Abstract
OBJECTIVE
We evaluated whether a whey preload could slow gastric emptying, stimulate incretin hormones, and attenuate postprandial glycemia in type 2 diabetes.
RESEARCH DESIGN AND METHODS
Eight type 2 diabetic patients ingested 350 ml beef soup 30 min before a potato meal; 55 g whey was added to either the soup (whey preload) or potato (whey in meal) or no whey was given.
RESULTS
Gastric emptying was slowest after the whey preload (P < 0.0005). The incremental area under the blood glucose curve was less after the whey preload and whey in meal than after no whey (P < 0.005). Plasma glucose-dependent insulinotropic polypeptide, insulin, and cholecystokinin concentrations were higher on both whey days than after no whey, whereas glucagon-like peptide 1 was greatest after the whey preload (P < 0.05).
CONCLUSIONS
Whey protein consumed before a carbohydrate meal can stimulate insulin and incretin hormone secretion and slow gastric emptying, leading to marked reduction in postprandial glycemia in type 2 diabetes.
The rate of gastric emptying and the incretin, glucagon-like peptide 1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP), response to a meal are known to be major determinants of postprandial blood glucose excursions (1,2). One strategy to minimize postprandial glycemia could be to administer a small load of protein or fat before a meal, so that the presence of nutrients in the small intestine induces the release of peptides such as GLP-1, GIP, and cholecystokinin (CCK) to slow gastric emptying and stimulate insulin secretion in advance of the main nutrient load (3,4). We hypothesized that a protein preload would reduce the postprandial glycemic excursion in type 2 diabetic patients by these mechanisms.
RESEARCH DESIGN AND METHODS
The protocol included eight diet-controlled type 2 diabetic patients (seven male, mean ± SE age 58 ± 3 years, BMI 28.6 ± 1.3 kg/m2, duration of known diabetes 5.4 ± 1.1 years, and A1C 6.5 ± 0.2%) who attended the laboratory after an overnight fast (14 h for solids and 12 h for liquids) on three separate occasions. Each patient consumed beef-flavored soup (3.8 g noncaloric beef flavoring dissolved in 350 ml water) 30 min before a mashed potato meal containing 65 g powdered potato (Deb Instant Mashed Potato, Epping, Australia) with 20 g glucose (total: 59.1 g carbohydrate, 4.3 g fat, 5.2 g protein; 1,276.5 kJ), labeled with 20 MBq 99mTc-sulfur colloid (4). On one day, 55 g whey protein (876.7 kJ) was added to the soup. On another day, 55 g whey was mixed into the potato meal. On a third day, neither the preload nor the meal contained whey. Blood was sampled frequently for blood glucose and plasma hormone measurements.
Measurements
Gastric emptying was assessed by scintigraphy. Data were corrected for radionuclide decay, subject movement, and γ-ray attenuation, and the gastric half-emptying time (T50) was calculated (4).
Blood glucose concentrations were measured using a glucometer (Medisense Precision QID; Abbott Laboratories, Bedford, MA), which we have validated against the hexokinase technique (5). Plasma insulin was measured by enzyme-linked immunosorbent assay (ELISA; Diagnostic Systems Laboratories, Webster, TX). Total GLP-1 (GLPIT-36HK; Linco Research, St. Charles, MO), total GIP, and CCK-8 were measured by radioimmunoassay (6).
Cardiovascular autonomic function was assessed by the variation in R-R interval during deep breathing and the systolic blood pressure changes in response to standing (7).
Data were evaluated using repeated-measures ANOVA with treatment and time as factors (StatView 5.0; Abacus Concepts, Berkeley, CA). Data are shown as means ± SE; P < 0.05 was considered significant.
RESULTS
Two of the eight subjects had definite autonomic dysfunction. The study was well tolerated.
On the no whey and whey in meal days, emptying was rapid initially and subsequently slower, whereas emptying after the whey preload approximated a linear pattern. Gastric emptying was slowest on the whey preload day (T50: 87.3 ± 5.4 min; P = 0.0001) and was slower with whey in the meal (53.0 ± 8.3 min; P < 0.01) than with no whey (39.0 ± 6.2 min).
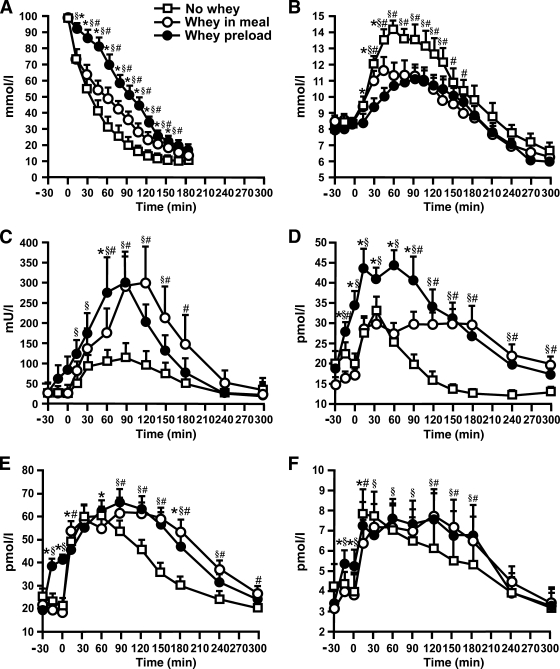
There were no differences in baseline blood glucose, plasma insulin, GLP-1, GIP, or CCK concentrations (Fig. 1). The incremental area under the curve (iAUC) for blood glucose was less after the whey preload (363.7 ± 64.5 mmol · min−1 · l−1) and whey in meal (406.3 ± 85.9 mmol · min−1 · l−1) compared with no whey (734.9 ± 98.9 mmol · min−1 · l−1; P < 0.005 for both). The iAUCs for insulin, GLP-1, GIP, and CCK were greater when whey was given as a preload (P < 0.05 for all) or in the meal (P < 0.005 for all) compared with no whey. Despite an earlier response, the iAUC for insulin did not differ between whey preload and whey in meal (P = 0.50). GLP-1 was greater between −15 min and 90 min with the whey preload compared with whey in meal (P = 0.0001), but the overall iAUC did not differ significantly.
Figure 1.
Gastric emptying (A), concentrations of blood glucose (B), plasma insulin (C), plasma GLP-1 (D), plasma GIP (E), and plasma CCK (F) in response to a mashed potato meal in eight type 2 diabetic patients. On each study day, subjects ingested 350 ml beef-flavored soup 30 min before a radiolabeled mashed potato meal; 55 g whey protein was added either to the soup (whey preload) or to the potato (whey in meal) or no whey was given (no whey). Data are means ± SE. *P < 0.05, whey preload vs. whey in meal; #P < 0.05, whey in meal vs. no whey; §P < 0.05, whey preload vs. no whey.
CONCLUSIONS
We demonstrated that whey protein, when given before or with a high-carbohydrate meal, resulted in a substantial reduction in postprandial glycemia in diet-controlled type 2 diabetic patients. Given that the magnitude of the reduction was comparable with what would be hoped for using pharmacological therapy, such as sulfonylureas, these data have considerable implications for nutritional strategies in the management of diabetes.
The pivotal role of the gastrointestinal tract in determining postprandial glycemia has often been overlooked, but it is assuming increasing prominence, partly because of the development of gut peptide–based therapies for diabetes, such as the GLP-1 analog exenatide (8) and the amylin analog pramlintide (9), which may act predominantly by slowing gastric emptying. Similar to what we reported after an oil preload (4), whey slowed gastric emptying substantially, in particular when given before the meal, and is associated with the stimulation of GLP-1 and CCK. However, in contrast to the delayed insulin response observed after oil, whey augmented insulin secretion markedly, possibly by a combination of the incretin effect and the direct stimulation of the β-cells by absorbed amino acids (10). It is likely that the stimulation of insulin by whey was responsible for the much greater reduction in glycemia after whey than after oil, given that the effects on gastric emptying were comparable.
Although our study involved a small number of subjects who had well-controlled, predominantly uncomplicated type 2 diabetes, the improvement in postprandial glycemia was marked and highly consistent. Further evaluation is now required in poorly controlled patients and those taking oral hypoglycemic agents in order to determine whether the acute effects are sustained in the longer term. It would also be important to confirm whether the effects are evident with a smaller load of protein in order to minimize additional energy intake. Although concerns have been raised about hyperinsulinemia as a risk factor for vascular disease (11), it is more likely that it represents a marker for other risk factors (12), and in the UK Prospective Diabetes Study (UKPDS), stimulation of insulin by sulfonylureas was not associated with increased cardiovascular events (13).
The concept of using dietary manipulations to treat type 2 diabetes, based on our knowledge of the contribution of gastric emptying and gut peptides to postprandial glycemic responses, appears to hold much promise.
Acknowledgments
This work was supported by the National Health and Medical Research Council (NHMRC) of Australia. The salary of K.L.J. is also funded by the NHMRC.
No potential conflicts of interest relevant to this article were reported.
Parts of this study were presented in abstract form at Digestive Diseases Week, San Diego, California, 17–22 May 2008. Complete data have been submitted for presentation at the annual meeting of the European Association for the Study of Diabetes, Vienna, Austria, 29 September–2 October 2009
We thank Murray Goulburn for supply of the whey protein isolate and Jane Bowen for advice about formulating the preloads.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1.Chaikomin R, Rayner CK, Jones KL, Horowitz M: Upper gastrointestinal function and glycemic control in diabetes mellitus. World J Gastroenterol 2006; 12: 5611– 5621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rayner CK, Samsom M, Jones KL, Horowitz M: Relationships of upper gastrointestinal motor and sensory function with glycemic control. Diabetes Care 2001; 24: 371– 381 [DOI] [PubMed] [Google Scholar]
- 3.Bowen J, Noakes M, Trenerry C, Clifton PM: Energy intake, ghrelin, and cholecystokinin after different carbohydrate and protein preloads in overweight men. J Clin Endocrinol Metab 2006; 91: 1477– 1483 [DOI] [PubMed] [Google Scholar]
- 4.Gentilcore D, Chaikomin R, Jones KL, Russo A, Feinle-Bisset C, Wishart JM, Rayner CK, Horowitz M: Effects of fat on gastric emptying of and the glycemic, insulin, and incretin responses to a carbohydrate meal in type 2 diabetes. J Clin Endocrinol Metab 2006; 91: 2062– 2067 [DOI] [PubMed] [Google Scholar]
- 5.Horowitz M, Edelbroek MA, Wishart JM, Straathof JW: Relationship between oral glucose tolerance and gastric emptying in normal healthy subjects. Diabetologia 1993; 36: 857– 862 [DOI] [PubMed] [Google Scholar]
- 6.Santangelo A, Peracchi M, Conte D, Fraquelli M, Porrini M: Physical state of meal affects gastric emptying, cholecystokinin release and satiety. Br J Nutr 1998; 80: 521– 527 [DOI] [PubMed] [Google Scholar]
- 7.Ewing DJ, Clarke BF: Diagnosis and management of diabetic autonomic neuropathy. Br Med J (Clin Res Ed) 1982; 285: 916– 918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Linnebjerg H, Park S, Kothare PA, Trautmann ME, Mace K, Fineman M, Wilding I, Nauck M, Horowitz M: Effect of exenatide on gastric emptying and relationship to postprandial glycemia in type 2 diabetes. Regul Pept 2008; 151: 123– 129 [DOI] [PubMed] [Google Scholar]
- 9.Kong MF, King P, Macdonald IA, Stubbs TA, Perkins AC, Blackshaw PE, Moyses C, Tattersall RB: Infusion of pramlintide, a human amylin analogue, delays gastric emptying in men with IDDM. Diabetologia 1997; 40: 82– 88 [DOI] [PubMed] [Google Scholar]
- 10.Fieseler P, Bridenbaugh S, Nustede R, Martell J, Orskov C, Holst JJ, Nauck MA: Physiological augmentation of amino acid-induced insulin secretion by GIP and GLP-I but not by CCK-8. Am J Physiol 1995; 268: E949– E955 [DOI] [PubMed] [Google Scholar]
- 11.Reaven GM: Insulin resistance and compensatory hyperinsulinemia: role in hypertension, dyslipidemia, and coronary heart disease. Am Heart J 1991; 121: 1283– 1288 [DOI] [PubMed] [Google Scholar]
- 12.Wingard DL, Barrett-Connor EL, Ferrara A: Is insulin really a heart disease risk factor? Diabetes Care 1995; 18: 1299– 1304 [DOI] [PubMed] [Google Scholar]
- 13.UK Prospective Diabetes Study (UKPDS) Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998; 352: 837– 853 [PubMed] [Google Scholar]