Abstract
Measuring cardiac troponin (cTn) I and T levels is currently considered to be a cornerstone for making the diagnosis of acute coronary syndrome (ACS).
Based on current literature, cTnI and cTnT are known to be very sensitive and specific for myocardial damage, regardless of the underlying cause. Lately, it has been found that cTns can be elevated and reflect worse prognoses in many situations where ACS is excluded. Such information can affect the validity of cTns as markers for ACS without classic symptoms. This may call for a revision of the troponin cutoff values to make a diagnosis of ACS. Furthermore, it opens a new field of study to determine appropriate management of patients with elevated cTn levels in whom ACS has been excluded.
Keywords: Coronary artery disease, Management, Nonischemic origin of troponin, Prognosis, Troponin
The patient who describes chest pain to the primary care physician represents an immediate challenge. Although chest pain can be a sign of a fatal heart attack, it can also stem from many other benign conditions. Creatine kinase (CK) and lactate dehydrogenase have been found to be nonspecific markers for acute coronary syndrome (ACS). In addition, troponins are highly accepted as more specific and sensitive markers that carry serious and fatal prognoses, even at low levels. More attention should be paid when making the diagnosis of ACS based on elevated troponin levels, because they are found to be elevated in many other conditions. The present review discusses the prognostic importance of elevated troponins level in ACS and other conditions, and emphasizes the need for more data to standardize the use of troponins in the diagnosis of ACS and to find appropriate management for many other conditions where ACS is excluded.
REVIEW OF TROPONINS
Pathophysiology of troponins
Troponins are protein complexes that modulate the contraction and relaxation of striated muscle. They are composed of three subunits: troponin I, T and C (TnI, TnT and TnC).
TnT binds to tropomyosin, thereby attaching the troponin complex to the thin filament. TnC binds to calcium ions, thereby exposing myosin-binding sites so that contraction can take place. TnI binds to actin and inhibits actin and myosin interaction (1). Troponins are found in skeletal and cardiac muscle, but not in smooth muscle. Approximately 7% of cardiac TnT (cTnT) and 3.5% of cTnI exist freely in the cardiac myocyte cytoplasm. The rest is bound to the sarcomere. cTnT content per gram of myocardium is roughly twice that of cTnI, and cTnI is smaller than cTnT (23.5 kDa versus 33 kDa) (1–3).
Studies have failed to find any cTnI outside the heart at any neonatal stage; in contrast, cTnT is expressed to a minor extent in skeletal muscle (4–6). These fetal isoforms are not detected by today’s techniques of immunohistochemistry and polymerase chain reaction (6,7).
Cardiac and skeletal troponins are encoded by different genes in the two types of muscle, yielding proteins that are immunologically distinct when identified by monoclonal antibodies. Because the amino acid sequence of TnC is the same in the two types of muscle, its detection is not useful (1,8).
Measuring troponin levels and interpretation of their elevation
Although cTnI and cTnT are specific markers for myocardial damage, different assays have different degrees of sensitivity and specificity. First-generation assays can mistakenly detect skeletal muscle troponin. cTnT assays are produced by a single manufacturer, and so tend to have relatively uniform cutoff concentrations. In contrast, cTnI assays, which use different kits to detect different epitopes, have different cutoff concentrations and standardizations (1).
The upper reference limit of cTn level is defined as the 97.5th percentile of the values measured in the normal control population (1). According to the American College of Cardiology (ACC) and the European Society of Cardiology (ESC), acute myocardial infarction (MI) should be diagnosed if cTnI or cTnT levels are higher than the 99th percentile with a coefficient of variation (a measure of how consistently an assay is able to produce the same result for the same sample) of 10% or less (very difficult to achieve), detected within 24 h after the index clinical event (1,9). Values in the intermediate zone suggest minor myocardial damage (1).
Macroinfarction is considered when the cTn level is higher than the 99th percentile and when the CK-MB fraction is elevated in the presence of ischemic symptoms. Microinfarction is considered when the cTn level is higher than the 99th percentile with a normal CK-MB fraction level.
According to the ACC/ESC definition of an acute MI, virtually all patients with unstable angina pectoris who have elevated cTns meet the criteria for an acute non-ST elevation MI (30% of previously diagnosed unstable angina pectoris cases are now considered to be non-ST elevation MI) (1).
The ACC/ECC joint committee disagreed with the suggestion of using two cutoff values, one for MI and one for unstable angina with myocardial necrosis. The committee believed it lacked a scientific basis and would lead to increased heterogeneity of diagnoses due to the different cutoff values used by different laboratory kits. In addition, patients with elevated cTn levels have similar risk profiles and coronary artery pathophysiology to patients who fit the diagnosis of non-Q wave MI (10).
After acute MI, cTnI and cTnT levels increase (first, by the release of the free cytosol fraction) after 6 h, are detected in the blood after 12 h, peak after one to two days, and reach the pre-MI normal levels after 10 days.
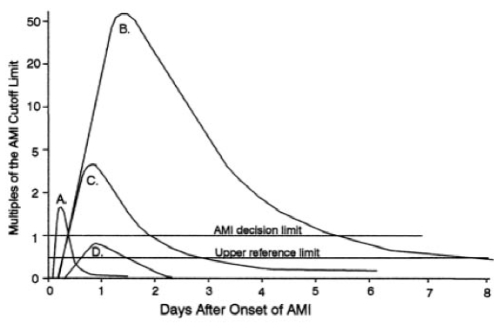
CK-MB isoforms (MB1 and MB2) are the most sensitive and specific markers for early (within 6 h) diagnosis of acute MI (11) (Figure 1). Their use is only indicated if positive results would change therapy. Their role has become less clear after the improvement of troponin assays (12).
Figure 1.
Time course of blood levels of cardiac markers after acute coronary syndromes. A Myoglobulin or creatine kinase (CK)-MB iso-forms. B Troponin. C Total CK-MB after acute myocardial infarction (AMI). D Troponin after unstable angina pectoris (the cutoff for AMI is at 1)
Prognostic values of elevated troponin levels
Any elevation of cTn levels in patients with ST elevation MI, non-ST elevation MI, unstable angina, congestive heart failure and chronic kidney insufficiency portends a worse outcome (13–17).
Patients with elevated cTns have a higher cardiac mortality rate, are more likely to have coronary thrombi, showers of emboli in the coronary microvasculature, and depressed ventricular function (1).
Recently, it has been found that elevations in cTn levels from causes other than ischemic heart disease (Table 1) are associated with worse prognoses (17,18).
TABLE 1.
Causes of cardiac troponin elevation other than ischemic heart disease
| Presumed mechanisms | Diagnoses |
|---|---|
| Myocardial stress | Congestive heart failure, hypertension with left ventricular hypertrophy, aortic valve disease, hypertrophic obstructive cardiomyopathy with significant left ventricular hypertrophy, strenuous exercise, pulmonary embolism, emphysema and asthma |
| Direct myocardial damage | Cardiac contusion, direct current cardioversion, ablation and toxins (adriamycin, 5-fluorouracil and transtuzumab) |
| Demand ischemia | Sepsis, systemic inflammatory response syndrome, burn, hypotension, hypovolemia, left ventricular hypertrophy, sympathomimetic agents and supraventricular tachycardia |
| Inflammation | Myocarditis, pericarditis, Kawasaki disease and parvovirus B19 infection |
| Infiltrative diseases | Amyloidosis, hemochromatosis, sarcoidosis and scleroderma |
| Immunological (autoantibodies, cytokines) causes | Cardiac transplantation, systemic lupus erythematosus, burn and sepsis |
| Unknown mechanism | Chronic renal insufficiency, neurological diseases (cerebrovascular accident, subarachnoid bleed) |
Prognostic value in unstable angina pectoris and non-ST elevation MI
According to the Fast Revascularization during InStability in CAD (FRISC) II trial (19), any elevation of cTnT in the noninvasive arm of the study increased the likelihood of severe three-vessel disease, an unstable plaque with thrombus and downstream microembolization, and impairment of coronary flow, all of which were associated with an increased risk for reinfarction and death. Higher serum troponin levels were associated with a greater likelihood of persistent occlusion of the culprit vessel, a reduced left ventricle ejection fraction and increased mortality (19).
In a meta-analysis of seven clinical trials and 19 cohort studies of patients with non-ST elevation MI (20), the mortality rate was found to be higher for patients with either a positive cTnT test at 28 weeks or a positive cTnI test at 10 weeks.
In another meta-analysis of 21 studies (21), patients with a non-ST elevation MI and a positive cTnT or cTnI level had a higher cardiac mortality rate in both short-term (30 days) and long-term (five months to three years) follow-up.
Similar results were observed in the Thrombolysis in Myocardial Infarction (TIMI) IIIB (22) and Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries (GUSTO) IIa trials (23).
Studies (14,24) also showed a reduction in both mortality and recurrent MI in patients with elevated troponin levels who were treated with delteparin or enoxaparin. No benefit was observed in patients without elevated troponin levels when treated with either drug. Only clopidogrel seems to be beneficial in patients regardless of troponin level elevations (25).
Prognostic value in ST elevation MI
The GUSTO-III trial studied patients with ST elevation MI who received thrombolytic therapy. Patients with elevated cTnT (greater than 0.2 ng/mL) at admission had a significantly higher 30-day mortality (26).
A pooled analysis (21) of 21 studies involving 18,982 patients with ACS found that elevated levels of cTnI or cTnT were associated with increased risk of cardiac death or reinfarction (at 30 days and at five months to three years) in both ST elevation MI and non-ST elevation MI.
A study (27) of 140 patients with ST elevation MI who underwent percutaneous coronary intervention (PCI) found that admission cTnT levels of more than 0.1 ng/mL were associated with persistent reduced blood flow (TIMI flow less than 3), higher incidence of no-reflow and higher mortality at 30 days and nine months.
Troponin and infarct size
Infarct size correlates with the troponin level measured at 72 h (more with cTnT than with cTnI) (28,29).
Troponin and reinfarction
Substantial re-elevation of cTnI level was found to occur after reinfarction (30), supporting the conclusion that changes in troponin levels are adequate to diagnose reinfarction (31,32).
Prognostic value after PCI
Troponin level elevation above the 99th percentile after PCI is indicative of cardiac cell injury and MI (33,34). The mechanism of this elevation is unknown (35,36). Some have suggested that increases of more than 25% are caused by the procedure itself, but the primary ACS that necessitated the PCI could still cause such an increase (12).
Prognostic value after open-heart surgery
In patients with coronary artery bypass surgery, cTnT was a highly sensitive and specific marker for perioperative MI (37). Elevated troponin levels were associated with increased short-and long-term mortality in patients who had undergone vascular surgery. Even small rises in serum troponin concentration after vascular surgery were associated with increased risk (38). Irrespective of the mechanism, the higher the value after surgery, the worse the prognosis (39,40).
Causes of cTn elevation other than ischemic heart disease
It has been found that troponin release can be caused not only by irreversible cell damage, but also by reversible damage (41).
Among 1000 consecutive patients presenting to the emergency department of a large urban hospital, cTnI level was elevated on admission in 112 patients, 45% of whom had a final diagnosis other than ACS (42).
Another study (43) of 102 patients with a cTnI level of more than 0.6 ng/mL, 66% of patients had a final diagnosis of ACS. Of the 34% of patients who did not have ACS, the elevation in troponin level was secondary to a variety of causes including electrical cardioversion, muscular disorders, chronic renal insufficiency, sepsis, lung disease, hypothyroidism, systemic lupus erythematosus and gynecomastia. The study also indicated that the higher the cTnI level, the higher the positive predictive value was for the diagnosis of ACS (43).
Ammann and colleagues (44) evaluated 58 patients who were admitted to the intensive care unit for diagnoses other than ACS. Among the 55% of patients with elevated troponin levels, tumour necrosis factore, interleukin-6 and C-reactive protein levels were significantly higher than among patients with undetectable troponin. Mortality was fourfold higher in the troponin-positive group. Coronary artery disease (CAD) was excluded in 72% of troponin-positive patients. Thus, troponin elevation among intensive care unit patients with sepsis or systemic inflammatory response syndrome and with or without shock is often seen without significant CAD, and carries a worse prognosis (41).
Mechanisms of cTn elevation in situations other than ACS
Any myocardial stress can lead to troponin release (10,45,46) (Table 1). Other factors causing troponin release include sympathetic discharge; cytokine release such as heat shock protein and tumour necrosis factor-alpha; and infections and autoantibodies such as in immune disease after cardiac transplantation and systemic lupus erythematosus (10,45,47).
Prognosis of cTn elevation in situations other than ischemic heart disease
Short- and/or long-term survival is impaired among patients with troponin elevation in many different clinical settings, including congestive heart failure, sepsis, pulmonary disease, acute pulmonary embolism, pericarditis, myocarditis, immune response after heart transplantation and renal insufficiency (18,41,48).
Management of cTns elevation in situations other than ischemic heart disease
Management is still unknown, but one has to exclude any possible underlying ischemic heart disease by clinical evaluation, electrocardiography, echocardiography, cardiac stress testing and, if necessary, coronary angiography.
Treatment should target underlying disorders. All patients should be on acetylsalicylic acid if there is no apparent contraindication. In addition, angiotensin-converting enzyme inhibitors, beta-blockers and statins should be used as indicated. There are no current data to support the use of antithrombotic or antiplatelet agents, or an early PCI in this group (41).
False-positive and false-negative results
Fibrin can confound the assay for cTnI, so heparinized plasma for this assay is preferred (27). Heterophilic antibodies and cross-reacting human antimouse antibodies in patients who make or receive antibodies can lead to false-positive results. Heparin can bind to troponin and lead to lower levels (dose-dependent) (49).
Autoantibodies against the central portion of cTnI can delay the diagnosis and/or result in false-negative results (50).
Elevation of cTns in renal insufficiency
Cardiovascular disease accounts for roughly 50% of deaths in patients with chronic renal failure. Patients with renal failure are at higher risk for silent ischemia (17%) and atypical clinical presentation. Electrocardiogram results are not reliable, because ST segment changes are difficult to interpret secondary to electrolyte imbalances, left ventricular hypertrophy and medications.
Using a second-generation assay, cTnT was found to be elevated in up to 53% of patients with renal failure with no clinical evidence of acute myocardial necrosis (51).
Despite using the latest generation assays and higher cutoff values (higher than the 99th percentile) cTnT and cTnI were positive in 82% and 6% of dialysis patients, respectively (results changed according to the cutoff values) (15).
Reasons for discordance between cTnI and cTnT elevation in chronic renal failure
Free cTnT (7%) is more abundant than free cTnI (3.5%) for each given myocyte cytoplasm. Furthermore, the cTnT content per gram is roughly twice that of cTnI. cTnI level decreased by up to 86% from pre- to postdialysis, possibly because it may adsorb to the dialysis membrane; however, cTnT levels tend to increase after dialysis, possibly due to hemoconcentration. Finally, cTnI undergoes more postrelease modifications (phosphorylation, proteolysis and oxidation) than cTnT (51).
Mechanism of cTn elevation in patients with renal insufficiency
The exact mechanism is still unknown (51–57) (Table 2). It is less likely due to decreased clearance of cTns, because patients with renal disease have the same clearance rate of troponin levels as patients without renal disease after ACS. Troponin levels remain elevated even after kidney transplantation (51).
TABLE 2.
Hypothesized causes of cardiac troponin (cTn) elevation and possible underlying mechanisms in patients with renal insufficiency
| Cause | Possible underlying mechanism |
|---|---|
| Uremic skeletal myopathy and/or re-expression of cTnT | Skeletal muscle injury caused by toxic uremic effect |
| Silent myocardial necrosis, recurrent silent microinfarctions, congestive heart failure, and left ventricular hypertrophy (more common in end-stage renal disease) | Perfusion defects, abnormal coronary vasomotor activity, and endothelial dysfunction due to oxidative stress and inflammation |
| Cardiac injury | Calcium and oxalate deposition |
| Episodes of hypotension | Fluid problems during hemodialysis |
| Decreased clearance of cTns | Defect of excretion process in renal failure |
Prognostic values of cTns in asymptomatic patients with end-stage renal disease
Serum elevation of cTn levels is highly prognostic for both short- and long-term outcomes in symptomatic and asymptomatic patients.
There is increasing evidence that elevation in serum cTnI and cTnT levels in stable asymptomatic patients with end-stage renal disease is predictive of worse long-term cardiovascular outcomes (15). The reason for this correlation is unknown, although a correlation between increased troponin levels and diffuse CAD in those patients has been reported (58,59).
A prospective study of 733 asymptomatic patients with end-stage renal disease showed that increased levels of both cTnT and cTnI were associated with increased risk of mortality at two years. Adjusted relative risks of death were two- to fivefold higher among those with increases in cTnT and cTnI values (as defined by the 99th percentile values of 0.01 μg/L and 0.1 μg/L for cTnT and cTnI, respectively) (15).
A study (16) of 107 hemodialysis patients found that elevation in cTnT was associated with an almost sevenfold increase in risk of death after two years.
Similar association has been reported in asymptomatic patients with chronic kidney disease who are not dialysis-dependent (60).
Prognostic values of cTns in symptomatic patients with end-stage renal disease
Elevation in cTnT levels may also be highly prognostic for both short- and long-term outcomes among patients with renal insufficiency who present with ACS.
Studying cTnT levels in the GUSTO-IV trial showed that increased cTnT levels are associated with a small but significant increased risk of MI or death in both patient groups of normal and low creatinine clearance (most patients had mild to moderate renal dysfunction and only 2% had creatinine clearance of less than 10%, so it is uncertain for patients with end-stage renal disease) (61).
Those patients had more severe coronary atherosclerosis, higher rates of restenosis and higher periprocedural morbidity and mortality (51).
Accuracy of elevated cTnT and cTnI levels in patients with end-stage renal disease
A number of studies have reported a large percentage of false-positive elevations of serum cTnT in patients with end-stage renal disease (15,62,63) up to 14 times above normal in one patient (64). cTnI is less likely to be associated with false-positive results in patients with end-stage renal disease (62,65). A higher troponin threshold was proposed as diagnostic of myocardial ischemia in patients with chronic renal insufficiency (66). Serial measurements, preferably of cTnI, and if not available, of cTnT and CK-MB, are suggested to diagnose ACS.
Management of patients with renal insufficiency and high cTn levels
There are no specific guidelines to date for managing such patients. A sequential rise in serum troponin is consistent with new myocardial damage in patients with renal insufficiency. Coronary angiography is still the gold standard for diagnosis of ACS in patients with end-stage renal disease.
It is reasonable to use acetylsalicylic acid, beta-blockers and angiotensin-converting enzyme inhibitors if not contraindicated (51). Recent data have shown effectiveness and safety of tirofiban in patients with mild to moderate renal insufficiency (51).
CONCLUSIONS
One should not make the diagnosis of ACS based solely on the presence of increased levels of cTns, because they can be increased by other factors.
The use of pretest probability when measuring cTns is helpful in making the diagnosis of ACS.
Mild elevation of cTnT or cTnI levels, even in patients without evidence of ischemic heart disease, carries important prognostic value, and should be managed appropriately.
Subsequent cTn level measurement in patients with renal failure and elevated cTn levels is important to differentiate acute from chronic events. In both symptomatic and asymptomatic patients, elevated cTn levels imply worse prognoses and should be managed appropriately.
More effort should be given to standardizing the use of both cTnI and cTnT in the diagnosis of ACS, taking into consideration the other causes of troponin elevation.
More studies are needed to establish the management of patients with elevated cTns in the absence of ischemic heart disease and in asymptomatic patients with renal failure.
REFERENCES
- 1.Antman EM. Decision making with cardiac troponin tests. N Engl J Med. 2002;346:2079–82. doi: 10.1056/NEJMe020049. [DOI] [PubMed] [Google Scholar]
- 2.Adams JE, 3rd, Abendschein DR, Jaffe AS. Biochemical markers of myocardial injury. Is MB creatine kinase the choice for the 1990s? Circulation. 1993;88:750–63. doi: 10.1161/01.cir.88.2.750. [DOI] [PubMed] [Google Scholar]
- 3.Katus HA, Remppis A, Scheffold T, Diederich KW, Kuebler W. Intracellular compartmentation of cardiac troponin T and its release kinetics in patients with reperfused and nonreperfused myocardial infarction. Am J Cardiol. 1991;67:1360–7. doi: 10.1016/0002-9149(91)90466-x. [DOI] [PubMed] [Google Scholar]
- 4.Adams JE, III, Bodor GS, Davila-Roman VG, et al. Cardiac troponin I: A marker with high specificity for cardiac injury. Circulation. 1993;88:101–6. doi: 10.1161/01.cir.88.1.101. [DOI] [PubMed] [Google Scholar]
- 5.Bodor GS, Porterfield D, Voss EM, Smith S, Apple FS. Cardiac troponin-I is not expressed in fetal and healthy or diseased adult human skeletal muscle tissue. Clin Chem. 1995;41:1710–5. [PubMed] [Google Scholar]
- 6.Ricchiuti V, Voss EM, Ney A, Odland M, Anderson PA, Apple FS. Cardiac troponin T isoforms expressed in renal diseased skeletal muscle will not cause false-positive results by the second generation cardiac troponin T assay by Boehringer Mannheim. Clin Chem. 1998;44:1919–24. [PubMed] [Google Scholar]
- 7.Ricchiuti V, Apple FS. RNA expression of cardiac troponin T isoforms in diseased human skeletal muscle. Clin Chem. 1999;45:2129–35. [PubMed] [Google Scholar]
- 8.Schreier T, Kedes L, Gahlmann R. Cloning, structural analysis, and expression of the human slow twitch skeletal muscle/cardiac troponin C gene. J Biol Chem. 1990;265:21247–53. [PubMed] [Google Scholar]
- 9.Panteghini M, Pagani F, Yeo KT, et al. Committee on Standardization of Markers of Cardiac Damage of the IFCC. Evaluation of imprecision for cardiac troponin assays at low-range concentrations. Clin Chem. 2004;50:327–32. doi: 10.1373/clinchem.2003.026815. [DOI] [PubMed] [Google Scholar]
- 10.Jaffe A, Ravkilde J, Roberts R, et al. It’s time for a change to a troponin standard. Circulation. 2000;102:1216–20. doi: 10.1161/01.cir.102.11.1216. [DOI] [PubMed] [Google Scholar]
- 11.Zimmerman J, Fromm R, Meyer D, et al. Diagnostic marker cooperative study for the diagnosis of myocardial infarction. Circulation. 1999;99:1671–7. doi: 10.1161/01.cir.99.13.1671. [DOI] [PubMed] [Google Scholar]
- 12.Eggers KM, Oldgren J, Nordenskjold A, Lindhal B. Diagnostic value of serial measurement of cardiac markers in patients with chest pain: Limited value of adding myoglobin to troponin I for exclusion of myocardial infarction. Am Heart J. 2004;148:574–81. doi: 10.1016/j.ahj.2004.04.030. [DOI] [PubMed] [Google Scholar]
- 13.Olatidoye AG, Wu AH, Feng YJ, Waters D. Prognostic role of troponin T versus troponin I in unstable angina pectoris for cardiac events with meta-analysis comparing published studies. Am J Cardiol. 1998;81:1405–10. doi: 10.1016/s0002-9149(98)00200-8. [DOI] [PubMed] [Google Scholar]
- 14.Heeschen C, Hamm CW, Goldmann B, Deu A, Langenbrink L, White HD for the PRISM Study Investigators. Troponin concentrations for stratification of patients with acute coronary syndromes in relation to therapeutic efficacy of tirofiban. PRISM Study Investigators Platelet Receptor Inhibition in Ischemic Syndrome Management Lancet. 1999;354:1757–62. doi: 10.1016/s0140-6736(99)10285-x. [DOI] [PubMed] [Google Scholar]
- 15.Apple FS, Murakami MM, Pearce LA, Herzog CA. Predictive value of cardiac troponin I and T for subsequent death in end-stage renal disease. Circulation. 2002;106:2941–5. doi: 10.1161/01.cir.0000041254.30637.34. [DOI] [PubMed] [Google Scholar]
- 16.Dierkes J, Domröse U, Westphal S, et al. Cardiac troponin T predicts mortality in patients with end-stage renal disease. Circulation. 2000;102:1964–9. doi: 10.1161/01.cir.102.16.1964. [DOI] [PubMed] [Google Scholar]
- 17.Horwich TB, Patel J, McLellan WR, Fonarow GC. Cardiac troponin I is associated with impaired hemodynamics, progressive left ventricular dysfunction, and increased mortality rates in advanced heart failure. Circulation. 2003;108:833–8. doi: 10.1161/01.CIR.0000084543.79097.34. [DOI] [PubMed] [Google Scholar]
- 18.Ni CY. Cardiac troponin I: A biomarker for detection and risk stratification of minor myocardial damage. Clin Lab. 2001;47:483–92. [PubMed] [Google Scholar]
- 19.Lindahl B, Diderholm E, Lagerqvist B, Venge P, Wallentin L FRISC II (Fast Revascularization during InStability in CAD) Investigators. Mechanisms behind the prognostic value of troponin T in unstable coronary artery disease: A FRISC II substudy. J Am Coll Cardiol. 2001;38:979–86. doi: 10.1016/s0735-1097(01)01501-7. [DOI] [PubMed] [Google Scholar]
- 20.Heidenreich PA, Alloggiamento T, Melsop K, McDonald KM, Go AS, Hlatky MA. The prognostic value of troponin in patients with non-ST elevation acute coronary syndromes: A meta-analysis. J Am Coll Cardiol. 2001;38:478–85. doi: 10.1016/s0735-1097(01)01388-2. [DOI] [PubMed] [Google Scholar]
- 21.Ottani F, Galvani M, Nicolini FA, et al. Elevated cardiac troponin levels predict the risk of adverse outcome in patients with acute coronary syndromes. Am Heart J. 2000;140:917–27. doi: 10.1067/mhj.2000.111107. [DOI] [PubMed] [Google Scholar]
- 22.Becker RC, Cannon CP, Tracy RP, et al. Relation between systemic anticoagulation as determined by activated partial thromboplastin time and heparin measurements and in-hospital clinical events in unstable angina and non-Q wave myocardial infarction. Thrombolysis in Myocardial Ischemia III B Investigators. Am Heart J. 1996;131:421–33. doi: 10.1016/s0002-8703(96)90519-0. [DOI] [PubMed] [Google Scholar]
- 23.Newby LK, Christenson RH, Ohman EM, et al. Value of serial troponin T measures for early and late risk stratification in patients with acute coronary syndromes. The GUSTO-IIa Investigators. Circulation. 1998;98:1831–3. doi: 10.1161/01.cir.98.18.1853. [DOI] [PubMed] [Google Scholar]
- 24.Hamm CW, Heeschen C, Goldmann B, et al. Benefit of abciximab in patients with refractory unstable angina in relation to serum troponin T levels. c7E3 Fab Antiplatelet Therapy in Unstable Refractory Angina (CAPTURE) Study Investigators. N Engl J Med. 1999;340:1623–9. doi: 10.1056/NEJM199905273402103. (Erratum in 1999;341:548) [DOI] [PubMed] [Google Scholar]
- 25.Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001;345:494–502. doi: 10.1056/NEJMoa010746. [DOI] [PubMed] [Google Scholar]
- 26.Ohman EM, Armstrong PW, White HD, et al. Risk stratification with a point-of-care cardiac troponin T test in acute myocardial infarction. GUSTOIII Investigators. Global Use of Strategies To Open Occluded Coronary Arteries. Am J Cardiol. 1999;84:1281–6. doi: 10.1016/s0002-9149(99)00558-5. [DOI] [PubMed] [Google Scholar]
- 27.Giannitsis E, Muller-Bardorff M, Lehrke S, et al. Admission troponin T level predicts clinical outcomes, TIMI flow, and myocardial tissue perfusion after primary percutaneous intervention for acute ST-segment elevation myocardial infarction. Circulation. 2001;104:630–5. doi: 10.1161/hc3101.093863. [DOI] [PubMed] [Google Scholar]
- 28.Licka M, Zimmermann R, Zehelein J, Dengler TJ, Katus HA, Kubler W. Troponin T concentrations 72 hours after myocardial infarction as a serological estimate of infarct size. Heart. 2002;87:520–4. doi: 10.1136/heart.87.6.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Panteghini M, Cuccia C, Bonetti G, Giubbini R, Pagani F, Bonini E. Single-point cardiac troponin T at coronary care unit discharge after myocardial infarction correlates with infarct size and ejection fraction. Clin Chem. 2002;48:1432–6. [PubMed] [Google Scholar]
- 30.Apple FS, Murakami MM. Cardiac troponin and creatine kinase MB monitoring during in-hospital myocardial reinfarction. Clin Chem. 2005;51:460–3. doi: 10.1373/clinchem.2004.042887. [DOI] [PubMed] [Google Scholar]
- 31.Falahati A, Sharkey SW, Christensen D, et al. Implementation of serum cardiac troponin I as marker for detection of acute myocardial infarction. Am Heart J. 1999;137:332–7. doi: 10.1053/hj.1999.v137.92412. [DOI] [PubMed] [Google Scholar]
- 32.Bodor GS, Porter S, Landt Y, Ladenson JH. Development of monoclonal antibodies for an assay of cardiac troponin-I and preliminary results in suspected cases of myocardial infarction. Clin Chem. 1992;38:2203–14. [PubMed] [Google Scholar]
- 33.Myocardial infarction redefined – a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. Eur Heart J. 2000;21:1502–13. doi: 10.1053/euhj.2000.2305. [DOI] [PubMed] [Google Scholar]
- 34.Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined – a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000;36:959–69. doi: 10.1016/s0735-1097(00)00804-4. [DOI] [PubMed] [Google Scholar]
- 35.Fuchs S, Stabile E, Mintz GS, et al. Intravascular ultrasound findings in patients with acute coronary syndromes with and without elevated troponin I level. Am J Cardiol. 2002;89:1111–3. doi: 10.1016/s0002-9149(02)02282-8. [DOI] [PubMed] [Google Scholar]
- 36.Herrmann J, Haude M, Lerman A, et al. Abnormal coronary flow velocity reserve after coronary intervention is associated with cardiac marker elevation. Circulation. 2001;103:2339–45. doi: 10.1161/01.cir.103.19.2339. [DOI] [PubMed] [Google Scholar]
- 37.Carrier M, Pellerin M, Perrault LP, Solymoss BC, Pelletier LC. Troponin levels in patients with myocardial infarction after coronary artery bypass grafting. Ann Thorac Surg. 2000;69:435–40. doi: 10.1016/s0003-4975(99)01294-1. [DOI] [PubMed] [Google Scholar]
- 38.Landesberg G, Shatz V, Akopnik I, et al. Association of cardiac troponin, CK-MB, and postoperative myocardial ischemia with long-term survival after major vascular surgery. J Am Coll Cardiol. 2003;42:1547–54. doi: 10.1016/j.jacc.2003.05.001. [DOI] [PubMed] [Google Scholar]
- 39.Greenson N, Macoviak J, Krishnaswamy P, et al. Usefulness of cardiac troponin I in patients undergoing open heart surgery. Am Heart J. 2001;141:447–55. doi: 10.1067/mhj.2001.113071. [DOI] [PubMed] [Google Scholar]
- 40.Lehrke S, Steen H, Sievers HH, et al. Cardiac troponin T for prediction of short and long-term morbidity and mortality after elective open heart surgery. Clin Chem. 2004;50:1560–7. doi: 10.1373/clinchem.2004.031468. [DOI] [PubMed] [Google Scholar]
- 41.Jeremias A, Gibson M. Alternative causes for elevated cardiac troponin levels when acute coronary syndromes are excluded. Ann Intern Med. 2005;142:786–91. doi: 10.7326/0003-4819-142-9-200505030-00015. [DOI] [PubMed] [Google Scholar]
- 42.Ng SM, Krishnaswamy P, Morrisey R, Clopton P, Fitzgerald R, Maisel AS. Mitigation of the clinical significance of spurious elevations of cardiac troponin I in settings of coronary ischemia using serial testing of multiple cardiac markers. Am J Cardiol. 2001;87:994–9. doi: 10.1016/s0002-9149(01)01436-9. [DOI] [PubMed] [Google Scholar]
- 43.Khan IA, Tun A, Wattanasauwan N, et al. Elevation of serum cardiac troponin I in noncardiac and cardiac diseases other than acute coronary syndromes. Am J Emerg Med. 1999;17:225–9. doi: 10.1016/s0735-6757(99)90110-9. [DOI] [PubMed] [Google Scholar]
- 44.Zeng L, Chen Y, Wu M. Cardiac troponin I: A marker for detecting non-ischemic cardiac injury. Zhonghua Yi Xue Za Zhi. 2001;81:393–5. [PubMed] [Google Scholar]
- 45.Babuin L, Jaffe AS. Troponin: The biomarker of choice for the detection of cardiac injury. CMAJ. 2005;173:1191–202. doi: 10.1503/cmaj.050141. (Errata in 2005;173:1490;2006;174:353) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ammann P, Maggiorini M, Bertel O, et al. Troponin as a risk factor for mortality in critically ill patients without acute coronary syndromes. J Am Coll Cardiol. 2003;41:2004–9. doi: 10.1016/s0735-1097(03)00421-2. [DOI] [PubMed] [Google Scholar]
- 47.Morrow D. Cardiac-specific troponins beyond ischemic heart disease. In: Wu AH, editor. Cardiac Markers. 2nd edn. Totowa, New Jersey: Humana Press Inc; 2003. pp. 149–70. [Google Scholar]
- 48.Francis GS, Tang WH. Cardiac troponins in renal insufficiency and other non-ischemic cardiac conditions. Prog Cardiovasc Dis. 2004;47:196–206. doi: 10.1016/j.pcad.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 49.Gerhardt W, Nordin G, Herbert AK, et al. Troponin T and I assays show decreased concentrations in heparin plasma compared with serum: Lower recoveries in early than in late phases of myocardial injury. Clin Chem. 2000;46:817–21. [PubMed] [Google Scholar]
- 50.Eriksson S, Hellman J, Pettersson K. Autoantibodies against cardiac troponins. N Engl J Med. 2005;352:98–100. doi: 10.1056/NEJM200501063520123. [DOI] [PubMed] [Google Scholar]
- 51.Freda BJ, Tang WH, Van Lente F, Peacock WF, Francis GS. Cardiac troponins in renal insufficiency. J Am Coll Cardiol. 2002;40:2065–71. doi: 10.1016/s0735-1097(02)02608-6. [DOI] [PubMed] [Google Scholar]
- 52.Iliou MC, Fumeron C, Benoit MO, et al. Factors associated with increased serum levels of cardiac troponins T and I in chronic haemodialysis patients: Chronic Haemodialysis And New Cardiac Markers Evaluation (CHANCE) study. Nephrol Dial Transplant. 2001;16:1452–8. doi: 10.1093/ndt/16.7.1452. [DOI] [PubMed] [Google Scholar]
- 53.Lowbeer C, Ottosson-Seeberger A, Gustafsson SA, Norrman R, Hulting J, Gutierrez A. Increased cardiac troponin T and endothelin-1 concentrations in dialysis patients may indicate heart disease. Nephrol Dial Transplant. 1999;14:1948–55. doi: 10.1093/ndt/14.8.1948. [DOI] [PubMed] [Google Scholar]
- 54.Porter GA, Norton TL, Lindsley J, Stevens JS, Phillips DS, Bennett WM. Relationship between elevated serum troponin values in end-stage renal disease patients and abnormal isotopic cardiac scans following stress. Ren Fail. 2003;25:55–65. doi: 10.1081/jdi-120017468. [DOI] [PubMed] [Google Scholar]
- 55.Thambyrajah J, Landray MJ, McGlynn FJ, Jones HJ, Wheeler DC, Townend JN. Abnormalities of endothelial function in patients with predialysis renal failure. Heart. 2000;83:205–9. doi: 10.1136/heart.83.2.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Scott B, Deman A, Peeters P, et al. Cardiac troponin T and malondialdehyde modified plasma lipids in haemodialysis patients. Nephrol Dial Transplant. 2003;18:737–42. doi: 10.1093/ndt/gfg020. [DOI] [PubMed] [Google Scholar]
- 57.Hung SY, Hung YM, Fang HC, et al. Cardiac troponin I and creatine kinase isoenzyme MB in patients with intradialytic hypotension. Blood Purif. 2004;22:338–43. doi: 10.1159/000079188. [DOI] [PubMed] [Google Scholar]
- 58.deFilippi C, Wasserman S, Rosanio S, et al. Cardiac troponin T and C-reactive protein for predicting prognosis, coronary atherosclerosis, and cardiomyopathy in patients undergoing long-term hemodialysis. JAMA. 2003;290:353–9. doi: 10.1001/jama.290.3.353. [DOI] [PubMed] [Google Scholar]
- 59.Jung HH, Ma KR, Han H. Elevated concentrations of cardiac troponins are associated with severe coronary artery calcification in asymptomatic haemodialysis patients. Nephrol Dial Transplant. 2004;19:3117–23. doi: 10.1093/ndt/gfh488. [DOI] [PubMed] [Google Scholar]
- 60.Goicoechea M, Garca de Vinuesa S, Gómez-Campderá F, et al. Clinical significance of cardiac troponin T levels in chronic kidney disease patients: predictive value for cardiovascular risk. Am J Kidney Dis. 2004;43:846–53. doi: 10.1053/j.ajkd.2003.12.048. [DOI] [PubMed] [Google Scholar]
- 61.Aviles RJ, Askari AT, Lindahl B, et al. Troponin T levels in patients with acute coronary syndromes, with or without renal dysfunction. N Engl J Med. 2002;346:2047–52. doi: 10.1056/NEJMoa013456. [DOI] [PubMed] [Google Scholar]
- 62.McLaurin MD, Apple FS, Voss EM, Herzog CA, Sharkey SW. Cardiac troponin I, cardiac troponin T, and creatine kinase MB in dialysis patients without ischemic heart disease: Evidence of cardiac troponin T expression in skeletal muscle. Clin Chem. 1997;43:976–82. [PubMed] [Google Scholar]
- 63.Hafner G, Thome-Kromer B, Schaube J, et al. Cardiac troponins in serum in chronic renal failure. Clin Chem. 1994;40:1790. (Lett) [PubMed] [Google Scholar]
- 64.Bhayana V, Gougoulias T, Cohoe S, Henderson AR. Discordance between results for serum troponin T and troponin I in renal disease. Clin Chem. 1995;41:312–7. [PubMed] [Google Scholar]
- 65.Martin GS, Becker BN, Schulman G. Cardiac troponin-I accurately predicts myocardial injury in renal failure. Nephrol Dial Transplant. 1998;13:1709–12. doi: 10.1093/ndt/13.7.1709. [DOI] [PubMed] [Google Scholar]
- 66.Van Lente F, McErlean ES, DeLuca SA, Peacock WF, Rao JS, Nissen SE. Ability of troponins to predict adverse outcomes in patients with renal insufficiency and suspected acute coronary syndromes: a case-matched study. J Am Coll Cardiol. 1999;33:471–8. doi: 10.1016/s0735-1097(98)00592-0. [DOI] [PubMed] [Google Scholar]