Abstract
Introduction:
There has been substantial clinical and research interest in describing the complete natural history of bipolar disorder, and related to this significant debate in regard to the validity of the bipolar diagnosis in very young children. Given the high heritability of bipolar disorder, longitudinal high risk studies can provide important information in regard to the evolution of the disorder.
Methods:
A selected review and discussion of the findings from key longitudinal high risk studies are presented focusing on the relevance for mapping the early course of illness, addressing the validity of the bipolar diagnosis in very young referred children and implications for diagnosis and organization of services.
Results:
To date, there have been findings reported from several longitudinal high risks studies starting with well characterized affected parents, all of which support an evolution of psychopathology from non-specific disorders to frank bipolarity. Early childhood antecedents include internalizing and sleep disorders and typically not behavioural disorders. In the majority of cases, the early mood pathology and associated morbidity is related to the depressive polarity. None of these studies have reported a single case of pre-pubertal mania.
Conclusions:
These findings highlight the importance of considering the clinical course and the family history in diagnostic formulation in pediatric patients early in the course of a psychiatric illness. The implications of these findings for early intervention and organization of child psychiatry services are discussed.
Keywords: antecedents, children at high risk, prepubertal bipolar disorder
RÉSUMÉ
Introduction:
Les chercheurs et les cliniciens s’intéressent fortement aux premières manifestations du trouble bipolaire, et donc à la question–controversée–du diagnostic de ce trouble chez les très jeunes enfants. En raison de la forte composante génétique du trouble bipolaire, les études longitudinales effectuées sur des enfants dont les parents souffrent de ce trouble peuvent répondre à ces questions et expliquer les résultats controversés majoritairement tirés d’échantillons hétérogènes formés de sujets à risque élevé et d’enfants référés.
Méthode:
Une revue des études pertinentes qui emploient comme critères, le diagnostique précis du trouble bipolaire chez les parents accompagnés des observations longitudinales de leurs enfants, est présentée.
Résultats:
À l’heure actuelle, les résultats d’études longitudinales sur ces enfants à risque élevé attestent tous d’une évolution de la psychopathologie, du trouble bipolaire non spécifié au trouble bipolaire marqué. Cependant ces études n’ont fait état d’aucun cas de manie prépubertaire. On retrouve plutôt les troubles d’anxiété et de sommeil et rarement le troubles de comportement. Dans les cas ou il y a une évolution vers les troubles affectifs, ils sont plutôt du pole dépressif.
Conclusion:
L’article présente les implications de ces constatations sur le diagnostic, l’intervention précoce et l’organisation des services de prévention.
Introduction
There has been increasing recognition that major psychiatric disorders including bipolar disorder (BD) often onset during adolescence (Paus et al., 2008), although not accurately diagnosed until many years later. Therefore, much effort has been focused on describing the early course of illness for patients suffering from bipolar and psychotic disorders, as evidenced for example by the number of publications about first episode patients (DelBello et al., 2007; Baethge et al., 2008). In relation to this effort, one of the most interesting and controversial debates in psychiatry over the past decade has centered on the validity of the bipolar diagnosis in very young, prepubescent children. This debate has been constructive in that it has highlighted a number of shortcomings of the current DSM diagnostic system (Duffy et al., 2007) and differences in the conceptualization and interpretation of clinical symptoms and course of illness (Dubicka et al., 2007). One very helpful research approach to clarify the early course of bipolar disorder is the longitudinal study of children of bipolar parents. A confirmed positive family history is the single most robust risk factor for developing the illness given the high heritability (higher than that of schizophrenia) (Duffy et al., 2000; Smoller & Finn, 2003). In this paper, I will outline the major findings pertaining to the early course of bipolar disorder as derived from longitudinal offspring studies and discuss the implications of these for the ongoing debate regarding the diagnosis of pediatric BD and for organization of psychiatric services.
Longitudinal studies of children of bipolar parents
There have been several reviews of studies of heterogeneous groups of bipolar parents and their offspring, largely cross-sectional in nature; that is findings based on a single assessment of lifetime psychopathology (for reviews see (Hodgins et al., 2002; Lapalme et al., 1997; DelBello & Geller, 2001). Most of these studies have reported an elevated rate of a broad range of lifetime psychiatric disorders among offspring including mood, anxiety and substance use disorders, as well as high rates of comorbidity. Some studies have found an elevated rate of attention deficit disorder (ADHD) and behavioural disorders (Chang et al., 2000), while others have not (Hillegers et al., 2005). A recent large cross-sectional study of high risk and control offspring reported that, after adjusting for confounding variables (i.e. socioeconomic status, psychiatric disorder in the non-proband parent, within family correlations), there was no elevated rate of ADHD in the overall high risk group compared to controls (Birmaher et al., 2009).
Despite the growing number of high risk studies, few have reported repeated longitudinal assessments of the same offspring over time and development. This likely reflects the fact that longitudinal studies are difficult and expensive to conduct. They are difficult to conduct because you need to engage and maintain contact with the families (parents and offspring) in order to communicate the findings and their relevance in order to encourage continued motivation, you must compete for research funding to ensure continuity with the families and with research staff and you must make a commitment to stay geographically local, with the flexibility of travel to reassess mobile offspring (away at university or in the event of family moves). These are not easy tasks in a large country like Canada, with relatively inadequate research funding (many outstanding competitors chasing few grant dollars), and limited funding terms (2 to 3 to 5 years terms). In spite of these challenges, there are four longitudinal high risk studies, in addition to the one I have been leading over the last 15 years.
Akiskal and colleagues described the course of psychopathology on average over a 3 year period in the clinically referred offspring or siblings of patients followed in their mood disorders subspecialty clinic (Akiskal et al., 1985). The proband bipolar patients were well known to the research team and expertly diagnosed; which is not a trivial point given that the validity of high risk studies begins with the accuracy of diagnosis in the parent. These referred young relatives (mostly adolescents), presented with neurotic (anxiety) disorders and mood disturbances (dysthymia, cyclothymia) and then went on to develop major mood episodes including major depression and hypomania. No referred youth developed mania prior to adolescence.
Subsequently, Hammen and colleagues reported an important study comparing outcomes up to 3 years among the offspring of women diagnosed with either unipolar depression, BD, chronic medical illness or no illness (controls) (Hammen et al., 1990). Children of bipolar mothers tended to develop anxiety and mild depressive disorders and functioned generally much better than the children of depressed mothers. However, activated symptoms below diagnostic threshold were observed in a few cases and the offspring of bipolar mothers were seen to develop more significant psychopathology later in development (adolescence). Again, there were no cases of prepubertal mania identified.
More recently, a Dutch research team, described psychopathological outcomes in offspring of bipolar parents over 5 years of prospective follow-up (Hillegers et al., 2005). The parents were conservatively diagnosed and the majority of these families were recruited from the community. The offspring developed an elevated rate of mood disorders, debuting most often with major depression. There were no cases of prepubertal mania, and activated episodes tended to onset several years following the first major depressive episode. There was no elevated rate of ADHD or behavioural disorders in this high risk cohort. Furthermore, the offspring of bipolar parents had comparable attachment and social functioning to controls, however following the onset of illness there were associated changes and impairment in these domains (Reichart et al., 2007; Reichart et al., 2009).
Finally, among the offspring of Amish bipolar probands previously identified for genetic studies, Shaw and colleagues studied the first reliable symptoms of impending BD (Shaw et al., 2005). Findings demonstrated that non-specific symptoms including anxiety and sleep problems later develop into activated, cognitive (distractibility) and mood symptoms and that these harbingers occurred episodically among the high risk offspring compared to controls. The episodic nature of BD is arguably the most characteristic feature of the illness (Angst & Marneros, 2001; Grof et al., 1995). Of note, there was no single case of prepubertal mania nor was there an elevated rate of ADHD or behavioural disorder in these high risk offspring.
In our own high risk study, we attempted to control for the effects of assortative mating and heterogeneity on psychopathological outcome and on the early course of mood disorder. Specifically, we limited inclusion to families in which there was one expertly diagnosed bipolar parent (based on a wealth of longitudinal clinical information) and one confirmed well parent (no lifetime major psychiatric illness) (Duffy et al., 1998; Duffy et al., 2002; Duffy et al., 2007a). Given that we treated these parents systematically in a clinical research environment, we were also able to divide the parents into unequivocal lithium responders or non-responders based on a research protocol described elsewhere (Turecki et al., 1998). There is convergent data showing that long-term response to lithium monotherapy (over 3 years minimum after a highly recurrent pre-treatment course), identifies a homogenous subtype of BD with characteristic genetic and neurobiological characteristics (Alda, 2004; Grof P., 2009; Mamdani et al., 2008; Kruger et al., 2006).
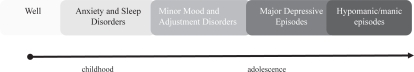
Over 15 years, we were able to show that despite controlling for assortative mating and heterogeneity of bipolar subtypes, offspring from both high risk groups manifest a broad range of psychopathological conditions. Furthermore, we found evidence that BD evolves in predictable clinical stages from non-specific anxiety and sleep disorders, to subthreshold mood disturbances and sensitivity to stress (adjustment disorders) and then starting in adolescence major mood episodes, typically depression (Duffy et al., 2009b please see Figure 1). While not all offspring developed all stages, the sequence was the same in the majority of cases. Once major mood episodes started, they recurred into adulthood (Duffy et al., 2009a).
We, like other groups, did not find any diagnosable cases of prepubertal mania. While ADHD was not elevated in the whole group compared to controls, it was elevated among the offspring of lithium non-responders as were other precursors including cluster A traits, learning disabilities and psychosis (Duffy et al., 2007a). This suggested to us that in a subgroup of offspring from atypical parents, there may be a neurodevelopmental overlap similar to that seen in children at risk for psychotic disorders (Sigurdsson et al., 1999).
The implications of the findings from high risk studies
Our work agrees with that of other research groups around the world who study offspring of well-characterized parents over time. That is, we have clearly found that BD can begin as anxiety, sleep and sub-threshold mood problems, as well as sensitivity to stress among children at confirmed familial risk. These non-specific presentations evolve into mood episodes and frank bipolarity later in adolescence and adulthood. While ADHD and behavioural problems do not characterize the overall population of high risk offspring of carefully diagnosed parents, cognitive problems do appear in a subgroup of children of parents with psychotic spectrum or atypical BD. These findings suggest that clinical staging may be an important and useful way to improve the early diagnosis of BD in high risk children, in a similar way to identifying prodromal stages in youth at risk for psychotic illnesses (McGorry et al., 2008). These findings also underscore the failure of our current diagnostic system to identify early stages of impending illness, especially early in development. To provide a clinically meaningful context to psychiatric presentations, we must include a carefully collected (if possible based on face to face interviews) family history of psychiatric disorder and a careful history of the evolving clinical course of illness – in other words, the symptom checklist driven DSM is not sufficient for early accurate diagnosis of BD.
In addition, high risk longitudinal studies of the offspring of carefully characterized parents do not find evidence of mania occurring prior to adolescence. However, studies of clinical samples of children unselected for family history report manic-like symptoms (Wozniak et al., 1995) and prepubertal mania (Geller et al., 2008), mostly in the United States compared to England (Harrington & Myatt, 2003). Some have offered that these presentations might in part reflect early exposure to antidepressants and/or stimulants (Reichart & Nolen, 2004; DelBello et al., 2001). Others have shown that the syndrome synonymous with pediatric BD may be more a barometer for poor outcome and a number of psychiatric disorders later in life (Dickstein et al., 2007; Brotman et al., 2007; Brotman et al., 2006; Meyer & Carlson, 2003). The bottom line is that clinical diagnosis in children early in the course has poor stability over time and poor prognostic accuracy. Unless we include familial risk and clinical course in the diagnostic formulation as in other areas of medicine, we really do not know what we are actually dealing with. In light of this, diagnosis relying on self-report symptom rating scales, not uncommonly the case in pediatric mental health, clearly is unacceptable and cannot replace a comprehensive psychiatric evaluation. We must think like our internal medicine colleagues and put together a complex number of valid clues in order to refine psychiatric diagnoses early in the course of illness.
Clinical Stages in the evolution of bipolar disorder based on high risk studies1
Is it important to refine the diagnosis?
Yes. It is estimated that patients with BD are generally not accurately diagnosed until at least 10 years of full blown illness (Ghaemi et al., 2000). Untreated illness is associated with the highest suicide risk (Baldessarini et al., 2003; Ahrens et al., 1995). In addition, there is evidence that repeated major mood episodes are associated with neuroanatomical changes, refractoriness to treatment, a higher rate of complications, comorbidity and morbidity and persistent neurocognitive changes (MacQueen et al., 2001; Duffy A. et al., 2009; Judd & Akiskal, 2003; Hajek et al., 2008). It is entirely plausible, although as yet not proven, that treating early in the course may be associated with a better or more complete response and less complicated treatment regime. We have provided preliminary evidence that early in the course affected offspring tolerate and respond to mood stabilizer monotherapy (Duffy et al., 2007b; Duffy et al., 2009c). We also know that there is a tragic disconnect between the high risk period for onset of major mood disorder and the least well served sector of the population; that being 15–25 year olds (Waddell et al., 2002). By working with families as the unit of surveillance (based on an affected 1st degree relative) we can identify high risk children early on and have the opportunity to engage these families and reduce the time to accurate diagnosis and effective treatment (Duffy, 2000; Harrington & Clark, 1998).
Does the current organization of child mental health services in Canada address the needs of high risk youth?
No. The current organization of mental health services in Canada fragments adult from child and adolescent services and these sectors operate as separate solitudes. Therefore, we are not properly organized to clinically address familial (genetically) based illnesses such as schizophrenia and BD. Further, the psychiatrically ill, such as bipolar patients and their families, are not well served in the current organization of mental health services. The problem here relates to the fact that surveillance and medical intervention (the primary treatment) necessary for patients suffering from BD is often delayed because the system does not differentiate between major psychiatric disorders and emotional/family problems that require a different approach to diagnosis, treatment and follow-up. In other words, child psychiatrists are often busy dealing with psychological and/or sociological issues and often in young children, while teens are less well served (some hospitals cut services at age 16) in spite of being the highest risk group for the first manifestation of major psychiatric disorders requiring as a first line pharmacological intervention. Furthermore, child mental health programs tend not to take into account the familial psychiatric risk and/or differentiate between primary, secondary and tertiary care needs.
Concluding remarks
High risk studies have reconciled seeming controversies in child psychiatry, including the question of the validity of the bipolar diagnosis in prepubertal children. Longitudinal studies of high risk children of bipolar parents have made possible the mapping of early clinical stages of illness. We now need to identify vulnerability markers and understand the nature of the inherited abnormalities indicating among those at familial risk who will become ill and how. We also need to identify the biological correlates of clinical stages to help us validate the clinical observation and understand factors important to the progression of illness. As in the case of breast cancer and other medical illnesses, we should be developing high risk screening programs that cover the adolescent and early adult period for those at confirmed familial risk of BD (as well as other major psychiatric disorders). Finally we need to study if intervening at early stages of illness provide a clear benefit in terms of preventing illness progression, reducing morbidity and mortality. This will require a fundamental change in how we are clinically organized and how we approach diagnosis early in the course of illness and over development.
Acknowledgements/Conflict of Interest
Many thanks to all of those who have made the high risk research possible and fruitful, in particular sincere and heartfelt thanks to our research families, to Paul Grof and Martin Alda for their collaboration, and to my family for their unwavering support. Dr. Duffy is the recipient of a Senior Clinical Research Scholar Award from the Faculty of Medicine at Dalhousie University. Dr. Duffy was supported during the tenure of the high risk research by a Canada Research Chair award and an Independent Investigator award from NARSAD. The high risk research was supported by operating grants from OMHF and the CIHR, as well as an investigator sponsored study funded by Astra Zeneca Canada. Dr. Duffy has no conflict with respect to this article.
Footnotes
Taken from Duffy et al, Journal of Affective Disorders, 2009 Epub ahead of print
References
- Ahrens B, Muller-Oerlinghausen B, Schou M, et al. Excess cardiovascular and suicide mortality of affective disorders may be reduced by lithium prophylaxis. Journal of Affective Disorders. 1995;33:67–75. doi: 10.1016/0165-0327(94)00074-j. [DOI] [PubMed] [Google Scholar]
- Akiskal HS, Downs J, Jordan P, Watson S, Daugherty D, Pruitt DB. Affective disorders in referred children and younger siblings of manic-depressives. Mode of onset and prospective course. Archives of General Psychiatry. 1985;42:996–1003. doi: 10.1001/archpsyc.1985.01790330076009. [DOI] [PubMed] [Google Scholar]
- Alda M. The phenotypic spectra of bipolar disorder. European Neuropsychopharmacology. 2004;14(Suppl. 2):94–99. doi: 10.1016/j.euroneuro.2004.03.006. [DOI] [PubMed] [Google Scholar]
- Angst J, Marneros A. Bipolarity from ancient to modern times: conception, birth and rebirth. Journal of Affective Disorders. 2001;67:3–19. doi: 10.1016/s0165-0327(01)00429-3. [DOI] [PubMed] [Google Scholar]
- Baethge C, Hennen J, Khalsa HM, Salvatore P, Tohen M, Baldessarini RJ. Sequencing of substance use and affective morbidity in 166 first-episode bipolar I disorder patients. Bipolar Disorders. 2008;10:738–741. doi: 10.1111/j.1399-5618.2007.00575.x. [DOI] [PubMed] [Google Scholar]
- Baldessarini RJ, Tondo L, Hennen J. Lithium treatment and suicide risk in major affective disorders: update and new findings. Journal of Clinical Psychiatry. 2003;64:44–52. [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Monk K, Kalas C, Goldstein B, Hickey MB, et al. Lifetime psychiatric disorders in school-aged offspring of parents with bipolar disorder: the Pittsburgh Bipolar Offspring study. Archives of General Psychiatry. 2009;66:287–296. doi: 10.1001/archgenpsychiatry.2008.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brotman MA, Kassem L, Reising MM, Guyer AE, Dickstein DP, Rich BA, et al. Parental diagnoses in youth with narrow phenotype bipolar disorder or severe mood dysregulation. American Journal of Psychiatry. 2007;164:1238–1241. doi: 10.1176/appi.ajp.2007.06101619. [DOI] [PubMed] [Google Scholar]
- Brotman MA, Schmajuk M, Rich BA, Dickstein DP, Guyer AE, Costello EJ, et al. Prevalence, clinical correlates, and longitudinal course of severe mood dysregulation in children. Biological Psychiatry. 2006;60:991–997. doi: 10.1016/j.biopsych.2006.08.042. [DOI] [PubMed] [Google Scholar]
- Chang KD, Steiner H, Ketter T. Psychiatric phenomenology of child and adolescent bipolar offspring. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:453–460. doi: 10.1097/00004583-200004000-00014. [DOI] [PubMed] [Google Scholar]
- DelBello MP, Geller B. Review of studies of child and adolescent offspring of bipolar parents. Bipolar Disorders. 2001;3:325–334. doi: 10.1034/j.1399-5618.2001.30607.x. [DOI] [PubMed] [Google Scholar]
- DelBello MP, Hanseman D, Adler CM, Fleck DE, Strakowski SM. Twelve-month outcome of adolescents with bipolar disorder following first hospitalization for a manic or mixed episode. American Journal of Psychiatry. 2007;164:582–590. doi: 10.1176/ajp.2007.164.4.582. [DOI] [PubMed] [Google Scholar]
- DelBello MP, Soutullo CA, Hendricks W, Niemeier RT, McElroy SL, Strakowski SM. Prior stimulant treatment in adolescents with bipolar disorder: association with age at onset. Bipolar Disorders. 2001;3:53–57. doi: 10.1034/j.1399-5618.2001.030201.x. [DOI] [PubMed] [Google Scholar]
- Dickstein BA, Nelson EE, McClure EB, Grimley ME, Knopf L, Brotman MA, et al. Cognitive flexibility in phenotypes of pediatric bipolar disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:341–345. doi: 10.1097/chi.0b013e31802d0b3d. [DOI] [PubMed] [Google Scholar]
- Dubicka B, Carlson GA, Vail A, Harrington R. Prepubertal mania: diagnostic differences between US and UK clinicians. European Child and Adolescent Psychiatry. 2007:649–657. doi: 10.1007/s00787-007-0649-5. [DOI] [PubMed] [Google Scholar]
- Duffy A, Hajek T, Alda M, Grof P, Milin R, MacQueen GM. Neurocognitive functioning in the early stages of bipolar disorder: Visual backward masking performance in high risk offspring. European Archives of Psychiatry and Clinical Neuroscience. 2009 doi: 10.1007/s00406-008-0862-3. [DOI] [PubMed] [Google Scholar]
- Duffy A, Alda M, Crawford L, Milin R, Grof P. The early manifestations of bipolar disorder: a longitudinal prospective study of the offspring of bipolar parents. Bipolar Disorders. 2007a;9:828–838. doi: 10.1111/j.1399-5618.2007.00421.x. [DOI] [PubMed] [Google Scholar]
- Duffy A, Alda M, Hajek T, Grof P.2009aThe early course of bipolar disorder in a prospective study of high-risk offspring British Journal of Psychiatry in press. [DOI] [PubMed] [Google Scholar]
- Duffy A, Alda M, Hajek T, Sherry S, Grof P.2009bEarly stages in the development of bipolar disorder Journal of Affective Disorders in press. [DOI] [PubMed] [Google Scholar]
- Duffy A, Milin R, Grof P. Maintenance treatment of adolescent bipolar disorder: Open study of the effectiveness and tolerability of quetiapine. BioMed Central Psychiatry. 2009c doi: 10.1186/1471-244X-9-4. Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy A. Toward effective early intervention and prevention strategies for major affective disorders: a review of antecedents and risk factors. The Canadian Journal of Psychiatry. 2000;45:340–348. doi: 10.1177/070674370004500402. [DOI] [PubMed] [Google Scholar]
- Duffy A. Does bipolar disorder exist in children? A selected review. Canadian Journal of Psychiatry. 2007a;52:409–417. doi: 10.1177/070674370705200702. [DOI] [PubMed] [Google Scholar]
- Duffy A. Does bipolar disorder exist in children? A selected review. Canadian Journal of Psychiatry. 2007b;52:409–417. doi: 10.1177/070674370705200702. [DOI] [PubMed] [Google Scholar]
- Duffy A, Alda M, Crawford L, Milin R, Grof P. The early manifestations of bipolar disorder: a longitudinal prospective study of the offspring of bipolar parents. Bipolar Disorders. 2007b;9:828–838. doi: 10.1111/j.1399-5618.2007.00421.x. [DOI] [PubMed] [Google Scholar]
- Duffy A, Alda M, Kutcher S, Cavazzoni P, Robertson C, Grof E, et al. A prospective study of the offspring of bipolar parents responsive and non-responsive to lithium treatment. Journal of Clinical Psychiatry. 2002;63:1171–1178. doi: 10.4088/jcp.v63n1213. [DOI] [PubMed] [Google Scholar]
- Duffy A, Alda M, Kutcher S, Fusee C, Grof P. Psychiatric symptoms and syndromes among adolescent children of parents with lithium-responsive or lithium-nonresponsive bipolar disorder. The American Journal of Psychiatry. 1998;155:431–433. doi: 10.1176/ajp.155.3.431. [DOI] [PubMed] [Google Scholar]
- Duffy A, Alda M, Milin R, Grof P. A consecutive series of treated affected offspring of parents with bipolar disorder: is response associated with the clinical profile? The Canadian Journal of Psychiatry. 2007b;52:369–375. doi: 10.1177/070674370705200606. [DOI] [PubMed] [Google Scholar]
- Duffy A, Grof P, Robertson C, Alda M. The implications of genetic studies of major mood disorders for clinical practice. Journal of Clinical Psychiatry. 2000;61:630–637. doi: 10.4088/jcp.v61n0906. [DOI] [PubMed] [Google Scholar]
- Geller B, Tillman R, Bolhofner K, Zimerman B. Child bipolar I disorder: prospective continuity with adult bipolar I disorder; characteristics of second and third episodes; predictors of 8-year outcome. Archives of General Psychiatry. 2008;65:1125–1133. doi: 10.1001/archpsyc.65.10.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghaemi SN, Boiman EE, Goodwin FK. Diagnosing bipolar disorder and the effect of antidepressants: a naturalistic study. Journal of Clinical Psychiatry. 2000;61:804–808. doi: 10.4088/jcp.v61n1013. [DOI] [PubMed] [Google Scholar]
- Grof P.2009Sixty year of lithium responders Neuropsychobiology in press. [DOI] [PubMed] [Google Scholar]
- Grof P, Alda M, Ahrens B. Clinical course of affective disorders: were Emil Kraepelin and Jules Angst wrong. Psychopathology. 1995;28(Suppl 1):73–80. doi: 10.1159/000284960. [DOI] [PubMed] [Google Scholar]
- Hajek T, Gunde E, Slaney C, Propper L, MacQueen G, Duffy A, et al. Striatal volumes in affected and unaffected relatives of bipolar patients - high-risk study. Journal of Psychiatric Research. 2008 doi: 10.1016/j.jpsychires.2008.10.008. [DOI] [PubMed] [Google Scholar]
- Hammen C, Burge D, Burney E, Adrian C. Longitudinal study of diagnoses in children of women with unipolar and bipolar affective disorder. Archives of General Psychiatry. 1990;47:1112–1117. doi: 10.1001/archpsyc.1990.01810240032006. [DOI] [PubMed] [Google Scholar]
- Harrington R, Clark A. Prevention and early intervention for depression in adolescence and early adult life. European Archives of Psychiatry and Clinical Neuroscience. 1998;248:32–45. doi: 10.1007/s004060050015. [DOI] [PubMed] [Google Scholar]
- Harrington R, Myatt T. Is pre-adolescent mania the same condition as adult mania? A British perspective. Biological Psychiatry. 2003;53:961–969. doi: 10.1016/s0006-3223(03)00315-9. [DOI] [PubMed] [Google Scholar]
- Hillegers MH, Reichart CG, Wals M, Verhulst FC, Ormel J, Nolen WA. Five-year prospective outcome of psychopathology in the adolescent offspring of bipolar parents. Bipolar Disorders. 2005;7:344–350. doi: 10.1111/j.1399-5618.2005.00215.x. [DOI] [PubMed] [Google Scholar]
- Hodgins S, Faucher B, Zarac A, Ellenbogen MA. Children of parents with bipolar disorder: a population at high risk for major affective disorders. Child and Adolescent Psychiatric Clinics of North America. 2002;11:533–554. doi: 10.1016/s1056-4993(02)00002-0. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS. The prevalence and disability of bipolar spectrum disorders in the US population: The ECA database taking into account subthreshold cases. Journal of Affective Disorders. 2003;73:123. doi: 10.1016/s0165-0327(02)00332-4. [DOI] [PubMed] [Google Scholar]
- Kruger S, Alda M, Young LT, et al. Risk and resilience markers in bipolar disorder: Brain responses to emotional challenge in bipolar patients and their healthy siblings. American Journal of Psychiatry. 2006;163:257–264. doi: 10.1176/appi.ajp.163.2.257. [DOI] [PubMed] [Google Scholar]
- Lapalme M, Hodgins S, Laroche C. Children of parents with bipolar disorder: a meta-analysis of risk for mental disorders. The Canadian Journal of Psychiatry. 1997;42:623–631. doi: 10.1177/070674379704200609. [DOI] [PubMed] [Google Scholar]
- MacQueen GM, Young LT, Joffe RT. A review of psychosocial outcome in patients with bipolar disorder. Acta Psychiatrica Scandinavica. 2001;103:163–170. doi: 10.1034/j.1600-0447.2001.00059.x. [DOI] [PubMed] [Google Scholar]
- Mamdani F, Alda M, Grof P, Young LT, Rouleau G, Turecki G. Lithium response and genetic variation in the CREB family of genes. American Journal of Medical Genetics, Behavioral Neuropsychiatry, Genetics. 2008;147B:500–504. doi: 10.1002/ajmg.b.30617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGorry P, Killackey E, Yung A. Early intervention in psychosis: concepts, evidence and future directions. World Psychiatry. 2008;7:148–156. doi: 10.1002/j.2051-5545.2008.tb00182.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer SE, Carlson G. Bipolar disorder in youth: An update. Current Psychosis and Therapeutics Reports. 2003;1:79–84. [Google Scholar]
- Paus T, Keshavan M, Giedd JN. Why do many psychiatric disorders emerge during adolescence? Nature Neuroscience. 2008;9:947–957. doi: 10.1038/nrn2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichart CG, Nolen WA. Earlier onset of bipolar disorder in children by antidepressants or stimulants? An hypothesis. Journal of Affective Disorders. 2004;78:81–84. doi: 10.1016/s0165-0327(02)00180-5. [DOI] [PubMed] [Google Scholar]
- Reichart CG, van der Ende J, Hillegers MHJ, Wals M, Bongers IL, Nolen W, et al. Perceived parental rearing of bipolar offspring. Acta Psychiatrica Scandinavica. 2009;115:21–28. doi: 10.1111/j.1600-0447.2006.00838.x. [DOI] [PubMed] [Google Scholar]
- Reichart CG, van der Ende J, Wals M, Hillegers MH, Nolen W, Ormel J, et al. Social functioning of bipolar offspring. Journal of Affective Disorders. 2007;98:207–213. doi: 10.1016/j.jad.2006.07.018. [DOI] [PubMed] [Google Scholar]
- Shaw JA, Egeland JA, Endicott J, Allen CR, Hostetter AM. A 10-year prospective study of prodromal patterns for bipolar disorder among Amish youth. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:1104–1111. doi: 10.1097/01.chi.0000177052.26476.e5. [DOI] [PubMed] [Google Scholar]
- Sigurdsson E, Fombonne E, Sayal K, Checkley S. Neurodevelopmental antecedents of early-onset bipolar affective disorder. British Journal of Psychiatry. 1999;174:121–127. doi: 10.1192/bjp.174.2.121. [DOI] [PubMed] [Google Scholar]
- Smoller JW, Finn CT. Family, twin, and adoption studies of bipolar disorder. American Journal of Medical Genetics Part C (SeminMedGenet) 2003;123C:48–58. doi: 10.1002/ajmg.c.20013. [DOI] [PubMed] [Google Scholar]
- Turecki G, Grof P, Cavazzoni P, Duffy A, Grof E, Ahrens B, et al. Evidence for a role of phospholipase c-y1 in the pathogenesis of bipolar disorder. Molecular Psychiatry. 1998;3:534–538. doi: 10.1038/sj.mp.4000447. [DOI] [PubMed] [Google Scholar]
- Waddell C, Offord DR, Shepherd CA, Hua JM, McEwan K. Child psychiatic epidemiology and canadian public policy-making: the state of the science and the art of the possible. Canadian Journal of Psychiatry. 2002;47:825–832. doi: 10.1177/070674370204700903. [DOI] [PubMed] [Google Scholar]
- Wozniak J, Biederman J, Kiely K, Ablon JS, Faraone SV, Mundy E, et al. Mania-like symptoms suggestive of childhood-onset bipolar disorder in clinically referred children. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:867–876. doi: 10.1097/00004583-199507000-00010. [DOI] [PubMed] [Google Scholar]