Abstract
Background: MET amplification has been detected in ∼20% of non-small-cell lung cancer patients (NSCLC) with epidermal growth factor receptor (EGFR) mutations progressing after an initial response to tyrosine kinase inhibitor (TKI) therapy.
Patients and methods: We analyzed MET gene copy number using FISH in two related NSCLC cell lines, one sensitive (HCC827) and one resistant (HCC827 GR6) to gefitinib therapy and in two different NSCLC patient populations: 24 never smokers or EGFR FISH-positive patients treated with gefitinib (ONCOBELL cohort) and 182 surgically resected NSCLC not exposed to anti-EGFR agents.
Results: HCC827 GR6-resistant cell line displayed MET amplification, with a mean MET copy number >12, while sensitive HCC827 cell line had a mean MET copy number of 4. In the ONCOBELL cohort, no patient had gene amplification and MET gene copy number was not associated with outcome to gefitinib therapy. Among the surgically resected patients, MET was amplified in 12 cases (7.3%) and only four (2.4%) had a higher MET copy number than the resistant HCC827 GR6 cell line.
Conclusions: MET gene amplification is a rare event in patients with advanced NSCLC. The development of anti-MET therapeutic strategies should be focused on patients with acquired EGFR-TKI resistance.
Keywords: EGFR, gefitinib, MET, non-small cell lung cancer, tyrosine kinase inhibitor
introduction
During the last years, improvements in the knowledge of cancer biology led to identification of new agents active against non-small-cell lung cancer (NSCLC). Drugs targeting the tyrosine kinase domain of the epidermal growth factor receptor-tyrosine kinase inhibitor (EGFR-TKI), such as gefitinib (ZD 1839, Iressa®, AstraZeneca, Macclesfield, UK) and erlotinib (OSI 774, Tarceva®, Genentech, South San Francisco, CA, USA), demonstrated to induce dramatic and durable responses in NSCLC patients harboring activating EGFR gene mutations [1] and increased EGFR gene copy number [2–5].
Unfortunately, ∼20% to 50% of patients with clinical or biological predictors for EGFR-TKI sensitivity are resistant to the drug (primary or de novo resistance) and although the majority initially shows a good clinical response, drug resistance invariably occurs and disease progresses (acquired resistance). Potential mechanisms involved in primary resistance to EGFR-TKIs have been explored in preclinical models [6–8] or, retrospectively, in cohorts of patients unselected for clinical or biological characteristics [9, 10]. However, none of them can account for the majority of resistant cases. For instance, presence of KRAS mutation was significantly associated with lack of response to EGFR-TKIs, but this biological event generally occurs in patients without EGFR mutations [10, 11] and only in 30% of adenocarcinomas.
A secondary EGFR gene mutation (T790M) was found in ∼50% of patients relapsing after an initial response [12] and, more recently, another secondary mutation (D761Y) was found in a brain metastasis of a lung cancer patient initially responsive to gefitinib [13]. Two recent studies revealed amplification of MET oncogene in ∼20% of patients with acquired resistance [14, 15]. MET is the receptor for hepatocyte growth factor overexpressed in various cancers, including NSCLC [16–20]. A somatic mutation in the MET gene has been identified in lung cancer, resulting in a deletion in the juxtamembrane domain and stimulation of MET transforming activity in vitro [21]. Several studies described MET gene amplification in up to 10% of gastric cancers [22–24] and in 4% of esophageal and lung cancers [25, 26]. In addition to proliferative and antiapoptotic activities that are common to many growth factors, MET activation demonstrated to stimulate cell–cell detachment, migration, and invasiveness [27]. Preclinical findings suggested that lung cancer cell lines harboring MET gene amplification are dependent on MET for growth and survival [28]. Engelman et al. [14] reported that NSCLC overcomes inhibition of EGFR-TKIs by amplifying the MET oncogene to activate HER3, a member of the EGFR family, and the PI3K-AKT cell survival pathway. That study represented the first report of HER3 activation through a kinase other than a receptor of the EGFR family and of a genetic alteration not involving EGFR that is associated with EGFR-TKI acquired resistance in humans. In another study, Bean et al. [15] showed MET amplification in 21% of patients with acquired resistance to gefitinib or erlotinib and only in 3% of untreated patients, confirming that MET could be a relevant therapeutic target for some individuals with acquired resistance to EGFR-TKIs.
Whether MET amplification is a phenomenon occurring only under therapeutic pressure or also plays a role in de novo resistance to EGFR-TKIs is unknown. Moreover, the incidence of MET amplification in patients with biological predictors for EGFR-TKI sensitivity has not been previously examined. In the present study, we investigated whether MET gene copy number was associated with primary resistance to gefitinib therapy and whether such event occurs in EGFR FISH-positive patients.
patients and methods
patients
The present study has been conducted in primary NSCLC from two cohorts: one with individuals with high chance to respond to EGFR-TKI and treated with gefitinib for advanced, metastatic disease (ONCOBELL cohort) and another with surgically resected patients not exposed to anti-EGFR agents (Humanitas cohort). The ONCOBELL trial was a prospective phase II study evaluating gefitinib sensitivity in never smokers or EGFR FISH and phospho-Akt-positive NSCLC that enrolled 42 patients and has all characteristics previously described [5]. For this study, tumor specimen collected before gefinitib therapy was available from 24 patients. Written informed consent was obtained from each patient before entering the study.
The Humanitas cohort included 182 NSCLC patients with pathologically confirmed stage III or IV who underwent radical surgery at the Istituto Clinico Humanitas in Rozzano (Italy) during the period 2000–2003. Paraffin-embedded tumor specimens were used to construct a tissue microarray (TMA) with 600 μm cores. An adhesive-coated tape system (Instrumedics, Hackensack, NJ) was used for sectioning the tumor array blocks at 4 μm.
The study was approved by the local Ethics Committee and was conducted in accordance with ethical principles stated in the most recent version of the Declaration of Helsinki or the applicable guidelines on good clinical practice, whichever represented the greater protection of the individuals.
FISH analysis
Unstained 4-μm sections from the TMA or tumor biopsies or resections were submitted to a dual-color FISH assay using a MET/CEP7 probe cocktail prepared with the in-house developed MET DNA (RP 11-95I20 BAC clone) labeled with SpectrumRed and the SpectrumGreen CEP7 (Abbott Molecular). The FISH assays were carried out according to protocol previously described [4], including pretreatment with 2× SSC at 75°C and digestion with Proteinase K for 7–15 min each, codenaturation at 85oC for 15 min, hybridization for ∼36 h, and rapid posthybridization washes with 2× SCC/0.4 NP40. Signals were enumerated in at least 50 tumor nuclei per specimen, using epifluorescence microscope with single-interference filter sets for green (FITC), red (Texas red), and blue (DAPI) as well as dual (red/green) and triple (blue, red, green) band pass filters. For each specimen, the mean and standard deviation of copy number per cell of each tested DNA sequence, the percentage of cells with less than two or two, three, and four or more copies of the MET gene, and the ratio MET/CEP7 were calculated. For documentation, images were captured using a CCD camera and merged using dedicated software (CytoVision, AI, Santa Clara, CA, USA).
NSCLC cell line analysis
Two related NSCLC cell lines were analyzed for genomic status of MET by FISH using the probe set described above and protocol described elsewhere [4]. The EGFR mutant HCC827 cell line (del E746_A750), which has been extensively characterized [14], was obtained from America Type Culture Collection (Manassas, VA). HCC827 GR6 (gefitinib resistant, clone 6) cell line was generated under experimental conditions as previously described [14]. HCC827 has an EGFR exon 19 deletion and gene amplification and is highly sensitive to gefitinib whereas HCC827 GR6 carries similar characteristics for the EGFR gene but has MET amplification and is resistant to gefitinib treatment [14]. Both cell lines were maintained in RPMI 1640 (Cellgro, Mediatech Inc., Herndon, CA) supplemented with 5% FBS, 100 units/ml penicillin, 100 units/ml streptomycin, and 2 mM glutamine.
statistical analyses
The primary end-point was to assess whether MET gene copy number impaired response to gefitinib therapy in an NSCLC population with clinical or biological predictors for EGFR-TKI responsiveness. Differences in response rate and association with clinical characteristics were compared by Fisher's exact test or χ2 test. Time to disease progression (TTP), calculated from the time of first gefitinib dose to time of disease progression or last disease assessment, overall survival (OS), calculated from the time of first gefitinib dose to patient death or last contact, and the 95% confidence intervals were evaluated by survival analysis using Kaplan–Meier method [29]. TTP and OS for the groups with negative and positive biomarkers were compared using the log-rank test. Statistical significance was set at <0.05 for each analysis. Analysis of receiver operating characteristic (ROC) curve was carried out with the aim of determining a cut-off point for MET gene copy number as a continuous variable [30]. All statistical analyses were carried out using SPSS version 11.5.1 (SPSS Italia srl, Bologna, Italy).
results
patient characteristics
All 24 patients from the ONCOBELL cohort included in this study had stage IV disease. As shown in Table 1, these patients were mainly females (70.8%), with adenocarcinoma (75.0%) and never smokers (89.3%). Seventeen patients (70.8%) were EGFR FISH positive (three with gene amplification and 14 with high polysomy) and 15 individuals (62.5%) harboured an EGFR mutation (exon 19 deletion in 11 cases, exon 21 point mutation in one case, and exon 20 insertion in three cases). Two patients harboured a HER2 mutation (exon 20 insertion) and one patient had a KRAS mutation (G12V). In this cohort, response rate was 37.5%, median TTP was 2.6 months, and median OS was 7.4 months.
Table 1.
ONCOBELL cohort: patient characteristics and outcome to gefitinib therapy
| Characteristics | Total | % |
| Evaluated | 24 | 100 |
| Gender | ||
| Male | 7 | 29.2 |
| Female | 17 | 70.8 |
| Median age (year, range) | 60.3 (43.4–80.4) | |
| Histology | ||
| Adenocarcinoma | 18 | 75.0 |
| Squamous cell carcinoma | 1 | 4.2 |
| Undifferentiated carcinoma | 4 | 16.6 |
| Large-cell carcinoma | 1 | 4.2 |
| Smoking history | ||
| Never | 20 | 83.3 |
| Former | 4 | 16.7 |
| EGFR FISH status | ||
| Positive | 17 | 70.8 |
| Negative | 7 | 29.2 |
| EGFR mutation status | ||
| EGFR mutated | 15 | 62.5 |
| EGFR wild type | 9 | 37.5 |
| Response to gefitinib therapy | ||
| Partial response | 9 | 37.5 |
| Stable disease | 1 | 4.2 |
| Progressive disease | 14 | 58.3 |
| Time to disease progression (months) | 2.6 | |
| Median survival (months) | 7.4 |
The table reports the characteristics of 24 patients selected among participating to the ONCOBELL study. The only criterion used for patient selection was availability of tumor tissue from primary lung cancer.
EGFR, epidermal growth factor receptor.
The 182 patients from the Humanitas cohort included NSCLCs with pathologically confirmed stage III (85.1%) or stage IV (14.9%) disease. As shown in Table 2, the majority of these patients were males (80.7%), former or current smokers (86.8%), and had adenocarcinoma with or without bronchioloalveolar features (53.2%).
Table 2.
Humanitas cohort: patient characteristics
| Total no. | % | |
| Total evaluated | 182 | 100 |
| Gender | ||
| Male | 147 | 80.7 |
| Female | 35 | 19.3 |
| Histology | ||
| Adenocarcinoma ± BAC | 97 | 53.2 |
| Squamous cell carcinoma | 46 | 25.3 |
| Other | 39 | 21.5 |
| Smoking history | ||
| Never | 17 | 9.3 |
| Former | 98 | 53.8 |
| Current | 60 | 33.0 |
| Unknown | 7 | 3.9 |
| Pathological stage | ||
| III | 155 | 85.1 |
| IV | 27 | 14.9 |
| EGFR status: total evaluable | 156 | |
| FISH positive | 76 | 48.7 |
| FISH negative | 80 | 51.3 |
The table reports the clinical characteristics of 182 NSCLC patients who underwent radical surgery. Patients with metastatic disease received surgery following or at the same time of single brain or lung lesion removal.
EGFR, epidermal growth factor receptor.
MET FISH results
NSCLC cell lines.
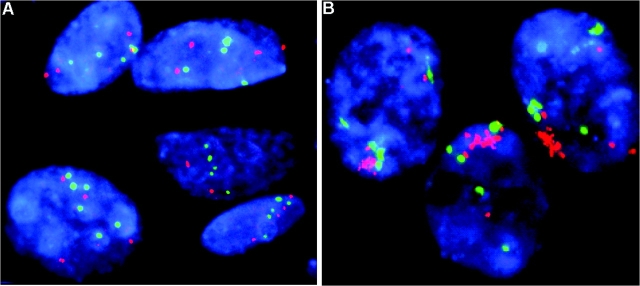
Figure 1 shows MET gene status in the two NSCLC cell lines analyzed. In the gefitinib-sensitive HCC827 cell line, the mean MET copy number was 4 (Figure 1A). The gefitinib-resistant HCC827 GR6 cell line displayed a clustered gene amplification in all nuclei, and the mean MET gene copy number was >12 (Figure 1B).
Figure 1.
Hybridization of MET/CEP7 probe set with specimens HCC827 (A) and HCC827 GR6 (B). On average four copies of MET signals (red) per cell were found in HCC827 while large clusters of MET signals were detected in all HCC827 GR6 nuclei.
ONCOBELL cohort (N = 24).
In this cohort, mean MET gene copy number per tumor nuclei ranged from 1.7 to 6.10, with a median value of 2.91 and no patient had true gene amplification as defined with criteria previously reported [31]. No patient had MET copy number equal or greater than the gefitinib-resistant EGFR mutant HCC827 GR6 cell line, and seven patients (29.1%), including three gefitinib responders, had a mean MET gene copy number higher than the sensitive HCC827 sensitive cell line. Among these seven patients, only two had a mean five or more copies per cell (mean 6.0 and 6.1), one EGFR FISH+/EGFR mutant and one EGFR FISH+/EGFR wild type and both responded to gefitinib therapy.
Data were further analyzed using a ROC curve and the area under the curve was 0.46, which was not satisfactory for discriminating responders versus resistant patients. Therefore, we decided to analyze the data using the median MET gene copy number value as cut-off for discriminating a high-copy number subset (mean ≥ 2.91) versus a low copy number subset (mean < 2.91), see Figure 2. As shown in Table 3, MET gene status was not associated to any clinical or biological characteristic. No difference in response rate (33.3% versus 41.7%, P = 1.0), TTP (2.6 versus 2.2 months, P = 0.6), and survival (18.7 versus 5.4 months, P = 0.15) was observed between MET FISH high-copy and low-copy carrier (Table 3). Among 19 EGFR FISH+ or EGFR mutation+ patients, 10 have not responded to gefitinib therapy and nine had a partial response. As shown in Table 4, no difference in response, TTP, and OS was observed according to MET gene copy number.
Figure 2.

In the ONCOBELL cohort, the median MET mean gene copy number per cell was 2.91. Time to disease progression was 2.6 months in patients with mean MET gene copy number ≥2.91 (MET high copy number) and 2.2 months in individuals with mean MET gene copy number <2.91 (MET low copy number). This difference was not statistically significant (P = 0.6). Median survival was 18.7 months in patients with mean MET gene copy number ≥2.91 and 5.2 months in individuals with mean MET gene copy number <2.91. The difference was not statistically significant (P = 0.15).
Table 3.
ONCOBELL cohort: association of MET gene copy number with patient characteristics and outcome to gefitinib therapy
| N (%) | MET high copy ≥2.91 (%) | MET low copy <2.91 (%) | P value | |
| Total | 24 (100) | 12 | 12 | |
| Gender | ||||
| Male | 7 (29.2) | 3 (25.0) | 4 (33.3) | 1.0 |
| Female | 17 (70.8) | 9 (75.0) | 8 (66.7) | |
| Smoking history | ||||
| Never | 20 (83.3) | 9 (75.0) | 11 (91.7) | 0.6 |
| Former | 4 (16.7) | 3 (25.0) | 1 (8.3) | |
| Histology | ||||
| Adenocarcinoma | 18 (75.0) | 9 (75.0) | 9 (75.0) | 1.0 |
| Other | 6 (25.0) | 3 (25.0) | 3 (25.0) | |
| EGFR FISH | ||||
| Positive | 17 (83.4) | 10 (83.3) | 7 (58.4) | 0.3 |
| Negative | 7 (16.6) | 2 (16.7) | 5 (41.6) | |
| EGFR mutation | ||||
| Positive | 15 (62.5) | 7 (58.4) | 8 (66.7) | 0.6 |
| Negative | 9 (37.5) | 5 (41.6) | 4 (33.3) | |
| Response to gefitinib therapy | ||||
| Partial response | 9 (37.5) | 4 (33.3) | 5 (41.6) | 0.6 |
| Stable + progressive disease | 15 (62.5) | 8 (66.7) | 7 (58.4) | |
| Time to progression (months) | 2.6 | 2.6 | 2.2 | 0.6 |
| Overall survival (months) | 7.4 | 18.7 | 5.2 | 0.15 |
The table reports the association of clinical characteristics of the 24 patients selected among participating to the ONCOBELL trial with MET gene copy number. The median MET mean gene copy number (2.91) was chosen as cut-off value. This cut-off was not able to discriminate sensitive versus resistant gefitinib treated patients.
EGFR, epidermal growth factor receptor.
Table 4.
ONCOBELL cohort: outcome of EGFR positive (FISH and/or mutation) patients according to MET gene copy number
| EGFR+ | MET ≥2.91 | MET <2.91 | P value | |
| Total | 19 | 11 | 8 | |
| Response rate (N/%) | 9/47.4 | 4/36.3 | 5/62.5 | 0.25 |
| Time to progression (months) | 3.7 | 3.9 | 3.2 | 0.8 |
| Overall survival (months) | 18.7 | 18.7 | 5.2 | 0.25 |
The table reports response rate, time to progression, and survival of 19 patients included in the ONCOBELL trial EGFR FISH or EGFR mutation positive according to MET mean gene copy number. The median MET mean gene copy number (2.91) was chosen as cut-off value. Also in this particularly selected group of patients, chosen cut-off did not discriminate sensitive versus resistant gefitinib-treated patients.
EGFR, epidermal growth factor receptor.
humanitas cohort (N = 182).
Because of the lack of association of MET gene copy number with gefitinib sensitivity in the ONCOBELL cohort, we extended our analysis to a large population of advanced NSCLC to investigate whether the absence of MET gene amplification was due to the particular characteristics of the ONCOBELL patients or was a general phenomenon in NSCLC. MET was successfully analyzed by FISH in 166 cases. Mean MET gene copy number ranged from 1.3 to 27.5 per tumor nuclei, with a median value of 3.6 per cell. MET gene amplification [31] was observed in 12 cases (7.2%), including four patients (2.4%) with a mean MET copy per cell higher than observed in the resistant HCC827 GR6 cell line. Additional 13 patients (7.8%) displayed high MET copy numbers (mean ≥ 5 copies per cell). MET gene amplification or overrepresentation was not significantly associated with gender (P = 0.7), smoking history (P = 0.7), or histology (P = 0.9). In this cohort of patients, we also evaluated the EGFR status by FISH using methods and scoring criteria previously described [4]. The analysis was successfully carried out in 156 individuals and a positive EGFR FISH result was observed in 48.7% of cases. Among the 76 EGFR FISH-positive patients, nine (11.8%) had MET amplification, including three patients (3.9%) with a mean MET copy number higher than in HCC827 GR6-resistant cell line. Among the 80 EGFR FISH-negative patients, MET gene amplification was observed in three (3.7%) cases, and only one (1.2%) had a MET copy number higher than in HCC827 GR6. The association between MET and EGFR gene copy number was not statistically significant (Pearson P value = 0.2).
discussion
The present study, one of the largest exploring the role of MET gene copy number in NSCLC patients exposed to EGFR-TKIs, has shown that MET FISH analysis carried out in pretreatment tumor biopsies did not identify patients with primary resistance to gefitinib therapy.
Although patients who are never smokers, EGFR mutant or EGFR FISH positive have a high chance to respond to gefitinib or erlotinib [1–5]; it is not uncommon in clinical practice to observe individuals who are refractory to the treatment even when presenting numerous clinical and biological features positively associated with EGFR-TKI sensitivity. In cohorts of patients not selected for biological characteristics, KRAS mutations emerged as the main mechanism involved in primary resistance to EGFR-TKIs [9, 10]. Nevertheless, these mutations generally occur in smokers and in individuals with no EGFR mutation [9–11], clearly suggesting that other biological events are responsible for the lack of EGFR-TKI sensitivity occasionally observed in a potentially sensitive population.
Previous studies showed that MET amplification was responsible for acquired EGFR-TKI resistance in ∼20% of NSCLC [14, 15]. Whether this event is responsible for primary resistance to gefitinib therapy in EGFR-positive (FISH or mutation), KRAS wild-type NSCLC patients is unknown. Therefore, in the present study, in order to investigate additional mechanisms involved in primary resistance, we analyzed MET gene copy number in a patient population with clinical or biological predictors for EGFR-TKI sensitivity. In the ONCOBELL cohort, KRAS, HER2, and EGFR gene status was known, allowing to analyze the impact of MET without the confounding effect of other biological mechanisms potentially responsible for primary resistance [9–11, 32, 33]. Although potentially sensitive to gefitinib therapy, a large percentage of the ONCOBELL patients did not respond to the treatment, and our current findings do not support that genomic gain for MET had a critical role in such clinical outcome, as suggested by the absence of amplification in all analyzed pretreatment specimens.
We further investigated the incidence of MET amplification in NSCLC, in order to assess whether genomic gain of MET sequences represents a rare phenomenon only in an EGFR-TKI potentially sensitive population or is a general event in NSCLC. Because the ONCOBELL cohort included only patients with metastatic disease, and because data on a possible association between MET gene copy number and tumor stage are not available, our analysis was conducted only in patients with advanced stage (stages III–IV). In the humanitas cohort, MET gene amplification was observed in <10% of cases, confirming that such phenomenon is not frequent in NSCLC.
To further interpret the lack of association of MET gene copy number with gefitinib sensitivity, we analyzed MET in two different NSCLC cell lines, one sensitive (HCC827) and one resistant (HCC827 GR6), aiming to explore whether the level of genomic gain in these two cell populations was comparable with the MET status observed in patient cohorts. The gefitinib-sensitive cell line HCC827 had moderate level of MET gene gain, whereas MET gene amplification was detected in the gefitinib-resistant HCC827 GR6. The very high MET copy number per cell (>12 copies) associated with resistance to gefitinib in HCC827 GR6 was comparable to the high level of MET amplification previously described for this cell line [14] and was found in none of the ONCOBELL patients. Recently, two studies investigated the impact of MET gene copy number in patients exposed to gefitinib therapy [34, 35]. In the study carried out by Sequist et al. [34], the only patient with EGFR mutation with MET amplification resistant to gefitinib therapy had an average of 12 MET signals per cell. In the study carried out by Yang et al. [35], among the 39 patients evaluated for MET, only one female patient had a MET copy number >5.5, and she had short time to progression and survival. In the present study, the only two ONCOBELL patients with high MET copy number were both sensitive to gefitinib and had a mean of 6 copies of MET gene per cell, considerably below the level observed in the HCC827 GR6 cell line and in the Sequist experience [34]. Although 7.3% of patients in the Humanitas cohort had MET amplification, only four patients (2.4%) had a level of gene amplification higher than in the HCC827 GR6 cell line. Importantly, MET gene copy number was not associated with EGFR FISH status and a level of MET amplification higher than in the HCC827 GR6 cell line was observed only in 3.9% of EGFR FISH-positive individuals. On the basis of these findings, it is possible to hypothesize that high level of MET amplification, known to be associated with gefitinib resistance in vitro, rarely occurs in untreated NSCLC irrespective of EGFR status and it may develop only under therapeutic pressure, leading to the conclusion that, in EGFR-TKI-naive patients, the level of genomic gain for MET is not increased enough to impact response to TKIs. This finding has clinical implications since support that anti-MET strategies should be focused on EGFR-TKI-resistant patients, where MET gene gain is more frequently observed and can drive tumor resistance [14].
In conclusion, this study showed that MET gene amplification is a rare event in advanced NSCLC, particularly at the high levels observed in a cell line-resistant model. Our results suggest that MET inhibitors currently under investigation in clinical trials may be effective only in a small percentage of NSCLC and should be investigated in patients with acquired resistance to EGFR-TKIs.
funding
Italian Association for Cancer Research to FC; US National Institute of Health 1R01CA114465-01 to PAJ.
Acknowledgments
The authors acknowledge the technical assistance of the Cytogenetics Core of the University of Colorado Cancer Center for all FISH analyses.
References
- 1.Paez JG, Janne PA, Lee JC, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 2004;304:1497–1500. doi: 10.1126/science.1099314. [DOI] [PubMed] [Google Scholar]
- 2.Tsao MS, Sakurada A, Cutz JC, et al. Erlotinib in lung cancer molecular and clinical predictors of outcome. N Engl J Med. 2005;353:133–144. doi: 10.1056/NEJMoa050736. [DOI] [PubMed] [Google Scholar]
- 3.Hirsch FR, Varella-Garcia M, Bunn PA, Jr, et al. Molecular predictors of outcome with gefitinib in a phase III placebo-controlled study in advanced non-small-cell lung cancer. J Clin Oncol. 2006;24:5034–5042. doi: 10.1200/JCO.2006.06.3958. [DOI] [PubMed] [Google Scholar]
- 4.Cappuzzo F, Hirsch FR, Rossi E, et al. Epidermal growth factor receptor gene and protein and gefitinib sensitivity in non-small cell lung cancer. J Natl Cancer Inst. 2005;97:643–655. doi: 10.1093/jnci/dji112. [DOI] [PubMed] [Google Scholar]
- 5.Cappuzzo F, Ligorio C, Janne PA, et al. Prospective study of gefitinib in EGFR FISH positive/P-Akt positive or never smoker patients with advanced non-small cell lung cancer (NSCLC): the ONCOBELL trial. J Clin Oncol. 2007;25:2248–2255. doi: 10.1200/JCO.2006.09.4300. [DOI] [PubMed] [Google Scholar]
- 6.She QB, Solit D, Basso A, et al. Resistance to gefitinib in PTEN-null HER-overexpressing tumor cells can be overcome through restoration of PTEN function or pharmacologic modulation of constitutive phosphatidylinositol 3′-kinase/Akt pathway signaling. Clin Cancer Res. 2003;9:4340–4346. [PubMed] [Google Scholar]
- 7.Bianco R, Shin I, Ritter CA, et al. Loss of PTEN/MMAC1/TEP in EGF receptor-expressing tumor cells counteracts the antitumor action of EGFR tyrosine kinase inhibitors. Oncogene. 2003;22:2812–2822. doi: 10.1038/sj.onc.1206388. [DOI] [PubMed] [Google Scholar]
- 8.Chakravarti A, Loeffler JS, Dyson NJ. Insulin-like growth factor receptor I mediates resistance to anti-epidermal growth factor receptor therapy in primary human glioblastoma cells through continued activation of phosphoinositide 3-kinase signaling. Cancer Res. 2002;62:200–207. [PubMed] [Google Scholar]
- 9.Pao W, Wang TY, Riely GJ, et al. KRAS mutations and primary resistance of lung adenocarcinomas to gefitinib or erlotinib. PLoS Med. 2005;2:e17. doi: 10.1371/journal.pmed.0020017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Massarelli E, Varella-Garcia M, Tang X, et al. Kras mutation is an important predictor of resistance to therapy with epidermal growth factor receptor tyrosine kinase inhibitors in patients with non-small cell lung cancer. Clin Cancer Res. 2007;13:2890–2896. doi: 10.1158/1078-0432.CCR-06-3043. [DOI] [PubMed] [Google Scholar]
- 11.Shigematsu H, Lin L, Takahashi T, et al. Clinical and biological features associated with epidermal growth factor receptor gene mutations in lung cancers. J Natl Cancer Inst. 2005;97:339–346. doi: 10.1093/jnci/dji055. [DOI] [PubMed] [Google Scholar]
- 12.Kobayashi S, Boggon TJ, Dayaram T, et al. EGFR mutation and resistance of non-small-cell lung cancer to gefitinib. N Engl J Med. 2005;352:786–792. doi: 10.1056/NEJMoa044238. [DOI] [PubMed] [Google Scholar]
- 13.Balak MN, Gong Y, Riely GJ, et al. Novel D761Y and common secondary T790M mutations in epidermal growth factor receptor-mutant lung adenocarcinomas with acquired resistance to kinase inhibitors. Clin Cancer Res. 2006;12:6494–6501. doi: 10.1158/1078-0432.CCR-06-1570. [DOI] [PubMed] [Google Scholar]
- 14.Engelman JA, Zejnullahu K, Mitsudomi T, et al. MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science. 2007;316:1039–1043. doi: 10.1126/science.1141478. [DOI] [PubMed] [Google Scholar]
- 15.Bean J, Brennan C, Shih JY, et al. MET amplification occurs with or without T790M mutations in EGFR mutant lung tumors with acquired resistance to gefitinib or erlotinib. Proc Natl Acad Sci USA. 2007;104:20932–20937. doi: 10.1073/pnas.0710370104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ma PC, Maulik G, Christensen J, et al. c-Met: structure, functions and potential for therapeutic inhibition. Cancer Metastasis Rev. 2003;22:309–325. doi: 10.1023/a:1023768811842. [DOI] [PubMed] [Google Scholar]
- 17.Christensen JG, Burrows J, Salgia R. c-Met as a target for human cancer and characterization of inhibitors for therapeutic intervention. Cancer Lett. 2005;225:1–26. doi: 10.1016/j.canlet.2004.09.044. [DOI] [PubMed] [Google Scholar]
- 18.Ichimura E, Maeshima A, Nakajima T, et al. Expression of c-met/HGF receptor in human non-small cell lung carcinomas in vitro and in vivo and its prognostic significance. Jpn J Cancer Res. 1996;87:1063–1069. doi: 10.1111/j.1349-7006.1996.tb03111.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tsao MS, Liu N, Chen JR, et al. Differential expression of Met/hepatocyte growth factor receptor in subtypes of non-small cell lung cancers. Lung Cancer. 1998;20:1–16. doi: 10.1016/s0169-5002(98)00007-5. [DOI] [PubMed] [Google Scholar]
- 20.Masuya D, Huang C, Liu D, et al. The tumour–stromal interaction between intratumoral c-Met and stromal hepatocyte growth factor associated with tumour growth and prognosis in non-small-cell lung cancer patients. Br J Cancer. 2004;90:1555–1562. doi: 10.1038/sj.bjc.6601718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kong-Beltran M, Seshagiri S, Zha J, et al. Somatic mutations lead to an oncogenic deletion of met in lung cancer. Cancer Res. 2006;66:283–289. doi: 10.1158/0008-5472.CAN-05-2749. [DOI] [PubMed] [Google Scholar]
- 22.Kuniyasu H, Yasui W, Kitadai Y, et al. Frequent amplification of the c-met gene in scirrhous type stomach cancer. Biochem Biophys Res Commun. 1992;189:227–232. doi: 10.1016/0006-291x(92)91548-5. [DOI] [PubMed] [Google Scholar]
- 23.Tsujimoto H, Sugihara H, Hagiwara A, et al. Amplification of growth factor receptor genes and DNA ploidy pattern in the progression of gastric cancer. Virchows Arch. 1997;431:383–389. doi: 10.1007/s004280050115. [DOI] [PubMed] [Google Scholar]
- 24.Hara T, Ooi A, Kobayashi M, et al. Amplification of c-myc, K-sam, and c-met in gastric cancers: detection by fluorescence in situ hybridization. Lab Invest. 1998;78:1143–1153. [PubMed] [Google Scholar]
- 25.Miller CT, Lin L, Casper AM, et al. Genomic amplification of MET with boundaries within fragile site FRA7G and upregulation of MET pathways in esophageal adenocarcinoma. Oncogene. 2006;25:409–418. doi: 10.1038/sj.onc.1209057. [DOI] [PubMed] [Google Scholar]
- 26.Zhao X, Weir BA, LaFramboise T, et al. Homozygous deletions and chromosome amplifications in human lung carcinomas revealed by single nucleotide polymorphism array analysis. Cancer Res. 2005;65:5561–5570. doi: 10.1158/0008-5472.CAN-04-4603. [DOI] [PubMed] [Google Scholar]
- 27.Birchmeier C, Birchmeier W, Gherardi E, et al. Met, metastasis, motility and more. Nat Rev Mol Cell Biol. 2003;4:915–925. doi: 10.1038/nrm1261. [DOI] [PubMed] [Google Scholar]
- 28.Lutterbach B, Zeng Q, Davis LJ, et al. Lung cancer cell lines harboring MET gene amplification are dependent on Met for growth and survival. Cancer Res. 2007;67:2081–2088. doi: 10.1158/0008-5472.CAN-06-3495. [DOI] [PubMed] [Google Scholar]
- 29.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1985;53:457–481. [Google Scholar]
- 30.Cai T, Moskowitz CS. Semi-parametric estimation of the binomial ROC curve for a continuous diagnostic test. Biostatistics. 2004;5:573–586. doi: 10.1093/biostatistics/kxh009. [DOI] [PubMed] [Google Scholar]
- 31.Wolff AC, Hammond ME, Schwartz JN, et al. American Society of Clinical Oncology; College of American Pathologists. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol. 2007;25:118–145. doi: 10.1200/JCO.2006.09.2775. [DOI] [PubMed] [Google Scholar]
- 32.Wang SE, Narasanna A, Perez-Torres M, et al. HER2 kinase domain mutation results in constitutive phosphorylation and activation of HER2 and EGFR and resistance to EGFR tyrosine kinase inhibitors. Cancer Cell. 2006;10:25–38. doi: 10.1016/j.ccr.2006.05.023. [DOI] [PubMed] [Google Scholar]
- 33.Cappuzzo F, Bemis L, Varella-Garcia M. HER2 mutation and response to trastuzumab therapy in non-small-cell lung cancer. N Engl J Med. 2006;354:2619–2621. doi: 10.1056/NEJMc060020. [DOI] [PubMed] [Google Scholar]
- 34.Sequist LV, Martins RG, Spigel D, et al. First-line gefitinib in patients with advanced non-small cell lung cancer harboring somatic EGFR mutations. J Clin Oncol. 2008;26:2442–2449. doi: 10.1200/JCO.2007.14.8494. [DOI] [PubMed] [Google Scholar]
- 35.Yang CH, Yu CJ, Shih JY, et al. Specific EGFR mutations predict treatment outcome of stage IIIB/IV patients with chemotherapy-naive non-small-cell lung cancer receiving first-line gefitinib monotherapy. J Clin Oncol. 2008;26:2745–2753. doi: 10.1200/JCO.2007.15.6695. [DOI] [PubMed] [Google Scholar]