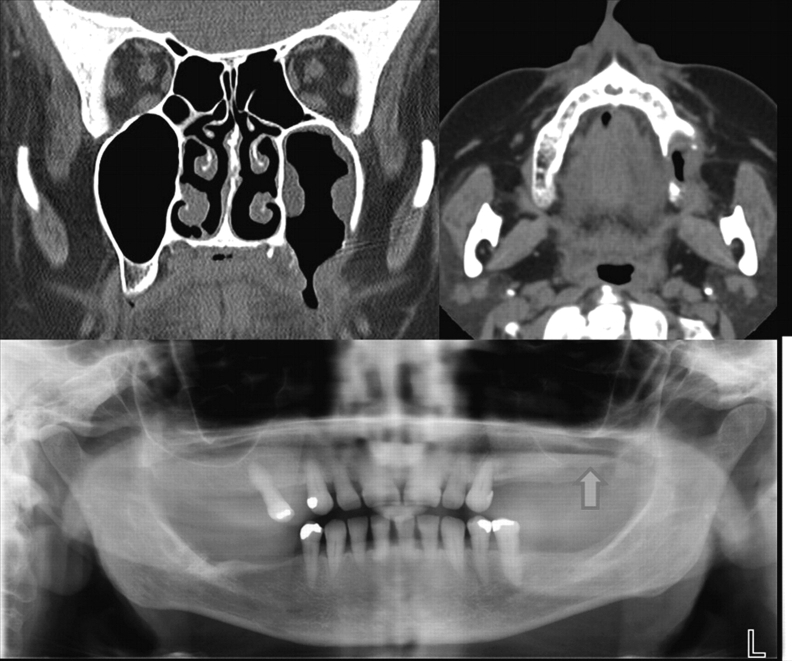
A 63-year-old woman suffered a local relapse of breast cancer. Baseline bone scan was normal and she had never received bisphosphonates previously. While being treated with liposomal doxorubicin and bevacizumab, she experienced left-sided maxillary pain after 1 month of therapy. A tooth infection was diagnosed and teeth number 25 and 26 were extracted. One month later, a mouth-antrum fistula was surgically revised and occluded. Shortly afterward the patient suffered from a trigeminal neuralgia. X-ray and computed tomography scan showed maxillary sinusitis and signs of osteonecrosis of the jaw (ONJ; Figure 1). The jaw lesion was carefully extirpated and the maxillary sinus was drained. Histological work-up verified the clinical diagnosis of ONJ, and an infiltration from the cancer was excluded. At 3 months of follow-up, the patient remains free of lesions and symptoms.
Figure 1.
Left-sided maxillary sinusitis and osteonecrosis of the jaw prior to surgical revision.
ONJ came up in connection with the use of bisphosphonates. The pathogenesis of ONJ remains unclear. More than half of all cases occur after dentoalveolar surgery due to a malfunctioning healing process. [1] Suppression of bone turnover, and inhibition of angiogenesis are the most likely contributing factors. Bisphosphonates block angiogenesis through inhibition of cell proliferation and vessel sprouting, as well as by decreasing circulating vascular endothelial growth factor (VEGF) levels. [2] Bevacizumab, a recombinant humanized mAb, achieves the same effect on binding to VEGF. [3] Known toxic effects associated with bevacizumab include hypertension, proteinuria, hemorrhage, wound-healing complications, thromboembolic events, and gastrointestinal perforations. Recently two cases of ONJ related to bevacizumab were published. [4]
Our patient is the third published case with a bevacizumab-associated ONJ. She developed a ‘classical’ ONJ (tooth infection followed by dentoalveolar surgery) without prior bisphosphonate exposure. Therefore other causes come into consideration. Infrequently, osteonecrosis has been recognized as a potential complication in patients having received radiotherapy or steroid-containing chemotherapy. Neither radiotherapy to the jaw nor corticosteroids had been administered in our patient. Liposomal doxorubicin is not known for causing ONJ. One patient receiving this drug developed necrosis of a distal phalange in the context of a severe hand–foot skin reaction. [5] Other possible contributing factors for ONJ, such as smoking, diabetes, vasculitis, or peripheral vascular disease, were not present in our patient. Therefore, we suspect bevacizumab, which hampers wound healing and possibly bone remodeling, as causative agent.
If more cases of bevacizumab-associated ONJ are reported, special dental management (jaw x-ray, optimal dental health, and good oral hygiene) should become standard before patients start bevacizumab.
References
- 1.Woo S-B, Hellstein JW, Kalmar JR. Narrative review: bisphosphonates and osteonecrosis of the jaw. Ann Intern Med. 2006;144:753–761. doi: 10.7326/0003-4819-144-10-200605160-00009. [DOI] [PubMed] [Google Scholar]
- 2.Vincenzi B, Santini D, Rocci L, Tonini G. Bisphosphonates: new antiangiogenic molecules in cancer treatment? Ann Oncol. 2003;14:806–807. doi: 10.1093/annonc/mdg194. [DOI] [PubMed] [Google Scholar]
- 3.Kim KJ, Li B, Houck K, et al. The vascular endothelial growth factor proteins: identification of biologically relevant regions by neutralizing monoclonal antibodies. Growth Factors. 1992;7:53–64. doi: 10.3109/08977199209023937. [DOI] [PubMed] [Google Scholar]
- 4.Estilo CL, Fornier M, Farooki A, et al. Osteonecrosis of the jaw related to bevacizumab. J Clin Oncol. 2008;26:4037–4038. doi: 10.1200/JCO.2007.15.5424. [DOI] [PubMed] [Google Scholar]
- 5.Palaia I, Angioli R, Bellati F, et al. Distal phalange necrosis: a severe manifestation of palmar plantar erythrodysesthesia. Am J Obstet Gynecol. 2006;195:e1–e2. doi: 10.1016/j.ajog.2006.05.018. [DOI] [PubMed] [Google Scholar]