Abstract
In Korea, Clonorchis sinensis infection is still highly prevalent because case detection in the field is difficult and the detected cases used to be incompletely cured due to treatment failure. The present study tried to control clonorchiasis in an endemic village by repeated treatments with praziquantel every 6 months and to evaluate sonography as a diagnostic measure. By stool examinations, the egg positive rate in the endemic village was 22.7%, but it decreased to 19.6% at 6 months, 15.1% at 12 months. 12.2% at 18 months, 6.3% at 24 months, 11.4% at 30 months, and 6.3% at 42 months after the beginning of repeated praziquantel administration. The sonography showed 61 (49.6%) positive cases of 123 screened residents: among egg-positives the sonography positive rate was 52.2% and among egg-negatives it was still 49%. The rate among cured cases was 64.3% after 6 months, 50.0% after 12 months, 50.0% after 18 months, and 66.7% after 24 months. In a non-endemic village, 64 residents were found egg-negative by fecal examination, but 20 (31.3%) of them were positive by sonography. The present findings indicate that control of clonorchiasis in an endemic village by repeated praziquantel treatment for 42 months is still insufficient and sonography is of little value for diagnosis of clonorchiasis.
Keywords: Clonorchis sinensis, fecal examination, sonography, repeated praziquantel treatment
INTRODUCTION
Clonorchis sinensis is known to be prevalent in China, East Russia, Korea, Taiwan, and Vietnam, and it is estimated that about 15 million people are infected (Rim, 1986; Li et al., 1997). According to national surveys, the overall egg-positive rate of C. sinensis in Korea was 4.6% in 1971, 1.8% in 1976, 2.6% in 1981, 2.7% in 1986, 2.2% in 1992, and 1.4% in 1997 (Ministry of Health and Welfare, 1997). Despite the fact that treatment of positive cases has been free of charge, clonorchiasis is still prevalent along rivers throughout the country. The sixth national survey revealed that in 1997 there were at least 626,000 cases of clonorchiasis in Korea and that this disease is the country's most prevalent parasitic infection (Ministry of Health and Welfare, 1997).
During infection by the fluke, the bile duct is severely dilated and the ductal wall is thickened due to mucosal hyperplasia and periductal fibrosis (Lee et al., 1978; Chen et al., 1994). As the infection becomes chronic and the number of infected fluke increases, pathological changes in the duct become worse and in certain occasions complications develop (Rim, 1990; Chen et al., 1994). Especially widening of the duct and thickening of the wall, which can be visualized by sonography, are known to be partially irreversible (Lee et al., 1987).
For the control of clonorchiasis, diagnosis is important, and for this, fecal examination is the preferred standard method. Other supplementary diagnostic methods have been applied, including intradermal test, ELISA, immunoblotting, sonography, CT scan, and cholangiography (Lim et al., 1989; Rim, 1990; Chen et al., 1994), but all have their limitations with regard to sensitivity, specificity, or applicability. None surpasses fecal examination, so this is the most commonly used method. In the field, however, fecal examination is becoming more and more difficult since people are tending to cooperate less. At present, clonorchiasis is incidentally diagnosed during sonographic scanning of the abdomen for routine check or for other purposes. Sonographic picture of diffuse dilatation of the small intrahepatic bile ducts with no or minimal dilatation of the large intrahepatic and extrahepatic bile ducts is regarded as the pathognomonic finding of clonorchiasis (Lim et al., 1989; Hong et al., 1994). In diagnosis of clonorchiasis, however, the sensitivity and specificity of sonography have not yet been accurately determined.
It is expected that continuous and repeated treatment should be excellent for mass control of clonorchiasis but no data have proven it. In the present study, we tried to control clonorchiasis by repeated praziquantel treatment with 6 months interval and to evaluate the efficacy of sonography for diagnosis of clonorchiasis in the field before and after treatment.
MATERIALS AND METHODS
Areas chosen for the study
A village in Koesan-gun, Chungchongbuk-do was chosen as an endemic focus of clonorchiasis. For comparison, a village in Pyongchang-gun, Kangwon-do, was chosen as a non-endemic focus. The study ran from July 1994 to January 1998. Residents of the Koesan-gun village underwent fecal examination and sonography every six months, and egg positive cases were treated with praziquantel (Distocide®, Shinpoong Pharmaceutical Co., Korea) 25 mg/kg, three times in a day.
Fecal examination
One specimen of feces was collected from the residents of the villages and examined once by cellophane thick smear (CTS) technique. To roughly estimate the intensity of infection, the number of C. sinensis eggs on a smear was counted. Residents of the endemic village were reexamined randomly every six months.
Sonography
A sonography scanner (Logic 500, GE, Milwaukee, USA) was rented from the Samsung GE Medical System, Seoul, Korea and set up in the villages. The subjected residents were scanned with a 3.5 MHz transducer by an experienced radiologist. As previously mentioned (Lim et al., 1989; Hong et al., 1994), visualization of the intrahepatic bile duct was regarded as positive. The sonography was done every 6 months at the 2 villages and some of treated cases were re-examined.
RESULTS
Fecal examination and egg-positive rate during the follow-up period
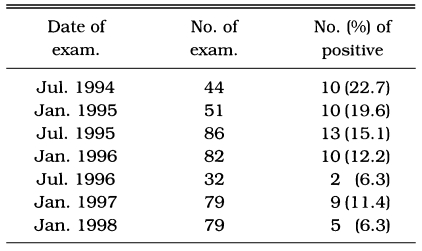
In July 1994, at the beginning of the study, the positive rate of C. sinensis eggs in the endemic village in Koesan-gun was 22.7%. All of the detected egg positive cases were treated with praziquantel and also educated for clonorchiasis. All of the residents in the village were subjected for fecal examination repeatedly every six months but actually some of them were randomly missed. The egg positive rate decreased to 19.6% in January 1995, 15.1% in July 1995, 12.2% in January 1996, 6.3% in July 1996, 11.4% in January 1997, and 6.3% in January 1998 (Table 1). In all of the positive cases, EPG (number of eggs per gram of feces) counted as less than 200. In the non-endemic village in Pyongchang-gun, 64 subjects were examined but none was positive for C. sinensis eggs (Table 2).
Table 1.
Egg positive rates during selective chemotherapy every six months in an endemic village in Koesan-gun, Korea
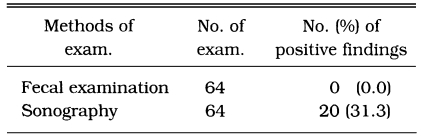
Table 2.
Findings of fecal examination and sonography for diagnosis of clonorchiasis in a non-endemic village in Pyongchang-gun, Korea
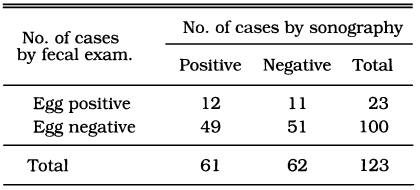
Sonography
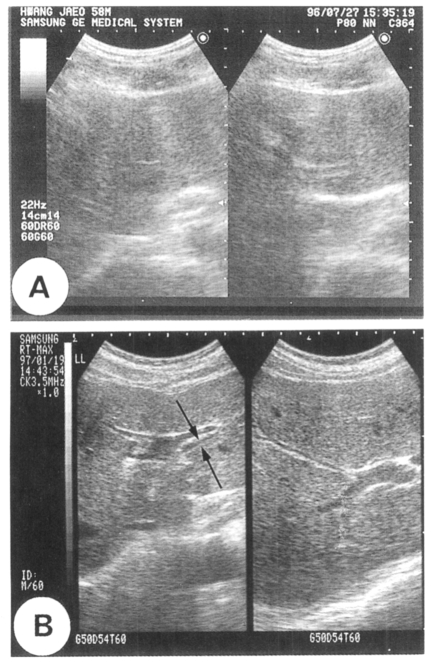
As presented in Figure 1, the sonography which showed the peripheral intrahepatic ducts was regarded as positive. On this basis, 61 (49.6%) of 123 residents, who were included more than once by both fecal examination and sonography in Koesan-gun village, were sonography-positive. Of the 123 residents, 23 were egg-positive and 100 were egg-negative. Twelve of 23 egg-positive cases (sensitivity, 52.2%) were sonography-positive and 51 of 100 egg-negative cases (specificity, 51%) were sonography-negative (Table 3).
Fig. 1.
Sonographic images of the liver. A. A normal resident with negative findings. B. An infected resident showing the intrahepatic bile duct (arrows).
Table 3.
Number of clonorchiasis cases by fecal examination and sonography in an endemic village in Koesan-gun
In the non-endemic village in Pyongchang-gun, 20 of 64 subjects examined (31.3%) were sonography-positive (Table 2). This result of false-positive sonography reflects the frequency of non-specific visualization of intrahepatic bile ducts in a rural area of Korea.
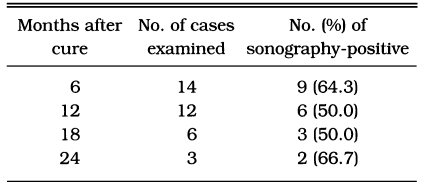
Table 4 shows changes in sonographic findings among cured clonorchiasis subjects by treatment. After 6 months of cure, nine of 14 (64.3%) were positive; half were still positive after 12 or 18 months, and two-thirds were positive after 24 months. Twenty of 35 subjects (57.1%) remained sonography-positive after being cured by praziquantel.
Table 4.
Number of clonorchiasis cases found by sonography among egg-negative converters in an endemic village in Koesan-gun
DISCUSSION
Since freshwater fish is the vehicle of human infection, endemic areas of clonorchiasis are scattered along rivers or reservoirs throughout the country. In Korea, the endemic areas are found along the middle or lower reaches of major rivers but the disease is rare in the upper reaches, where the snail intermediate host of C. sinensis is absent (Seo et al., 1981). The endemic focus of the present study, a village in Koesan-gun, is in the middle reaches of the Hangang (River) and the non-endemic focus, a village in Pyongchang-gun, is in the upper reaches of this same river. In Koesangun, the egg positive rate was initially 22.7% and at the end of the follow-up period was 6.3%, which is still far higher than 1.4% recorded for the whole country in 1997 (Ministry of Health and Welfare, 1997). Even though the intensity of infection was less than EPG 200, the present result is unsatisfactory and this control method is inefficient. This may be because such field work is labor intensive, and residents involved in the study are extremely reluctant to change their eating habits. Due to this habit, most of those who have been cured are reinfected and this is mainly why the control of clonorchiasis in Korea is inefficient. In addition, treatment failure due to incomplete or inadequate administration of praziquantel may partly be involved in this low efficiency.
Detectability of C. sinensis eggs by fecal examination of one CTS smear was shown by Chai et al. (1982) to be 44.7%, though this detection rate differs according to the intensity of infection of the subjects involved. If the intensity is low, the detection rate is substantially reduced. Because of the introduction of praziquantel, most clonorchiasis cases in Korea now involve light infection, and diagnosis can thus be problematic (Ministry of Health and Welfare, 1997). In the present study, all egg positive cases in the endemic village were lightly infected, and this should be borne in mind. In the lightly infected group, the sensitivity of ELISA diagnosis is also known to be low (Hong, 1988).
Lim et al. (1989) recorded that the diagnosis of clonorchiasis by sonography was efficient by verifying diffuse dilatation of the intrahepatic bile ducts or thickening of the ductal wall during abdominal sonographic scanning. In the present study, sonographic diagnosis was less sensitive and also less specific than fecal examination. Its sensitivity was 52.2% and specificity was 51%.
In the endemic village in Koesan-gun, a total of 123 residents were scanned more than once, and in 61 (49.6%) the result was positive; only 12 (19.7%) of these, however, were found egg-positive and 49 (80.3%) were egg-negative. This low sensitivity and specificity of sonographic scanning may be an outcome of the light intensity of infection among the population examined; heavier infection might have resulted in higher sensitivity and specificity. Cases in which the result of sonography was false-negative might include light infection of one or two worms, and detection of these cases by any kind of method even including fecal examination is hard. In addition, most of egg positive residents who had fatty liver were found false-negative due to the increased background echogenicity from the fatty tissue.
The sonography also showed a false-positive result in 49 cases, which might have been due to visualization of the normal bile ducts, cured but scarred ducts or bile duct pathology resulting from other diseases. This high false-positive rate was partly contributed by slender residents. The sonographs of slender ones were so well visualized that the small normal intrahepatic bile ducts could be easily identified to have been regarded as false-positive. Even in the non-endemic village in Pyongchang-gun, the intrahepatic bile ducts were visualized in 31.3% of the 64 scanned residents. The present frequency of sonographic visualization of the ducts indicates that the criteria for sonographic diagnosis of clonorchiasis should be amended (Lim et al., 1989). Any sonographic feature which can specify mucosal hyperplasia would be necessary for the diagnosis.
Sonographic follow-up data of cured cases did not reveal decreased positivity after praziquantel treatment. Six to 24 months later, sonography still visualized dilated bile ducts in egg negative converters (cured cases). The sonographic positive rate was 52.2% before treatment but 64.3%, 50%, 50%, and 66.7% among cured cases 6, 12, 18, and 24 months after treatment, respectively. Total 20 of 35 cured cases (57.1%) were sonographic positive. This result demonstrates that for the differentiation of cured clonorchiasis, sonography is less useful. An animal experiment suggested the possibility of residual positive sonographic findings after treatment (Hong et al., 1994). Since abdominal sonography reflects not the worm but pathological changes in the bile duct (Lim et al., 1989) and the changes were found pathologically irreversible even after cure by praziquantel treatment (Lee et al., 1987), the sonographic differentiation has been expected hard. The present study confirmed that the sonographic finding of infected bile ducts remained for more than two years after treatment.
ACKNOWLEDGEMENT
We thank student members of the Songchon Medical Association and Medical Frontier Club (MFC), Seoul National University College of Medicine, for their help in the field.
Footnotes
This study was supported by a grant No. 01-97-062 from Seoul National University Hospital research fund (1997).
References
- 1.Chai JY, Yang YT, Lee SH, Seo BS. The detectability of helminth eggs from feces by cellophane thick smear technique. Korean J Parasitol. 1982;20(1):14–20. doi: 10.3347/kjp.1982.20.1.14. [DOI] [PubMed] [Google Scholar]
- 2.Chen M, Lu Y, Hua X, Mott KE. Progress in assessment of morbidity due to Clonorchis sinensis infection: a review of recent literature. Trop Dis Bull. 1994;91:R7–R67. [Google Scholar]
- 3.Hong ST. Changes of anti-Clonorchis sinensis IgG antibody in serum after praziqauntel treatment in human clonorchiasis. Korean J Parasitol. 1988;26(1):1–8. doi: 10.3347/kjp.1988.26.1.1. [DOI] [PubMed] [Google Scholar]
- 4.Hong ST, Park KH, Seo M, Choi BI, Chai JY, Lee SH. Correlation of sonographic findings with histopathological changes of the bile ducts in rabbits infected with Clonorchis sinensis. Korean J Parasitol. 1994;32(4):223–230. doi: 10.3347/kjp.1994.32.4.223. [DOI] [PubMed] [Google Scholar]
- 5.Lee SH, Hong ST, Kim CS, Sohn WM, Chai JY, Lee YS. Histopathological changes of the liver after praziquantel treatment in Clonorchis sinensis infected rabbits. Korean J Parasitol. 1987;25(2):110–122. doi: 10.3347/kjp.1987.25.2.110. [DOI] [PubMed] [Google Scholar]
- 6.Lee SH, Shim TS, Lee SM, Chi JG. Studies on pathological changes of the liver in albino rats infected with Clonorchis sinensis. Korean J Parasitol. 1978;16(2):148–155. doi: 10.3347/kjp.1978.16.2.148. [DOI] [PubMed] [Google Scholar]
- 7.Li BZ, Wang YY, Zhao YY, Zhao YN. Clonorchis sinensis and clonorchiasis. Shenyang, China: Shenyang Publ Co.; 1997. [Google Scholar]
- 8.Lim JH, Ko YT, Lee DH, Kim SY. Clonorchiasis: Sonographic findings in 59 proved cases. Am J Roentgenol. 1989;152:761–764. doi: 10.2214/ajr.152.4.761. [DOI] [PubMed] [Google Scholar]
- 9.Ministry of Health and Welfare and Korea Association of Health. Prevalence of intestinal parasitic infections in Korea - The Sixth Report. Seoul, Korea: 1997. [Google Scholar]
- 10.Rim HJ. The current pathobiology and chemotherapy of clonorchiasis. Korean J Parasitol. 1986;24(suppl):5–141. doi: 10.3347/kjp.1986.24.suppl.1. [DOI] [PubMed] [Google Scholar]
- 11.Rim HJ. Clonorchiasis in Korea. Korean J Parasitol. 1990;28(suppl):63–78. doi: 10.3347/kjp.1990.28.suppl.63. [DOI] [PubMed] [Google Scholar]
- 12.Seo BS, Lee SH, Cho SY, et al. An epidemiological study on clonorchiasis and metagonimiasis in riverside area in Korea. Korean J Parasitol. 1981;19(2):137–150. doi: 10.3347/kjp.1981.19.2.137. [DOI] [PubMed] [Google Scholar]