Abstract
OBJECTIVE
Understanding the reasons and eliminating the pervasive health disparities in diabetes is a major research, clinical, and health policy goal. We examined whether health literacy, general numeracy, and diabetes-related numeracy explain the association between African American race and poor glycemic control (A1C) in patients with diabetes.
RESEARCH DESIGN AND METHODS
Adults with type 2 diabetes (n = 383) were enrolled in a cross-sectional study at primary care and diabetes clinics at three medical centers. Data collected included the following: self-reported race, health literacy, general numeracy, diabetes-related numeracy, A1C, and sociodemographic factors. A series of structural equation models were estimated to explore the interrelations between variables and test for mediation.
RESULTS
In model 1, younger age (r = −0.21, P < 0.001), insulin use (r = 0.27, P < 0.001), greater years with diabetes (r = 0.16, P < 0.01), and African American race (r = 0.12, P < 0.01) were all associated with poorer glycemic control. In model 2, diabetes-related numeracy emerged as a strong predictor of A1C (r = −0.46, P < 0.001), reducing the association between African American and poor glycemic control to nonsignificance (r = 0.10, NS). In model 3, African American race and older age were associated with lower diabetes-related numeracy; younger age, insulin use, more years with diabetes, and lower diabetes-related numeracy were associated with poor glycemic control.
CONCLUSIONS
Diabetes-related numeracy reduced the explanatory power of African American race, such that low diabetes-related numeracy, not African American race, was significantly related to poor glycemic control. Interventions that address numeracy could help to reduce racial disparities in diabetes.
Limited literacy in adults may contribute to racial disparities in health (1,2). According to the Institute of Medicine, 90 million people in the U.S. lack the literacy proficiency needed to effectively understand and act on health information (3). This has often been referred to as health literacy: a reflection of the complex interface between a patient's ability and the literacy prerequisites of participating in one's health and interacting with the health care system (3). Low health literacy is common among patients with diabetes. Patients with lower health literacy have greater difficulty understanding their disease (4), worse glycemic control (5,6), and worse clinical outcomes (7) than patients with adequate health literacy. Individuals at highest risk for low health literacy include individuals who are elderly, publicly insured or uninsured, lack English proficiency, and/or are members from a racial or ethnic minority group (8).
Numeracy is an important component of literacy and has been defined as “the ability to understand and use numbers in daily life” (9). In a national survey, 61% of adults in the U.S. could not perform the most rudimentary of quantitative skills, and another 26% of respondents had only basic skills (10). A few recent studies have found numeracy to be important in health (11); and while health literacy and numeracy may be related (10), we have found many patients with adequate health literacy skills who lack basic numeracy skills (9). Thus, the impact of literacy and/or numeracy on patient health outcomes may vary according to the requisite skills needed for self-management in a given disease context (12–14).
In diabetes, both limited health literacy and numeracy, and African American race have been associated with poorer glycemic control (6,15). Furthermore, the prevalence of low health literacy and numeracy has been significantly higher among African American individuals with diabetes than whites (14,15). Recent studies in other diseases suggest that health literacy is a more powerful predictor of health outcomes than race (1,2). However, the role of numeracy as a determinant of racial differences in health outcomes, and whether numeracy is more likely than health literacy to explain these differences, is unknown. The objective of this study was to examine the mediating effect of health literacy and numeracy (general and diabetes-related) on the relationship between African American race and glycemic control.
RESEARCH DESIGN AND METHODS
Setting and study participants
From March 2004 until November 2005, study participants were enrolled in a cross-sectional study from two primary care clinics and two diabetes specialty clinics located at three medical centers. Inclusion criteria included a diagnosis of type 1 or type 2 diabetes, age 18–85 years, and English-speaking. Exclusion criteria included a previous diagnosis of dementia, psychosis, or blindness. In addition, patients with a corrected visual acuity of 20/50 or worse using a Rosenbaum Screener (Prestige Medical, Northridge, CA) were excluded. Participants received $20 for participation. The Veterans Affairs Tennessee Valley Healthcare System Research & Development Committee and Institutional Review Boards at Vanderbilt University Medical Center and the University of North Carolina at Chapel Hill approved this study. Written consent was obtained from all participants.
Data and procedure
Trained research assistants received referrals of potential patients from clinic health providers and then engaged in an informed consent process and conducted a structured interview with enrolled patients. Information gathered included demographic information, literacy, general numeracy, diabetes-related numeracy, and glycemic control. Demographic and clinical self-reported information included patient age, sex, education level, annual income, race/ethnicity, the use of insulin, diabetes type, and years of diagnosed diabetes.
Measures
Literacy.
Literacy was assessed using the Rapid Estimate of Adult Literacy in Medicine (REALM), a validated measure of reading ability that correlates with reading comprehension (16). If the patient scored less than a sixth-grade reading level by the REALM, then the remainder of the instruments were administered orally to ensure that the content of the survey questions were understood by the patient. All subjects were given the option of oral administration if desired.
General numeracy.
General numeracy skills were measured with the math section of the Wide Range Achievement Test, 3rd Edition (WRAT-3), a validated instrument that evaluates calculation skills (17).
Diabetes-related numeracy.
Diabetes-related numeracy skills were measured with the recently validated Diabetes Numeracy Test (DNT) (13). In contrast to the WRAT-3, which primarily measures calculation skills, the DNT is composed of word problems assessing calculation, interpretation of tables, graphs or figures, and the application of necessary numeracy skills to solve problems and perform self-management tasks specific to diabetes care.
Glycemic control.
Glycemic control was assessed by the most recent A1C value in the patient's medical record; 96% were obtained within 6 months of the subject evaluation and the median time between A1C and evaluation was 15 days (range 0–323).
Analyses
Structural equation models (SEM), specifying the relationships between variables, were estimated using AMOS, version 17. Advantages of this procedure include the generality and flexibility of model specification and the ability to assess fit of the hypothesized model to the observed data.
Model fit using maximum likelihood estimation can be evaluated through use of the χ2 goodness-of-fit statistic. If χ2 is large relative to the degrees of freedom, this represents a poor fit of the estimated model to the data. Conversely, when χ2 is small relative to the degrees of freedom, this represents adequacy of model fit. Because sample size may unpredictably influence the evaluation of the fit of the model to the observed data, supplemental indicators of model fit, such as the comparative fit index (CFI) and root mean square error of approximation (RMSEA), were also applied (18). CFI values that exceed 0.90 and RMSEA values below 0.08 indicate acceptable model fit (18). The CFI and the RMSEA are both sensitive to model misspecification and are minimally affected by sample size (18). Hypotheses regarding the specific structural relations of the constructs in the model were also evaluated through inspection of the direction and magnitude of the path coefficients.
Three structural equation models were estimated with a correlation matrix generated by 383 cases—a sample size considered to be of adequate power to detect large effects (19). There were no missing data. Model 1 tested whether African American race predicted higher A1C levels after controlling for age, sex, years of education, annual income, insulin use (yes or no), diabetes type, and years of diagnosed diabetes. Model 2 tested whether African American race predicted low literacy skills, low general numeracy skills, and low diabetes-related numeracy skills, and whether these variables, in turn, predicted A1C levels. Finally, an adjustment for other predictors was accounted for in model 3, which tested all predicted pathways to A1C.
RESULTS
Participant characteristics
From March 2004 to November 2005, 615 patients were referred for possible enrollment. Of these, 191 refused participation and 18 were excluded due to poor vision (n = 7), age (n = 4), non–English speaking (n = 2), or other exclusion criteria (n = 5). Of the 406 patients who were consented, 398 (98%) completed the study. Only patients who reported being African American or white were included in the current analysis (n = 383). Characteristics of these patients are presented in Table 1. The associations between patient characteristics were analyzed using the Cuzick nonparametric test for trend across the four diabetes numeracy test score quartiles using Stata 9.0 (20). The median age for the entire sample was 56 years, 50% were male, and 65% were white. Fifty-six percent of the patients reported having greater than a high school level education, 31% had less than a ninth-grade reading level (on REALM), and 69% had less than a ninth-grade level of general numeracy skills (on WRAT-3R). The median (interquartile range) diabetes numeracy test score was 65% (42–81%). The majority of the patients (62%) were on insulin, and the median A1C was 7.2% (6.5–8.3%).
Table 1.
Characteristics of study population and by DNT score quartile
| All subjects | DNT |
|||||
|---|---|---|---|---|---|---|
| Quartile 1 | Quartile 2 | Quartile 3 | Quartile 4 | P* | ||
| Quartile range | [0–42%] | [43–65%] | [66–82%] | [66–82%] | ||
| n | 383 | 104 | 97 | 98 | 84 | |
| Age (years) | 56 (47–64) | 61 (51–67) | 57 (49–66) | 56 (47–62) | 50 (41–56) | <0.001 |
| Female | 193 (50) | 63 (60) | 43 (44) | 49 (50) | 38 (45) | 0.07 |
| Race | ||||||
| White | 249 (65) | 32 (31) | 65 (67) | 77 (79) | 75 (89) | <0.001 |
| Nonwhite | 134 (35) | 72 (69) | 32 (33) | 21 (21) | 9 (11) | |
| Income (n = 375) | ||||||
| <20,000 USD | 166 (44) | 80 (80) | 47 (49) | 23 (23) | 16 (20) | <0.001 |
| ≥20,000 USD | 209 (56) | 20 (20) | 48 (51) | 75 (77) | 66 (80) | |
| Education (n = 377) | ||||||
| Less than high school or GED | 163 (43) | 74 (73) | 47 (49) | 29 (30) | 13 (15) | <0.001 |
| High school or GED or more | 214 (57) | 27 (27) | 49 (51) | 67 (70) | 71 (85) | |
| Private insurance (% yes) | 185 (48) | 32 (31) | 39 (40) | 58 (59) | 56 (67) | <0.001 |
| Literacy status, REALM | ||||||
| Less than ninth grade | 120 (31) | 71 (68) | 30 (31) | 15 (15) | 4 (5) | <0.001 |
| Ninth grade or higher | 263 (69) | 33 (32) | 67 (69) | 83 (85) | 80 (95) | |
| Numeracy, WRAT-3 | ||||||
| Less than ninth grade | 266 (69) | 103 (99) | 84 (87) | 52 (53) | 27 (32) | <0.001 |
| Ninth grade or higher | 117 (31) | 1 (1) | 13 (13) | 46 (47) | 57 (68) | |
| Diabetes: type 2 (% yes) | 327 (85) | 100 (96) | 90 (93) | 86 (88) | 51 (61) | <0.001 |
| Years of diabetes | 9 (3.5–17) | 8 (3–15) | 9 (4–16) | 10 (4–19) | 9 (5–17) | 0.48 |
| Insulin use (% yes) | 236 (62) | 65 (63) | 57 (59) | 51 (52) | 63 (75) | 0.25 |
| BMI (kg/m2) | 32 (28–38) | 33 (28–39) | 33 (29–38) | 31 (28–37) | 32 (26–38) | 0.20 |
| A1C (%) | 7.2 (6.5–8.3) | 7.6 (6.5–9.0) | 7.2 (6.3–8.3) | 7.2 (6.5–8.0) | 7.2 (6.4–8.2) | 0.24 |
Data are medians (interquartile range) or n (%) unless otherwise stated.
*Test for trend (nonparametric) comparing across DNT quartiles.
Test of structural models
Model 1 included eight predictor variables: age, sex (male or female), years of education, annual income, insulin use (no or yes), diabetes type, years of diagnosed diabetes, and race (white or African American); and one outcome variable: A1C. Examination of the path coefficients in this just identified model suggested that younger age (r = −0.21, P < 0.001), using insulin (r = 0.27, P < 0.001), having been diagnosed with diabetes for more years (r = 0.16, P < 0.01), and African American race (r = 0.12, P < 0.01) were associated with higher A1C levels and accounted for 17% of the variability in A1C levels.
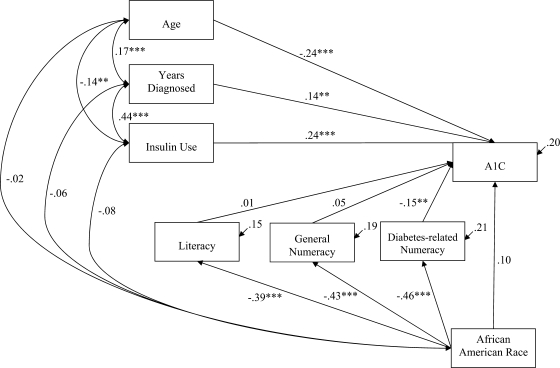
Significant predictors of A1C identified in model 1 were retained in model 2 (Fig. 1), and nonsignificant variables were omitted. Literacy (REALM scores), general numeracy (WRAT-3 scores), and diabetes-related numeracy (DNT scores) were included in model 2 as potential mediators (i.e., explanatory factors) in the predicted pathway from African American race to A1C. Examination of the path coefficients suggested that African American race was associated with limited literacy skills (r = −0.39, P < 0.001), limited general numeracy skills (r = −0.43, P < 0.001), and limited diabetes-related numeracy skills (r = −0.46, P < 0.001). Of these skills, only diabetes-related numeracy significantly predicted A1C levels. Higher diabetes-related numeracy was associated with lower A1C levels (r = −0.15, P < 0.01) and reduced the effect of African American race to nonsignificance (r = 0.10, NS), thereby accounting for the association between African American race and A1C levels. As shown in Fig. 1, the estimated model demonstrated poor fit of the data [χ2 (12, n = 383) = 485.47, P < 0.001, CFI = 0.464, RMSEA = 0.32 (90% CI 0.30–0.35)] likely due to a net effect of constructs in the model (i.e., too many paths being estimated relative to the sample size), not because of the structural relations specified.
Figure 1.
Model 2: initial model (model 1) adding in literacy and numeracy as potential mediators. Coefficients are standardized path coefficients. Overall model fit, χ2 (12, n = 383) = 485.47, P < 0.001, CFI = 0.464, RMSEA = 0.32 (90% CI 0.30–0.35). For tests of significance of individual paths: **P < 0.01, and ***P < 0.001.
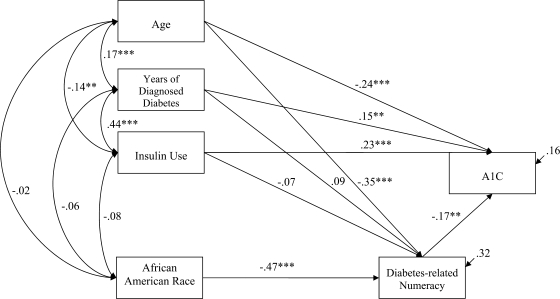
Significant predictors of A1C in model 1 and 2 were retained in model 3, including the significant path from African American race to diabetes-related numeracy, and diabetes-related numeracy to A1C (i.e., the direct path from African American race to A1C was omitted along with omitting literacy and general numeracy from the model). In model 3 (Fig. 2), the relationships between age and diabetes numeracy, insulin use and diabetes numeracy, and years of diagnosed diabetes and diabetes numeracy were added and evaluated. Examination of the path coefficients suggested that, in addition to African American race (r = −0.47, P < 0.001), older age was associated with lower diabetes-related numeracy (r = −0.35, P < 0.001). Insulin use and years of diagnosed diabetes were unrelated to diabetes-related numeracy. As indicated in Fig. 2, the estimated model demonstrated good fit of the data: χ2 (1, n = 383) = 3.02, P = 0.08, CFI = 0.99, RMSEA = 0.07 (90% CI 0.00–0.17).
Figure 2.
Model 3: significant predictors from model 2 adding in age, years of diagnosed diabetes, and insulin use as potential predictors of numeracy. Coefficients are standardized path coefficients. Overall model fit, χ2 (1, n = 383) = 3.02, P = 0.08, CFI = 0.99, RMSEA = 0.07 (90% CI 0.00–0.17). For tests of significance of individual paths: **P < 0.01, and ***P < 0.001.
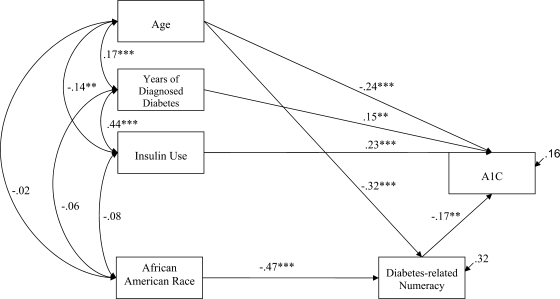
Significant predictors of A1C and diabetes-related numeracy in previous models were retained in a trimmed version of model 3 (i.e., excluding all nonsignificant paths). In the trimmed model, African American race and older age were associated with lower diabetes-related numeracy, accounting for 32% of the variability in diabetes numeracy. Younger age (r = −0.24, P < 0.001), using insulin (r = 0.23, P < 0.001), having been diagnosed with diabetes for more years (r = 0.15, P < 0.01), and having more diabetes-related numeracy (r = −0.47, P < 0.001) were associated with higher A1C levels, accounting for 17% of the variability in A1C. As indicated in Fig. 3, the estimated model demonstrated good fit of the data, χ2 (3, n = 383) = 6.91, P = 0.07, CFI = 0.99, RMSEA = 0.06 (90% CI 0.00–0.12). A χ2 difference test was performed to compare whether the trimmed version of model 3 was significantly different from the full model 3, χ2 difference (2, n = 383) = −3.89 (NS). After dropping the paths from insulin use to diabetes-related numeracy skills, and years of diagnosed diabetes to diabetes-related numeracy in the trimmed model 3, the χ2 difference indicated that compared with the more complex model (full model 3), the more parsimonious model (trimmed model 3) should be retained.
Figure 3.
Model 3: trimmed to significant predictors. Coefficients are standardized path coefficients. Overall model fit, χ2 (3, n = 383) = 6.91, P = 0.07, CFI = 0.99, RMSEA = 0.06 (90% CI 0.00–0.12). For tests of significance of individual paths, *P < 0.05, **P < 0.01, and ***P < 0.001.
CONCLUSIONS
Understanding the reasons and eliminating the pervasive health disparities across race and ethnicity is a major research, clinical, and health policy goal (21). Consistent with prior work (22), we found that African American race predicted poor glycemic control. Uniquely, we found that diabetes-related numeracy reduced the explanatory power of African American race, such that diabetes-related numeracy, not African American race, significantly predicted glycemic control. To our knowledge, our study is the first to examine health literacy, general numeracy, and diabetes numeracy as mediators of the relationship between African American race and poor glycemic control.
The relationship between African American race and glycemic control is likely due to a complex interaction between many patient, provider, and system-level factors (23). Recently, it has been suggested that physician-level factors may explain the relationship between race and glycemic control (23). The same authors also acknowledge that up to 38% of racial differences in glycemic control may be due to patient sociodemographic factors (23), but this analysis did not include a measure of education. Given the often-recommended and required patient self-adjustment of diabetes therapy, which relies heavily on numeracy skills, we believe diabetes numeracy is an important patient-level factor to consider when exploring disparities in diabetes. According to our study findings, diabetes numeracy indeed may be a significant contributor to mediating the relationship between race disparities and glycemic control.
The findings of this study also suggest that patients who are older or African American are at particularly higher risk of lower diabetes numeracy skills, and, in turn, worse glycemic control. Lower numeracy could be, in part, due to 1) opportunity factors (e.g., coursework), 2) propensity factors (e.g., prerequisite skills), and 3) distal factors (e.g., SES) (24). Identification of patients with lower diabetes numeracy skills may allow for the implementation of diabetes educational programs tailored to a patient's individual needs (25). Further research is needed to determine the impact of literacy and numeracy-sensitive diabetes care programs on diabetes outcomes, with special attention to a possible role in the reduction of racial disparities in glycemic control.
Although literacy has been shown to reduce the effect of African American race on other health outcomes (1,2), it did not explain the association between African American race and A1C in our study. In fact, literacy, as measured by the REALM, was unrelated to A1C. One explanation may be that for patients with diabetes, reading skill or literacy, while necessary, may not sufficiently capture all of the complexities related to the needs of day-to-day diabetes care. Yet, accurate interpretation and application of quantitative information is likely required for successful diabetes medication, dietary, and glucose monitoring management. Another possibility is that our measure of literacy, the REALM, while well validated, may not assess patient's literacy level to the most specific level possible, especially for patients with more advanced skills (i.e., ceiling effect).
There are limitations in our study that should be acknowledged. First, although structural equation modeling proposes a causal relationship between variables, the current study measured all variables cross-sectionally and, thus, can most appropriately speak to associations between variables observed at a single point in time, not causality. Future research is needed to investigate the longitudinal effects of these variables on changes in glycemic control over time. Second, whereas the DNT was designed to measure patients' existing diabetes-related numeracy skills, performance on the DNT may also reflect differences in diabetes knowledge, prior diabetes education, or differences in provider management and communication. Third, although the structural models adjusted for many potential confounding variables, there remains the possibility of residual confounding. Finally, this study excluded non–English-speaking participants, who may be at high risk for limited diabetes-related numeracy skills and worse glycemic control. Despite these limitations, our study is the first to assess the impact of literacy, general numeracy, and diabetes-related numeracy in explaining racial differences in glycemic control in a diverse patient population.
Low diabetes-related numeracy presents a wide-reaching barrier to successful disease management that is potentially modifiable. The development of educational programs and adaptive tools designed to facilitate effective patient-provider communication and accommodate patients with low numeracy skills could potentially be a useful approach to improving glycemic control. In addition, these improvements may help decrease well-noted racial disparities in glycemic control and, ultimately, also contribute to reducing racial disparities in the development of diabetes complications and related mortality. Future research should explore the role of numeracy-focused interventions in reducing racial disparities in diabetes outcomes.
Acknowledgments
This research was funded with support from the American Diabetes Association (Novo Nordisk Clinical Research Award), the Pfizer Clear Health Communication Initiative, and the Vanderbilt Diabetes Research and Training Center (NIDDK 5P60DK020593). C.Y.O. was supported by a Diversity Supplement Award (NIDDK 3P60DK020593). R.L.R. (NIDDK 1 K23 DK080952 DK065294) and K.C. (NIDDK 1 K23 DK080952) were supported by Career Development Awards.
No potential conflicts of interest relevant to this article were reported.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
See accompanying editorial, p. 1746.
References
- 1.Wolf MS, Knight SJ, Lyons EA, Durazo-Arvizu R, Pickard SA, Arseven A, Arozullah A, Colella K, Ray P, Bennett CL: Literacy, race, and PSA level among low-income men newly diagnosed with prostate cancer. Urology 2006; 68: 89– 93 [DOI] [PubMed] [Google Scholar]
- 2.Osborn CY, Paasche-Orlow MK, Davis TC, Wolf MS: Health literacy: an overlooked factor in understanding HIV health disparities. Am J Prev Med 2007; 33: 374– 378 [DOI] [PubMed] [Google Scholar]
- 3.Institute of Medicine: Health Literacy: A Prescription to End Confusion Washington, DC, National Academies Press, 2004 [PubMed] [Google Scholar]
- 4.Williams MV, Baker DW, Parker RM, Nurss JR: Relationship of functional health literacy to patients' knowledge of their chronic disease: a study of patients with hypertension and diabetes. Arch Intern Med 1998; 158: 166– 172 [DOI] [PubMed] [Google Scholar]
- 5.Rothman R, Malone R, Bryant B, Dewalt D, Pignone M: Association of health literacy with diabetes outcomes (comment). JAMA 2002; 288: 2687– 2688 [PubMed] [Google Scholar]
- 6.Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, Palacios J, Sullivan GD, Bindman AB: Association of health literacy with diabetes outcomes. JAMA 2002; 288: 475– 482 [DOI] [PubMed] [Google Scholar]
- 7.Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J: Health literacy and mortality among elderly persons. Arch Intern Med 2007; 167: 1503– 1509 [DOI] [PubMed] [Google Scholar]
- 8.Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR: The prevalence of limited health literacy. J Gen Intern Med 2005; 20: 175– 184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rothman RL, Housam R, Weiss H, Davis D, Gregory R, Gebretsadik T, Shintani A, Elasy TA: Patient understanding of food labels: the role of literacy and numeracy. Am J Prev Med 2006; 31: 391– 398 [DOI] [PubMed] [Google Scholar]
- 10.Kutner M, Greenberg E, Jin Y, Paulsen C: The Health Literacy of America's Adults: results from the 2003 National Assessment of Adult Literacy, 2006. ( pub. no. NCES 2006483) [Google Scholar]
- 11.Rothman RL, Montori VM, Cherrington A, Pignone MP: Perspective: the role of numeracy in health care. J Health Commun 2008; 13: 583– 595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Apter AJ, Cheng J, Small D, Bennett IM, Albert C, Fein DG, George M, Van Horne S: Asthma numeracy skill and health literacy. J Asthma 2006; 43: 705– 710 [DOI] [PubMed] [Google Scholar]
- 13.Huizinga MM, Elasy TA, Wallston KA, Cavanaugh K, Davis D, Gregory RP, Fuchs LS, Malone R, Cherrington A, Dewalt DA, Buse J, Pignone M, Rothman RL: Development and validation of the Diabetes Numeracy Test (DNT). BMC Health Serv Res 2008; 8: 96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huizinga MM, Beech BM, Cavanaugh KL, Elasy TA, Rothman RL: Low numeracy skills are associated with higher BMI. Obesity (Silver Spring) 2008; 16: 1966– 1968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cavanaugh K, Huizinga MM, Wallston KA, Gebretsadik T, Shintani A, Davis D, Gregory RP, Fuchs L, Malone R, Cherrington A, Pignone M, DeWalt DA, Elasy TA, Rothman RL: Association of numeracy and diabetes control. Ann Intern Med 2008; 148: 737– 746 [DOI] [PubMed] [Google Scholar]
- 16.Davis TC, Crouch MA, Long SW, Jackson RH, Bates P, George RB, Bairnsfather LE: Rapid assessment of literacy levels of adult primary care patients. Fam Med 1991; 23: 433– 435 [PubMed] [Google Scholar]
- 17.Wilkinson GS: WRAT3: Wide Range Achievement Test Administration Manual Wilmington, DE, Wide Range, 1993 [Google Scholar]
- 18.Ridgon E: CFI versus RMSEA: comparison of two fit indexes for structural equation modeling. Structural Equation Modeling 1996; 3: 369– 379 [Google Scholar]
- 19.Kline R: Principles and Practice of Structural Equation Modeling New York, Guilford, 2004 [Google Scholar]
- 20.Cuzick J: A Wilcoxon-type test for trend. Stat Med 1985; 4: 87– 90 [DOI] [PubMed] [Google Scholar]
- 21.Lurie N, Jung M, Lavizzo-Mourey R: Disparities and quality improvement: federal policy levers. Health Aff 2005; 24: 354– 364 [DOI] [PubMed] [Google Scholar]
- 22.Gary TL, McGuire M, McCauley J, Brancati FL: Racial comparisons of health care and glycemic control for African American and white diabetic adults in an urban managed care organization. Dis Manag 2004; 7: 25– 34 [DOI] [PubMed] [Google Scholar]
- 23.Sequist TD, Fitzmaurice GM, Marshall R, Shaykevich S, Safran DG, Ayanian JZ: Physician performance and racial disparities in diabetes mellitus care. Arch Intern Med 2008; 168: 1145– 1151 [DOI] [PubMed] [Google Scholar]
- 24.Byrnes JP, Miller DC: The relative importance of predictors of math and science achievement: an opportunity-propensity analysis. Contemporary Educational Psychology 2007; 32: 599– 629 [Google Scholar]
- 25.Wolff K, Cavanaugh K, Malone R, Hawk V, Gregory BP, Davis D, Wallston K, Rothman RL: The Diabetes Literacy and Numeracy Education Toolkit (DLNET): Materials to facilitate diabetes education and management in patients with low literacy and numeracy skills. Diabetes Educ 2009; 35: 233– 245 [DOI] [PMC free article] [PubMed] [Google Scholar]