Abstract
Aims: Studies have yielded conflicting results regarding alcohol's influence on HIV outcomes, particularly after highly active antiretroviral treatment (HAART). Discrepant findings may be related to confounding variables, including gender, patterns of alcohol abuse and type of alcohol beverage beyond the amount consumed. Methods: Using a cohort study, differences in HAART effectiveness after 24 weeks of therapy were compared as a function of amount and preference for alcohol, drinking only liquor (LI, n = 55) or only wine or beer (BW, n = 110). Given the critical role of thymus on HAART response, changes in thymus size, CD4s, naïve lymphocytes and viral loads were assessed. Results: After HAART, positive increases in both CD4s (+12 cell counts/mm3) and thymus size (+0.7 mm3) were evident in the BW group. In contrast, the LI subgroup exhibited a decline in both parameters (−4 CD4 cells/mm3 and −0.6 mm3 in thymus size). Women in the LI group exhibited significantly lower CD4 (163.4 ± 46.2) and naïve counts (178 ± 69.5) than LI men (CD4: 281.6 ± 203, P = 0.05; lymphocytes: 301.4 ± 198, P = 0.04). In adjusted regression models, the LI compared to the BW subgroup had greater odds of maintaining detectable viral loads (RR = 1.35, 95% CI 1.04–1.75; P = 0.03), increased thymus volumes (RR = 3.8, P = 0.04) and replenished naïve cells (RR = 13, P = 0.02). Conclusions: Liquor was associated with thymus deterioration and thus with poorer viro-immune outcomes after HAART. Subtyping participants by alcohol consumption patterns seems to be clinically relevant and needs to be accounted for in future studies.
INTRODUCTION
Immune reconstitution is a critical component of HAART recovery, and adults should be able to at least partially increase the total number of T cells lost to HIV-1 infection after controlling viremia. CD4 cell repopulation following HAART is associated with both cellular redistribution from lymph nodes and with de novo generation (Gaulton et al., 1997; Heitger et al., 1997; Nobile et al., 2004). Because the thymus is the source of new T cells, examining the thymus function during HIV infection and therapy is critical to studies of T-cell dynamics (Heitger et al., 1997; Teixeira et al., 2001; Míguez et al., 2008). The degree of CD4 cell repopulation induced by HAART, however, depends upon several host factors. Our previous studies, along with others, indicate that antiretroviral-treated patients with hazardous/heavy alcohol consumption are less likely to achieve positive virological or immunological improvements (Fabris et al., 2000; Conigliaro et al., 2003; Míguez et al., 2003; Samet et al., 2003,2007; Chander et al., 2006; Finucane et al., 2007). What is unclear is if the type of alcohol consumed has any role beyond that of the amount of alcohol used alone.
Whether different types of beverages confer dissimilar risks is also uncertain. Limited data among the general population suggest a more favorable morbidity and mortality experience for drinkers of wine or beer than that for drinkers of liquor (Grønbæk et al., 1995, 2000; Truelsen et al., 1998; Prescott et al., 1999). To the best of our knowledge, no HIV studies have reported the difference or negative association of immune or thymus responses with the type of alcohol beverage. Given the rapid growth of the HIV-infected population receiving HAART and the widespread use of alcohol (Lefevre et al., 1995; Cook et al., 2001; Shor-Posner and Miguez, 2001; Bryant, 2006), there is an urgent need to fully delineate the role of alcohol in HAART effectiveness.
Gender is another important variable that is predictive of drinking patterns and problems related to alcohol use (Míguez and Shor-Posner, 2001; Hessol et al., 2007). Evidence suggests that the problematic effects produced by both drinking and HIV vary depending on gender, but a paucity of data exists on the interactive effects of these two factors according to gender. Because the Miami Alcohol Research Cohort of HIV-infected individuals (MARCH) study includes an ethnically and gender diverse sample of participants, with substantial variation in alcohol use, we were afforded a valuable opportunity to explore the multifaceted associations among alcohol use and immune responses to HAART.
METHODS
Sampling
MARCH was a longitudinal observational study to evaluate the impact of hazardous versus non-hazardous alcohol use on the health status of HIV-infected individuals receiving HAART. HIV seropositive participants aged 18–55 years were eligible if they were starting a HAART regimen, regardless of previous exposure to antiretrovirals. The definition of HAART for analyses was guided by published guidelines (AIDSinfo, 2003; DHHS, 2004). Patients were excluded if they were non-ambulatory or if they had other underlying diseases known to be associated with cognitive or immune impairments (i.e. current or past CNS opportunistic infection, head injury, tumors, major psychiatric disease, or other immune or nutritional illness).
Participants were recruited from the University of Miami Miller School of Medicine and Jackson Memorial clinics, where they were followed at regular intervals. Those who provided written informed consent and medical release were enrolled. The Institutional Review Board at the University of Miami approved the study.
Exposure: alcohol consumption patterns
Alcohol consumption assessments included widely used standardized and validated brief screening questionnaires: the Physician's guide of the National Institute on Alcohol Abuse and Alcoholism, American Association, CAGE, AUDIT and ADS (NIAAA, 1995; Reid et al., 1999). CAGE is an acronym formed from the italicized letters in the questionnaire (cut-annoyed-guilty-eye) and it is a standardized instrument used worldwide to identify problems with alcohol (NIAAA, 1995). The World Health Organization's Alcohol Use Disorders Identification Test (AUDIT) has three questions on alcohol consumption, three questions on drinking behavior and dependence and four questions on the consequences or problems related to drinking (NIAAA, 1995). The ADS (Alcohol Dependence Scale) is a widely used research and clinical tool that provides a quantitative measure of the severity of alcohol dependence. Its 25 items cover alcohol withdrawal symptoms, impaired control over drinking, awareness of a compulsion to drink, increased tolerance to alcohol and salience of drink-seeking behavior. Studies have found the ADS to be a reliable and valid instrument (NIAAA, 1995). The combination of assessments permitted cross-validation of participants’ responses.
We assessed alcohol consumption in general and with separate items for beer, white wine, red wine, and liquor. Participants were asked to specify the number of days per week they drank, and the quantity they consumed each time. We defined standard portions as a glass, bottle or can of beer, a 4-ounce glass of wine and a shot of liquor.
Definition of alcohol groups
For the purpose of these analyses, participants were divided into two groups: those who could be reliably classified into preferring to drink only liquor (tequila, gin, vodka, scotch, rum, whiskey and liqueurs, either alone or mixed: LI) or preferring to drink only beer or wine (BW) groups. The group selection was based on several factors. (1) In the medical literature, liquor has been most frequently related to deleterious health effects. (2) On the other hand, the beneficial health effects of moderate alcohol consumption have been attributed to the antioxidants and phenols contained in beers and wines. (3) In our research experience, beer and wine drinkers consume a greater variety of alcohol beverages and are more likely to be binge drinkers. Liquor drinkers mostly prefer liquors, and many of them are heavy drinkers. (4) Recently, liquor consumption has been an increasing problem among young Americans (Roeber et al., 2007). Thus, from a public health point of view, our findings may be highly relevant to exploring these new trends.
Outcome variables
The main study outcomes are the three laboratory tests and the radiological procedure most related to HAART response: thymus volumes, viral load, CD4 and naïve cells (counts and percentages). The HIV viral burden was quantified using the Amplicor HIV monitor test (Roche Diagnostic System). The lower threshold for detection at the time of the study was 400 copies/ml. The percentage and absolute numbers of T lymphocyte subpopulations CD3+/CD4+ and CD3+/CD8+ cell counts were determined by flow cytometry per National Institute of Allergy and Infectious Diseases laboratory protocols. The thymus size and naïve cells (CD45RA+CD62L+) were examined as complementary measures of immune reconstitution, which may better reflect HAART response (Giorgi et al., 1990). Magnetic resonance (MR) imaging without contrast was used to determine the thymus volume. The MRI was performed using a thoracic surface coil and electrocardiographic gating, and consisted of the following sequences: (1) sagittal and coronal pilots; (2) T1-weighted in-phase axial, slice thickness 6mm, interslice gap 1 mm, four averages; (3) T1-weighted opposed-phase axial, slice thickness 6 mm, interslice gap 1 mm, four averages; and (4) T2-weighted fast spin echo axial fat-suppressed, slice thickness 6 mm, interslice gap 1 mm, four averages. The thymic volume was calculated using a quantitative method to evaluate the true glandular composition of the thymus, correcting for the degree of fatty infiltration. Quantitative calculation of the thymic volume was performed on T1-weighted in-phase axial slices by multiplying the prevascular mediastinal area on each slice by a correction factor, using fat and muscle signal intensities (SI) to estimate the range of percent glandular composition of the thymus (0–100%):
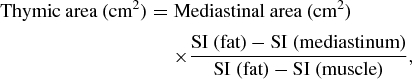 |
where SI (mediastinum) = mean mediastinal signal intensity, SI (fat) = maximal pixel value of mediastinal fat, and SI(muscle) = pectoralis muscle signal intensity. The areas were then summed and multiplied by the 7 mm geometric factor to obtain the thymic volume.
Control variables
At baseline, a series of structured comprehensive assessments on sociodemographic characteristics, health history, alcohol and drug use, medication and adherence were completed. Research assessments were followed by a brief physical examination and phlebotomy. AIDS-defining Centers for Disease Control and Prevention (CDC) criteria were used to establish the HIV disease status. Anthropometrics and dietary intake were obtained using standard procedures. Adherence was calculated using both pharmacy records and the standardized ACTG antiretroviral adherence questionnaire (Chesney et al., 2000). This questionnaire assesses both weekday and weekend activities to capture consistent and inconsistent patterns of missing doses.
A follow-up visit was scheduled semiannually and included repeat assessments, physical examinations and laboratory tests. After completing the visit, the medical chart and pharmacy records were abstracted, and patient information was validated.
Statistical analyses
The data were analyzed using SPSS 15.0 for Windows (Statistical Package for the Social Sciences, Chicago, IL, USA) and P values <0.05 were considered to be statistically significant. Subsequent to descriptive statistical analyses, the mean variables were compared using Student's t-test and one-way analysis of variance (ANOVA) procedures to determine the covariates for inclusion in the univariate analyses and in the multivariate model (e.g. age, race/ethnicity, education level, stress and depression). Fisher's exact tests were used when appropriate.
Univariate analyses were used to calculate odds ratios (OR) and 95% confidence intervals (CI). In consideration of the potential confounding effect of heavy drinking, our outcome variables were adjusted by total amounts of alcohol consumed. Outcomes and observed covariates that were significantly associated with HAART responses (P < 0.05) in univariate analysis were then included in a multivariable model. In addition, potential patient predictors, such as gender, race/ethnicity, CDC status, drug use and body mass index (BMI), were selected, based on findings in the HIV literature, and were added to the model (Egger et al. 2002). Non-significant variables (P ≥ 0.05) were removed, beginning with the least significant, until the final full model was determined. Model statistics included adjusted OR, 95% CI and their corresponding P values. Analyses were restricted only to those whose alcohol consumption did not significantly change from baseline to final evaluation (approximately one-half drink per day).
RESULTS
Study population characteristics
As discernible in Table 1, groups were comparable on dietary intake, anthropometrics, CD4 counts, tobacco use and sociodemographic variables with the following exceptions: liquor drinkers were younger and less likely to be Hispanics (OR = 0.34, 95% CI: 0.13–0.84). Despite similar CDC stage and CD4 cell counts, a higher viral burden was also observed at baseline in the LI group (279,750 ± 48,964/4.5 ± 1.3 log10 versus 149,675 ± 25,977/3.9 ± 1.5 log10 equivalent copies per milliliter, P = 0.01) compared to the BW group. Finally, liquor drinkers were more likely to report more drinks per occasion or episode than wine/beer users.
Table 1.
Study group characteristics
| LI group | BW group | ||
|---|---|---|---|
| Variables | (n = 55) | (n = 110) | P value |
| Age at start of regimen | 38.5 ± 7 | 41.5 ± 7 | 0.02 |
| Gender | |||
| Men | 36 (65%) | 77 (70%) | 0.4 |
| Women | 19 (35%) | 33 (30%) | |
| Race/ethnicity | |||
| African Americans | 36 (67%) | 61 (56%) | 0.009 |
| Hispanics | 9 (16%) | 39 (35%) | |
| Caucasians | 8 (14%) | 9 (8%) | |
| Other | 2 (3%) | 1 (1%) | |
| Years drinking | |||
| Alcohol users | 13 ± 8.9 | 11.4 ± 9.4 | 0.05 |
| Number of days/week drinking | 4 ± 2.2 | 3.2 ± 2.7 | 0.1 |
| Number of drinks in one single | 8 ± 7 | 5 ± 4 | 0.01 |
| occasion | |||
| Cigarette smoking | 43 (79%) | 77 (70%) | 0.2 |
| Body mass index | 27.4 ± 7.5 | 26.5 ± 6.1 | 0.4 |
| CD4 cell counts | 237 ± 187 | 252 ± 173 | 0.6 |
Values are either numbers, with the corresponding percentages on parenthesis, or means ± SD.
Baseline alcohol and immune parameters
No significant correlation was observed between age and thymus volume, at both baseline and at the 24-week visit. Table 2 displays the baseline immune profiles of the two alcohol groups, including P values from comparison tests. The LI group had significantly fewer naïve CD4+ lymphocytes compared to the BW group. Even though not reaching statistical significance, the LI group also exhibited a smaller thymus (6.8 ± 4.5 versus 8.8 ± 5.1 cm3).
Table 2.
Baseline immune parameters by alcohol groups
| LI group | BW group | ||
|---|---|---|---|
| (n = 55) | (n = 110) | ||
| Variables | Mean ± SD | Mean ± SD | P value |
| CD3 percentages | 74.6 ± 9.2 | 78.0 ± 9.6 | 0.04 |
| CD4 percentages | 13 ± 10 | 14 ± 8.3 | 0.6 |
| CD8 percentages | 57.2 ± 11.6 | 60.2 ± 10.5 | 0.1 |
| CD3CD45RA+CD62L+ | 16.2 ± 13 | 23 ± 15 | 0.004 |
| percentages naïve | |||
| Thymus volume (cm3) | 6.8 ± 4.5 | 8.8 ± 5.1 | 0.08 |
Values are means ± SD.
Additional analyses revealed that women in the LI group had half the thymus size, when compared to any other group. As illustrated in Table 3, women in the LI group also exhibited significantly lower CD4 counts (163.4 ± 46.2) and naïve lymphocyte cell counts (CD3+CD45+CD62+: 178 ± 69.5) than those in LI men (CD4: 281.6 ± 203, P = 0.05; lymphocytes: 301.4 ± 198, P = 0.04) and BW women. In contrast, among the beer and wine drinkers, women tended to exhibit higher CD4 cell counts than their male counterparts (women CD4: 264.6 ± 151 versus 239 ± 182, P = 0.09). Although no significant gender differences in viral loads were observed, women in the LI group exhibited the highest viremia.
Table 3.
Baseline immune and virological status by both alcohol and gender groups
| Variables | P value | Men LI group | Women LI group | P value | Women BW group | Men BW group | P value |
|---|---|---|---|---|---|---|---|
| CD4 cell counts/mm3 | 0.05 | 281.6 ± 203 | 163.4 ± 46.2 | 0.03 | 264.6 ± 151 | 239 ± 182 | 0.09 |
| Thymus (cm3) | 0.09 | 9.9 ± 4 | 4.8 ± 1.8 | 0.1 | 8.2 ± 1.2 | 9.3 ± 1.3 | 0.5 |
| HIV viral load copies/mL | 0.6 | 262,159 ± 58,958 | 316,104 ± 89,993 | 0.05 | 143,383 ± 41,527 | 155,030 ± 33,581 | 0.8 |
Values are means ± SD.
After 24 weeks on HAART
As a continuous outcome, the adjusted percent adherence difference between the two groups was only 3%. Accordingly, both alcohol groups exhibited a significant improvement in HIV viral control at 24 weeks (BW: P = 0.05 versus LI: P = 0.04). Although liquor users experienced a greater drop in mean viral loads than did BW users (141,953 ± 52,329 versus BW = −81,752 ± 25,360 RNA copies, respectively), the LI compared to the BW subgroup had greater odds of maintaining detectable viral loads (RR = 1.35, 95% CI: 1.04–1.75; P = 0.03). The thymus volume significantly increased after 24 weeks of HAART, and increases correlated with the total number of CD4 cells (r2 = 0.7, P = 0.0001) and naïve CD4+ cell counts (r2 = 0.4, P = 0.007), but not with viral loads.
Despite similar adherence and achieving statistically significant reductions in viral loads, immune responses were dissimilar (see Table 4). A positive increase in both CD4 cell counts (from the pre-HAART values + 12 cell counts/mm3) and thymus size (+0.7 cm3) was evident in the BW group. In contrast, the LI subgroup showed a decline in both parameters (−4 CD4 cells/mm3 and −0.6 cm3 in thymus size). After controlling for alcohol amounts, 50% of the BW group, but only 10% of the LI group, obtained an increase in CD4+ counts ≥50 cells/mm3 after HAART initiation (P = 0.04). Over the entire follow-up period, 10% of the BW users and none of the LI users (n = 8) obtained an increase in CD4+ cell count ≥200 cells/mm3 after HAART initiation (p = 0.03). Moreover, liquor drinkers accounted for a significant proportion (65%) of those who exhibited discordant responses (no CD4 increases with viral suppression) after 6 months of HAART (P = 0.05).
Table 4.
Immunological and virological responses after 24 weeks of HAART by the alcohol group
| Variable | Liquor group | Beer/wine group | P value |
|---|---|---|---|
| Viral load | −141,953 ± 52,329 | −81,752 ± 25,360 | 0.03 |
| Change in CD4 cell counts | −4 cells | +12 cells | 0.001 |
| 200 CD4 cells/mm3 after HAART | 0% | 10% | 0.01 |
| 50 CD4 cells/mm3 after HAART | 10% | 50% | 0.04 |
| Thymus volumes in cm3 | −0.6 | +0.7 | 0.05 |
Values are means ± SD or percentages.
Regression analyses
Thymus size increase
In fully adjusted models (sociodemographics, baseline CDC stage, total alcohol consumption, drug use and adherence), the liquor subgroup (RR = 3.8; 95% CI: 1.0–7.4, P < 0.04) and platelet counts (RR = 0.24, 95% CI: 0.04–0.33, P < 0.03), but not hemoglobin, were significant predictors of the thymus size increase. In terms of immune responses, cell replenishment (>50 cells/mm3) was lower in liquor users.
Increased production of naïve cells
After adjustment for confounding variables, the associated adjusted ratios were 0.4 (95% CI: 0.19–0.90, P = 0.01) for the liquor subgroup, 12.8 (95% CI: 2.3–23.3, P = 0.02) for undetectable viral loads and −0.24 (0.1–0.5, P = 0.0001) for baseline CD4 cell counts below 200.
Risks associated with liquor use were unaffected by hazardous drinking and not significantly by heavy use, suggesting that the observed effects need to be attributed to liquor components, rather than doses.
DISCUSSION
A balanced view of alcohol drinking and health should consider the amount of alcohol, beverage choice, drinking patterns and gender disparities. However, few studies with the general population (Grønbæk et al., 1995, 2000; Truelsen et al., 1998; Prescott et al., 1999) and none with HIV-infected populations have examined these aspects until now. One major finding in our data of HAART initiators was the highest risk associated with liquor use on each of the main outcome variables. Furthermore, previously published studies have demonstrated that an increase of at least 50 CD4+ cell counts immediately after HAART initiation is associated with a markedly improved prognosis (Jacobson et al., 2002). Liquor users, however, were less likely to attain this response. From a clinical perspective, these findings have two important implications. First, by providing a biological explanation, our findings challenge previous alcohol studies attributing HAART differences mainly to poor adherence, which was carefully controlled in this study. Secondly, it indicates the need for health-care providers to be vigilant regarding alcohol use, particularly liquor use.
Because CD4 recovery may be associated with CD4 redistribution/peripheral expansion, increased thymus production (naïve cells) or both, it was important to undertake a detailed evaluation of each parameter (Gaulton et al., 1997; Heitger et al., 1997; Teixeira et al., 2001; Nobile et al., 2004). From a clinical and immunological perspective, the generation of naïve T cells is of greatest relevance because they are more effective in responding to neoantigens (Heitger et al., 1997; Douek et al., 2000; Teixeira et al., 2001). In this regard, findings from this cohort indicate that the thymus size increase and replenishment of cells were constrained by alcohol use, particularly by liquor consumption. Similarly, animal studies have demonstrated that alcohol decreases the cellularity of the thymus by inducing apoptotic changes, impairing mitochondrial function and decreasing the total glutathione concentration in the thymocytes (Monahan et al., 1997; Wang and Spitzer, 1997; Starkenburg et al., 2001; Pruett et al., 2003). However, alcohol impact was also evident over memory T cells indicating that additional mechanisms were impairing the immune system of drinkers.
While it is unclear why liquor is riskier than wine and beer, several potential mechanisms can be postulated. First, our results indicate that liquor users exhibited higher viral loads, and their viremia was less well controlled with treatment. This is consistent with the literature showing that virus replication in alcohol-dependent animals is significantly higher compared to controls and probably associated with the increased NF-κB activity (Dong et al., 2000; Wang et al., 2002). It could be hypothesized that animal findings, which utilize pure ethanol, are probably comparable to those of liquor.
Differences may also be attributed to their concentration of antioxidants, since antioxidants have been associated with increased proliferative responses, reduced lymphocyte apoptosis and viral replication (Roederer et al., 1990; Raju et al., 1994; Cayota et al., 1996; Kotler, 1998). Wine and beer possess high levels of vitamins and phytochemicals, and liquors are notably absent of them. Thus, the wine and beer containing antioxidants may lessen the deleterious effects of alcohol on total circulating CD4+ cells in patients on HAART (Cayota et al., 1996).
Besides, it is also possible that some trait(s) influencing a liquor preference may predispose an unhealthy lifestyle; however, we could not identify any additional risk factor. Tobacco smoking was similar between the groups. Thus, the mechanisms of the deleterious effects of liquor warrant further investigation.
A paucity of data exists regarding the impact of gender on the co-morbidity of HIV and alcohol. Moreover, the results concerning the gender effect on the immunovirological response to HAART have been mixed (Nicastri et al., 2007). However, most authors, after adjustment for potential confounders, do not report any difference in terms of these outcomes. We could have arrived at a similar conclusion if data had not been analyzed by alcohol types. Liquor and wine/beer had opposing effects, while women who consumed non-hazardous amounts of wine/beer had consistently better responses than their male drinking counterparts, and hazardous female drinkers of liquor performed poorer than hazardous and non-hazardous liquor-drinking males. Poorer responses parallel thymus volumes, suggesting an increased susceptibility to thymus damage caused by liquor consumption among women. However, the exact mechanism needs to be established in future studies.
We are aware that our observed significant effects may seem small. However, the context of change is important to be considered, namely, the early recuperation of lymphocyte counts and production of naïve cells are also small in order. Moreover, the changes we observed were mostly in opposite directions, adding further credence to the relevance of our findings for future research.
The current analysis of alcohol's impact on the health of HIV-infected individuals adds to the literature in several ways. First, to our knowledge, this is the first cohort study of HAART initiators that considers both the volume and pattern of consumption, as they relate to HAART response. Secondly, we included measurements of recent T-cell outputs and other clinically relevant outcome measurements (i.e. cognition and immune function). Third, contrary to most prior studies, our analysis of alcohol was in a longitudinal design with an ethnically diverse population and included a sizeable proportion of women. Fourth, the study design permitted us to examine the clinical trajectory of study subjects over time, and thus to delineate the role of adherence and other factors that might confound the biological effect of alcohol use on HAART effectiveness. Finally, we were able to avoid the confounding effects of individuals in therapy at diverse times, with all our participants initiating treatment. At present, alcohol studies that elucidate causal factors are needed to help inform public health authorities and health care providers.
Acknowledgments
The authors thank Rhonda Rosenberg for critical reading of the manuscript and for expert editorial assistance. The study was funded by the NIAAA of the United States (5R21AA13793-3 and 3R01AA017405-02S1 M.J.M.).
References
- AIDSinfo: A service of US Department of Health and Human Services Overview of guidelines. 2003. Available at http://www.aidsinfo.nih.gov/guidelines . (16 May 2003, date last accessed)
- Bryant KJ. Expanding research on the role of alcohol consumption and related risks in the prevention and treatment of HIV/AIDS. Subst Use Misuse. 2006;41::1465–1507. doi: 10.1080/10826080600846250. [DOI] [PubMed] [Google Scholar]
- Cayota A, Vuillier F, Gonzalez G, et al. In vitro antioxidant treatment recovers proliferative responses of anergic CD4+ lymphocytes from human immunodeficiency virus-infected individuals. Blood. 1996;87:4746–53. [PubMed] [Google Scholar]
- Chander G, Lau B, Moore RD. Hazardous alcohol use: a risk factor for non-adherence and lack of suppression in HIV infection. J Acquir Immune Defic Syndr. 2006;43:411–7. doi: 10.1097/01.qai.0000243121.44659.a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chesney MA, Ickovics JR, Chambers DB, et al. Patient Care Committee & Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG) Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: the AACTG adherence instruments. AIDS Care. 2000;12::255–66. doi: 10.1080/09540120050042891. [DOI] [PubMed] [Google Scholar]
- Conigliaro J, Gordon AJ, McGinnis KA, et al. How harmful is hazardous alcohol use and abuse in HIV infection: Do health care providers know who is at risk? J Acquir Immune Defic Syndr. 2003;33:521–5. doi: 10.1097/00126334-200308010-00014. [DOI] [PubMed] [Google Scholar]
- Cook RL, Sereika SM, Hunt SC, et al. Problem drinking and medication adherence among persons with HIV infection. J Gen Intern Med. 2001;16:83–6. doi: 10.1111/j.1525-1497.2001.00122.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DHHS/Henry J. Kaiser Family Foundation Panel on Clinical Practices for the Treatment of HIV infection Guidelines for the use of antiretroviral agents in HIV-infected adults and adolescents. October 2004 revision. Available at http://aidsinfo.nih.gov/guidelines/adult/AA_040705.pdf .
- Dong Q, Kelkar S, Xiao Y, et al. Ethanol enhances TNF-alpha-inducible NFkappaB activation and HIV-1-LTR transcription in CD4+ Jurkat T lymphocytes. J Lab Clin Med. 2000;136:333–43. doi: 10.1067/mlc.2000.110104. [DOI] [PubMed] [Google Scholar]
- Douek DC, Vescio RA, Betts MR, et al. Assessment of thymic output in adults after haematopoietic stem-cell transplantation and prediction of T-cell reconstitution. Lancet. 2000;355:1875–81. doi: 10.1016/S0140-6736(00)02293-5. [DOI] [PubMed] [Google Scholar]
- Egger M, May M, Chene G, et al. Prognosis of HIV-1-infected patients starting highly active antiretroviral therapy: a collaborative analysis of prospective studies. Lancet. 2002;360:119–29. doi: 10.1016/s0140-6736(02)09411-4. [DOI] [PubMed] [Google Scholar]
- Fabris P, Tositti G, Manfrin V, et al. Does alcohol intake affect highly active antiretroviral therapy (HAART) response in HIV-positive patients? J Acquir Immune Defic Syndr. 2000;25:92–3. doi: 10.1097/00042560-200009010-00013. [DOI] [PubMed] [Google Scholar]
- Finucane MM, Samet JH, Horton NJ. Translational methods in biostatics: linear mixed effects regression models of alcohol consumption and HIV disease progression over time. Epidemiol Perspect Innov. 2007;4:8. doi: 10.1186/1742-5573-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaulton GN, Scobie JV, Rosenzweig M. HIV-1 and the thymus. AIDS. 1997;11:403–14. doi: 10.1097/00002030-199704000-00002. [DOI] [PubMed] [Google Scholar]
- Giorgi JV, Cheng HL, Margolick JB, et al. Quality control in the flow cytometric measurement of T-lymphocyte subsets. Clin Immunol Immunopathol. 1990;55:173–86. doi: 10.1016/0090-1229(90)90096-9. [DOI] [PubMed] [Google Scholar]
- Grønbæk M, Becker U, Johansen D, et al. Type of alcohol consumed and mortality from all causes, coronary heart disease, and cancer. Ann Intern Med. 2000;133:411–19. doi: 10.7326/0003-4819-133-6-200009190-00008. [DOI] [PubMed] [Google Scholar]
- Grønbæk M, Deis A, Sørensen TI, et al. Mortality associated with moderate intakes of wine, beer or spirits. BMJ. 1995;310:1165–9. doi: 10.1136/bmj.310.6988.1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heitger A, Neu N, Kern H, et al. Essential role of the thymus to reconstitute naive (CD45RA+) T-helper cells after human allogeneic bone marrow transplantation. Blood. 1997;90:850–7. [PubMed] [Google Scholar]
- Hessol NA, Kalinowski A, Benning L, et al. Mortality among participants in the Multicenter AIDS Cohort Study and the Women's Interagency HIV Study. Clin Infect Dis. 2007;44:287–94. doi: 10.1086/510488. [DOI] [PubMed] [Google Scholar]
- Jacobson LP, Li R, Phair J, et al. Evaluation of the effectiveness of highly active antiretroviral therapy in persons with human immunodeficiency virus using biomarker-based equivalence of disease progression. Am J Epidemiol. 2002;155:760–70. doi: 10.1093/aje/155.8.760. [DOI] [PubMed] [Google Scholar]
- Kotler DP. Antioxidant therapy and HIV infection. Am J Clin Nutr. 1998;67:7–9. doi: 10.1093/ajcn/67.1.7. [DOI] [PubMed] [Google Scholar]
- Lefevre F, O’Leary B, Moran M, et al. Alcohol consumption among HIV-infected patients. J Gen Intern Med. 1995;10:458–60. doi: 10.1007/BF02599920. [DOI] [PubMed] [Google Scholar]
- Míguez MJ, Lewis JE, Moreno J, et al. Cognitive performance and the thymus among HIV infected subjects receiving HAART. J Biologics: Targets Ther. 2008;2:321–7. doi: 10.2147/btt.s1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Míguez MJ, Shor-Posner G. Alcohol use and HIV infection in the HAART era. Am Clin Lab, HIV Forum. 2001;20:20–3. [PubMed] [Google Scholar]
- Míguez MJ, Shor-Posner G, Morales G, et al. HIV treatment in drug abusers: impact of alcohol use. Addict Biol. 2003;8:33–7. doi: 10.1080/1355621031000069855. [DOI] [PubMed] [Google Scholar]
- Monahan CM, Padgett EL, Biber KL, et al. Dose response to ethanol-containing liquid diets for use in a murine model for studies of biological effects due to ethanol consumption. Alcohol Clin Exp Res. 1997;21:1092–9. [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism . Washington, DC: Government Printing Office; 1995. The Physicians’ Guide to Helping Patients with Alcohol Problems. Publication NIH 95, 3769. [Google Scholar]
- Nicastri E, Leone S, Angeletti C, et al. Sex issues in HIV-1-infected persons during highly active antiretroviral therapy: a systematic review. J Antimicrob Chemother. 2007;60:724–32. doi: 10.1093/jac/dkm302. [DOI] [PubMed] [Google Scholar]
- Nobile M, Correa R, Borghans JA, et al. De novo T-cell generation in patients at different ages and stages of HIV-1 disease. Blood. 2004;104:470–7. doi: 10.1182/blood-2003-12-4265. [DOI] [PubMed] [Google Scholar]
- Prescott E, Grønbæk M, Becker U, et al. Alcohol intake and the risk of lung cancer: influence of type of alcoholic beverage. Am J Epidemiol. 1999;149:463–70. doi: 10.1093/oxfordjournals.aje.a009834. [DOI] [PubMed] [Google Scholar]
- Pruett SB, Fan R, Zheng Q, et al. Modeling and predicting immunological effects of chemical stressors: characterization of a quantitative biomarker for immunological changes caused by atrazine and ethanol. Toxicol Sci. 2003;75:343–54. doi: 10.1093/toxsci/kfg200. [DOI] [PubMed] [Google Scholar]
- Raju PA, Herzenberg L, Roedered M. Glutathione precursor and antioxidant activities of N-acetylcysteine and oxothaizolidine carboxylate compared in vitro studies of HIV replication. AIDS Res Hum Retroviruses. 1994;10:961–7. doi: 10.1089/aid.1994.10.961. [DOI] [PubMed] [Google Scholar]
- Reid M, Carrington Fiellin DA, O’Connor P. Hazardous and harmful alcohol consumption in primary care. Arch Intern Med. 1999;159:1681–9. doi: 10.1001/archinte.159.15.1681. [DOI] [PubMed] [Google Scholar]
- Roeber J, Green DL, Meurer KM, et al. Types of alcoholic beverages usually consumed by students in 9th–12th grades—four states, 2005. Morb Mortal Wkly Rep. 2007;56:737–40. [PubMed] [Google Scholar]
- Roederer M, Staal FJT, Raju PA, et al. Cytokine-stimulated human immunodeficiency virus replication is inhibited by N-acetyl-l-cysteine. Proc Natl Acad Sci USA. 1990;87:4884–8. doi: 10.1073/pnas.87.12.4884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samet JH, Cheng DM, Libman H, et al. Alcohol consumption and HIV disease progression. J Acquir Immune Defic Syndr. 2007;46:194–9. doi: 10.1097/QAI.0b013e318142aabb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samet JH, Horton NJ, Traphagen ET, et al. Alcohol consumption and HIV disease progression: are they related? Alcohol Clin Exp Res. 2003;27:862–7. doi: 10.1097/01.ALC.0000065438.80967.56. [DOI] [PubMed] [Google Scholar]
- Shor-Posner G, Miguez MJ. Heavy alcohol use hinders HIV therapy: study. AIDS Alert. 2001;16:88–90. [PubMed] [Google Scholar]
- Starkenburg S, Munroe ME, Waltenbaugh C. Early alteration in leukocyte populations and Th1/Th2 function in ethanol-consuming mice. Alcohol Clin Exp Res. 2001;25:1221–30. [PubMed] [Google Scholar]
- Teixeira L, Valdez H, McCune JM, et al. Poor CD4 T cell restoration after suppression of HIV-1 replication may reflect lower thymic function. AIDS. 2001;15:1749–56. doi: 10.1097/00002030-200109280-00002. [DOI] [PubMed] [Google Scholar]
- Truelsen T, Grønbæk M, Schnohr P, et al. Intake of beer, wine, and spirits and risk of stroke: the Copenhagen City Heart Study. Stroke. 1998;29:2467–72. doi: 10.1161/01.str.29.12.2467. [DOI] [PubMed] [Google Scholar]
- Wang X, Douglas SD, Metzger DS, et al. Alcohol potentiates HIV-1 infection of human blood mononuclear phagocytes. Alcohol Clin Exp Res. 2002;26:1880–6. doi: 10.1097/01.ALC.0000042148.50808.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Spitzer J. Alcohol-induced thymocyte apoptosis is accompanied by impaired mitochondrial function. Alcohol. 1997;14:99–105. doi: 10.1016/s0741-8329(97)86148-4. [DOI] [PubMed] [Google Scholar]


