Abstract
To ascertain residual sonographic and histopathological findings of clonorchiasis after treatment, the present study evaluated sonographic findings in rabbits which were infected with 500 metacercariae of C. sinensis every 6 months for 18 months after treatment with praziquantel. The sonographic findings were analyzed in terms of intrahepatic bile duct dilatation and periductal echogenicity, and histopathological findings were observed after the last sonographic examination. Compared with the sonographic findings before treatment, dilatation of the intrahepatic bile ducts became mild to some degree in four of the seven cases and increased periductal echogenicity resolved in four of them. The histopathological specimens after 18 months showed that periductal inflammation has almost resolved but moderate dilatation of the intrahepatic ducts and mucosal hyperplasia persisted. The periductal fibrosis minimally resolved. The long-lasting sonographic findings in cured clonorchiasis make sonography less specific.
Keywords: Clonorchis sinensis, rabbits, treatment, sonography, pathology
INTRODUCTION
Clonorchis sinensis is an important widely-distributed human parasite in East Asia, and it is the most prevalent parasitic helminth in Korea (Rim, 1986; MHW and KAH, 1997). It mainly involves the intrahepatic bile ducts and sometimes extrahepatic biliary tree including the gallbladder.
The clonorchiasis is principally diagnosed by detection of eggs in the feces (Rim, 1986; Chen et al., 1994). Among other diagnostic tools such as skin test, ELISA and some radiologic techniques, sonographic examination is known to be most effective and feasible. Clonorchiasis is commonly diagnosed during sonographic screening of the abdomen for other purposes. The characteristic finding of diffuse dilatation of intrahepatic bile ducts (IHDD) with increased wall echogenicity on sonograms well reflects the pathology of clonorchiasis (Lim et al., 1989; Rhu et al., 1993; Hong et al., 1994).
A recent study reported that sonographic examination showed low sensitivity and low specificity in diagnosis of clonorchiasis in the field (Hong et al., 1998). The study mentioned low sensitivity of sonography due to low infection intensity and low specificity due to residual pathology after cure. Some cured cases were found to be positive by sonography even after 2 years. Some literature suggested that dilated bile ducts could not been completely decompressed after praziquantel treatment in rabbits, which are a good experimental host for C. sinensis (Lee et al., 1987, 1988; Hong et al., 1990, 1994).
The present study consecutively followed the sonographic findings up to 18 months after treatment in rabbit clonorchiasis in order to evaluate sonographic diagnosis after cure.
MATERIALS AND METHODS
C. sinensis infection of rabbits
The freshwater fish, Pseudorasbora parva collected at the Nakdonggang (River), were digested in pepsin solution, and the metacercariae of C. sinensis were isolated under a stereomicroscope. Thirteen New Zealand white rabbits, 2 months old, were infected with 500 metacercariae into the stomach through a tube. They were kept in the animal laboratory and fed with commercial pellets and piped water. All rabbits were treated with praziquantel (Distocide®, Shinpoong Pharmaceutical Co., Seoul, Korea) 100 mg/kg for three days, 10 weeks after infection. If C. sinensis eggs were found in feces, the treatment had been done repeatedly. Five of the 13 rabbits died during the experiment and one of the remaining rabbits was not cured by 18 months after treatment. Therefore, 10 rabbits were subjected at 6 months and 7 were finally subjected at 18 months after treatment.
Sonographic examination
The rabbits were prepared for sonography by anesthesia with intramuscular injection of Ketamine HCl (Ketalar®, 10 mg/ml, Yuhan Co., Seoul, Korea) 5 mg/kg and Xylazine HCl (Rompun, 2%, Bayer Korea, Seoul, Korea) 0.1 ml/kg. They were shaved on the upper abdomen and dressed with jelly. An experienced abdominal radiologist obtained sonograms of the liver with 4-7 or 5-10 MHz linear probes on high-resolution ultrasound scanner (ATL, HDI 3000, USA). Sonographic examination was performed before infection and at nine weeks after infection, and at 6, 12 and 18 months post-treatment.
Histopathological examination
After the last sonographic examination, the rabbits were sacrificed by ether anesthesia and bleeding by heart puncture at 18 months after treatment. Their livers were removed and separated of the lobes, and were fixed in Carnoy fixative. Lobes of the livers were sliced at the proximal and distal sites. They were prepared for paraffin embedding and stained with hematoxylin-eosin. An experienced parasitologist assessed the degrees of IHDD, mucosal hyperplasia, periductal fibrosis and periductal inflammation. They were evaluated on a semi-quantitative scale of mild, moderate and severe degree.
Fecal examination
Just before treatment, fecal specimens of the rabbits were microscopically examined for counting the eggs of C. sinensis by Stoll's method. Also their fecal specimens were examined 2 weeks after treatment to confirm cure of clonorchiasis.
RESULTS
Sonographic examination before the infection showed no peripheral intrahepatic bile ducts of the rabbits, but the examination at 9 weeks after infection showed many peripheral intrahepatic bile ducts in all of the subjected rabbits (Fig. 1; Table 1). The dilated intrahepatic bile ducts (IHDD) were larger (+++) than or similar (++) to the adjacent portal veins in 9 cases. Mild (+) degree of IHDD was observed in only one rabbit, which had the lowest EPG (number of eggs per gram offeces). Six of the 10 rabbits showed the increased echogenicity of the ductal walls and coarse periductal hepatic echogenicity (Fig. 1).
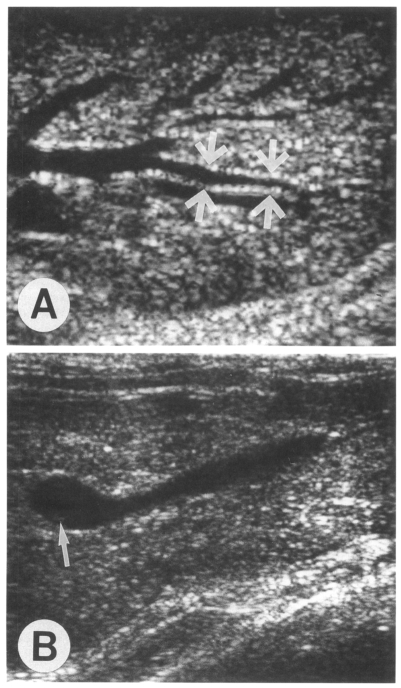
Fig. 1.
Sonograms of a rabbit (ID, 500-1) 9 weeks after infection with 500 metacercariae of Clonorchis sinensis. A. Transverse scan of the left hepatic lobe shows severe dilatation of the intrahepatic ducts (arrows). Note the hyperechoic bands along the duct wall, representing periductal fibrosis. B. Oblique scan of the gallbladder shows a few small echogenic foci (arrow) possibly indicating worms or desquamated materials.
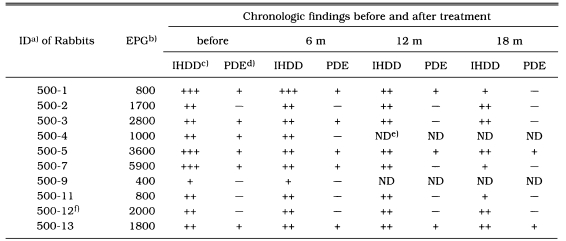
Table 1.
Sonographic findings of Clonorchis sinensis infected rabbits before and after treatment
a)identification number of the rabbits infected with 500 metacercariae; b)numbers of eggs per gram of feces before treatment; c)intrahepatic bile duct dilatation, +++ for larger ducts than adjacent portal vein, ++ for similar ducts with adjacent portal vein, + for smaller ducts than adjacent portal vein, - for normal sized distal ducts; d)periductal echogenicity, + for increased echogenicity, - for normal echogenicity; e)not done; f)the rabbit not cured at 18 months after treatment.
At 6 months after treatment, follow-up sonograms revealed that 2 of the 3 rabbits with severe IHDD changed to moderate IHDD. The degrees of IHDD have persisted in the remaining 8 rabbits. The increased periductal echogenicity resolved in only one of 6 positive rabbits.
At 12 months after treatment, follow-up sonogram was not performed in 2 rabbits because they had died. Compared with results at 6 months after treatment, all of 8 rabbits still showed moderate degree of IHDD. The increased periductal echogenicity was recovered in 2 of 5 positive rabbits.
The last follow-up sonograms 18 months after treatment revealed that IHDD in 3 of the 8 rabbits became mild from moderate degree in comparison with results at 12 months after treatment. The remaining five still showed moderate IHDD. There was increased periductal echogenicity in 2 rabbits (Fig. 2A).
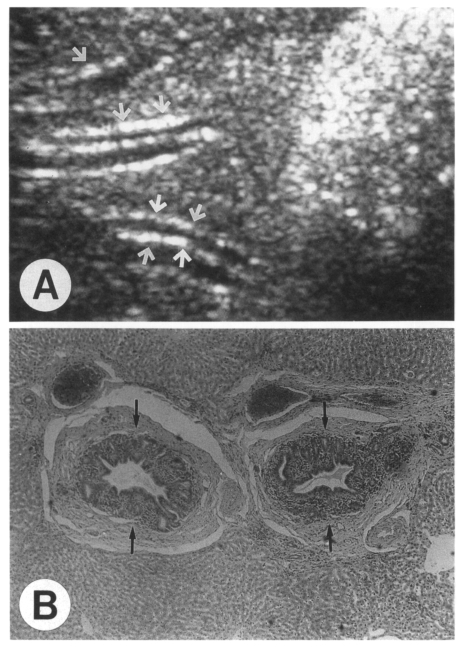
Fig. 2.
A rabbit (ID, 500-5) 18 months after treatment. A. Sonogram still shows moderate dilatation of the peripheral intrahepatic ducts with increased periductal echogenicity (arrows). B. Photomicrograph shows moderately persisted dilatation of the intrahepatic ducts and mucosal hyperplasia (arrows). Also note remaining periductal fibrosis which has been least resolved.
Microscopically, the hematoxylin-eosin stained section of the livers 18 months after treatment disclosed most features of chronic clonorchiasis, i.e., IHDD, mucosal hyperplasia of bile ducts, periductal fibrosis and periductal inflammation. IHDD and mucosal hyperplasia persisted moderately. The periductal fibrosis minimally resolved but periductal inflammation almost resolved (Fig. 2B; Table 2). However, in the liver of one rabbit (ID 500-12), the findings of periductal inflammation and desquamation of duct epithelium were observed, which indicated active inflammation or infection. A few adult flukes were found in the bile ducts.
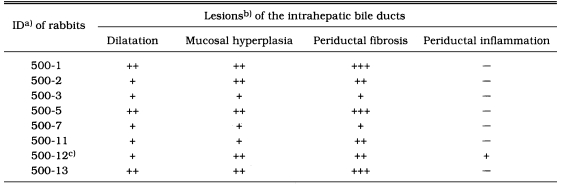
Table 2.
Histopathological findings of Clonorchis sinensis infected rabbits 18 months after treatment
a)identification number of the rabbits infected with 500 metacercariae; b)subjective grading of severity of the lesions, +, mild; ++, moderate; +++, severe; c)the rabbit which was not cured.
DISCUSSION
The present findings of persistent IHDD and thickened wall of the bile ducts by 18 months after treatment strongly suggest that the pathological lesion of clonorchiasis may last life-long even after cure. Two previous studies repeatedly reported that the histopathological changes of the intrahepatic bile ducts of experimental animals remained for 12 weeks (Lee et al., 1987) or 22 weeks (Hong et al., 1994) after treatment. These findings could be interpreted that the nature of IHDD, mucosal hyperplasia and periductal fibrosis might be irreversible. However, the remaining histopathological lesion may possibly further resolve quite slowly after 2 years though the resolution is incomplete.
Sonographic examination has been considered as a good radiologic tool for diagnosis of clonorchiasis, particularly in cases with moderate or heavy burden of the worms (Lim et al., 1989; Rhu et al., 1993; Lee et al., 1995). However, there is an important clinical implication that cured cases are continuously diagnosed as being positive as the pathological changes persist after therapy for substantial period of time (Hong et al., 1998).
The present sonographic results presented that IHDD became mild to some degree after cure in 4 of the 7 rabbits. Also the findings of increased periductal echogenicity resolved in 4 of the 6 rabbits. These results coincide well with the clinical experiences that the findings of some patients with clonorchiasis have resolved on follow-up sonography a few years later.
According to the present histopathological results, periductal fibrosis has persisted or minimally resolved. Hong et al. (1990) presumed that the persisting periductal-fibrosis was caused by resistance to resorption of collagen fibers and lasted long after treatment. In the present results, one rabbit was not cured and showed active inflammation, hyperplasia and desquamation of the duct epithelium. Although no egg was detected in feces of the rabbit, the treatment must have been insufficient, and thus it was excluded for final analysis.
The recovery of pathological changes greatly depends upon duration and burden of infection. There was a report that the rabbits which had been treated earlier than four weeks after infection did not have the residual pathology (Lee et al., 1987). However, it is clinically impossible to diagnose such an early clonorchiasis, because the eggs are usually found in feces from one month after infection (Rim, 1986; Lee et al., 1987).
The long-lasting lesion of the bile ducts in the liver is directly visualized through sonography in the present study. A field study on human clonorchiasis observed persistent sonographic evidence of dilatation of intrahepatic bile ducts for 2 years after cure in half of the subjected population (Hong et al., 1998). The study presented that the sonography showed some false negative as well as many false positive cases. Only 12 of 23 egg positive cases and 49 of 100 egg negative cases were sonographically positive at an endemic area while 20 of 64 egg negative cases at a non-endemic area were found positive. The study also proposed the possibility of some other conditions for visualization of intrahepatic bile ducts in humans. In the present study, no rabbits were found positive by sonography unless they were infected by C. sinensis. It is a topic of further study to specifically differentiate clonorchiasis from other biliary disease conditions by sonographic examination. Another sonographic study commented low sensitivity of sonography but its specificity was rather high as 95% (Lee et al., 1995).
Another experimental study on sonography of rabbit clonorchiasis, which was simultaneously executed by the present authors, revealed very good sensitivity of sonography for diagnosis of clonorchiasis (unpublished data). According to the study, the infection as early as 3 weeks was detected by sonography in a rabbit infected with 5 worms. Also the bile duct of a rabbit infected by only 2 worms was visualized by sonography 4 weeks after infection. According to the experiment, sonography can demonstrate early minimal change of the infected bile ducts of rabbits.
The diagnostic sensitivity by sonography greatly depends upon the burden of infected worms and their location in the liver. It is known that C. sinensis is randomly distributed in the liver (Hong et al., 1993). The worms may invade any branch of the intrahepatic bile ducts and be scattered in the liver. Since sonography scans the liver from the abdomen, a minimal change in the liver at the backside or under the diaphragm may be missed. Sonographic detection of the bile ducts infected by only a few worms may be more difficult in human than in rabbits because the human liver is much larger than that of rabbits. In this context, the false negative cases by sonography of Hong et al. (1998) can be explained as that most of them might have been lightly infected as EPG less than 100, which is estimated less than 5 flukes. Practically it is quite plausible that most of the lightly infected cases with one or two worms may be missed by sonography.
In conclusion, since mucosal hyperplasia, bile duct dilatation and periductal fibrosis persist as long as 18 months after treatment, sonographic visualization of the intrahepatic bile ducts may persist after cure of clonorchiasis.
Footnotes
This study was supported by a grant No. 01-96-068 from Seoul National University Hospital research fund (1996).
References
- 1.Chen M, Lu Y, Hua X, Mott KE. Progress in assessment of morbidity due to Clonorchis sinensis infecton: a review of recent literature. Trop Dis Bull. 1994;91(3):R7–R65. [Google Scholar]
- 2.Hong ST, Huh S, Kho WG, et al. Changes in histopathological and serological findings of the liver after treatment in rabbit clonorchiasis. Seoul J Med. 1990;31(2):117–127. [Google Scholar]
- 3.Hong ST, Kho WG, Kim WH, Chai JY, Lee SH. Turnover of biliary epithelial cells in Clonorchis sinensis infected rats. Korean J Parasitol. 1993;31(2):83–89. doi: 10.3347/kjp.1993.31.2.83. [DOI] [PubMed] [Google Scholar]
- 4.Hong ST, Park KH, Seo M, Choi BI, Chai JY, Lee SH. Correlation of sonographic findings with histopathological changes of the bile ducts in rabbits infected with Clonorchis sinensis. Korean J Parasitol. 1994;32(4):223–230. doi: 10.3347/kjp.1994.32.4.223. [DOI] [PubMed] [Google Scholar]
- 5.Hong ST, Yoon K, Lee M, et al. Control of clonorchiasis by repeated praziquantel treatment and low diagnostic efficacy ofsonography. Korean J Parasitol. 1998;36(4):249–254. doi: 10.3347/kjp.1998.36.4.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hou PC. The pathology of Clonorchis sinensis infestation of the liver. J Pathol Bacteriol. 1955;70:53–64. doi: 10.1002/path.1700700106. [DOI] [PubMed] [Google Scholar]
- 7.Lee HK. Evaluation of sonography and skin test in diagnosis of clonorchiasis at the Hyongsan-gang (River) area. Korean J Parasitol. 1995;33(2):117–123. doi: 10.3347/kjp.1995.33.2.117. [DOI] [PubMed] [Google Scholar]
- 8.Lee SH, Chai JY, Yang EC, Yun CK, Hong ST, Lee JB. Observation of liver pathology after praziquantel treatment in experimental Clonorchis sinensis infection in guniea pig. Seoul J Med. 1988;29(3):253–262. [Google Scholar]
- 9.Lee SH, Hong ST, Kim CS, Sohn WM, Chai JY, Lee YS. Histopathological changes of the liver after praziquantel treatment in Clonorchis sinensis infected rabbits. Korean J Parasitol. 1987;25(2):110–122. doi: 10.3347/kjp.1987.25.2.110. [DOI] [PubMed] [Google Scholar]
- 10.Lee SH, Lee JI, Huh S, et al. Secretions of the biliary mucosa in experimental clonorchiasis. Korean J Parasitol. 1993;31(1):13–20. doi: 10.3347/kjp.1993.31.1.13. [DOI] [PubMed] [Google Scholar]
- 11.Lee SH, Shim TS, Lee SM, Chi JG. Studies on pathological changes of the liver in albino rats infected with Clonorchis sinensis. Korean J Parasitol. 1978;16(2):148–155. doi: 10.3347/kjp.1978.16.2.148. [DOI] [PubMed] [Google Scholar]
- 12.Lim JH, Ko YT, Lee DH, Kim SY. Clonorchiasis: sonographic findings in 59 proved cases. Am J Roentgenol. 1989;152(4):761–764. doi: 10.2214/ajr.152.4.761. [DOI] [PubMed] [Google Scholar]
- 13.Ministry of Health and Welfare; Korean Association of Health. Prevalence of intestinal parasitic infections in Korea - The Sixth Report. Seoul, Korea: 1997. [Google Scholar]
- 14.Rhu KN, Lim JH, Cho YJ, Yang MH. Comparative study of radiologic-pathologic findings of experimental clonorchiasis in rabbits. J Korean Radiol Soc. 1993;29(1):1–8. [Google Scholar]
- 15.Rim HJ. The current pathobiology and chemotherapy of clonorchiasis. Korean J Parasitol. 1986;24(suppl.):3–141. doi: 10.3347/kjp.1986.24.suppl.1. [DOI] [PubMed] [Google Scholar]