Abstract
A 54-year-old male farmer residing in Chunchon, Korea, complaining of blood tinged discharge and tinnitus in the left ear for two days, was examined in August 16, 1996. Otoscopic examination revealed live maggots from the ear canal. The patient did not complain of any symptoms after removal of maggots. Five maggots recovered were identified as the third stage larvae of Lucilia sericata (Diptera: Calliphoridae). This is the first record of aural myiasis in Korea.
Keywords: myiasis, Diptera, Calliphoridae, Lucilia sericata, tinnitus, otorrhea
The aural myiasis is not a common infestation in Korea. Although it is not a common manifestation in the field of otorhinolaryngology, the possibility of its occurrence always exists. The clinical spectrum was wide from maggots in the ear to otalgia, otorrhea, perforation of drum, bleeding, itching, roaring sound, tinnitus, furuncle of the external ear, and restlessness. Referral of species identification of maggots by clinicians are necessary for the collection of epidemiological data of aural myiasis cases. We report the larval infestation of Lucilia sericata in the left external auditory canal of a man in Chunchon, Korea. This case is the first written report of aural myiasis in Korea.
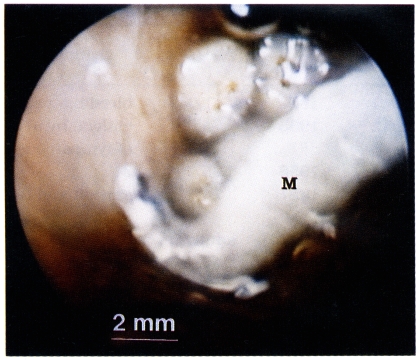
A 54-year-old male farmer visited the outpatient clinic of the Department of Otorhinolaryngology, Hallym University Hospital in August 16, 1996. He complained of blood tinged discharge and tinnitus for two days. Otoscopic examination revealed a number of maggots, blood tinged discharges, and cerumen in the left external auditory canal (Fig. 1). The external auditory canal showed no hyperemic inflammation and tympanic membrane was intact. There were no maggots or lesions in the right external auditory canal. Maggots were removed under the light microscopic field. The external auditory canal was washed with ether to anesthesize worms. There were no maggots or any discharge in the following examinations in one and three weeks. He no longer complained of tinnitus after treatment.
Fig. 1.
Lucilia sericata maggot (M) in the left external auditory canal of the male farmer seen via otoscope.
The size of 5 live maggots removed was 10.0-14.1×2.0-2.5 mm (mean 11.5×2.1 mm). The maggots were identified as the third stage larvae of Lucilia (Phaenicia) sericata Meigen (Diptera: Calliphoridae) according to following criteria: mouthparts with no accessory oral sclerite; cephalopharyngeal skeleton without pigmented area below posterior extremity of ventral cornua; posterior spiracle with complete peritreme enclosing a button; inner tubercles of upper margin of anal segment separated by a distance approximately equal to distance between inner and medial tubercles. Speciemen was deposited in the Systematic Entomology Laboratory, Agricultural Research Service, US Department of Agriculture (identificaton lot number 9807357).
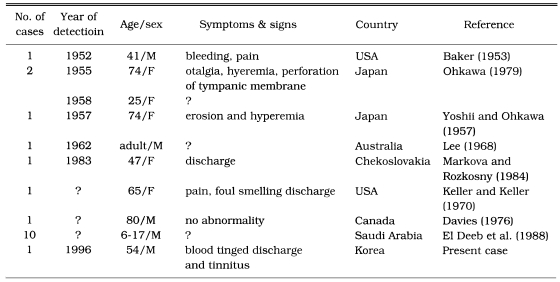
Recently there was a case of the third stage larval infestation of Lucilia sp. in the gastrointestinal system of a 91-year-old man admitted due to cerebral infarct in Inchon, Korea. A total of 45 maggots were recovered for two days through nasogastric tube (Chung et al., 1996). Twenty six cases of aural myiasis had been reported in Japan (Chigusa et al., 1994). From literatures, we could find 19 cases of aural myiasis caused by L. sericata including the present case. Blood tinged discharge, tinnitus, discharge, bleeding, pain, and foul smelling discharge were reported symptoms (Table 1). Aural myiasis, like this case, is easily detectable by otoscopic examination.
Table 1.
Summary of the aural myiasis cases caused by Lucilia sericata
The treatment of aural myiasis is simple in early manifestation stage, such as removal of maggots and cleansing lesion with 70% ethanol, 10% chloroform, or normal saline (Keller and Keller, 1970; Mendivil and Shamma, 1979; Braverman et al., 1994). If the tympanic membrane is perforated in aural myiasis case, cleansing with normal saline and concomitant suction would be appropriate. When there was a furuncle, the application of antibiotics ointment after cleansing and intake of antibiotics are recommended. In this case, audiogram was not done. If there was a perforation of the tympanic membrane and hearing loss, the examination of auditory function before and after treatment would be necessary. If it is not treated appropriately, the chronic inflammation of the external auditory canal, chronic otitis media or bony destruction from chronic suppuration may be developed (Turnbull and Franklin, 1942).
ACKNOWLEDGEMENTS
We appreciate Mr. Norman E. Woodley, Systematic Entomology Laboratory, Agricultural Research Service, US Department of Agriculture, Building 046, BARC-W, 10300 Baltimore Avenue, Beltsville, MD 20705, USA for his kind identification of maggot.
References
- 1.Baker MC. Green bottle fly worm infestation of the ear. Laryngoscope. 1953;63:545–548. doi: 10.1288/00005537-195306000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Braverman I, Dano I, Saah D, Gapany B. Aural myiasis caused by flesh fly larva, Sarcophaga haemorrhoidalis. J Otolaryngol. 1994;23:204–205. [PubMed] [Google Scholar]
- 3.Chigusa Y, Tanaka K, Yokoi H, et al. Two cases of otomyiasis caused by Sarcophaga peregrina and S. similis (Diptera: Sarcophagidae) Jpn J Sanit Zool. 1994;45:153–157. [Google Scholar]
- 4.Chung PR, Jung Y, Kim KS, Cho SK, Jeong S, Ree HI. A case of internal myiasis in Korea. Korean J Parasitol. 1996;34:151–154. doi: 10.3347/kjp.1996.34.2.151. [DOI] [PubMed] [Google Scholar]
- 5.Davies DM. Human aural myiasis: a case in Ontario, Canada, and a partial review. J Parasitol. 1976;62:124. [PubMed] [Google Scholar]
- 6.El Deeb NE, El Matarawy OM, Ali AA, et al. Human aural myiasis in Taif, Saudi Arabia. J Egypt Soc Parasitol. 1988;18:129–132. [PubMed] [Google Scholar]
- 7.Keller AP, Keller AP. Myiasis of the middle ear. Laryngoscope. 1970;80:646–650. doi: 10.1288/00005537-197004000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Lee HL. Human myiasis in Australia. Med J Aust. 1968;1:170–173. doi: 10.5694/j.1326-5377.1968.tb28850.x. [DOI] [PubMed] [Google Scholar]
- 9.Markova M, Rozkosny R. Myiasis in the ORL area. Cesk Otolaryngol. 1984;33:257–259. [PubMed] [Google Scholar]
- 10.Mendivil JA, El Shamma NA. Aural myiasis caused by Cochliomyia hominivorax: case report. Mil Med. 1979;144:261–262. [PubMed] [Google Scholar]
- 11.Ohkawa T. Biotic foreign bodies in otolaryngology. Pract Otol Kyoto. 1979;72:1105–1175. [Google Scholar]
- 12.Turnbull FM, Franklin LB. Aural infestation with screw worms. JAMA. 1942;120:117–119. [Google Scholar]
- 13.Yoshi M, Ohkawa C. A case of otomyiasis caused by Phaenicia sericata. J Otolaryngol Jpn. 1957;60:994. [Google Scholar]