Abstract
BACKGROUND
Recent research and contemporary ST elevation myocardial infarction guidelines emphasize the importance of prompt reperfusion and have redefined the traditional time to treatment metric to include prehospital paramedical staff as the point of first medical contact. However, an important knowledge gap exists relating to data systematically addressing the impact of arrival at the hospital by ambulance and the delays inherent in transfer from a community hospital to tertiary centres for percutaneous coronary intervention (PCI).
METHODS
The Which Early ST Elevation Myocardial Infarction Therapy (WEST) study initiated treatment at the point of first medical contact, including prehospital contact. Patients were randomly assigned to receive fibrinolysis with usual care or coupled with mechanical cointervention, or primary PCI. To assess the impact of this strategy on time to treatment, the following randomly assigned patient groups were compared: prehospital versus in-hospital; those arriving at the hospital by ambulance versus ambulatory self transport; and those whose initial hospital care was a community versus PCI centre.
RESULTS
Of the 328 patients enrolled in the study, 221 received fibrinolysis and 107 received primary PCI. Compared with the in-hospital group, patients who underwent prehospital random assignment (44%, n=145) experienced a 48 min reduction in median (interquartile range) time from symptom onset to first study medication (87 min [65 min to 147 min] versus 135 min [95 min to 186 min]; P<0.001) and a 56 min reduction in time to first balloon inflation (148 min [117 min to 214 min] versus 204 min [166 min to 290 min]; P<0.001). Arrival by ambulance without prehospital random assignment (n=90) incurred a substantial delay from first medical contact to reperfusion (fibrinolysis 76 min [63 min to 105 min] and PCI 160 min [141 min to 212 min]) compared with prehospital random assignment (n=145; fibrinolysis 43 min [33 min to 54 min] and PCI 105 min [90 min to 127 min]) or ambulatory patients (n=93; fibrinolysis 47 min [32 min to 68 min] and PCI 108 min [85 min to 150 min]). Community (n=165) versus PCI hospital (n=163) random assignment was associated with a longer delay from first medical contact to reperfusion: fibrinolysis, 56 min versus 47 min (P=0.008) and primary PCI, 139 min versus 105 min (P=0.001).
DISCUSSION
Prehospital diagnosis, random assignment and treatment substantially reduced treatment delay with both pharmacological and mechanical reperfusion. Those activating the prehospital medical response system without receiving prehospital random assignment experienced the longest delay from first medical contact to reperfusion, indicating a lost opportunity to enhance ST elevation myocardial infarction patient outcomes.
Keywords: Fibrinolysis, Myocardial infarction, Prehospital, Primary PCI, Systems of care
Abstract
HISTORIQUE
La recherche récente et les directives actuelles relativement à l’infarctus du myocarde avec élévation du segment ST rappellent l’importance d’administrer promptement un traitement de reperfusion et ont redéfini les délais à respecter pour inclure désormais l’intervention paramédicale préhospitalière comme premier contact médical. On déplore toutefois l’absence de données systématiques relatives à l’impact de l’arrivée à l’hôpital par ambulance et aux retards inhérents au transfert d’un hôpital régional vers un centre de soins tertiaires pour intervention coronarienne percutanée (ICP).
MÉTHODES
Dans l’étude WEST (pour Which Early ST Elevation Myocardial Infarction Therapy), on instaurait un traitement dès le premier contact médical, y compris préhospitalier. Les patients ont été assignés aléatoirement à un traitement fibrinolytique allié soit aux soins usuels, soit à une co-intervention mécanique ou une ICP primaire. Pour évaluer l’impact de cette stratégie sur le délai avant traitement, on a comparé les groupes de patients randomisés suivants: intervention pré-versus perhospitalière, arrivée à l’hôpital par ambulance ou non et soins hospitaliers initiaux administrés dans un hôpital régional ou dans un centre d’ICP.
RÉSULTATS
Parmi les 328 patients inscrits à l’étude, 221 ont reçu un traitement fibrinolytique et 107 on subi une ICP primaire. Comparativement au groupe soumis à l’intervention perhospitalière, les patients assignés à l’intervention préhospitalière (44 %, n = 145) ont connu une réduction de 48 minutes de l’éventail du quartile médian pour ce qui est du délai entre le déclenchement des symptômes et le premier médicament de l’étude (87 minutes [de 65 à 147] versus 135 minutes [de 95 à 186], p < 0,001) et une réduction de 56 minutes du délai avant la première expansion du ballonnet (148 minutes [de 117 à 214] versus 204 minutes [de 166 à 290], p < 0,001). L’arrivée en ambulance, sans randomisation à l’intervention préhospitalière (n = 90) a causé un délai substantiel entre le premier contact médical et la reperfusion (fibrinolyse 76 minutes [de 63 à 105] et ICP 160 minutes [de 141 à 212]), comparativement à la randomisation à l’intervention préhospitalière (n = 145, fibrinolyse 43 minutes [de 33 à 54] et ICP 105 minutes [de 90 à 127]) ou aux patients ambulatoires (n = 93, fibrinolyse 47 minutes [de 32 à 68] et ICP 108 minutes [de 85 à 150]). La randomisation à un hôpital régional (n = 165) plutôt qu’à un centre d’ICP (n = 163) a été associée à un délai plus long entre le premier contact médical et la reperfusion: fibrinolyse, 56 minutes versus 47 minutes (p = 0,008) et ICP primaire 139 minutes versus 105 minutes (p = 0,001).
DISCUSSION
Le diagnostic, la randomisation et le traitement préhospitaliers ont substantiellement réduit les délais pour l’application du traitement de reperfusion, tant pharmacologique que mécanique. Les sujets ayant activé le système d’intervention médicale préhospitalière sans recevoir de randomisation préhospitalière ont été soumis au délai le plus long entre le premier contact médical et la reperfusion, ce qui représente autant d’occasions perdues d’améliorer le pronostic des patients victimes d’un infarctus du myocarde avec élévation du segment ST.
The importance of time to treatment in patients with acute ST elevation myocardial infarction (STEMI) has long been recognized (1–4). Analyses of trials comparing mechanical or pharmacological reperfusion reinforce the need for timely therapy and underscore the importance of understanding regional-specific primary percutaneous coronary intervention (PCI)-related reperfusion delay (ie, door-to-balloon time minus door-to-needle time), on informing reperfusion strategies (5). Although primary PCI provides more effective reperfusion, this advantage is attenuated when significantly delayed (more than 60 min PCI reperfusion delay). The 2004 American College of Cardiology/American Heart Association STEMI guidelines re-emphasized the importance of time to treatment and defined the goal times to reperfusion from first medical contact at 30 min for fibrinolysis and 90 min for primary PCI, respectively (6,7). The guidelines also encouraged the development of regional systems-based treatment protocols and recognized the potential of prehospital treatment strategies to reduce reperfusion delays (6,7).
Notwithstanding the promotion of these guidelines and other continuous quality improvement efforts, time from symptom onset to initiation of reperfusion therapy remains suboptimal (8–10). Systematic data assessing the impact of ‘process of care’ factors on patient treatment delay and clinical outcomes are limited. Such process of care factors include the mode of presentation to the hospital (emergency medical services [EMS] versus ambulatory self transport) and the characteristics of the receiving hospital (ie, community versus tertiary care PCI centre), including the need for interfacility transport for mechanical reperfusion. Furthermore, there is a paucity of data assessing these issues specific to the metric of time from first medical contact to reperfusion relating to STEMI patients who activate the prehospital EMS. In the current report, within the Which Early ST Elevation Myocardial Infarction Therapy (WEST) study, we evaluate the impact of systematic protocol-driven measures to minimize treatment delays including prehospital diagnosis and treatment. Furthermore, the influence of the location of first medical contact on time to treatment and clinical outcomes is assessed.
METHODS
Detailed descriptions of the WEST study results were previously reported (11). Briefly, treatments included fibrinolysis with routine clinical care (group A), fibrinolysis with protocol-defined rescue PCI or angiography and PCI as required within 24 h (group B), and primary PCI (group C). All patients received acetylsalicylic acid (160 mg to 325 mg) and subcutaneous enoxaparin (1 mg/kg) at the time of random assignment, with subsequent use recommended every 12 h for a minimum of 72 h. Additional intravenous enoxaparin (0.3 mg/kg to 0.5 mg/kg) was permitted during PCI. The fibrinolytic groups (A and B) received weight-adjusted tenecteplase. Patients randomly assigned to primary PCI received a 300 mg loading dose of clopidogrel on study entry and abciximab at the time of PCI (in 97%). The primary analysis was based on a prespecified sample size of 304 patients. An additional 24 patients were subsequently enrolled to expand the prehospital cohort, for a total of 328 patients.
The present multicentre study was conducted within four Canadian metropolitan regions, with experienced tertiary care primary PCI centres acting as ‘hub’ sites for ‘spoke’ referral non-PCI centres. A systematic approach to STEMI was encouraged to facilitate expeditious treatment. The trial focused on diagnosis, random assignment and treatment of STEMI patients at the earliest point of care, including before hospital arrival in three regions. These three regions accounted for the majority of patients (n=321) enrolled in the study. For prehospital patients, advanced cardiac life support-trained paramedical staff undertook prehospital patient identification, consent and treatment, and physician overview with remote 12-lead electrocardiogram (ECG) interpretation was provided. In the prehospital patients randomly assigned to primary PCI, prenotification of the PCI centre receiving staff with transfer directly to the participating cardiac catheterization laboratory, bypassing regional hospitals and the emergency department, was undertaken to minimize delay. In the prehospital patients randomly assigned to fibrinolysis, two regions administered fibrinolysis before hospital arrival (131 of 145 prehospital randomly assigned patients), whereas one region prenotified the emergency department to expedite in-hospital fibrinolysis (14 of 145 patients).
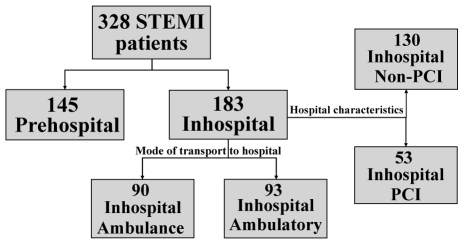
For the current analysis, the study population was classified according to whether random assignment occurred in a prehospital or in-hospital setting (Figure 1). The in-hospital patient group was then further divided based on whether patients arrived at the hospital by ambulance without prehospital random assignment (in-hospital-ambulance) or by ambulatory presentation (in-hospital-ambulatory). A further allocation was made according to the nature of the receiving hospital, ie, primary PCI centre (in-hospital-PCI) or community hospital (in-hospital-community). First medical contact was defined as the point at which medical personnel arrived to assist the patient and included prehospital paramedical staff, regardless of the above patient groupings.
Figure 1.
Study comparison groups. The study population was analyzed after separation into groups dependent on point of random assignment (pre-hospital or in-hospital). The in-hospital randomly assigned population was further divided by mode of presentation to the hospital and hospital characteristics. PCI Percutaneous coronary intervention; STEMI ST elevation myocardial infarction
Statistical analyses
Time to medical treatment was defined as the time to administration of the first study medication – fibrinolysis in groups A and B, and an anticoagulant in group C. Time to PCI was defined as the time to first balloon inflation (group C). The 30-day composite end point (death, reinfarction, refractory ischemia, congestive heart failure, cardiogenic shock and major ventricular arrhythmias) and dual end point (death and repeat myocardial infarction) were compared between groups, consistent with the primary analysis of the WEST study (12). Data were presented as count (percentage) for categorical variables and as median (interquartile range) for continuous variables. The χ2 test and nonparametric tests (ie, Wilcoxon Rank Sum, Kruskal-Wallis) with exact test methods were used where appropriate.
RESULTS
Of the 328 patients enrolled, 221 received fibrinolysis (groups A and B) and 107 received primary PCI (group C). Forty-four per cent of patients (n=145) were randomly assigned in the prehospital setting.
Baseline patient characteristics and clinical outcomes
Prehospital versus in-hospital random assignment
The baseline patient characteristics and outcomes according to prehospital and in-hospital randomly assigned groups are presented in Table 1. Prehospital randomly assigned patients were more frequently admitted to a PCI tertiary care centre (prehospital 75.9%, in-hospital 29%; P<0.001). There was no difference in the 30-day primary composite end point or the dual end point of 30-day death and repeat myocardial infarction between these groups.
TABLE 1.
Baseline patient characteristics and 30-day outcomes according to location of random assignment
| All (n=328) | Prehospital (n=145) | In-hospital (n=183) | P | |
|---|---|---|---|---|
| Age, years | 58 (50–69) | 58 (49–71) | 58 (51–68) | 0.836 |
| Women, % | 21.6 | 22.8 | 20.8 | 0.687 |
| Hypertension, % | 41.8 | 41.4 | 42.1 | 0.911 |
| Diabetes mellitus, % | 12.8 | 14.5 | 11.5 | 0.506 |
| CAD family history, % | 37.7 | 37.5 | 37.9 | 1.000 |
| History of angina, % | 25.3 | 24.1 | 26.2 | 0.702 |
| Previous MI, % | 12.8 | 13.8 | 12.0 | 0.740 |
| Previous PCI, % | 7.0 | 8.3 | 6.0 | 0.618 |
| Current smoker, % | 46.2 | 51.0 | 42.3 | 0.120 |
| Anterior MI, % | 39.9 | 38.6 | 41.0 | 0.734 |
| Killip class I, % | 96.0 | 98.6 | 93.8 | 0.043 |
| SBP, mmHg | 140 (124–160) | 131 (118–148) | 150 (130–163) | <0.001 |
| DBP, mmHg | 82 (70–95) | 78 (69–90) | 90 (75–100) | <0.001 |
| Pulse, beats/min | 73 (62–86) | 74 (62–84) | 72 (62–88) | 0.522 |
| Weight, kg | 83 (73–94) | 84 (72–95) | 83 (73–93) | 0.856 |
| Height, cm | 173 (167–178) | 173 (165–179) | 173 (167–178) | 0.764 |
| Primary composite end point*, % | 24.4 | 23.4 | 25.1 | 0.796 |
| 30-day death, % | 2.1 | 2.1 | 2.2 | 1.000 |
| 30-day re-MI, % | 6.4 | 6.9 | 6.0 | 0.822 |
| 30-day death/re-MI, % | 8.5 | 9.0 | 8.2 | 0.844 |
Data presented as median (interquartile range) unless otherwise specified.
Primary composite end point is 30-day death, reinfarction (re-myocardial infarction [MI]), refractory ischemia, congestive heart failure, cardiogenic shock and major ventricular arrhythmias. CAD Coronary artery disease; DBP Diastolic blood pressure; PCI Percutaneous coronary intervention; SBP Systolic blood pressure
In-hospital random assignment – mode of presentation and hospital characteristics
The baseline patient characteristics and outcomes of the in-hospital randomly assigned patients are presented in Table 2. Of the 183 patients randomly assigned in-hospital, 90 arrived by ambulance and 93 were ambulatory. Of these, the initial admitting hospital was a PCI centre in 26% and 32%, respectively. As expected, the majority of in-hospital patients were randomly assigned in non-PCI hospitals (n=130), consistent with study enrollment criteria (ie, patients able to undergo primary PCI within 60 min of random assignment were excluded) (11). Baseline characteristics of the four defined in-hospital groups were well balanced and there was no difference in the 30-day primary composite end point or the dual end point of 30-day death and repeat myocardial infarction between these groups.
TABLE 2.
Baseline characteristics and 30-day outcomes of in-hospital patients according to transport mode and arrival to index hospital
| In-hospital
|
In-hospital
|
||||
|---|---|---|---|---|---|
| In-hospital (n=183) | Ambulance (n=90) | Ambulatory (n=93) | PCI center (n=53) | Community center (n=130) | |
| Age, years, median (IQR) | 58 (51–68) | 58 (52–69) | 57 (50–67) | 57 (50–68) | 59 (52–68) |
| Women, % | 20.8 | 22.2 | 19.4 | 18.9 | 21.5 |
| Hypertension, % | 42.1 | 44.4 | 39.8 | 43.4 | 41.5 |
| Diabetes mellitus, % | 11.5 | 13.3 | 9.7 | 7.5 | 13.1 |
| Family history of CAD, % | 37.9 | 36.7 | 39.1 | 35.8 | 38.8 |
| History of angina, % | 26.2 | 26.7 | 25.8 | 26.4 | 26.2 |
| Previous MI, % | 12.0 | 14.4 | 9.7 | 13.2 | 11.5 |
| Previous PCI, % | 6.0 | 8.9 | 3.2 | 7.6 | 5.4 |
| Current smoker, % | 42.3 | 50.0 | 34.8 | 43.4 | 41.9 |
| Anterior MI, % | 41.0 | 44.4 | 37.6 | 41.5 | 40.8 |
| Killip class I, % | 93.8 | 90.8 | 96.7 | 91.7 | 94.6 |
| SBP, mmHg, median (IQR) | 150 (130–163) | 146 (128–160) | 151 (134–164) | 150 (130–164) | 150 (132–162) |
| DBP, mmHg, median (IQR) | 90 (75–100) | 87 (72–97) | 90 (77–100) | 90 (73–101) | 89 (76–98) |
| Pulse, beats/min, median (IQR) | 72 (62–88) | 72 (62–90) | 73 (63–88) | 72 (60–91) | 72 (64–87) |
| Weight, kg, median (IQR) | 83 (73–93) | 80 (73–92) | 85 (75–95) | 85 (77–96) | 82 (73–91) |
| Height, cm, median (IQR) | 173 (167–178) | 173 (165–178) | 173 (170–178) | 172 (165–180) | 173 (168–178) |
| Primary composite end point*, % | 25.1 | 25.6 | 24.7 | 28.3 | 23.8 |
| 30-day death, % | 2.2 | 3.3 | 1.1 | 1.9 | 2.3 |
| 30-day re-MI, % | 6.0 | 4.4 | 7.5 | 9.4 | 4.6 |
| 30-day death/MI, % | 8.2 | 7.8 | 8.6 | 11.3 | 6.9 |
Primary composite end point is 30-day death, reinfarction (re-myocardial infarction [MI]), refractory ischemia, congestive heart failure, cardiogenic shock and major ventricular arrhythmias. CAD Coronary artery disease; DBP Diastolic blood pressure; IQR Interquartile range; PCI Percutaneous coronary intervention; SBP Systolic blood pressure
Temporal delay from symptom onset to treatment
Prehospital versus in-hospital random assignment
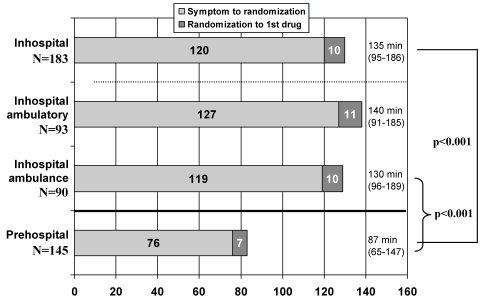
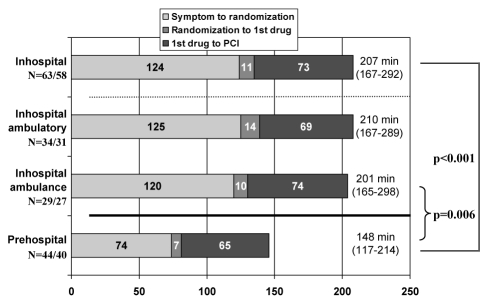
Compared with in-hospital random assignment, prehospital random assignment was associated with a 48 min reduction in time from symptom onset to medical treatment (median [interquartile range] time 135 min [95 min to 186 min] versus 87 min [65 min to 147 min]; P<0.001 (Figure 2). The prehospital subset randomly assigned to receive primary PCI (group C) underwent first balloon inflation 56 min earlier (148 min [117 min to 214 min]; P=0.001) than those randomly assigned in-hospital (204 min [166 min to 290 min]) (Figure 3).
Figure 2.
Time from symptom onset to medical treatment by point of random assignment. Median time to medical treatment with interquartile ranges are presented by point of patient random assignment and mode of presentation to the hospital. Median time from symptom onset to random assignment and random assignment to administration of the first study medication are shown
Figure 3.
Time from symptom onset to primary percutaneous coronary intervention (PCI) by point of random assignment. Median time to primary PCI with interquartile ranges are presented by point of patient random assignment and mode of presentation to the hospital. Median time from symptom onset to random assignment, random assignment to administration of the first study medication, and administration of first study medication to primary PCI are shown
Overall, among all patients arriving at the hospital by ambulance (n=235), prehospital random assignment (n=145) was associated with a 43 min advantage (87 min [65 min to 147 min]) compared with patients randomly assigned in-hospital (n=90; 130 min [96 min to 189 min]; P<0.001) (Figure 2). Among the primary PCI cohort, pre-hospital random assignment (n=44) was associated with a 53 min reduction in time to PCI (148 min [117 min to 214 min]) compared with ambulance patients randomly assigned in-hospital (n=29; 201 min [141 min to 212 min]; P=0.006) (Figure 3).
In-hospital random assignment – mode of presentation and hospital characteristics
Arriving at the hospital by ambulance without pre-hospital random assignment provided no advantage compared with ambulatory patients for time from symptom onset to medical treatment (Figure 2; 130 min [96 min to 189 min] versus 140 min [91 min to 185 min], respectively) or time from symptom onset to primary PCI (Figure 3; 201 min [165 min to 298 min] versus 210 min [167 min to 289 min], respectively).
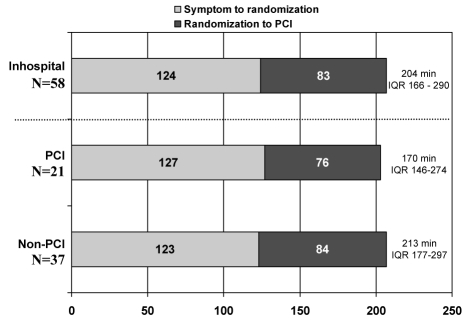
Time from random assignment to medical treatment was earlier in community than in PCI hospitals (10 min [6 min to 16 min] versus 15 min [10 min to 25 min]; P=0.031). Patients requiring transfer to a tertiary PCI centre from a community hospital for primary PCI tended to have a longer delay from symptom onset to first balloon inflation (213 min [177 min to 297 min]) than patients at a tertiary PCI hospital (170 min [146 min to 274 min]; P=0.108) (Figure 4).
Figure 4.
Time from symptom onset to primary percutaneous coronary intervention (PCI) by type of randomizing hospital. Median time to primary PCI with interquartile ranges (IQRs) are presented for in-hospital patients separated by type of randomizing hospital: PCI (tertiary care PCI centre) or non-PCI. Median time from symptom onset to random assignment and random assignment to primary PCI are shown
Temporal delay from first medical contact to treatment
Overall time from first medical contact to medical treatment was reduced with prehospital compared with in-hospital random assignment (43 min [33 min to 54 min] versus 65 min [42 min to 84 min]; P<0.001). Time from first medical contact to PCI was also reduced (105 min [90 min to 127 min] versus 143 min [100 min to 169 min]; P<0.001).
Table 3 demonstrates median and interquartile range times from first medical contact to reperfusion therapy by location of random assignment and mode of presentation to the hospital. Prehospital randomly assigned patients achieved the earliest time from first medical contact to reperfusion with fibrinolysis or primary PCI compared with in-hospital randomly assigned patients who arrived by ambulance or were ambulatory. The longest delay from first medical contact to the initiation of reperfusion therapy occurred in patients who activated the emergency medical system but were not randomly assigned prehospital (ie, an excess of 33 min for fibrinolysis and 55 min for primary PCI).
TABLE 3.
Median time from first medical contact to treatment compared by location of random assignment and mode of presentation to the hospital
| Location of random assignment and mode of transportation | Time to 1st drug (min)
|
Time to PCI (min) Group C† (n=98) | ||
|---|---|---|---|---|
| All (n=321) | Groups A* and B* (n=218) | Group C† (n=103) | ||
| Prehospital (n=145) | 43 | 43 | 41 | 105 |
| In-hospital-ambulatory (n=93) | 47 | 46 | 48 | 108 |
| In-hospital-ambulance (n=90) | 76 | 76 | 77 | 160 |
| P | <0.001 | <0.001 | <0.001 | <0.001 |
Fibrinolytic treated
Primary percutaneous coronary intervention (PCI) patients
Patients randomly assigned in-hospital at community centres experienced a prolonged time from first medical contact to reperfusion compared with PCI centres, with an initial study medication time of 56 min versus 47 min (P=0.008) and first balloon inflation of 139 min versus 105 min (P<0.001) for community and PCI hospital patients, respectively.
DISCUSSION
These data, acquired on mode of transportation and point of random assignment from the WEST study, provide several novel findings that have implications for systems planning to deliver optimal STEMI therapy. Patients who received advanced prehospital management with diagnosis, random assignment and treatment achieved the shortest delay from first medical contact (as well as symptom onset) to reperfusion, regardless of whether fibrinolysis or primary PCI was used. By contrast, those presenting to the hospital via ambulance but without advanced prehospital management had no temporal advantage over ambulatory patients. In fact, using the current metric of time from first medical contact to reperfusion, this group paradoxically experienced the longest delay to treatment. Within the environment of a clinical trial with an enhanced systematic approach to STEMI management, community hospital random assignment with subsequent transfer for PCI was associated with a modest prolongation in both time from first medical contact and symptom onset until first balloon inflation compared with patients randomly assigned within tertiary care PCI centres; 34 min and 43 min, respectively.
Canadian and international STEMI guidelines have recognized the potential advantages of enabling prehospital paramedical staff to diagnose, triage and treat STEMI patients before hospital arrival (6,7). Despite this appreciation, uptake of dedicated prehospital STEMI treatment programs within North America has been limited. This may relate, at least in part, to the perceived limitation of evidence supporting the efficacy, safety and feasibility of such programs, as well as the lack of physicians available for prehospital roles in North America as is commonly utilized in Europe. Our previous evaluation of prehospital personnel within the ASsessment of the Safety and Efficacy of a New Thrombolytic regimen (ASSENT)-3 PLUS trial (12) demonstrated similar efficacy and safety in prehospital systems whether a physician was present. Furthermore, the capability of paramedics to safely assess, diagnose, randomly assign and treat patients in the prehospital environment has been previously documented in North America and reaffirmed in the current study, which demonstrated that prehospital randomly assigned and treated patients were afforded the fastest time to reperfusion (11–14).
Previous analysis of the National Registry of Myocardial Infarction suggested a modest reduction in reperfusion delay of 10 min with fibrinolysis and 16 min with primary PCI, through completion of prehospital ECGs (15). Despite the limitations of these observational data, such an approach has been promoted and implemented in several regions within North America. By contrast, in the current study, we were unable to demonstrate a benefit of arriving by ambulance without prehospital random assignment compared with ambulatory patients. This suggests that it is not simply ambulance transport or prehospital 12-lead ECGs that facilitates early treatment, but the prehospital capability of clinical and ECG assessment linked to diagnosis and decision for reperfusion, that enhances the efficiency of care. These observations support the need for development of full paramedic-based prehospital diagnosis, triage and treatment capabilities in regions throughout the world with or without the presence of pre-hospital physicians.
Within the WEST study, encouraging systematic approaches to STEMI with early diagnosis, triage and treatment, achieved abbreviated time for symptom onset until reperfusion. The prehospital patients within the study received fibrinolysis and first balloon inflation within 87 min (65 min to 147 min) and 148 min (117 min to 214 min) of symptom onset, respectively. In the Comparison of Angioplasty and Prehospital Thrombolysis in Acute Myocardial Infarction (CAPTIM) trial (16), which used similar prehospital strategies, time to fibrinolysis and first balloon inflation were 130 min (95 min to 180 min) and 190 min (119 min to 255 min). Although direct comparison is not possible, the 30-day mortality associated with early reperfusion in the prehospital patients in WEST was 2.1%, comparing favourably with CAPTIM in which fibrinolysis patients and primary PCI patients experienced a 3.8% and 4.8% mortality rate, respectively.
Guidelines have identified optimal time to treatment goals for fibrinolysis and primary PCI of 30 min and 90 min from first medical contact, respectively (6,7). Embedded in these temporal recommendations is the differential delay of 60 min between modes of reperfusion, after which, attenuation of the benefits of primary PCI occurs. Despite focusing on systematic strategies to decrease reperfusion delay in the WEST study, the aforementioned goal times to reperfusion were not achieved. This remains true even if we account for the inherent delay associated with enrollment and random assignment (ie, approximately 10 min) within a clinical trial. Despite the requirements of paramedics to assess patients in the prehospital environment, complete all study documentation, transmit the 12-lead ECG and contact an on-call physician for random assignment, the prehospital randomly assigned patients were the only group close to achieving the guideline time to reperfusion (43 min from first medical contact to initiation of fibrinolysis and 105 min to first balloon inflation with primary PCI). Furthermore, the perceived differential delay of 60 min – at which time, primary PCI loses its advantage over fibrinolysis – was achieved in the minority of the patient population (62 min in prehospital randomly assigned patients and 78 min in the entire cohort of in-hospital randomly assigned patients). These results further stress the importance of continuous quality improvement programs to provide reality checks on actual treatment delays that are region specific.
An important practical consideration is the logistics, travel distance and time that are acceptable for STEMI patients to be transported for primary PCI rather than receiving in-hospital fibrinolysis in centres incapable of delivering timely primary PCI performed by an experienced physician. Such delays in transporting patients from non-PCI centres to PCI centres are well documented within registry data (17). Within the current analysis, transfer of patients for primary PCI from participating community hospitals to tertiary PCI centres was associated with an increased delay compared with time to treatment in PCI centres. In addition, there is significant risk to the community, patients and EMS personnel of travelling ‘lights and sirens’ associated with the hazards of accidental collision during interfacility transport (18–20).
The present analysis is based on a post hoc retrospective comparison of patients randomly assigned within the open-label WEST trial dependent on point of random assignment and type of receiving hospital. Within each participating WEST study region, different patient process of care factors exist, which may cause unanticipated bias. Although we have presented clinical events within the various subgroups for completeness, the sample size limits the capability of assessing differences between the various subgroups.
Optimal care in STEMI can be achieved via rapid prehospital diagnosis and prompt reperfusion therapy. Although timelines for reperfusion are explicitly stated in STEMI guidelines, there is little evidence to show that efforts are being made at a national level to improve systems to successfully implement guideline-stipulated goals in Canada. The current study provides evidence to energize their implementation.
REFERENCES
- 1.Boersma E, Maas AC, Deckers JW, Simoons ML. Early thrombolytic treatment in acute myocardial infarction: Reappraisal of the golden hour. Lancet. 1996;348:771–5. doi: 10.1016/S0140-6736(96)02514-7. [DOI] [PubMed] [Google Scholar]
- 2.McNamara RL, Wang Y, Herrin J, et al. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2006;47:2180–6. doi: 10.1016/j.jacc.2005.12.072. [DOI] [PubMed] [Google Scholar]
- 3.Nallamothu B, Fox KA, Kennelly BM, et al. Relationship of treatment delays and mortality in patients undergoing fibrinolysis and primary percutaneous coronary intervention. The Global Registry of Acute Coronary Events. Heart. 2007;93:1552–5. doi: 10.1136/hrt.2006.112847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pinto DS, Southard M, Ciaglo L, Gibson CM. Door-to-balloon delays with percutaneous coronary intervention in ST-elevation myocardial infarction. Am Heart J. 2006;151(6 Suppl):S24–9. doi: 10.1016/j.ahj.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 5.Nallamothu BK, Bates ER. Percutaneous coronary intervention versus fibrinolytic therapy in acute myocardial infarction: Is timing (almost) everything? Am J Cardiol. 2003;92:824–6. doi: 10.1016/s0002-9149(03)00891-9. [DOI] [PubMed] [Google Scholar]
- 6.Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction; A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of patients with acute myocardial infarction) J Am Coll Cardiol. 2004;44:E1–211. doi: 10.1016/j.jacc.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 7.Armstrong PW, Bogaty P, Buller CE, Dorian P, O’Neill BJ. The 2004 ACC/AHA Guidelines: A perspective and adaptation for Canada by the Canadian Cardiovascular Society Working Group. Can J Cardiol. 2004;20:1075–9. [PubMed] [Google Scholar]
- 8.Bradley EH, Herrin J, Wang Y, et al. Strategies for reducing the door-to-balloon time in acute myocardial infarction. N Engl J Med. 2006;355:2308–20. doi: 10.1056/NEJMsa063117. [DOI] [PubMed] [Google Scholar]
- 9.Henry TD, Sharkey SW, Burke MN, et al. A regional system to provide timely access to percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation. 2007;116:721–8. doi: 10.1161/CIRCULATIONAHA.107.694141. [DOI] [PubMed] [Google Scholar]
- 10.Ting HH, Rihal CS, Gersh BJ, et al. Regional systems of care to optimize timeliness of reperfusion therapy for ST-elevation myocardial infarction: The Mayo Clinic STEMI Protocol. Circulation. 2007;116:729–36. doi: 10.1161/CIRCULATIONAHA.107.699934. [DOI] [PubMed] [Google Scholar]
- 11.Armstrong PW. A comparison of pharmacologic therapy with/without timely coronary intervention versus primary percutaneous intervention early after ST-elevation myocardial infarction: The WEST (Which Early ST-elevation myocardial infarction Therapy) study. Eur Heart J. 2006;27:1530–8. doi: 10.1093/eurheartj/ehl088. [DOI] [PubMed] [Google Scholar]
- 12.Welsh RC, Chang W, Goldstein P, et al. Time to treatment and the impact of a physician on prehospital management of acute ST elevation myocardial infarction: Insights from the ASSENT-3 PLUS trial. Heart. 2005;91:1400–6. doi: 10.1136/hrt.2004.054510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Welsh RC, Travers A, Senaratne M, Williams R, Armstrong PW. Feasibility and applicability of paramedic-based prehospital fibrinolysis in a large North American center. Am Heart J. 2006;152:1007–14. doi: 10.1016/j.ahj.2006.06.022. [DOI] [PubMed] [Google Scholar]
- 14.Weaver WD, Cerqueira M, Hallstrom AP, et al. Prehospital-initiated vs hospital-initiated thrombolytic therapy. The Myocardial Infarction Triage and Intervention Trial. JAMA. 1993;270:1211–6. [PubMed] [Google Scholar]
- 15.Curtis JP, Portnay EL, Wang Y, et al. The pre-hospital electrocardiogram and time to reperfusion in patients with acute myocardial infarction, 2000-2002: Findings from the National Registry of Myocardial Infarction-4. J Am Coll Cardiol. 2006;47:1544–52. doi: 10.1016/j.jacc.2005.10.077. [DOI] [PubMed] [Google Scholar]
- 16.Bonnefoy E, Lapostolle F, Leizorovicz A, et al. Primary angioplasty versus prehospital fibrinolysis in acute myocardial infarction: A randomised study. Lancet. 2002;360:825–9. doi: 10.1016/S0140-6736(02)09963-4. [DOI] [PubMed] [Google Scholar]
- 17.Nallamothu BK, Bates ER, Herrin J, Wang Y, Bradley EH, Krumholz HM. Times to treatment in transfer patients undergoing primary percutaneous coronary intervention in the United States: National Registry of Myocardial Infarction (NRMI)-3/4 analysis. Circulation. 2005;111:761–7. doi: 10.1161/01.CIR.0000155258.44268.F8. [DOI] [PubMed] [Google Scholar]
- 18.Clawson JJ, Martin RL, Cady GA, Maio RF. The wake-effect – emergency vehicle-related collisions. Prehosp Disaster Med. 1997;12:274–7. [PubMed] [Google Scholar]
- 19.Custalow CB, Gravitz CS. Emergency medical vehicle collisions and potential for preventive intervention. Prehosp Emerg Care. 2004;8:175–84. doi: 10.1016/s1090-3127(03)00279-x. [DOI] [PubMed] [Google Scholar]
- 20.Vukmir RB. Medical malpractice: Managing the risk. Med Law. 2004;23:495–513. [PubMed] [Google Scholar]