Abstract
Background: The provision of palliative care (PC) and opioids is difficult to ensure in remote areas in low- and middle-income countries. We describe here the set up of a home-care program in Sarawak (the Malaysian part of the Borneo Island), where half the population lives in villages that are difficult to access.
Methods: The establishment of this program, initiated in 1994 by the Department of Radiotherapy of Sarawak General Hospital, consisted of training, empowering nurses, simplifying referral, facilitating access to medication, and increasing awareness among public and health professionals about PC.
Results: The program has been sustainable and cost efficient, serving 936 patients in 2006. The total morphine usage in the program increased from <200 g in 1993 to >1400 g in 2006. The results show that pain medication can be provided even in remote areas with effective organization and empowerment of nurses, who were the most important determinants for the set up of this program. Education of family was also a key aspect.
Conclusion: The authors believe that the experience gained in Sarawak may help other regions with low or middle resources in the set up of their PC program especially for their remote rural population.
Keywords: morphine, pain control, palliative care
introduction
According to the World health Organization, the main priority of cancer centers in low- and middle-income countries should be the provision of palliative care (PC) for terminally ill cancer patients [1, 2]. PC was not considered a priority even in developed countries for a long time [3]; instead of adequate PC, terminally ill cancer patients were commonly subjected to costly nonpalliative interventions [4, 5]. In countries with limited resources, emphasis on symptom control, especially pain, should be of highest priority, and home-based PC should be integrated into the health-care system [1, 2].
The main obstacles to cancer pain relief in low- and middle-income countries are an inadequate supply of opioid drugs because of regulatory and pricing obstacles [6, 7], lack of knowledge and poor attitudes of health staff, and lack of knowledge in the community [8–10]. These obstacles can be surmounted by demonstration—by educating professionals, patients, and families about models of care that work, as shown in a study in Taiwan [11]. Training the care givers in patient's family in nursing skills allows less hospitalization and more time spent at home, reducing the need for travel to the hospital.
We describe here a home-care program set up in Sarawak, where half of the population lives in remote areas (18 inhabitants/km2). The program was based on education of health-care professionals in PC, with emphasis on achieving pain control and provision of good nursing care to minimize complications that would arise from morbidity in advanced stages of cancer. The overall aim was to ensure good PC for all terminally ill patients in Sarawak, with emphasis on drug availability especially for pain and home care.
background
Sarawak, one of the 13 states of Malaysia, is located on Borneo Island. Sarawak covers 124 450 km2 and has 2.25 million inhabitants. According to the United Nations human development index, Malaysia is ranked 61 out of 177 countries [12] and is thus a country with medium human development. Sarawak, however, is less developed than mainland Malaysia.
The main public health facilities consist of 21 Government hospitals, with 379 doctors and 37 specialists. These include the Sarawak General Hospital, which is the regional referral hospital, located in the capital and has the only cancer center of Sarawak: the Department of Radiotherapy and Oncology (DRO). Two smaller referral hospitals are located in the second and third towns of the State, while the remaining 18 hospitals are district hospitals, none of which has a PC unit. The other public heath centers of Sarawak include eight polyclinics (i.e. clinics with 6–10 medical officers located in urban areas), 119 health centers, and 97 rural clinics. The typical health center has senior and junior nurses and a small laboratory facility. Typical rural clinics have a male and a female nurse, who spend 70% of their time in villages. The private sector represents only 11% of hospital beds of Sarawak. In Malaysia, the cost of medications and travel for treatment are subsidized by the Ministry of Health (MoH).
In 1994, when starting the program, the DRO of Sarawak General Hospital had one oncologist, one physicist, one medical officer, and 18 nurses. By 2006, these numbers had reached two, two, six, and 63 respectively.
Cancer is an important disease in Sarawak, with an age-standardized incidence of 146/100 000 [13]. The number of new patients with cancer seen at the DRO increased from 749 in 1994 to 1296 in 2006, mainly for cancers of the lung and breast. Although poor patients in remote areas might not have reached the DRO during this period, greater awareness was raised by an ‘early cancer surveillance’ program [14], initiated in 1994, which leads us to estimate that >90% of all adult cancer patients of Sarawak are presently being seen at the DRO. In 1994, 79% of patients presented at a late stage, making PC an important priority [15]. Before the start of the palliative program presented here, terminally ill patients were sent home with a limited amount of medication, and no follow-up was ensured.
materials and methods
The program was designed and implemented by the DRO, especially by Dr Devi who decided to apply what she had learnt in the Master in Palliative Medicine program in Perth (Australia). The PC program consisted of seven components: training, empowering nurses, simplified referral, facilitating access to medication, pain reduction, political support and funds, and public awareness.
training
Nurses, pharmacists, and doctors from all Government hospitals and rural clinics were enrolled in the training program. Each session had 40 participants. Phase I (3 days) of the training covered the basics of PC, with practical sessions based on case studies of pain management, difficult wound management, pressure sore prevention, physiotherapy, occupational therapy, nutritional advice, aromatherapy ,and counseling. Phase II was conducted 1–1.5 years later and consisted of practical discussions with experienced nurses on case studies of home care.
empowering nurses
Doctors and nurses from the DRO were designated as resource personnel, the nurse in charge being contactable by phone 24 h a day, 7 days a week, so that continuous care could be provided. Owing to the high turnover of doctors in rural areas, the system was designed to allow all trained staff, especially nurses, to liaise with the staff of the PC unit at the DRO about follow-up and medication supply.
simplified referral
Patients could be referred to the DRO by any doctor, nurse, or family member. After an assessment by the oncologist, a management plan was drawn up, and the patient was referred to the nurse coordinator for further follow-up on home care. She called PC-trained staff in the rural clinic nearest to the patient's home when the patient was discharged from hospital, with instructions in a ‘home-based record’, in which all instructions for continuing care were detailed and which was given to the patient. If the patient could not come to the DRO, the assessment was made by telephone with the last doctor who had seen the patient.
facilitating access to medication
Our highest priority was to make drugs, especially aqueous morphine, available at all levels, including rural clinics. Following a request to the Sarawak State Director of Health, the policy of making morphine available for 2 weeks was changed to extend it to 1 month. When a patient was sent home, instructions for medications were faxed from the DRO's pharmacy to the hospital or clinic nearest to the patient's home, and medications were sent if they were not available. Each patient was given a month's supply of medication to avoid a shortfall. For patients living in certain remote areas, the oncologist prescribed a supply of medication for at least 3 months. Such special requests were documented in pharmacy records.
pain reduction
Pain management was ensured by radiotherapy and use of oral morphine. Morphine was available from the beginning of the program; we then have been able to procure sustained-release morphine tablets since 1995, transdermal patches (fentanyl) since 2004, and oxycodone since 2007. The other pain medications used, which were generic and inexpensive, were tramadol, codeine, nonsteroidal anti-inflammatory drugs, and adjuvant drugs like steroids, carbamazapine, and amitriptyline. Massage, a culturally acceptable practice, was included in phase I training for the nurses to teach the simple techniques to the care givers in the family during home visits.
political support and funds
Hospital management support and funds are important determinants of the success of a program. The first PC training course for nurses, in 1994, was proposed by the authors to the head of Sarawak General Hospital. In the first course, most of the 40 nurses were from the DRO, so that the PC service could start. For statewide training, the Sarawak State Director of Health was asked to issue invitations to nurses and allocated funds for claims and per diem. The 850 rural nurses who attended found that the courses gave them additional skills for handling terminally ill cancer patients. In 1998, when the MoH decided to set up PC units throughout the country, we informed them that we planned to designate 8 of 56 beds in the DRO for PC. For that purpose, a yearly budget of 10 000 Ringgit (US$ 2857) was provided, which in 2006 was increased to 25 000 Ringgit (US$ 6579).
The materials specific to PC were financed from the operating budget of the DRO. The authors realized, however, that certain equipments (e.g. an oxygen concentrator, a suction machine, wheelchairs, ripple mattresses, and bedpan) are necessary to improve the quality of life of dying patients, many of whom are of low socioeconomic status. In 1998, therefore, the authors decided to set up a nongovernmental organization, the ‘Sarawak Hospice Society’, for this purpose. The fund began with donations from patients’ families, and, gradually, some major donations came from individuals and organizations that became aware of the program. The initial start-up cost was about 3000 Ringgit (US$ 790).
public awareness
The Sarawak Hospice Society organized exhibitions of posters about home care in the capital of Sarawak and in some rural areas. During these exhibitions, an important local official was invited to create public enthusiasm and support for the program.
results
In 8 years, between 1994 and 2002, 1239 pharmacists, doctors, and nurses were trained. As there was a high turnover of doctors, only doctors who volunteered were trained (n = 50). Phase I training sessions began in 1994 and from 1995 to 2000 five sessions per year were held. In 2001 and 2002, three sessions per year were held and from 1998 we conducted one phase II course every 2 years. As experienced nurses motivated the junior nurses, there was active transfer of knowledge. Trained nurses receive technical support and advice from the staff of the DRO.
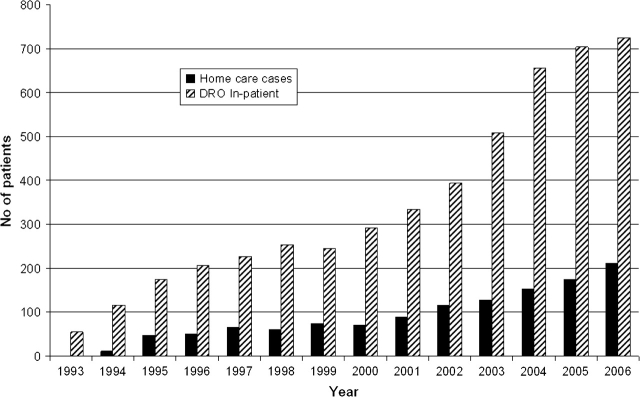
Figure 1 shows the number of patients who have benefited from the PC program since 1994. The inpatient group corresponds to patients receiving various types of PC, while the home-care group received only end-of-life care. The number of patients increased by 661% from 1994 to 2006 owing to the increase in the number of trained health staff and also the general increase of total cancer cases (+73%). It has to be noted that the overall proportion of late stage cancer (those requiring PC) has not varied much in Sarawak between 1994 and 2006 from 79% to 71%. In 2006, the number of patients receiving PC reached 936; we believe that this number is not far from the total number of cancer patients who need PC. Some patients may not have benefited from the program as they died before any form of care could be arranged, while others (approximately six to eight patients) refused home care for personal reasons; nevertheless, they continued to attend the clinic for their medication and hospitalization when required. Of the 936 patients who benefited PC in 2006, 58% were women and 42% men. Age ranged from 18 to 80 years with a mean age of 53. Most common primary tumors were nasopharynx and lung for men and breast and ovary for women. Most common symptoms at entry into the program were pain (80%), followed by shortness of breath due to pleural effusion/ lung metastases, abdominal distension, pressure sore, and dehydration. Duration of care at home varied from 4 days to 6 weeks according to the needs and life duration of patients.
Figure 1.
Total number of patients benefiting from palliative Care for 1993–2006.
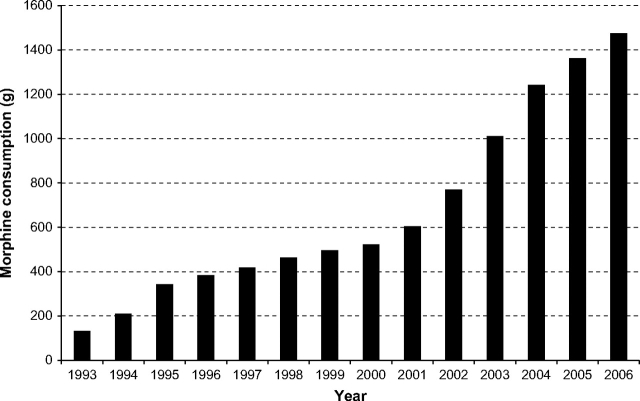
The medication supply system shown in Figure 2 was found to be practical, particularly for rural areas. Global morphine consumption is used by the World Health Organization (WHO) as a broad indicator of progress to improve cancer pain relief [16]. The total consumption of opiate per year in the program is displayed in Figure 3. In order to calculate opiate use, we converted the doses of all other forms of strong opioids, like parenteral morphine, long-acting oral morphine, and fentanyl patches, into the equivalent dose of aqueous morphine. Figure 3 shows that there was an important increase in opiate use between 1993 and 2006 as more patients were benefiting the program. The average consumption of opiate per patient did not vary much, from 2.2 g per patient in 1994 to 2.0 g per patient in 2006. The prescription practices stayed unchanged with 10 mg/4 h as the entry prescription and an average dose of opiate ∼120 mg per day per patient.
Figure 2.
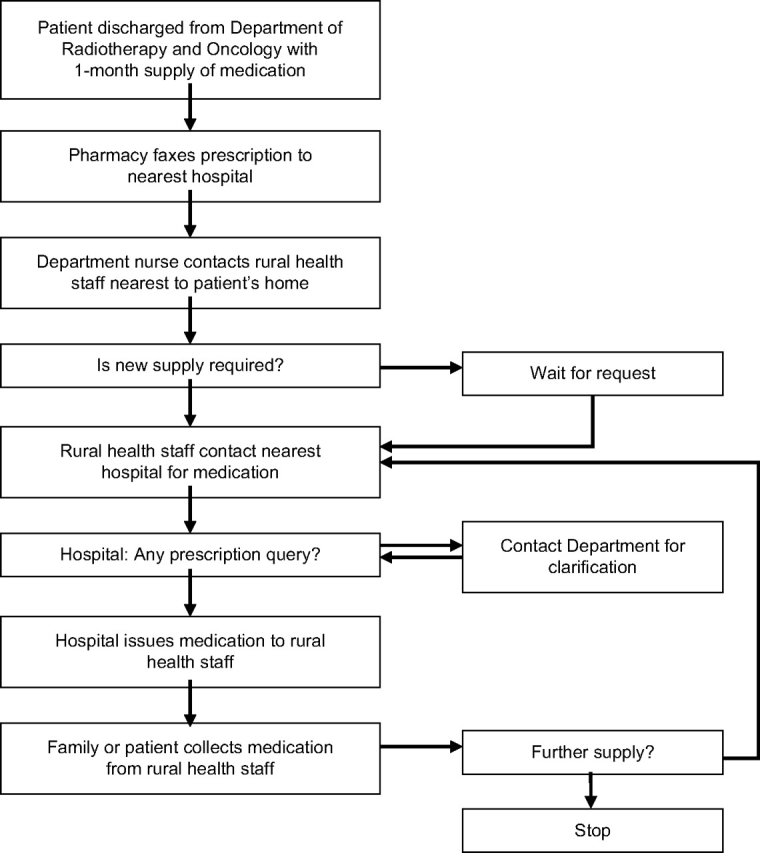
Supply of drugs, including morphine, to patients in rural Sarawak.
Figure 3.
Total consumption of morphine (g) in the palliative care programme from 1993 to 2006.
No illegal abuse of morphine occurred during the 13 years of the program, as we had no requests for morphine after the death of patients, and families returned medications to the nearest hospital or rural clinics upon the death of their loved ones. In addition, decisions to adjust the dose of morphine were made after consultation with the oncologist or medical officers at the DRO.
The main barriers to efficient home care that nurses faced in their practice were family beliefs in alternative medicine and reduction in morphine dosage because the family feared addiction. Although educating the families was time consuming, these barriers were tackled efficiently by the nurses.
discussion
We have not conducted a survey to quantify how our program has benefited the community or to measure quality of life from patient's perspective but we feel that the increasing number of cases referred for PC between 1994 and 2006 reflects a change in the attitude of health professionals and public and indicates that physicians of Sarawak are confident in our program.
The increase in morphine consumption corresponds to the increase in number of PC patients, which indicates acceptance by both professionals and patients of the use of morphine for pain management.
Experience of home-care programs similar to ours has been reported in Kerala [17, 18] and in Native American Indian populations [19]. The program in Kerala relied on active participation of trained volunteers from the community as very few health staff could be entrusted with PC. The free access to care for patient was ensured, thanks to charity funding from the local communities. No material support could be provided by the government, endangering the sustainability of the program. The situation in Sarawak is more comfortable as, in public hospitals, health-care delivery, cost of travel and drugs are subsidized. Hence, it was possible for patient to benefit PC at very minimal cost. The good rural primary health-care infrastructure existing in Sarawak allowed us to train rural health staff and thus to ensure continuity of care without having to get the patient to travel long distances. The sustainability of the Sarawak program was ensured by incorporating PC as part of the duties of the public health-care professionals. In our community, it would have been difficult to rely on NGO's and volunteer's goodwill to provide care and it would not have been sustainable.
The tribally based, culturally proficient PC program set up in a Zuni native community in Pueblo in the United States within the local health-care system [19], in which inpatient care was integrated with outpatient hospice care, is quite similar to our program.
Our program differs from other PC programs as, apart from symptom management, we lend equipment for home care free of cost with the assistance of the Sarawak Hospice Society. In many developing countries, the poor have difficulty in accessing the kind of care that people in developed countries have readily. We consider that poverty should not be the determinant of access to better care.
In order to improve quality of life, we incorporated massage therapy, which is a culturally acceptable practice, as part of PC. As alternative treatment is a key element of care in our community as in most part of Asia [20], our training emphasizes acceptable practices like massage and inexpensive, noninvasive rejuvenating herbal supplements. Nurses, who play a vital role in communication, must be made aware that some common traditional practices should be allowed.
Availability of opioids is not an issue in Sarawak, as what was observed in India where in 1997 there was a drastic reduction of morphine consumption due to the NDPS act [21]. This was brought to the attention of the Indian government to take the necessary remedial measures. However, in Sarawak we had to convince the authorities to extend the 2 weeks morphine availability policy to 1 month and 3 months if prescribed by oncologist. The main barrier to the use of opioids remaining was fear of addiction among heath staff and patient. Both the public and the health-care providers align morphine use to being a ‘drug addict’. Only with education and communication this belief can be changed.
conclusions
Models of PC vary based on the availability of resources. WHO state that ‘Home-based care is generally the best way of achieving good quality care and coverage in countries with strong family support and poor health infrastructure’ [2]. The present article describes the set up of such a PC program in Sarawak, Malaysia. This program has shown to be sustainable, not costly, and served 936 patients in 2006.
Training and educating health professionals with a well-organized system for delivering PC and availability of opiates were the pillars of this program. Empowerment of nurses and families were important determinants of its efficiency. The authors hope that the experience gained in Sarawak will help other regions with limited resources to set up PC programs, especially for patients in remote rural areas.
Acknowledgments
We would like to thank Dr Yao SC, State Director of Medical Health, Sarawak, Dr Zulkipli Jantan, Deputy Director, Medical Health, and Dr Yao SK, Hospital Director, for their assistance in approving and funding the program. We thank all the health staff in the hospital and clinics of Sarawak for assistance in the program. We would also like to thank Dr Elisabeth Heseltine for editing this paper.
References
- 1.Sikora K, editor. World Health Organization Programme on Cancer Control: Developing a Global Strategy for Cancer. Geneva: WHO; 1998. [Google Scholar]
- 2.World Health Organization. Cancer Pain Relief with a Guide to Opioid Availability. 2nd edition. Geneva: WHO; 1996. [Google Scholar]
- 3.Field MJ. The quality of dying: how can we improve care at the end of the life? Jt Comm J Qual Improv. 1997;23:498–504. [PubMed] [Google Scholar]
- 4.Abroneim JC, Morrison RS, Baskin SA, et al. Treatment of the dying in the acute care hospital. Advanced dementia and metastatic cancer. Arch Int Med. 1995;156:2094–2100. [PubMed] [Google Scholar]
- 5.Naik G. Unlikely way to cut hospital costs: comfort the dying. Wall St J. 2004;10 [PubMed] [Google Scholar]
- 6.World Health Organization. Symptom Relief in Terminal Illness. Geneva: World Health Organization; 1998. [Google Scholar]
- 7.International Narcotics Control Board. Availability of Opiates for Medical Needs. New York: United Nations; 1996. [Google Scholar]
- 8.Vainio A. Treatment of terminal cancer pain in France: a questionnaire study. Pain. 1995;62:155–162. doi: 10.1016/0304-3959(94)00264-F. [DOI] [PubMed] [Google Scholar]
- 9.Elliott TE, Murray DM, Elliott BA, et al. Physician knowledge and attitudes about cancer pain management: a survey from the Minnesota cancer pain project. J Pain Symptom Manage. 1995;10:494–504. doi: 10.1016/0885-3924(95)00100-d. [DOI] [PubMed] [Google Scholar]
- 10.Devi BCR, Tang TS, Corbex M. What doctors know about cancer pain management: an exploratory study in Sarawak, Malaysia. J Pain Palliat Care Pharmacother. 2006;20:15–22. [PubMed] [Google Scholar]
- 11.Liu WJ, Hu WY, Chiu TY, et al. Factors that influence physicians in providing palliative care in rural communities in Taiwan. Support Care Cancer. 2005;13:781–789. doi: 10.1007/s00520-005-0778-7. [DOI] [PubMed] [Google Scholar]
- 12.United Nations Development Programme. Human Development Index for Malaysia. Vienna: UNDP; 2006. [Google Scholar]
- 13.Ooi CH, Kiyu A, Yao SK, et al. Epidemiology of cancer in Sarawak, 1996–2000. Sarawak Cancer Registry, published by Sarawak Health Department. Malaysia: Kuching 2005. [Google Scholar]
- 14.Devi BCR, Tang TS, Corbex M. Reducing by half the percentage of late-stage presentation for breast and cervix cancer over 4 years: a pilot study of clinical downstaging in Sarawak, Malaysia. Ann Oncol. 2007;18:1172–1176. doi: 10.1093/annonc/mdm105. [DOI] [PubMed] [Google Scholar]
- 15.Merriman A. Pain and Symptom Control in the Cancer and/or AIDS Patient in Uganda and Other African Countries. 3rd edition. Kampala: Hospice Africa Uganda; 2000. [Google Scholar]
- 16.Colleau SM, editor. Cancer Pain Release. Making opioids available to treat cancer pain: the international system. 1994; 7: 1–4. [Google Scholar]
- 17.Rajagopal MR, Gayatri P. Status of cancer pain relief and palliative care, Kerala, India. J Pain Symptom Manage. 2002;2:191–193. doi: 10.1016/s0885-3924(02)00441-4. [DOI] [PubMed] [Google Scholar]
- 18.Kumar S, Numpelli M. Neighborhood network in palliative care. Indian J Palliat Care. 2005;11:6–9. [Google Scholar]
- 19.Finke B, Bowannie T, Kitzes J. Palliative care in the Pueblo of Zuni. J Palliat Med. 2004;7:135–143. doi: 10.1089/109662104322737403. [DOI] [PubMed] [Google Scholar]
- 20.Chiu TY, Hu WY, Cheng SY, Chen CY. Ethical dilemmas in palliative care: a study in Taiwan. J Med Ethics. 2000;26:353–357. doi: 10.1136/jme.26.5.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rajagopal MR, Joranson DE, Gilson AM. Medical use, misuse, and diversion of opioids in India. Lancet. 2001:358–443. doi: 10.1016/s0140-6736(01)05322-3. [DOI] [PubMed] [Google Scholar]