Abstract
Objective
To investigate the use of an upper cervical low-force (UCLF) chiropractic procedure, based on a vertebral alignment model, in the management of neck pain and disability by assessing the impact on valid patient outcome measures.
Design
A retrospective case series.
Methods
Consecutive patient files at a private chiropractic practice over a 1-year period were reviewed for inclusion. Data for the first visit, pre- and post-adjustment atlas alignment radiographic measurements, baseline and 2-weeks NDI (100 point) and verbal NRS (11 point) were recorded. The data were analyzed in their entirety and by groups comparing <30% vs. >30% post adjustment atlas alignment changes.
Results
Statistically significant clinically meaningful improvements in neck pain NRS (P < 0.01) and disability NDI (P < 0.01) after an average of 13.6 days of specific chiropractic care including 5.7 office visits and 2.7 upper cervical adjustments were demonstrated. There were no serious adverse events. Cases with the post-adjustment skull/atlas alignment measurement (atlas laterality) that were changed more than 30% on the first visit toward the orthogonal alignment predicted a statistically and clinically significant better outcome for NDI in 2 weeks.
Conclusions
UCLF chiropractic instrument adjustments utilizing a vertebral alignment model are promising for the management of patients with neck pain based on assessment using valid outcome measures.
Keywords: chiropractic, neck pain, evidence-based outcomes, neck disability index (NDI), validity, orthospinology, upper cervical
Abstract
Objectif
Enquêter sur le recours à la procédure chiropratique de la manipulation cervicale supérieure de faible intensité (UCLF), fondée sur le modèle de l’alignement vertébral, dans la gestion de la douleur au cou et de l’incapacité fonctionnelle en évaluant les conséquences des critères valables d’efficacité pour les patients.
Concept
Une rétrospective de séries de cas.
Méthodes
On a effectué une révision des dossiers médicaux des patients, sur une période d’un an, dans une clinique chiropratique privée. On a consigné les données portant sur la première visite, les dimensions sur les radiographies de l’alignement de l’atlas, avant et après l’ajustement, la base de référence, les deux (2) semaines de NDI (100 points) et le NRS verbal (11 points). Les données ont été analysées dans leur intégralité et par groupes, en observant <30 % c. >30 % des changements à l’alignement de l’atlas après ajustement.
Résultats
important au plan statistique, significatif au plan clinique, on a démontré des améliorations sérieuses à la douleur au cou, NRS (P < 0.01), et à l’incapacité fonctionnelle, NDI (P < 0.01), après une moyenne de 13,6 jours de traitement chiropratique spécifique, y compris 5,7 visites au bureau et 2,7 ajustements cervicaux supérieurs. On n’a observé aucun effet secondaire défavorable. Pour les cas affichant une mesure d’alignement après ajustement au crâne/atlas (latéralité de l’atlas), qui ont été modifiés plus de 30 % à la première visite, vers un alignement orthogonal, on a démontré une amélioration supérieure aux plans statistique et clinique pour le NDI en deux semaines.
Conclusions
L’instrument d’ajustement chiropratique UCLF, combiné à un modèle d’alignement vertébral, semble prometteur pour la gestion des patients souffrant de douleurs au cou si on se fie à l’évaluation des critères valables d’efficacité.
Introduction
Neck pain affects two thirds of people at some point in their lives and is almost as common as low back pain.1 The point prevalence of neck pain for North America is somewhere between 13–22.2%, with high-intensity low-disability pain at 10.1% and disabling neck pain affecting 4.6% of the population.1,2 Chiropractors frequently care for patients with neck pain using varying techniques or procedures. They typically use spinal manipulative therapy (SMT) to address a segmental joint hypomobility within the cervical spine as determined by joint motion palpation and endplay assessment.3 Such manipulation involves a specific spinal segmental contact, passive lateral flexion and rotation of the head and neck to the point of increased joint tension followed by a high-velocity low-amplitude (HVLA) thrust. The thrust has been measured at 100 Newtons and is usually accompanied by and audible sound theorized to occur from cavitation.4
Recent systematic reviews of HVLA-style spinal manipulative therapy have shown that there is moderate to high-quality evidence that HVLA is better than placebo for chronic neck pain, better than general medical care and about the same as rehabilitation.5,6 However, there has been considerable controversy regarding the safety of HVLA manipulation in the cervical spine7,8 but a recent study shows concerns may be unfounded.9
Chiropractors also use other forms of spinal manipulation aside from HVLA to care for patients suffering from neck pain. Upper cervical low-force (UCLF) procedures, in particular, use a low-force thrust (on the order of 9–13 Newtons in some cases) and require no lateral flexion or rotation of the head and neck or joint cavitation for the management of neck pain and disability. Many UCLF procedures are based on the Grostic model of upper cervical analysis, which was developed in the late 1930s and early 1940s.10 The care can be delivered by hand or hand-held and table-mounted instruments. Grostic, Orthospinology, Atlas Orthogonal, Advanced Orthogonal and National Upper Cervical Chiropractic Association (NUCCA) are some of the named techniques that are UCLF procedures. These systems use the supine leg check to test for functional leg length inequality (FLLI) as one of the main clinical assessments along with a radiological analysis for the quantification of upper cervical alignment.11–13 The Grostic model hypothesizes that a neuromusculoskeletal link exists between the upper cervical spine, bilateral spinal skin temperature regulation asymmetry, postural asymmetry and FLLI.13 The supine leg check determines when an upper cervical adjustment should be given and the x-ray analysis determines how to deliver the adjustment based on alignment measurements and the observed resultant alignment after the first adjustment. The supine leg check has demonstrated clinical validity as a stand-alone test for recurring back pain,14 exhibited high (ICC>0.9) agreement among examiners and the inter-examiner reliability was good at 0.7.15 However, the validity of using supine leg length asymmetry change following an atlas adjustment as a measure of improved neurological function is mostly unknown. FLLI may be linked to increased latencies found on somatosensory evoked potential (SEP) tests of the common peroneal nerve at the cortex.16 The removal of FLLI (i.e. a balanced supine leg check) coupled with a change in upper cervical alignment toward the orthogonal position on post-adjustment radiographic analysis following upper cervical chiropractic intervention, is thought to indicate the absence or improvement of biomechanical and neurological dysfunction within the cervical spine. The measurement of atlas alignment relative to the skull (atlas laterality) from x-rays demonstrates good to excellent reliability17–22 (0.83 to 0.99 R) with 1 exception23 (range of error 2°); however, its measurement is 2-dimensional, representing anatomical relationships in only 1 plane of motion with the validity unknown. A premise of many upper cervical chiropractic techniques is that it is the maintenance or “holding” of the upper cervical alignment correction after an adjustment that allows the patient to improve, not just the manipulation procedure.
Since the adjusting technique and post-adjustment analysis do rely on radiographs, the procedure may introduce some risk due to the exposure to ionizing radiation. This procedure uses at least 3–4 additional cervical x-ray views in order to achieve optimal results. Groups using UCLF procedures advocate methods to limit the risk of exposure to radiation, including the use of lead foil filters in addition to the collimator and internal filters to significantly minimize radiation to more sensitive tissues like the brain, eyes and thyroid. A recent study indicates the total radiation for UCLF x-rays are estimated from 136 to 211 milliroentgens (mR) at skin entrance when using lead filters. This compares similarly to a standard 2 view cervical series without lead filters at 178 mR.24
Are the UCLF X-rays dangerous? Wall et al. indicates the risk band for radiography to the head, neck and joints is minimal with a risk range of between 1 in a million and 1 in 100,000.25 The thyroid gland may be the most sensitive tissue to radiation that is exposed to the largest dose with the current study’s radiographic procedures. The life time age-adjusted background risk for developing thyroid cancer is 0.79%.26 Preston et al. provides information that is used to express the elevated relative risk (ERR) using a single formula: ERR = 0.57 × Dose × EXP (−0.037 (ae −30) −1.51n (age/70)), where “ae” means age at exposure and “age” indicates attained age.27 Another study using atomic bomb survivors found the relative risk per Gray (ERR/Gy) was not significantly elevated among the cervical cancer patients and atomic bomb survivors studies exposed after age 15. There was a 7.7 ERR/Gy (one Gray is approximately 100,000 mR) and an excess absolute risk per 104 person years (PY) Gy (EAR/104 PY Gy) of 4.4 for those exposed before age 15.28 For the exposure ages 5–9 and 10–14 the modifiers were 0.5 and 0.2 respectively indicating significantly reduced risk with increasing age at exposure. The U.S. Environmental Protection Agency (EPA) has a formula for estimating mortality risk from radiation for thyroid cancer as well.29 Biological Risk from Exposure to Low Levels of Ionizing Radiation: BEIR VII Phase 2 (2006) provides a lifetime attributable risk (LAR) of thyroid cancer incidence for age and gender from a single exposure to 0.1 Gy (approximately 10,000 mR).30 The LAR varies significantly with age at exposure with decreasing age having larger LARs. The LAR for females is higher than males.
Chiropractic could base its methods on scientific data using information demonstrated in practice through clinical research.31 The purpose of this study is to assess the impact of the UCLF procedure on pain levels and disability ratings in a population of neck pain patients seen in a private practice setting. A second goal is to examine the predictive value and risk of taking post x-ray alignment measurements by determining if patients who receive a more completely reduced upper cervical spine misalignment on the first visit experience better clinical improvement. The hypothesis is that a statistically and clinically significant improvement occurs following UCLF chiropractic procedures. Also, a better outcome is predicted within 2 weeks when the first chiropractic atlas adjustment more completely reduces upper cervical vertebral alignment toward the orthogonal configuration. These data are necessary to begin to address the question: “Are there any benefits for patients suffering from neck pain following the application of UCLF chiropractic procedures?”
Methods
Criteria for Inclusion
This study was an outcome-based analysis that reviewed consecutive patient files over a 1-year period. In order to be selected the patient’s file must have met the following inclusion criteria:
A chief complaint of neck pain
Completed the Neck Disability Index (NDI) on the first visit
Re-evaluation date after approximately 2 weeks but not to exceed 30 days
Have a numeric pain rating score (NRS) on the same dates as the NDI
Have had detectable supine leg length alignment asymmetry
Radiographic findings indicative of upper cervical misalignment based on the Grostic model
Cases were excluded if there were confounding examination or history findings such as laminectomy at C2 or gross congenital or traumatic malformations in the upper cervical spine that would affect the measurement system.
Data for the first visit, pre- and post-adjustment atlas alignment radiographic measurements, baseline and 2-week NDI (100 point) and verbal NRS (11 point) were recorded. To determine the percent of change for atlas alignment, the net difference was divided by the baseline measurement with the quotient converted to a percentage. Data were tabulated and analyzed using Excel spreadsheets with the data analysis toolpack (Microsoft Corp, WA). Student t-tests, Mann-Whitney test and Chi-square test were used for statistical comparisons. Statistical tests were two-sided and P-values less than 0.05 were considered significant. The data were analyzed in their entirety and by groups comparing <30% vs. >30% post adjustment atlas laterality changes.
Criteria for Chiropractic Adjustment
Each patient completed an application for care, consultation, informed consent, privacy policy notification, examination, x-rays and spinal adjustment on the first visit. The consent form and privacy statement include the notification that patient data may be used for research purposes, but that in no case will it be possible to identify any patient associated with these data. The examination consisted of standard orthopedic, neurological, range of motion and chiropractic tests. The chiropractic examination involved palpation of the joints and muscles for resistance to joint motion, the level of tenderness, the presence of inflammation and postural analysis in the standing and supine positions.32,33
Radiographic examination
Radiographic procedures were performed on the first visit if exam findings suggested the presence of red flags or upper cervical chiropractic dysfunction. Each patient included in the study received a minimum of 5 x-rays: lateral cervical, vertex, 2 nasium cervical views (before and after the first chiropractic adjustment) and either an A-P cervical or an A-P open mouth view. The cervical x-rays were used for pathology and chiropractic radiographic analysis to provide specific adjustments based on the Orthospinology technique procedures and to determine upper cervical alignment change following the first adjustment. Radiation exposure was minimized through the use of high-speed films, rare earth screens, lead filters, and a lead apron. Lead filters for the nasium views reduced radiation to the eyes, skull, and brain by an average of 95.1% per nasium. The area from C1 to C3 was filtered achieving a 90.4% average reduction of radiation per nasium while an area from C4-T1 had no filtration.34
Intervention
Chiropractic Adjustments
Chiropractic care was provided at each visit and included only upper cervical adjustments as dictated by the supine leg check for patients with neck pain. Supine leg length asymmetry and upper cervical adjustments were performed according to the Orthospinology procedure. Orthospinology is a technique system that is based on the research of John F. Grostic, D.C. It provides methods of determining a patient’s eligibility, an x-ray analysis that quantifies relative upper cervical vertebral alignment and a formula that calculates a pathway for the adjustment. The adjustment force can be delivered by hand and hand-held or table mounted instruments. The system provides a protocol for post-adjustment physical re-evaluation and analysis of vertebral alignment measurement changes on the first visit. This allows the doctor to assess the results of the adjustment and modify future adjustments if necessary.35
Though the current study looks only at atlas laterality, many other measurements are used to deliver the adjustment. Atlas and axis rotation relative to the skull, the atlas alignment relative to the axis (lower angle), the relationship of directions and magnitudes of the upper and lower angles as well as the architecture of the atlas and axis joint surfaces are just a few. For adjustment, patients were placed in a side-lying position with the head’s mastoid resting on a solid mastoid support headpiece. Upper cervical adjustments were delivered with a solenoid-driven stylus, hand-held instrument (Laney instrument) with less than a 1/16″ excursion. The thrusts were administered along a lateral to medial vector as determine by the Orthospinology procedure x-ray analysis. The thrusts were high-velocity in nature, with little depth and are estimated at 2 pounds-force plus the pre-load against the skin and 2–3 milliseconds in duration.36 Audible sound from the joint was not observed on any patient.
Outcome Assessments
The Neck Disability Index (NDI) was used at the first visit and following approximately two weeks as the primary outcome measure and captures the patient’s perceived disability that results from their neck pain (100-point scale). An 11-point verbal numeric pain rating scale (NRS) for pain was used on a visit-by-visit basis.
Data Collected
The following factors were recorded from each patient file.
Baseline and 2-week NDI
NRS on each visit
First visit pre- and post-adjustment chiropractic radiographic analysis data
Time between the onset of the current episode of symptoms and the initiation of care
Days between Pre and Post NDI and NRS scores
Patient’s Age
Patient’s Gender
Number of visits between baseline and post evaluations
Number of positive supine leg checks which indicates the number of upper cervical adjustments given between the pre and post evaluations
The hypothesis is that a better outcome should occur when the first chiropractic atlas adjustment changes atlas laterality by more than 30% toward the orthogonal upper cervical alignment. C1 laterality is defined as the side of the acute angle and magnitude in degrees away from 90°, of the angle formed by the atlas plane line and the central skull line. The atlas plane line is constructed through points at the right and left intersections of the inferior posterior arch and the lateral masses of C1 on the nasium view. The central skull line is determined from the nasium view by curve fitting (by template or computer) the first 1–1.5 inches of the right and left lateral aspect of the skull above the squamosal suture. Alignment reduction toward the orthogonal position is expressed as “percentage of correction.” The percentage of correction is either 0 or a positive number for initial correction estimates; however, the means will be used for final comparisons. Essentially, these x-rays reduce a complex 3-dimensional structure into 2 dimensions and the analysis measures angular relationships between the 2 dimensional structures and does not purport to measure alignment in 3 dimensions.
Results
Sixty-six cases met the inclusion and exclusion criteria and were selected for the study. A total of 309 case files were reviewed with care beginning between August 1, 2004 and July 31, 2005. One hundred ninety-two had low back pain, 49 had some combination of neck pain, mid back pain, low back pain, extremity pain, headache, third-party contract exclusions or absent follow-up data. Two cases had significant structural abnormalities, one congenital and one surgical.
The data for 66 patients were tabulated and then divided into 2 groups, based on the percentage of atlas alignment change after the first chiropractic adjustment. Group 1 had <30% correction and Group 2 had >30% correction. The baselines of the variables and care delivery factors are summarized and show no differences between the groups (Table 1).
Table 1.
The baselines of each group’s variable characteristics are statistically no different
| Variable | All Cases | <30% Atlas Alignment Change Group | >30% Atlas Alignment Change Group | p-value from paired t-test |
|---|---|---|---|---|
| n | 66 | 13 | 53 | |
| Age | 48.3 ± 14.7 | 55.5 ± 18.4 | 46.5 ± 13.3 | 0.095* |
| Episode Onset <4 weeks (%) | 56.1 | 46.2 | 58.5 | 0.422** |
| Neck Disability Index | 35.1 ± 16.4 | 33.8 ± 15.0 | 35.4 ± 16.9 | 0.733 |
| Verbal Numeric Pain Rating | 5.89 ± 2.05 | 5.92 ± 2.6 | 5.89 ± 1.9 | 0.963 |
| Days between outcome measurements | 13.6 ± 4.4 | 13.7 ± 2.8 | 13.6 ± 4.7 | 0.916 |
| Female (%) | 72.7 | 69.2 | 73.6 | 0.770 |
| Care Delivery Factors | ||||
| # Office Visits | 5.7 ± 1.4 | 6.1 ± 1.3 | 5.7 ± 1.4 | 0.308 |
| # Atlas Adjustments | 2.7 ± 1.5 | 2.8 ± 1.3 | 2.7 ± 1.6 | 0.248 |
| Atlas Laterality (Degrees) | 2.83 ± 2.20 | 3.08 ± 2.21 | 2.76 ± 2.21 | 0.653 |
Although the t-test demonstrated 0.122, the Mann-Whitney test (0.095) is more appropriate for age due to the distribution not being normal.
Chi-square test.
Data analysis revealed statistically significant and clinically meaningful improvements for both NDI and NRS. No serious adverse events occurred. The average baseline NDI with the standard deviation was 35.1 (SD 16.4) and post-care NDI was 14.3 (SD 9.9). This represents a 20.8-point improvement (59.2%), which is both statistically (p < 0.01) and clinically significant (>10 points). The average time between the first and second NDI was in 13.6 (SD 4.4) days with 5.7 (SD 1.4) office visits and 2.7 (SD 1.5) C1 adjustments. The average pre-adjustment NRS was 5.89 (SD 2.0) and the post-care NRS was 1.76 (SD 1.3), a 70.1% improvement (p < 0.01). The average percentage of correction for C1 laterality was 48%. The pre-C1 laterality average was 2.83° (SD 2.20) and the post laterality was 1.48° (SD 1.74) (p < 0.01) (Table 2). Cases with a chronic onset were very similar showing baselines/2-week follow-up NDI and NRS scores of 32.9 (SD 13.9)/15.0 (SD 9.7) and 5.48 (SD 1.84)/1.79 (SD 1.21) respectively. Also the days 13.8 (SD3.7) and the number of visits/adjustments 5.9 (SD 1.1)/2.8 (SD 1.6) were comparable as well as the atlas alignment changes 2.66° (SD 1.90)/1.48° (SD 1.62). All were statistically and clinically significant.
Table 2.
Pre- and Post-care NDI, verbal NRS and radiographic atlas alignment
| Variable | Pre-care Mean (SD) | Post-care Mean (SD) | p-value from paired t-test |
|---|---|---|---|
| Neck Disability Index (100-point scale) | 35.1 ± 16.4 | 14.3 ± 9.9 | < 0.01 |
| Verbal Numeric Pain Scale (11-point scale) | 5.89 ± 2.05 | 1.76 ± 1.29 | < 0.01 |
| Atlas Laterality (Degrees) | 2.83 ± 2.20 | 1.48 ± 1.74 | < 0.01 |
Subgroup analysis found 13 cases with <30% reduction of atlas laterality (Group 1) and 53 with >30% (Group 2). (Table 3) Group 2 had a statistically and clinically meaningful better outcome for NDI at 2 weeks, compared to Group 1 (Table 4). Both groups showed improvement in the 2-week verbal numeric pain rating score. Group 2 showed more improvement on the average than group 1 (net improvement 4.24/10 vs. 3.69/10 respectively), but the difference was not statistically or clinically significant.
Table 3.
Distribution of atlas laterality corrections
| % C1 Correction | Case Frequency | Category % |
|---|---|---|
| 0 | 4 | 6.06% |
| 1 to 30 | 9 | 13.64% |
| 31 to 60 | 21 | 31.82% |
| 61 to 90 | 12 | 18.18% |
| >90 | 20 | 30.30% |
Table 4.
Comparison of NDI and NRS net differences between <30% vs. >30% Atlas laterality correction groups
| <30% C1 Correction Group | >30% C1 Correction Group | D | Sig. | |||||
|---|---|---|---|---|---|---|---|---|
| Outcomes | Baseline | 2 Week | Δ | Baseline | 2 Week | Δ | ||
| NDI | 33.8 | 21.1 | −12.7 | 35.4 | 12.7 | −22.8 | 10.1 | 0.010 |
| NRS | 5.92 | 2.23 | −3.69 | 5.89 | 1.64 | −4.25 | 0.56 | 0.241 |
Discussion
The data in this study indicate that a clinically and statistically significant improvement in valid outcome measures for neck pain and disability occurred following approximately 2 weeks, 6 visits and 3 UCLF adjustments based on the Grostic model. Furthermore, a superior outcome for disability may be linked to a threshold of improved upper cervical alignment. Of the 2 outcome measures, NDI was seen to improve more when the 1st adjustment produced more reduction of atlas laterality. The extent of atlas laterality change did not affect the outcome assessed by NRS for pain; however, in that both groups of patients had the same clinically meaningful improvement in NRS.
These results are interesting when contrasted with other reports in the literature that used similar outcome measurements in patients with neck pain of various onsets treated with a variety of chiropractic procedures reporting similar follow-up periods.37–42 Although varying patient populations and study designs make a direct comparison for effectiveness impossible, it stimulates questions that could be further investigated using well designed prospective studies. Table 5 lists the results of the current study and articles found in the literature. Studies reported using the 100-point NDI scale are converted to the 50-point NDI scale for consistency (Table 5).
Table 5.
Summary of the current study and some of the articles in the literature that use NDI to report the progress of patients following various techniques of chiropractic care reporting similar time periods. For consistency, the data is converted to the 50-point scale if it were originally reported using the 100-point scale by dividing by 2
| Study | Baseline NDI | 2-Week NDI | 4-Week NDI | Net Change | Net Change % | Number of manipulation / adjustments |
|---|---|---|---|---|---|---|
|
Current Study (N = 66) |
17.5
(Converted to 50 point) |
7.2
(Converted to 50 point) |
−10.3
(Converted to 50 point) |
59% | 2.7
Range (1 to 7) |
|
|
Rubinstein et al.37 (N = 529) |
12.0
(50 point) |
8.0
(50 point) |
−4.0
(50 point) |
33% | 3 to 9
@ 4th visit 8 days–6 weeks |
|
|
Hurwitz38 (N = 336) |
13.2
(50 point) |
9.7
(50 point) |
−3.5
(50 point) |
27% | No Data | |
|
McMorland and Suter39(Neck Pain Only Group) (N = 43) |
18.5
(50 point) |
9.0
(50 point) |
−9.5
(50 point) |
51% | 12 tx over 4 weeks | |
|
Giles and Muller40Manipulation Group (N = 23) |
16.0
(Converted to 50 point) |
11.0
(Converted to 50 point) |
−5
(Converted to 50 point) |
31% | 6 tx over 3–4 weeks | |
|
Giles and Muller41Manipulation Group (N = 18) |
13
(Converted to 50 point) |
8.5
@ 9 weeks (Converted to 50 point) |
−4.5
(Converted to 50 point) |
38% | 2 tx per week up to 9 weeks
(18) |
|
|
Wood et al.42Activator Group (N = 15) |
15.9 (Converted to 50 point) | 6.8
(Converted to 50 point) |
−9.1
(Converted to 50 point) |
57% | 8 | |
|
Wood et al.42Manual Thrust Group (N = 15) |
13.4
(Converted to 50 point) |
5.5
(Converted to 50 point) |
−7.9
(Converted to 50 point) |
59% | 8 |
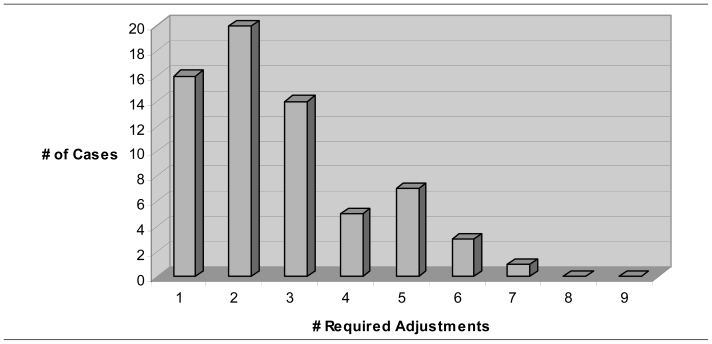
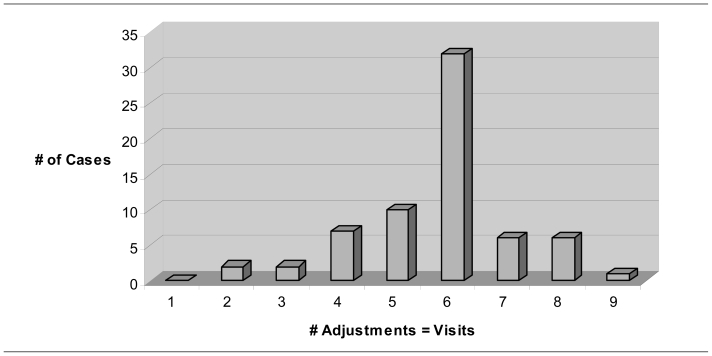
Three prominent differences between some of the above studies and the current study are the number of adjustments, the length of time between outcome measures and the percentage of patients that achieved a “normal” NDI score. The current study used approximately the same number of adjustments as the reported number of visits (4th visit) in Rubinstein, et al., however, the current study demonstrates a clinically significant change for NDI (>5/50 or 10/100) and NRS (>2 points). Also the current study shows 34.8% of cases achieved a normal NDI (<5 or <10 for the 50 or 100 point scale, respectively) from a baseline of 3%, a 31.4% net gain (Table 6). Rubenstein demonstrates 19% at the 4th visit from a baseline of 7.4%, a net gain of 11.6%.37 Differing patient populations could explain this variance therefore a direct comparison for efficacy is not possible. The present study’s design reports fewer adjustments and a shorter follow-up period than McMorland,39 Giles,40,41 Wood, Colloca and Mathews42 with similar or better-improved outcome levels. The current study’s data indicate the average patient had almost 6 office visits over a period of two weeks followed by re-evaluation. Using functional leg length asymmetry as a guide for when a patient required an atlas adjustment reduced the average number of adjustments to just below 3, yet clinical outcomes are parallel to other reports in the literature. Even though the patient was examined, it was determined that they did not need an adjustment on each visit. Typically, without using the supine leg check, a patient would receive an adjustment on each visit. These data show that the number of adjustments (dosage) was reduced by 52.6% relative to the number of visits (Figure 1).
Table 6.
The current study’s NDI histogram tables (100 point scale)
| Baseline NDI | Frequency | Category % |
|---|---|---|
| None (0–8) | 2 | 3.0 |
| Mild (9–28) | 26 | 39.4 |
| Moderate (29–48) | 26 | 39.4 |
| Severe (>50) | 12 | 18.2 |
| 2-Weeks NDI | Frequency | Category % |
| None (0–8) | 23 | 34.8 |
| Mild (9–28) | 38 | 57.6 |
| Moderate (29–48) | 5 | 7.6 |
| Severe (>50) | 0 | 0.0 |
Figure 1A.
Shows the frequency distribution (dosage) of adjustments required while using the upper cervical alignment model and the supine leg check. (N = 66)
Figure 1B.
Demonstrates the frequency of the current study’s visits and would equal the number of adjustments without using the upper cervical alignment model and the supine leg check. The premise of using the supine leg check is to eliminate unnecessary upper cervical adjustments. It follows that a patient may not receive an adjustment on each visit but will be examined to see if an adjustment is needed. The clinical utility of the supine leg check might be demonstrated by comparing the modes of each graph. The most frequent combination was 6 office visits but only 2 upper cervical adjustments indicating the supine leg check was negative or balanced on 4 visits. (N = 66)
Reducing dosage and utilizing UCLF procedures may be significant when determining risk to the patient for two reasons. First, the adjusting procedure itself may entail less risk. There is no rotation of the patient’s head and very limited lateral flexion. The adjustment is delivered with the patient’s neck in a nearly neutral posture in the side lying position. The joints are not taken to tension prior to the thrust; the thrust is of lower magnitude and does not produce cavitation of the joints. Hence, the light-force technique might avoid the perceived or theorized mechanism of “vertebral artery dissections due to intimal tearing as a result of over-stretching the artery during rotational manipulation.”43,44 Second, assuming any risk for stroke is similar per adjustment technique, simply reducing the dosage (number of adjustments) should also reduce the risk of stroke proportionately if there is a causal relationship. Little research is available in the published literature at this time for any side effects from UCLF techniques or similar procedures. The authors of 2 randomized controlled studies using upper cervical adjustments comparable to the procedure in the current study report no adverse effects.45,46
The results of the current study are very similar to the findings of Grostic and DeBoer47 concerning the magnitude in degrees of pre- and post-adjustment alignment average values (2.63/1.43 vs. 2.83/1.48) and the average percentage (47 vs. 48%) of atlas laterality correction. They also resemble some of the results found by Eriksen, in that a larger improvement in upper cervical alignment demonstrated a statistically better outcome, although Eriksen used a more stringent 50% x-ray correction to define his patient groups.48 He demonstrated a 40.5% average correction of all measured alignment components. Eriksen also found that patients with higher percent corrections on the first visit had a decreased need for follow-up visits. The current study only had 2 weeks of data so it would be difficult to make any conclusions about the need for follow-up care. The current study improves on Eriksen’s by using the patient-centered outcomes (NRS and NDI) as measures of clinical improvement. These findings support the validity of Grostic’s alignment model and the goal of reducing atlas laterality toward the orthogonal configuration.
What is the risk from the required radiographic procedures? The ERR for thyroid cancer is calculated using the current study’s average age at exposure of 48.3 with a range of 24 to 72 years, the attained age of 72 and the formula developed from Preston et al.27 The ERR is 0.0006 with a range of 0.0014 to 0.0002. Combining the ERR with the background risk of 1 equals 1.0006 with a range of 1.0014 to 1.0002. Using the lifetime background risk of developing thyroid cancer in the U.S. at 0.79%26 multiplied by 1.0006 (1.0014 to 1.0002) we find a total risk after UCLF X-rays is 0.7905% with a range of 0.7911% to 0.7902%. Based on the findings of Ron, et al.28 there is no significantly elevated excess relative risk from thyroid cancer for those exposed after age 15 to a 211 mR dose of radiation. The thyroid cancer mortality risk estimate using the U.S. Environmental Protection Agency (EPA) formula29 for a 211 mR dose is 0.68 per one million person years. Using linear interpolation of the BEIR VII Phase II30 data and the average age for the current study (48.3 ± SD14.7), an exposure of 211 mR results in an LAR for thyroid cancer incidence of 0.0283 per an exposed population of 100,000 for a male (0 to 0.443, 95% CI) and 0.120 for a female (0 to 2.384, 95% CI). According to the above studies the elevated risk from thyroid cancer is either zero or very small due to radiation exposure to the patient from UCLF X-rays.
The data from the current study indicate patients with neck pain experience improvement following UCLF procedures. Analysis of the data stimulates additional research questions. Should upper cervical alignment be considered when delivering a cervical adjustment? Does using the upper cervical alignment model and the supine leg check eliminate unnecessary adjustments and as a result, reduce the dosage? Will using UCLF decrease risk or side effects and improve patient satisfaction? Can implementation of UCLF procedures reduce health care costs for those suffering from neck pain and disability? Additional research is necessary to investigate these questions.
Study Limitations
The results of this study should be read with some caution. A definitive determination of cause and effect cannot be accomplished using this type of study. Weaknesses include having no control group and being retrospective. A prospective study would be stronger. There were no follow-up data for longer than 2 weeks largely because the majority of patients were released from active care before 4 weeks. The doctor was not blinded during the application of the mediating variables, so unintentional bias cannot be eliminated. A blinded X-ray analysis would improve the design for future studies. The small sample size increases the likelihood of sampling error. Unknown confounding variables might explain the observations in this study. The majority of the patients in the current study had histories of chronic neck pain with acute, sub-acute and chronic onsets of episodes. Differences in age and onset are complicating co-variables, making it impossible to compare effectiveness to results reported in other studies. Although the ages for our comparison groups were not statistically different at baseline, lower ages did show a weak trend for larger improved NDI scores. A prospective RCT could minimize confounding variables and should use experienced upper cervical technique practitioners.
Conclusion
The data supports the alignment model’s predictive validity by suggesting that a threshold of altered atlas alignment toward the orthogonal configuration following the first adjustment was associated with a better outcome in 2-weeks for disability from neck pain. The risk associated with UCLF X-rays is minimal for the current studies demographics. UCLF chiropractic instrument adjustments utilizing a vertebral alignment model are promising for the management of patients with neck pain based on assessments using valid outcome measures.
Acknowledgements
I would like to extend my sincere appreciation to Edward F. Owens, MS, DC, Dana J. Lawrence, DC, FICC, Eric Hurwitz, DC, PhD, Ronald S. Hosek, PhD, DC, MPH and Kirk Eriksen, DC for their contributions to this manuscript.
References
- 1.Cote P, Cassidy JD, Carroll L. The Saskatchewan health and back pain survey: The prevalence of neck pain and related disability in Saskatchewan adults. Spine. 1998;23(15):1689–1698. doi: 10.1097/00007632-199808010-00015. [DOI] [PubMed] [Google Scholar]
- 2.Bovim G, Scharader H, Sand T. Neck pain in the general population. Spine. 1994;19:1207. doi: 10.1097/00007632-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Bergmann TF, Peterson DH, Lawrence DJ. Chiropractic Technique: Principles and Practice. New York: Churchill Livingstone; 1993. [Google Scholar]
- 4.Kawchuk GN, Herzog W. Biomechanical characterization (fingerprinting) of five novel methods of cervical spine manipulation. J Manipulative Physiol Ther. 1993;16(9):573–577. [PubMed] [Google Scholar]
- 5.Vernon H, Humphreys K, Hagino C. Chronic mechanical neck pain in adults treated by manual therapy: a systematic review of change scores in randomized clinical trials. J Manipulative Physiol Ther. 2007;30(3):215–27. doi: 10.1016/j.jmpt.2007.01.014. [DOI] [PubMed] [Google Scholar]
- 6.Bronfort G, Haas M, Evans RL, Bouter LM. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis. Spine J. 2004;4(3):335–356. doi: 10.1016/j.spinee.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 7.Ernst E. Adverse effects of spinal manipulation: A systematic review. J R Soc Med. 2007;100(7):330–8. doi: 10.1258/jrsm.100.7.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bronfort G, Haas M, Moher D, Bouter L, van Tulder M, Triano J, Assendelft WJ, Evans R, Dagenais S, Rosner A. Review conclusions by Ernst and Canter regarding spinal manipulation refuted. Chiropr Osteopat . 2006 Aug 3;14:14. doi: 10.1186/1746-1340-14-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cassidy JD, Boyle E, Côté P, He Y, Hogg-Johnson S, Silver FL, Bondy SJ. Risk of vertebrobasilar stroke and chiropractic care: results of a population-based case-control and case-crossover study. Spine . 2008 Feb 15;33(4 Suppl):S176–183. doi: 10.1097/BRS.0b013e3181644600. [DOI] [PubMed] [Google Scholar]
- 10.Eriksen K, Rochester R. Orthospinology Procedures: An Evidence-Based Approach to Spinal Care. Philadelphia: Lippincott, Williams and Wilkins; 2007. History of the Grostic/Orthospinology Procedure; pp. 18–36. [Google Scholar]
- 11.McAlpine JE, Humber JK. Chiropractic Orthospinology. Todays Chiropr. 1983 Jan–Feb;:24–8. [Google Scholar]
- 12.Wiedemann RL. Measurement: The supine leg check; Thermal instrumentation. In: Thomas MD, editor. Nucca protocols and perspectives: A textbook for the National Upper Cervical Chiropractic Association Monroe, MI. National upper cervical chiropractic association; 2002. pp. 3-1–4-12. [Google Scholar]
- 13.Grostic JD. Dentate ligament cord distortion hypothesis. Chiropr Res J. 1988;1:47–55. [Google Scholar]
- 14.Knutson GA. Incidence of foot rotation, pelvic crest unleveling, and supine leg length alignment asymmetry and their relationship to self-reported back pain. J Manipulative Physiol Ther . 2002 Feb;25(2):110E. doi: 10.1067/mmt.2002.121414. [DOI] [PubMed] [Google Scholar]
- 15.Hinson R, Brown SH. Supine leg length differential estimation: an inter- and intra-examiner reliability study. Chiropr Res J. 1998;5:17–22. [Google Scholar]
- 16.Collins KF, Pfleger B. Significance of functional leg length inequality upon somatosensory evoked potential findings. Eleventh Annual Upper Cervical Spine Conference; Life College. 1994. [Google Scholar]
- 17.Jackson BL, Barker W, Bentz J, Gambale AG. Inter- and intra-examiner reliability of the upper cervical x-ray marking system: A second look. J Manipulative Physiol Ther. 1987;10(4):157–63. [PubMed] [Google Scholar]
- 18.Jackson BL, Barker WF, Gambale AG. Reliability of the upper cervical x-ray marking system: A replication study. J Clin Invest Res. 1988;1(1):10–13. [Google Scholar]
- 19.Rochester RP. Inter- and intra-examiner reliability of the upper cervical x-ray marking system: A third and expanded look. Chiropr Res J. 1994;3(1):23–31. [Google Scholar]
- 20.Seemann DC. A reliability study using a positive nasium to establish laterality. Upper Cervical Monograph. 1994;5(4):7–8. [Google Scholar]
- 21.Grostic JD, Marshall WG. Accuracy of an upper cervical measuring system: A validity study. Proceeding 1992 ICSM; Chicago, IL. pp. 146–147. [Google Scholar]
- 22.Rochester RP, Owens EF. Patient placement error in rotation and its affect on the upper cervical measuring system. Chiropr Res J. 1996;3(2):40–53. [Google Scholar]
- 23.Sigler DC, Howe JW. Inter- and intra examiner reliability of the upper cervical x-rays marking system. J Manipulative Physiol Ther. 1985;8:75–80. [PubMed] [Google Scholar]
- 24.Eriksen KA. Lead foil compensating filters and their impact on reducing radiation exposure for cervical spine x-rays. J Vertebral Subluxation Res. 2007 Apr;:1–9. [Google Scholar]
- 25.Wall BF, Kendall GM, Edwards AA, Bouffler S, Muirhead CR, Meara JR. What are the risks from medical X-rays and other low dose radiation? Br J Radiol. 2006;79:285–294. doi: 10.1259/bjr/55733882. [DOI] [PubMed] [Google Scholar]
- 26.Ries LAG, Melbert D, Krapcho M, Stinchcomb DG, Howlader N, Horner MJ, Mariotto A, Miller BA, Feuer EJ, Altekruse SF, Lewis DR, Clegg L, Eisner MP, Reichman M, Edwards BK, editors. SEER Cancer Statistics Review, 1975–2005. National Cancer Institute; Bethesda, MD: http://seer.cancer.gov/csr/1975_2005/, based on November 2007 SEER data submission, posted to the SEER web site, 2008. [Google Scholar]
- 27.Preston DL, Ron E, Tokuoka S, Funamoto S, Nishi N, Soda M, Mabuchi K, Kodama K. Solid cancer incidence in atomic bomb survivors: 1958–1998. Radiat Res. 2007;168(1):1–64. doi: 10.1667/RR0763.1. [DOI] [PubMed] [Google Scholar]
- 28.Ron E, Lubin JH, Shore RE, Mabuchi K, Modan B, Pottern LM, Schneider AB, Tucker MA, Boice JD. Thyroid cancer after exposure to external radiation: a pooled analysis of seven studies. Rad Res. 1995;141:259–277. [PubMed] [Google Scholar]
- 29.U.S. Environmental Protection Agency. Estimating radiogenic cancer risks. 1994 Jun;:29–30. EPA 402-R-93-076. [Google Scholar]
- 30.Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation; Nuclear and Radiation Studies Board, Division on Earth and Life Studies, National Research Council of the National Academies. Health Risks From Exposure to Low Levels of Ionizing Radiation: BEIR VII Phase 2. Washington, DC: The National Academies Press; 2006. p. 311. [Google Scholar]
- 31.Keating JC., Jr Basic vs. applied science. J Manipulative Physiol Ther. 1988;11(5):438–40. [PubMed] [Google Scholar]
- 32.Reinert OC, editor. Chiropractic procedure and practice. Florissant (MO): Marian Press; 1976. pp. 78–95. [Google Scholar]
- 33.Downe JW, editor. Technique manual of Life College, School of Chiropractic. Marietta (GA): Life University; 1993. pp. 14–34. [Google Scholar]
- 34.Rochester RP. X-ray Safety and Quality. In: Eriksen K, editor. Upper cervical subluxation complex: A review of the chiropractic and medical literature. Philadelphia: Lippincott, Williams and Wilkins; 2004. p. 191. [Google Scholar]
- 35.Eriksen K, Rochester R. Orthospinology Procedures: An Evidence-Based Approach to Spinal Care. Philadelphia: Lippincott, Williams and Wilkins; 2007. Analyzing the Nasium X-Ray; p. 70. [Google Scholar]
- 36.Owens EF, Hosek RS. Thrust magnitudes and rates in upper cervical adjustment. In: Eriksen K, editor. Upper cervical subluxation complex: A review of the chiropractic and medical literature; 16th Annual biomechanics of the spine conference; Boulder, Colorado. June 1985; Baltimore: Lippincott Williams & Wilkins; 2004. [Google Scholar]
- 37.Rubinstein SM, Leboeuf-Yde C, Knol DL, de Koekkoek TE, Pfeifle CE, van Tulder MW. The benefits outweigh the risks for patients undergoing chiropractic care for neck pain: A prospective, multicenter, cohort study. J Manipulative Physiol Ther. 2007;30:408–418. doi: 10.1016/j.jmpt.2007.04.013. [DOI] [PubMed] [Google Scholar]
- 38.Hurwitz EL, Morgenstern H, Kominski GF, Yu F, Adams AH. A randomized trial of chiropractic manipulation and mobilization for patients with neck pain: clinical outcomes from the UCLA neck-pain study. Am J Public Health. 2002;92(10):1634–1641. doi: 10.2105/ajph.92.10.1634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McMorland G, Suter E. Chiropractic management of mechanical neck and low-back pain: A retrospective, outcome-based analysis. J Manipulative Physiol Ther . 2000 Jun;23(5):307–11. [PubMed] [Google Scholar]
- 40.Giles LG, Muller R. Chronic spinal pain syndromes: a clinical pilot trial comparing acupuncture, a nonsteroidal anti-inflammatory drug, and spinal manipulation. J Manipulative Physiol Ther. 1999 Jul–Aug;22(6):376–381. doi: 10.1016/s0161-4754(99)70082-5. [DOI] [PubMed] [Google Scholar]
- 41.Giles LG, Muller R. Chronic spinal pain: a randomized clinical trial comparing medication, acupuncture, and spinal manipulation. Spine. 2003 Jul 15;28(14: ):1490–1502. doi: 10.1097/00007632-200307150-00003. discussion 1502–1503. [DOI] [PubMed] [Google Scholar]
- 42.Wood TG, Colloca CJ, Mathews R. A pilot randomized clinical trial on the relative effect of instrumental (MFMA) versus manual (HVLA) manipulation in the treatment of cervical spine dysfunction. J Manipulative Physiol Ther . 2001 May;24(4):260–271. doi: 10.1067/mmt.2001.114365. [DOI] [PubMed] [Google Scholar]
- 43.Ernst E. Adverse effects of spinal manipulation: A systematic review. J R Soc Med . 2007 Jul;100(7):330–338. doi: 10.1258/jrsm.100.7.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yokota J, Amakusa Y, Tomita Y, Takahashi S. The medial medullary infarction (Dejerine syndrome) following chiropractic neck manipulation. No To Shinkei. 2003;55:121–125. [PubMed] [Google Scholar]
- 45.Bakris G, Dickholtz M, Sr, Meyer PM, Kravitz G, Avery E, Miller M, Brown J, Woodfield C, Bell B. Atlas vertebra realignment and achievement of arterial pressure goal in hypertensive patients: a pilot study. J Hum Hypertens . 2007 May;21(5):347–52. doi: 10.1038/sj.jhh.1002133. [DOI] [PubMed] [Google Scholar]
- 46.Hoiriis KT, Pfleger B, McDuffie FC, Cotsonis G, Elsangak O, Hinson R, Verzosa GT. A randomized clinical trial comparing chiropractic adjustments to muscle relaxants for subacute low back pain. J Manipulative Physiol Ther . 2004 Jul–Aug;27(6):388–398. doi: 10.1016/j.jmpt.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 47.Grostic JD, DeBoer KF. Roengenographic measurement of atlas laterality and rotation: A retrospective pre- and post-manipulation study. J Manipulative Physiol Ther. 1982;5(2):63–71. [PubMed] [Google Scholar]
- 48.Eriksen K, Owens EF. Upper cervical post x-ray reduction and its relationship to symptomatic improvement and spinal stability. Chiropr Res J. 1997;4(1):10–17. [Google Scholar]