1a | 0.6 ± 0.2ab | 1.0 ± 0.2b |
Data are means ± SE unless otherwise indicated. a, b Comparisons are between time intervals within each row. Rates that do not share a letter are significantly different (P < 0.05); rates that share a letter are not significantly different. Rows with no letters have no significant differences. During each interval, for all rates there were no significant differences between male and female subjects.
Figure 1.
Current prevalence of CFRD in the 527 patients actively followed at the University of Minnesota, 15 September 2008. A: CFRD total (■), CFRD with fasting hyperglycemia (▨), and CFRD without fasting hyperglycemia (□) by decade of age. B: CFRD total men (■) versus women (□) by decade of age. The number of total subjects (with and without diabetes) in each age-group is noted. *P = 0.02, men vs. women.
CFRD incidence
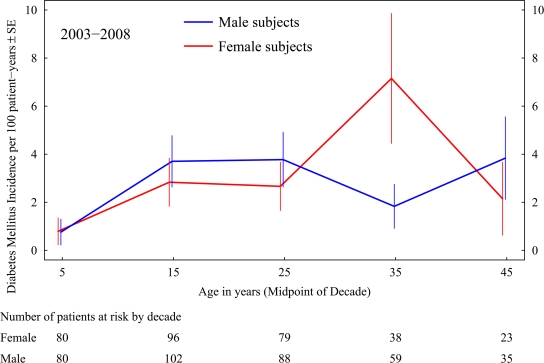
While diabetes prevalence rose, incidence fell significantly: from four cases per 100 patient-years during the 1998–2002 interval to 2.7 cases per 100 patient-years during 2003–2008, representing a 40% decrease in the number of diabetes diagnoses (Table 1). The decrease in incidence occurred for both male and female subjects, with a larger decrease in female subjects. During the 1990s, annual OGTT surveillance was just being established as the standard; thus, many of those receiving a new diagnosis of diabetes at their first screening may have had the disease for some time, inflating incidence. Currently, a peak in incidence is noted in women aged 30–39 years (Fig. 2).
Figure 2.
The University of Minnesota CFRD incidence per 100 patient-years by sex and age decade 2003–2008. Sample sizes for the incidence rates are shown below the figure.
CFRD mortality
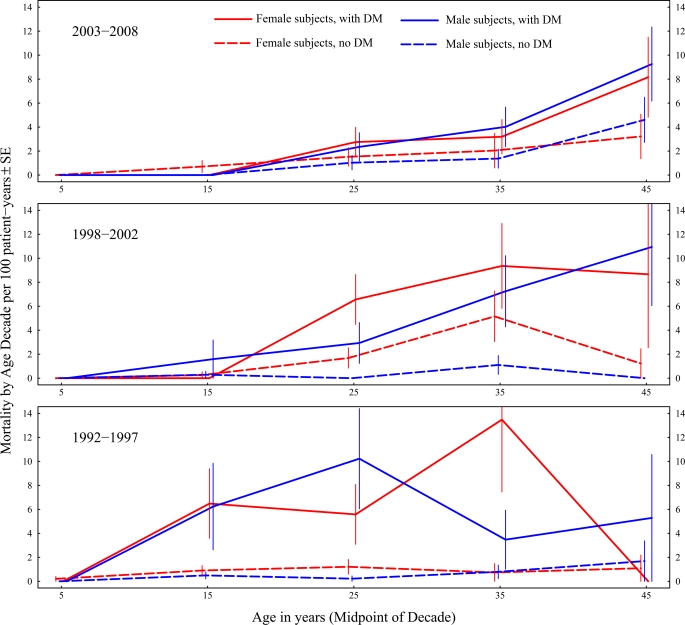
The increase in diabetes prevalence with a decrease in diabetes incidence resulted from a significant decrease in mortality in patients with diabetes. From 1992–1997 to 2003–2008, mortality in female subjects with diabetes dropped by >50%, from 6.9 to 3.2 deaths per 100 patient-years, and the decrease in male subjects was nearly as large, from 6.5 to 3.8 deaths per 100 patient-years (Table 1). During the earlier two time periods, diabetes was frequently diagnosed as a perimorbid event. Of 108 patients diagnosed with diabetes during 1992–1997, 18 died during that same interval, and results were nearly identical during 1998–2002. During 2003–2008, 61 patients were diagnosed with diabetes, of whom only 2 died during the interval.
Mortality is shown in Fig. 3 by diabetes status, sex, and age decade over the three time intervals. Over time, there has been a steady decrease in mortality in CF patients with diabetes. In the most recent time period, overall mortality still remained significantly higher in those with CFRD compared with those without diabetes, but the gap has considerably narrowed compared with the earlier time periods. Importantly, during 2003–2008, sex differences in mortality by diabetes status appear to have disappeared.
Figure 3.
The University of Minnesota CFRD and CF mortality per 100 patient-years by sex and age decade over three time periods: 2003–2008, 1998–2002, and 1992–1997. CF patients with diabetes (DM) are shown with solid lines, while CF patients without diabetes are shown with dashed lines. Zero rates estimated from <10 patients are not shown. The gap in mortality between those with and those without diabetes has diminished over these time periods, and the sex difference in mortality has disappeared in the most current analysis.
Clinical characteristics of the 2008 CFRD patient cohort
In September 2008, only 2 of 93 children aged <11 years had diabetes (a boy and a girl both without fasting hyperglycemia). Of 75 adolescents aged 11–17 years, 19% had diabetes (6 girls and 8 boys [4 of the girls and 1 of the boys with fasting hyperglycemia]). There was a trend toward lower percent predicted FEV1 in those with diabetes, but this did not achieve statistical significance in this age-group (83 ± 29 vs. 95 ± 17; P = 0.055). CF adolescents were generally normally nourished, and there were no significant differences in BMI percentile (47 ± 27 vs. 51 ± 25 kg/m2; P = 0.65) or BMI z-score (−0.1 ± 0.9 vs. 0.0 ± 0.8; P = 0.6) between those with and without CFRD. Among the 14 adolescents with CFRD, there were no significant differences in pulmonary or nutritional end points between those with and without fasting hyperglycemia.
Mortality has previously been shown to be greater in adult CF patients with diabetes; the adult data are shown in Table 2. Of subjects aged ≥18 years, 155 of 359 (43%) had diabetes, half with and half without fasting hyperglycemia. There was no difference in age or nutritional status between subjects with and without diabetes. Lung function, however, was significantly worse in subjects with diabetes (percent predicted FEV1 65 ± 24 vs. 71 ± 24, P < 0.05). Surprisingly, this mean difference was almost entirely a result of worse lung function in male subjects. Among diabetic subjects, those with fasting hyperglycemia tended to be older, with longer duration of diabetes but with similar nutritional status and FEV1 than those without fasting hyperglycemia.
Table 2.
Characteristics of the 2008 adult CF population, aged ≥18 years, followed at the University of Minnesota (n = 359)
| Total population |
Male subjects |
Female subjects |
||||||
|---|---|---|---|---|---|---|---|---|
| CFRD | No CFRD | Without fasting hyperglycemia | With fasting hyperglycemia | No CFRD | Without fasting hyperglycemia | With fasting hyperglycemia | No CFRD | |
| N | 155 | 204 | 35 | 43 | 110 | 43 | 34 | 94 |
| Age (years) | 33 ± 10 | 32 ± 10 | 32 ± 10 | 35 ± 10 | 33 ± 9 | 32 ± 8 | 35 ± 11 | 31 ± 11 |
| Duration of diabetes (years) | 10 ± 5 | — | 9 ± 5 | 9 ± 5 | — | 8* ± 4 | 13* ± 4 | — |
| BMI (kg/m2) | 22.6 ± 4 | 23.3 ± 4 | 21.8 ± 4 | 23.7† ± 6 | 24.0† ± 4 | 22.2 ± 3 | 22.5† ± 4 | 22.6† ± 4 |
| Percent predicted FEV1 | 65‡ ± 24 | 71‡ ± 24 | 60‡ ± 21 | 61‡ ± 22 | 72‡ ± 24 | 67 ± 23 | 71 ± 29 | 69 ± 24 |
Data are means ± SD unless otherwise indicated. Data are not shown for 167 children and adolescents in whom there were no significant differences in pulmonary function or BMI between those with and those without diabetes. (See text for details.)
*Significant difference (P < 0.05) in duration of diabetes between female subjects with and without fasting hyperglycemia.
†Significant differences (P < 0.05) between male and female subjects within a diagnostic subgroup (with fasting hyperglycemia, without fasting hyperglycemia, or with no CFRD).
‡Significant differences (P < 0.05) between CFRD and no CFRD.
CONCLUSIONS
The 527 patients currently followed at the University of Minnesota Cystic Fibrosis Center are well characterized with regard to diabetes prevalence, incidence, and mortality. CFRD is present in 2% of children, 19% of adolescents, 40% of individuals in their 20s, and 45–50% of those aged ≥30 years. In the age-group of 30–39 years, women with CFRD outnumber men, but otherwise we do not observe a sex difference in prevalence. Incidence is 2.7 cases per 100 patient-years, with the exception of women in their 30s, in whom the incidence more than doubles. Although mortality is still greater in CF patients who develop diabetes, over the last 15 years this difference has steadily and markedly diminished, and the previously noted sex difference in mortality appears to have completely disappeared.
Since 1988, several reports have documented worse clinical status in CF patients who developed diabetes. Both a 2005 North American review of 8,247 CF patients (8) and a 2001 European study of 7,500 patients (6) found that CFRD was associated with more severe pulmonary disease and worse nutritional status, and this finding was also documented in multiple smaller studies (1,4,5,7). This has been postulated to be related to both insulin deficiency (with resultant protein catabolism and malnutrition) and the influence of hyperglycemia on inflammation and infection. The current assessment demonstrates that although we still find worse lung function in patients with CFRD, the mortality associated with this condition has steadily and substantially decreased over time. We speculate that this is related to both earlier detection of diabetes and more aggressive treatment. CFRD is generally clinically silent and only detected by screening. In the past, diabetes was often diagnosed in patients with existing but previously undetected (and untreated) disease, often in the perimorbid period. Routine screening now ensures that diabetes is detected early in its course.
CFRD treatment is also much more aggressive today than in the past. The goals of treatment are to achieve near-normalization of blood glucose levels and to deliver as much insulin as possible without producing hypoglycemia in order to maximize the anabolic effects of insulin. At the time of the last CFRD consensus conference in 1998, it was not clear whether CFRD without fasting hyperglycemia was a milder form of diabetes requiring less intensive treatment. The current assessment suggests that pulmonary and nutritional parameters do not differ by fasting glucose status and that patients without fasting hyperglycemia are not “less sick” than those with fasting hyperglycemia. The standard of care at the University of Minnesota is now insulin therapy for CFRD patients with and without fasting hyperglycemia.
When the University of Minnesota CF mortality data from 1987 to 2002 were previously analyzed (2), women with CF and diabetes had dramatically worse survival. This could not be explained by age, age of diagnosis of CF or diabetes, A1C, BMI, pregnancy, glucocorticoid use, microorganism colonization, or genotype. A sex difference was also found in a multicenter British study that reported worse lung function in women with CF and diabetes (10). We speculated that diabetes might exacerbate CF-related pulmonary inflammation and protein catabolism and that the presence of anabolic steroids might offer men natural protection from the catabolic effects of these two diseases. With modern intensive diabetes treatment, the sex difference in mortality appears to have disappeared.
In summary, diabetes is an expected complication as individuals with CF grow older. It is encouraging to note that previous sex differences in mortality have disappeared and that the gap in mortality between CF patients with diabetes and CF patients without diabetes has considerably narrowed. Although many factors have changed in the management of individuals with CF over the last decade, we believe that early diagnosis and aggressive treatment of CFRD have played a major role in improving survival in these patients.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1.Finkelstein SM, Wielinski CL, Elliott GR, Warwick WJ, Barbosa J, Wu SC, Klein DJ: Diabetes mellitus associated with cystic fibrosis. J Pediatr 1988; 112: 373– 377 [DOI] [PubMed] [Google Scholar]
- 2.Milla CE, Billings J, Moran A: Diabetes is associated with dramatically decreased survival in female but not male subjects with cystic fibrosis. Diabetes Care 2005; 28: 2141– 2144 [DOI] [PubMed] [Google Scholar]
- 3.Schwarzenberg SJ, Thomas W, Olsen TW, Grover T, Walk D, Milla CE, Moran A: Microvascular complications in cystic fibrosis-related diabetes. Diabetes Care 2007; 30: 1056– 1061 [DOI] [PubMed] [Google Scholar]
- 4.Bismuth E, Laborde K, Taupin P, Velho G, Ribault V, Jennane F, Grasset E, Sermet I, De Buc J, Lenoir G, Robert J-J: Glucose tolerance and insulin secretion, morbidity and death in patients with CF. J Pediatr 2008; 152: 540– 545 [DOI] [PubMed] [Google Scholar]
- 5.Cawood TJ, McKenna MJ, Gallagher CG, Smith D, Chung WY, Gibney J, O'Shea D: Cystic fibrosis-related diabetes in adults. Ir Med J 2006; 99: 83– 86 [PubMed] [Google Scholar]
- 6.Koch D, Rainisio M, Madessani U, Harms HK, Hodson ME, Mastella G, McKenzie SG, Navarro J, Strandvik B: Presence of cystic fibrosis-related diabetes mellitus is tightly linked to poor lung function in patients with cystic fibrosis: data from the European Epidemiologic Registry of Cystic Fibrosis. Pediatr Pulmonol 2001; 32: 343– 350 [DOI] [PubMed] [Google Scholar]
- 7.Lanng S, Thorsteinsson B, Nerup J, Koch C: Influence of the development of diabetes mellitus on clinical status in patients with cystic fibrosis. Eur J Pediatr 1992; 151: 684– 687 [DOI] [PubMed] [Google Scholar]
- 8.Marshall BC, Butler SM, Stoddard M, Moran AM, Liou TG, Morgan WJ: Epidemiology of cystic fibrosis-related diabetes. J Pediatr 2005; 146: 681– 687 [DOI] [PubMed] [Google Scholar]
- 9.Moran A, Hardin D, Rodman D, Allen HF, Beall RJ, Borowitz D, Brunzell C, Campbell PW, Chesrown SE, Duchow C, Fink RJ, FitzSimmons SC, Hamilton N, Hirsch I, Howenstine MS, Klein DJ, Madhun Z, Pencharz PB, Quittner AL, Robbins MK, Schindler T, Schissel K, Schwarzenberg SJ, Stallings VA, Tullis DE, Zipf WB: Diagnosis, screening, and management of CFRD: a consensus conference report. Diabetes Res Clin Pract 1999; 45: 55– 71 [DOI] [PubMed] [Google Scholar]
- 10.Sims EJ, Green MW, Mehta A: Decreased lung function in female but not male subjects with established cystic fibrosis-related diabetes. Diabetes Care 2005; 28: 1581– 1587 [DOI] [PubMed] [Google Scholar]