Abstract
Objective
The purpose of this study is to reassess the projected rate of Electronic Health Record (EHR) diffusion and examine how the federal government's efforts to promote the use of EHR technology have influenced physicians' willingness to adopt such systems. The study recreates and extends the analyses conducted by Ford et al. 1 The two periods examined come before and after the U.S. Federal Government's concerted activity to promote EHR adoption.
Design
Meta-analysis and bass modeling are used to compare EHR diffusion rates for two distinct periods of government activity. Very low levels of government activity to promote EHR diffusion marked the first period, before 2004. In 2004, the President of the United States called for a “Universal EHR Adoption” by 2014 (10 yrs), creating the major wave of activity and increased awareness of how EHRs will impact physicians' practices.
Measurement
EHR adoption parameters—external and internal coefficients of influence—are estimated using bass diffusion models and future adoption rates are projected.
Results
Comparing the EHR adoption rates before and after 2004 (2001–2004 and 2001–2007 respectively) indicate the physicians' resistance to adoption has increased during the second period. Based on current levels of adoption, less than half the physicians working in small practices will have implemented an EHR by 2014 (47.3%).
Conclusions
The external forces driving EHR diffusion have grown in importance since 2004 relative to physicians' internal motivation to adopt such systems. Several national forces are likely contributing to the slowing pace of EHR diffusion.
Introduction
In 2004, then President Bush 2,3 established a goal for implementing electronic health records (EHRs) nationwide within ten years. President Obama has also adopted the 2014 target date and promised more funding to achieve the goal. 2 There has been a significant amount of research and rhetoric surrounding the issue in both the scientific and mainstream media since the 2014 goal was initially proposed. Researchers have developed in-depth EHR surveys that assess general adoption rates among practices as well as levels of EHR functionality and system interoperability. 3–6 As to the rhetoric, both EHR proponents and detractors have been putting more stories into the media speculating on whether the 2014 goal will be met or should even be the focus of government efforts. 7,8
In May of 2008 in an interview with The Hill, Health and Human Services Secretary Mike Leavitt stated, “I believe that [the 10-year plan for EHR adoption] will be accomplished. I think the goal may be exceeded” (http://thehill.com/business–lobby/qa-with-mike-leavitt-2008-05-07.html). The other side of the discussion characterizes physicians resisting the adoption of EHR technologies because they are perceived as a potential threat to their professional autonomy 9–12 and fail to provide an adequate return on investment (ROI). 13 Within the context of these two perspectives lies the reality that most physicians will use an EHR system eventually. Given the eventuality of adoption, the questions of timing and conflict emerge. When will EHR's be widely adopted? Additionally, it is unclear how the dynamic of external pressure versus internal resistance will shape that time frame. Is the push for adoption by policymakers, purchasers and EHR advocates helping or hurting the cause?
The current study replicates and then extends an earlier meta-analysis conducted by Ford, Menachemi and Phillips 1 to explore changes in the external and internal motivators driving physicians in small practices to adopt EHR systems. The earlier study was based on survey data gathered before President Bush's 2004 announcement and the concomitant increase in government programs designed to accelerate EHR adoption since. This study analyzes three years of additional survey data (2005–2007) drawn from this period of increased government activity and significant discussion in the medical literature related to the EHR's pros and cons.
This updated study has two aims. First, we quantify and graphically depict the historic trend of EHR adoption among United States physicians in small practices (10 or fewer members) by applying diffusion modeling techniques 14 to EHR adoption estimates from thirteen 13 previous studies. 3,15–26 Based on that information, we extrapolate future implementation trends and discuss the two factors that drive the diffusion process—internal and external social influences. 27 Second, based on published studies and the derived models, we discuss the most probable time horizon for achieving ubiquitous EHR adoption and the impact of government efforts promoting adoption on physicians' attitudes.
The current study makes three new contributions to the EHR research literature and policy debate. First, it allows policy makers to better understand how external and internal influences in the small practice setting will affect EHR adoption among physicians. Second, it provides an updated benchmark that can be further used for planning and evaluating EHR adoption incentive programs that target small practices. Because small medical practices' are expected to be the last setting to widely adopt EHR technology, 28 they in effect become the leading indicator for achieving a universally paperless outpatient health system by 2014. The current study also provides a continual means for systematically quantifying and tracking that indicator. Finally, the present study empirically estimates future adoption scenarios using the Technology Diffusion Model.
Background—the Technology Diffusion Model (TDM)
Rogers 27 is credited with creating the technology diffusion theory that describes innovators (i.e., first adopters), early adopters, early majority, late majority, and laggards' adoption pattern. Further research by Bass 14 empirically modeled the factors that predict new technologies' diffusion patterns as a function of External and Internal Influences. External influences, commonly labeled in the diffusion literature as innovation factors, are driven by information from a source outside the potential adopter's social system. Internal influences on a provider's decision to adopt a new technology, within their social system and are often referred to as social contagions in the diffusion literature. 29
The social components of diffusion, rather than economic or external factors, play a major role in consumers' decisions to adopt a technology. 30 It is commonly accepted that new product diffusion is often driven by social contagion, in other words, that actors' adoptions are a function of their exposure to other actors' knowledge, attitudes, or behaviors concerning the new product. Researchers have offered different theoretical accounts of social contagion, including social learning under uncertainty, social-normative pressures, competitive concerns, and performance network effects (van den Bulte and Lilien 2001).
Bass 14 was the first to develop commercial applications of such diffusion models. His models were developed to predict the uptake of consumer products based on the influence of various types of advertising campaigns. The bass model predicts how many customers will eventually adopt a new product, and when they will do so, based on early market penetration rates. The basic formula for calculating the percentage of adopters at any point, using discrete time notation, can be written as, 31 where:
| (1) |
F(t) = the number of adoptions occurring in period t,
p = coefficient of innovation, capturing the intrinsic tendency to adopt, and the effect of time invariant external influences,
q = coefficient of imitation or social contagion, capturing the extent to which the probability that one adopts (given that one has not yet done so) increases with the proportion of eventual adopters who have already opted in, and
t = period of measurement.
The model has several advantageous properties. For example, given multiple time point measurements, it is possible to solve for p and q. The parameters p and q provide information about the rate of diffusion. A high value for p indicates that the diffusion has a quick start but also tapers off quickly. A high value of q indicates that the diffusion starts slow but later accelerates. When q is larger than p, the cumulative number of adopters F(t) + F(t-1) follows the type of S-shaped curve often observed for high risk, innovative products that take extended time frames to become widely used. When q is smaller than p, the cumulative number of adopters follows an inverse J-shaped curve often observed for less risky innovations, such as the adoption of new consumer durables (e.g., washers and dryers). Once p and q are known, the time (t*) at which the peak adoption rate occurs (i.e., the period when the largest number of individuals adopts) can be calculated as 32
| (2) |
This calculation is commonly referred to as the inflection or “tipping point” 29 when the diffusion paradigm becomes self-sustaining.
Once sufficient data on adoption level becomes available, usually after three or more periods, researchers can estimate p and q using the basic bass model (Eq 1). In the case of EHRs, empirically derived point estimates of medical practices' adoption levels have been measured annually since 2001—albeit using a variety of instruments and sampling frames. These studies are described in the next section.
Methods
Data Sources
Data for the current analyses were drawn from thirteen 13 previous studies conducted between 2001 and 2008 (see ▶). Early studies tended to use independently developed survey instruments and sampling designs. The idiosyncratic nature of early surveys meant there was no clear agreement on what constituted adoption. In addition, many studies focused on either a specific geographic area or on a particular type of practice defined either by size, specialty, setting (ambulatory v. hospital based), or some combination. Therefore, the early studies have the potential for a wide range of point estimates for EHR adoption. Despite the inconsistencies in research designs, most of the early studies' findings tend to track with the pattern the Technology Diffusion Model (TDM) predicted by our previous analysis. 1 Further, they were also consistent with the Heuristic estimates, or “best-guesses”, of physicians' EHR adoption levels being discussed at the time. 33,34
Table 1.
Table 1 Studies of EHR Adoption in the Small Practice Setting 2001–2007
| Authors, Date Published | Year Collected | Sample | Methodology | Comments | Average EHR Adoption Proportion | EHR Adoption Proportion (By Practice Size) |
|---|---|---|---|---|---|---|
| 17 | 2001 | 1,200 physicians | Survey | 12.9% | ||
| 59 | 2002 | 1,328 Indiana Family Physicians | Survey; 51.7% response rate, n = 687 | 14.4% | ||
| 21 | 2003 | 1,008 group practices | Survey | Study looked at practices′, rather than physicians' adoption rates. In addition, smaller practices had lower rates but were not broken-out in the reporting. Therefore, the estimates may be inflated in two dimensions. | 17.1% | |
| (60) Commonwealth Fund's study | 2003 | 3,598 randomly selected physicians | Survey; 52.8% response rate, n = 1,837 | Generally, considered the first national study with both high methodological and sampling reliability. | 18% |
|
| 18 | 2003 | 116 primary care physicians in the Kentucky Ambulatory Research Network | Survey; 51% response rate, n = 59 | Sample of physicians may represent a market segment likely to be “Early Adopters” of technology; therefore the estimate may be inflated | 21% | |
| 61 | 2003 | 2,011 doctors, primarily practices in office | Survey; 55% response rate, n = 1,114 | Most respondents were from small practices, but the mix is unclear, therefore the estimate may be slightly inflated according to the authors. | 17.2% | |
| Terry, 2005 | 2004 | 10,000 offices based MDs and DOs | Mail survey; 19% response rate, n = 1,916 | The sampling frames were not disclosed; therefore, it is not possible to aggregate the small practices mathematically. | ∼ |
|
| Menachemi and Brooks 2006 | 2004 | Physicians in Florida | Mail survey; 28.2% response rate; n = 4,203 | The study provided the weighting, but cut the practice size at 9 rather than the more commonly used 10 physicians. | 19.5% |
|
| Simon, Kaushal, Cleary, et al, 2007 | 2005 | Massachusetts | Mail survey n = 1,345 71.4% response rate | The survey did provide the weighting information necessary to make an accurate estimate. The authors cautioned that their state was likely to have an EHR adoption rate well above the national average. | 28.8% |
|
| Hing and Burt, 2008 | 2005 | CDC conducted survey of 3,000 office based physicians | n = 1,281 | Minimum required features include computerized prescription ordering, computerized test ordering, electronic results and electronic physician clinical notes |
|
|
| Hing, Burt, and Woodwell, 2007 | 2006 | CDC conducted survey of 3,350 office based physicians | n = 1,311 (61.9%) |
|
|
|
| California Healthcare Foundation, 2008 | 2007 | 1,000 California physicians from the American Medical Association's Masterfile | Mail survey, 39% | The methodology used to estimate the national average is unclear. |
|
|
| Desroches, et al, 2008 | 2007 | Physicians randomly drawn from the American Medical Association's Physician Masterfile; focus on the minimally functional EHR. | n = 2,758 | This report's definition of a “Minimally Functional EHR” required the availability of far more features than most of the prior literature. It included: clinical notes, record orders for prescriptions, laboratory tests, radiological examinations, view laboratory and imaging results. Had the authors applied a definition similar to prior research their estimates would have been consistent with earlier estimates. | 13% had the minimum required features to be considered an “system” |
|
More recent studies have been more rigorous in their item development and sampling strategies. The surveys conducted by the Commonwealth Fund 15 and the Centers for Disease Control and Prevention (CDC, 19 ) have high scores for methodological rigor and sampling representativeness. 35 The CDC's instrument, the National Ambulatory Medical Care Survey (NAMCS), has the added benefit of being fielded annually. Therefore, it is the most reliable and valid longitudinal assessment of EHR adoption by physicians in small practices. 36
Using published data, point estimates for EHR adoption rates were obtained. For example, empiric studies of EHR adoption conducted in both 200117 and 200220 served as those periods' estimates. Additionally, there were four separate studies conducted during 2003. 15,18,19,21 The Audet et al 15 study is the most extensive to date and found that between 18 and 24% of physicians' in small practices used EHRs routinely in their offices during 2003. The other three studies' estimates also fell within that range. Therefore, the four studies' estimates of office based EHR use, in practices with less than 10 practitioners were averaged and gave a point estimate of 18.325% (s.d. = 1.828). For the years after 2003, the NACMS studies' results were given greater weighting. Nevertheless, where other surveys were available, those findings have been included in ▶.
In 2008, another large-scale study 3 was released that recalibrated the definition (based on the level of EHR functionality required) to classify a physician as having adopted the technology. The study received a significant amount of attention in the popular press because it represented a dramatic reduction in the prevalence of EHRs compared to earlier estimates. However, the findings have limited value as a benchmark because they are based a new definition that is inconsistent with previous work studying EHR adoption. Therefore, for the purposes of this research, the DesRoaches et al study's estimate has not been used.
Given the point estimates used in our models, it is possible to empirically derive the diffusion curves' historical shape, potential future trends, and the external (p) and internal (q) influence coefficients.
Diffusion Estimation Technique
The statistical extrapolation was conducted in Microsoft Excel using the linear optimization tool. The objective was to have unique estimates for the External and Internal Influence coefficients that approximated the known adopter percentages as closely as possible for all three years. The objective function was the summed differences between estimated and actual adoption levels for the all known years, and the target value was zero—or as close to zero as possible. One constraint was applied to the optimization routine. The difference between the actual and estimated percentages of adopters for any year had to be less than 0.5% in absolute terms.
All the studies analyzed provided either current adoption level ranges or enough information to calculate the standard deviation of estimates for that year. For 2003, the year with four separate analyses, the standard deviation of the individual estimates was calculated (s.d. = 1.828). The 2001 and 2002 studies' standard deviations were 0.75 and 1.75 respectively. The standard deviation was added to the “Best” estimate to create an “Optimistic” diffusion curve estimate; then subsequently the standard deviation was subtracted from the “Best” estimate to create a “Conservative” diffusion curve—using the linear optimization approach described above. For the studies conducted since 2004, the NAMCS was given the heaviest weighting when it was available.
Results
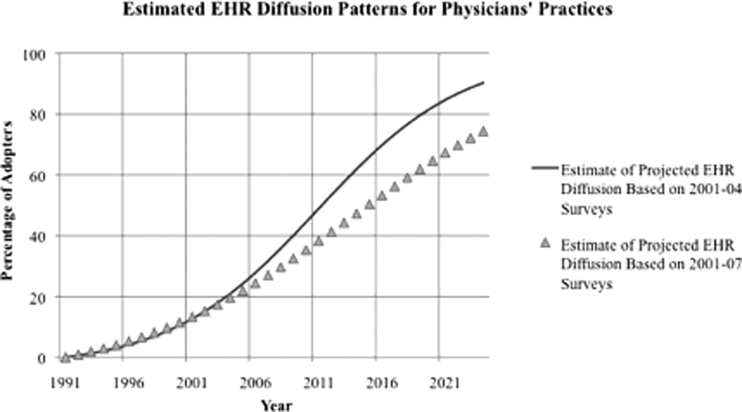
Using Eq 1 and linear optimization, the coefficients of external (p) and internal (q) influences were estimated for two time periods. ▶ presents the two different diffusion scenarios' external and internal influence coefficients, the ratio of external to internal influence, their tipping points (Eq 2), and the projected adoption levels in 2014. The scenario based on the 2001–2004 estimate displays the characteristic S-shaped curve that is indicative that the technology is likely to achieve significant market penetration, given enough time (see ▶). The diffusion profile based on 2001 through 2007 surveys is far shallower than the earlier estimate indicating that external pressures to adopt are increasing relative to potential adopters' desire to have an EHR system in their practice.
Table 2.
Table 2 Diffusion Coefficient Estimates, Tipping Points, and 2014 Adoption Rates
| Scenarios | External Diffusion Coefficient (p) | Internal Diffusion Coefficient (q) | p/q Ratio | Tipping Point | 2014 Adoption Percentage |
|---|---|---|---|---|---|
| Estimate based on 2001–2003 Surveys | 0.0054 | 0.1673 | 0.0323 | 2011 | 61.94% |
| Estimate based on 2001–2007 Surveys | 0.0083 | 0.1038 | 0.0800 | 2014 | 47.33% |
Figure 1.
Two Estimates of EHR Diffusion.
The external diffusion coefficient estimates for EHRs were relatively large in the analysis conducted on the 2001–2003 studies (p = 0.0054) compared to other medical equipment technologies'—such as ultrasound imaging (p = 0.000) and mammography (p = 0.000)—both of which diffused quickly. 37,38 For the period 2001–2007 the external coefficient of influence increased to 0.0083 indicating that factors such as policy pressure, EHR vendors' marketing efforts and public discourse were playing a larger role than in the earlier time frame.
Compared to other medical technologies that diffused rapidly, such as ultrasound imaging (Q = 0.510, c.f. the current study's result Q = 0.1038) and mammography (Q = 0.738, c.f. the current study's result p = 0.0083), the internal influence coefficients for EHR use is relatively low. To rapidly accelerate a technology's diffusion it is essential to increase the internal or social contagion factors that influence adoption decisions. Otherwise, EHR adoption rates among small practices will remain relatively low and time horizons for complete adoption will remain distant.
Comparing the changes in the diffusion coefficients from the earlier period of measurement to the longer time span, the external influence factor increased by 54% and the internal influence factor declined by 38%. In Monte Carlo simulations using similar bass Modeling techniques and time frames, the algorithm introduced a systematic downward bias in the external and upward bias in the internal coefficients' estimates as the number of time frames increased. 39 To the extent that the estimates in this study are biased, they are understating the changing dynamic in potential adopters' resistance toward EHR promotion by external stakeholders. The implications of the models' results are discussed next.
Discussion
The Growing Resistance to EHR Adoption
Since 2004, when a confluence of events made increased EHR use among physicians a major public policy aim, there has been a significant amount of research and discussion surrounding the topic. Undoubtedly, physicians have felt increased external pressures to adopt EHRs. the Centers for Medicare and Medicaid Services (CMS) has introduced several new reporting requirements for hospitals with quality improvement and cost control as the primary objectives. 40 As reporting requirements increase, the role of the EHR as mechanism for gathering, integrating and disseminating such data will likely grow. CMS is beginning to design and field similar initiatives targeted at individual physicians.
However, countervailing forces also have emerged from within the medical community to resist adoption. For example, there are significant professional autonomy issues that have been raised in relation to EHRs being used. 41 In particular, physicians are concerned that policymakers, insurers and administrators will use EHRs as a proxy mechanism to influence, restrict, or dictate how medicine is practiced. While EHRs have not hit the critical mass necessary to enable such actions, the increased availability of information that an EHR implementation offers, creates the opportunity for government (or other payer) interventions in medical practices' day-to-day operations as cost and quality control programs. In other attempts at external quality control over care using comparative performance information, physicians were antipathetic toward the release of such data, especially when the data could be presented more accurately, more meaningfully, and in a more transparent manner. 42
The policy mechanism most commonly discussed for increasing EHR's external influence coefficient is the introduction of clinical reporting mandates. As part of the legislation that delayed cuts to Medicare part B payments in 2008, CMS asked the Congress to include a provision to promote the use of electronic prescribing (e-prescribing) by physicians. The program begins with a two-percent incentive for doctors that move to e-prescribing by 2009. This is to be followed with a two-percent penalty for physicians that fail to adopt e-prescribing technology by 2012. The e-prescribing initiative is part of a larger CMS strategy to move all physicians to an interoperable EHR—an effort that is aimed at both controlling costs and improving quality.
There are also initiatives to help subsidize the adoption of EHR technology. In the purest form, grants are given directly to providers to purchase systems. 43 The other commonly promoted subsidization scheme is to have hospitals underwrite the costs of EHR hardware for practices in their community. 44
While such programs may be of some use, they are not likely to advance the goal of full EHR adoption significantly, because providers tend to respond negatively to such mandated-use policies. 45,46 The medical community's professional culture makes it a very close-knit social network that views external attempts at instituting controls as an assault on its autonomy. 47 Physicians have historically relied upon their professional peers as their primary source of information related to new technologies. 48,49 Further, the physician community does not, in general, have a strong grasp of the quality improvement processes that are being targeted at them. 50 Collectively, the medical community's social mechanisms that influence adoption decisions view EHRs as a potential threat to professional autonomy. This may be particularly true among physicians in small practice settings who value the freedom and autonomy the setting they practice in provides.
There is extensive research on ways of influencing physicians' internal social networks. Passive dissemination strategies, such as journal articles and mailings, are ineffective. 51 The use of “thought leaders” to influence social networks and change clinical behaviors has experienced some success. However, given that small practices are, by their nature, on the periphery of such networks, this may not be a broadly applicable intervention. An interactive-educational strategy may offer a route for penetrating physicians' social networks—particularly those in small practices.
There are three interactive-educational mechanisms external stakeholders might use to increase the internal influence coefficient related to EHR use, the first of which is medical education. Many medical schools do not employ EHRs nor train students in their use. Training medical students to rely upon EHRs and their decision support tools can only serve to accelerate universal EHR adoption. By establishing the expectation, through training, that medicine is a practice that relies on the data captured in EHRs to improve patient outcomes, the process of inculcation into the culture of medicine accelerates adoption through the creation of expectations of minimum technology for good practice. Further, the acculturating of medical student to EHRs during this formative period sends a signal that the profession values EHRs.
The second potential channel for influencing physicians' social networks is through the Continuing Medical Education (CME) requirement. However, CME interventions have not proven to be particularly effective in changing providers' behaviors in other clinical areas. 52,53 While CMEs can inform, they rarely are organized to offer a business case for EHRs. While they may offer data on adoption costs, physicians often hear from their colleagues about the costs and challenges of implementation that serve to deter small practices from adoption.
The last active-educational mechanism for accessing physicians' social networks is Academic Detailing. Academic Detailing involves in-depth one-on-one training sessions with physicians and is an effective mechanism for altering physicians' behaviors. 54–56 This mechanism can circumvent the challenges faced by CME-driven initiatives because of the nature of the interaction and the context in which it takes place and is more akin to the impact created by mentoring than simple information dissemination.
Collectively, the interactive-educational approaches hold the greatest power to hasten universal EHR adoption. However, they also carry the highest price tag and require major coordination efforts to implement. It is essential that medical education, including residency programs, take place in environments that use EHRs. In addition, programs designed to give physicians extensive Academic Detailing in their practices can provide the greatest promise for spurring universal adoption by 2014.
Uncertainty and Implementation
While there are several factors that are serving to drive adoption, uncertainty is functioning as both an internal and external factor to suppress adoption rates. We identify three sources of uncertainty that may be delaying adoption: uncertainty about implementation costs, causes and effects, uncertainty about shifting standards and finally, uncertainty about potential policy interventions.
The costs of implementation of EHR system have long been cited as a factor that has slowed adoption rates. Besides the costs and learning curve involved, there is a concern from practitioners about the effects of EHR companies that go out of business. 57 EHR providers that cater to the needs and budgets of smaller practices are also more likely to be the same companies that go out of business because of the lack of a critical mass supporting the required development of the data systems. Often, practices request special features, or add-ons, to the base implementation, which then increase the cost of the adoption. Furthermore, these changes demonstrate how the current generation of product offerings does not fully meet the needs of the practitioner's workflow and practice. Such fears only bolster the belief that investing in an EHR can have significant unforeseen costs. Amplified by the social networks of small practice doctors, the stories of failed implementations can scare even the most stalwart EHR champion. In the face of such risk, small practices may choose to wait for the “cream to rise to the top.” In contrast with concerns about such bottom-up implementation challenge, there is a significant and realistic concern of top-down implementation and rule changes that would have deleterious effects on EHR adopters that would disproportionally impact small practices.
Additionally, the discussion, in the political discourse, about the adoption of a universal healthcare plan has created a new layer of uncertainty. While the economic reality of such an initiative is clouded, the rhetoric of from both political parties have included references to EHRs as a cost management solution. These two policy issues may create a nexus of events that link the two efforts such that access to a new and significant patient base will be linked to adoption of a specific EHR standard, which may not align with current products. Finally, the desire for medical record portability may create a push for a unitary system under a centralized control, the result of which would be a government-sponsored EHR. In such a scenario, small practice investments into an EHR may become a moot point or seen as an unnecessary expense.
The American Health Information Community Quality Work Group has identified the absence of EHR standards as a significant impediment to EHR adoption. 58 From the practitioner's perceptive, the risk associated with selecting an EHR format that is incompatible with the current, fractured systems that exist, or that a standard will be linked to an implementation of an EHR that is provided by an agency like CMS that will supersede previous efforts. The impact of “standards wars” was seen in the VHS/Betamax debacle, and in the consumer market, the fight between Blu-Ray and HD-DVD. It is the uncertainty of the future of American healthcare that contributes to the pause that surrounds EHR adoption.
Conclusions
Research on this issue will undoubtedly continue and will be made even more relevant as healthcare advances in the political arena. Both political parties have highlighted EHRs as a solution for the growing costs of health service delivery. The discourse itself may be impacting adoption as uncertainty is amplified in the process. While the mandates for CMS will eventually move medical practice towards adoption, the uncertainty created by both the economic realities and political landscape may be doing more to stymie adoption than simply allowing the system to reorganize of its own volition. CMS-mandated documentation and data transmittal rules may serve to make the EHR a de facto necessity to be compliant. Policies that penalize practices that do not issue electronic prescriptions will also move practices towards compliance. The uncertainty of the solution to the healthcare crisis in the U.S. is, at least, contributing to both the internal perspectives of the costs as well as providing the external backdrop within which these efforts take place.
In the face of new data, we find the tipping point to be delayed three years as compared to the previous study. 1 The delay may be a dynamic process itself that will see an increasing horizon over time. As we have argued, uncertainty may be contributing to the shift in the tipping point. We suggest that uncertainty, as we have defined it, can be reduced in three ways. First, the publication of a single EHR standard that is certifiable by a third-party agency. The certification process currently in use by the CCHIT does not ensure interoperability or future compliance. Second, a clear and durable agreement on healthcare policy in the U.S. and its implications for the EHR needs to be established. Lastly, a statement about how the government will transition from the current mode of care delivery to the new system should be articulated. With large hospitals better able to shoulder the costs of larger IT implementations, it is the small practices that will be most impacted by these decisions and will likely be the most interested in their eventual solution. EHRs are the future, and resistance is futile; however, current exigencies and uncertainties are slowing, not accelerating adoption.
References
- 1.Ford EW, Menachemi N, Phillips MT. Predicting the adoption of electronic health records by physicians: When will health care be paperless? J Am Med Inform Assoc 2006;13(1):106-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Obama B. Affordable health care for all Americans: The Obama-Biden plan J Am Med Assoc 2008;300(16):1927-1928. [DOI] [PubMed] [Google Scholar]
- 3.DesRoches CM, Campbell EG, Rao SR, et al. Electronic health records in ambulatory care: A national survey of physicians N Engl J Med 2008;359(1):50-60. [DOI] [PubMed] [Google Scholar]
- 4.Menachemi N, Ford EW, Beitsch LM, Brooks RG. Incomplete EHR. Adoption: Late uptake of patient safety and cost control functions. Am J Med Qual 2007;22(5):319-326. [DOI] [PubMed] [Google Scholar]
- 5.Conn J. HHS shifts IT into high gear. New plan to promote information technology released to mostly good reviews, but concerns remain about its scope and funding. Mod Healthc 2008;38(23):6-71. [PubMed] [Google Scholar]
- 6.Morris M, Evans D. States should focus on EHR interoperability Behav Healthc 2008;28(7):23-25. [PubMed] [Google Scholar]
- 7.Diamond CC, Shirky C. Health information technology: A few years of magical thinking? Health Aff Millwood 2008;27(5):w383-w390. [DOI] [PubMed] [Google Scholar]
- 8.Greer S. Medical autonomy: Peeling the onion J Health Serv Res Policy 2008;13:1-2. [DOI] [PubMed] [Google Scholar]
- 9.Sidorov J. It Ain't necessarily so: The electronic health Record and the unlikely prospect of reducing health care costs Health Aff 2006;25(4):1079. [DOI] [PubMed] [Google Scholar]
- 10.Handel DA, Hackman JL. Implementing electronic health records in the Emergency Department J Emerg Med 2008. September 12. [DOI] [PubMed]
- 11.Walter Z, Succi-Lopez M. Physician acceptance of information technologies: Role of perceived threat to professional autonomy Decis Support Syst 2008.
- 12.Ward R, Stevens C, Brentnall P, Briddo J. The attitudes of health care staff to information technology: A comprehensive review of the research literature Health Info Libr J 2008;25(2):81-97. [DOI] [PubMed] [Google Scholar]
- 13.Menachemi N, Brooks RG. Reviewing the benefits of electronic health records and associated patient safety technologies J Med Syst 2006;30(3):159-168. [DOI] [PubMed] [Google Scholar]
- 14.Bass FM. A new product growth model for consumer durables Manag Sci 1969;15:215-227. [Google Scholar]
- 15.Audet A-M, Doty M, Peugh J, et al. Information technologies: When will they make it into the physicians' black bags? Med Gen Med 2004;6(4):2. [PMC free article] [PubMed] [Google Scholar]
- 16.Terry K. Doctors and EHRs Med Econ 2005;82(2)On-line. [PubMed]
- 17.Miller RH, Hillman JM, Given RS. Physician use of IT: Results from the Deloitte Research survey J Healthc Inf Manag 2004;18(1):72-80. [PubMed] [Google Scholar]
- 18.Andrews JE, Pearce KA, et al. Current state of information technology use in US primary care practice-based research network Inform Prim Care 2004;12:11-18. [DOI] [PubMed] [Google Scholar]
- 19.Burt CW, Hing E. Use of computerized clinical support systems in medical settings: United States, 2001–03 Advances Data 2005;353:1-5. [PubMed] [Google Scholar]
- 20.Loomis GA, Ries JS, Saywell Jr RM, Thakker NR. If electronic medical records are so great, why aren't family physicians using them? J Fam Pract 2002;51(7):636-641. [PubMed] [Google Scholar]
- 21.Versel N. Connect the docs Mod Healthc 2004;34(8):48. [PubMed] [Google Scholar]
- 22.Simon JS, Rundall TG, Shortell SM. Drivers of electronic medical record adoption among medical groups Joint Commun J Qual Patient Saf. 2005;31(11):631-639. [DOI] [PubMed] [Google Scholar]
- 23.Hing ES, Burt CW, Woodwell DA. Electronic medical record use by office-based physicians and their practices: United States, 2006 Adv Data 2007;393:1-7. [PubMed] [Google Scholar]
- 24.Hing E, Burt CW. Characteristics of office-based physicians and their medical practices: United States, 2005–2006 Vital health Stat 2008;13(166):1-34. [PubMed] [Google Scholar]
- 25.California Healthcare Foundation The State of Health Information Technology in California: Use Among Physicians and Community ClinicsOakland, CA: California Healthcare Foundation; 2008. Contract No.
- 26.Menachemi N, Brooks RG. Adoption among physicians: Results of a large-scale statewide analysisEHR, other IT J Healthc Inf Manag 2006;20(3):79-87. [PubMed] [Google Scholar]
- 27.Rogers EM. Diffusion of innovationsNew York: Free press of Glencoe; 1962.
- 28.Ash JS, Bates DW. Factors and forces affecting EHR system adoption: Report of a 2004 ACMI discussion J American Medical Informatics Association 2005;12(1):8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gladwell M. The tipping point: How little things can make a big differenceBoston: Little. Brown; 2000.
- 30.Valente TW. Social network thresholds in the diffusion of innovations Soc Netw 1996;18:69-89. [Google Scholar]
- 31.Robert-Ribes J. Predicting the speed of technology introduction. Australian Venture Capital. [Internet] 2005;131:34-36. [Google Scholar]
- 32.Van den Bulte C. Want to know how diffusion speed varies across countries and products? Try using a bass model PDMA visions 2002;XXVI(4):12-15. [Google Scholar]
- 33.Blair R, EM. RS, quality of care and patient perception Health Manag Technol 2003;24(11):38. [PubMed] [Google Scholar]
- 34.Rogoski RR. You say tomato and Health Manag Technol October2002;23(10):24. [PubMed] [Google Scholar]
- 35.Jha AK, Ferris TG, Donelan K, et al. How common are electronic health records in the United States?. A summary of the evidence. Health Aff Millwood 2006;25(6):w496-w507. [DOI] [PubMed] [Google Scholar]
- 36.Hing E, Burt CW. Office-based medical practices: Methods and estimates from the national ambulatory medical care survey Adv Data 2007;383:1-15. [PubMed] [Google Scholar]
- 37.Lilien GL, Van de Bulte C. Diffusion Models: Managerial Application and SoftwareUniversity Park, PA: Pennsylvania State University; 1999. Contract No.: Document Number.
- 38.Sillup GP. Forecasting the adoption of new medical technology using the bass model J Health Care Mark 1992 Dec 1992;12(4):42. [PubMed] [Google Scholar]
- 39.Van den Bulte C, Lilien GL. Bias and systematic change in the parameter estimates of macro-level diffusion models Mark Sci 1997;16(4):338-353. [Google Scholar]
- 40.Gebhart F. CMS dangles carrot in hopes of improving care in hospitals Drug Top 2003 Oct 6 2003;147(19):80. [Google Scholar]
- 41.Manos D. Physicians reluctant to adopt EHR systems, survey finds Journal [serial on the Internet] 2008. Date.
- 42.Davies HTO. Public release of performancedata and quality improvement: Internal responses to external data by US health care providers Qual Health Care 2001;10:104-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Middleton B, Hammond WE, Brennan PF, Cooper GF. Accelerating U.S. EHR adoption: How to get there from here: Recommendations based on the 2004 ACMI retreat J American Medical Informatics Association 2005;12(1):13-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Terry K. Will relaxing stark bind you tighter? Med Econ 2006;83(3):40-43. [PubMed] [Google Scholar]
- 45.Doolan DF, Bates DW. Computerized physician order entry systems in hospitals: Mandates and incentives Health Aff 2002;21(4):180. [DOI] [PubMed] [Google Scholar]
- 46.Brown SA, Massey AP, Montoya-Weiss MM, Burkman JR. Do I. Really have to?. User acceptance of mandated technology. Eur J Inf Syst 2002;11(4):283. [Google Scholar]
- 47.Edwards N, Kornacki MJ, Silversin J. Unhappy doctors: What are the causes and what can be done? Br Med J 2002;324:835-838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gabbay J, le May A. Evidence based guidelines or collectively constructed “mind lines?”: Ethnographic study of knowledge management in primary care Br Med J 2004;329(7473):1013A-1016A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Coleman JS, Menzel H, Katz E. Medical Innovation: A Diffusion StudyIndianapolis: Bobbs-Merrill; 1966.
- 50.Audet A-MJ, Doty MM, Shamasdin J, Schoenbaum SC. Measure, learn, and improve: Physicians' involvement in quality improvement Health Aff 2005;24(3):843-853. [DOI] [PubMed] [Google Scholar]
- 51.Heffner JE. Altering physician behavior to improve clinical performance Top Health Inf Manag 2001;22(2):1-9. [PubMed] [Google Scholar]
- 52.Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance. A systematic review of the effect of continuing medical education strategies. J Am Med Assoc 1995;274(9):700-705. [DOI] [PubMed] [Google Scholar]
- 53.Oxman AD, Thomson MA, Davis DA, Haynes RB. No magic bullets: A systematic review of 102 trials of interventions to improve professional practice Can Med Assoc J 1995;153(10):1423-1431. [PMC free article] [PubMed] [Google Scholar]
- 54.Levac KA. Putting outcomes into practice in physician offices J Nurs Care Qual 2002;17(1):51-62Quiz:90. [DOI] [PubMed] [Google Scholar]
- 55.Landry MD, Sibbald WJ. Changing physician behavior: A review of patient safety in critical care medicine J Crit Care 2002;17(2):138-145. [DOI] [PubMed] [Google Scholar]
- 56.Badger SL, Bosch RG, Toteja P. Rapid implementation of an electronic health record in an academic setting J Healthc Inf Manag 2005;19(2):34-40. [PubMed] [Google Scholar]
- 57.Adler KG. How to select an electronic health record system Fam Pract Manag 2005;12(2)(55)*62. [PubMed]
- 58.American Health Information Community (AHIC) Quality Work group Analysis of requirements for health information technology to the Quality WorkGroup's future vision for longitudinal quality measurement and improvement Journal [serial on the Internet] 2008. Date.
- 59.Loomis GA, Ries JS, Saywell RMJ, Thakker NR. If electronic medical records are so great, why aren't family physicians using them? J Fam Pract 2002;51(7):636-641. [PubMed] [Google Scholar]
- 60.Audet AM, Doty MJP. Information technologies: When will they make it into the physician's black bags? MedGenMed 2004;6(4):2. [PMC free article] [PubMed] [Google Scholar]
- 61.Burt CW, Hing E. Use of computerized clinical support systems in medical settings: United States 2001–2003 Adv Data 2005;353:1-5. [PubMed] [Google Scholar]