Abstract
Two decades of research on euthanasia in the Netherlands have resulted into clear insights in the frequency and characteristics of euthanasia and other medical end-of-life decisions in the Netherlands. These empirical studies have contributed to the quality of the public debate, and to the regulating and public control of euthanasia and physician-assisted suicide. No slippery slope seems to have occurred. Physicians seem to adhere to the criteria for due care in the large majority of cases. Further, it has been shown that the majority of physicians think that the euthanasia Act has improved their legal certainty and contributes to the carefulness of life-terminating acts. In 2005, eighty percent of the euthanasia cases were reported to the review committees. Thus, the transparency envisaged by the Act still does not extend to all cases. Unreported cases almost all involve the use of opioids, and are not considered to be euthanasia by physicians. More education and debate is needed to disentangle in these situations which acts should be regarded as euthanasia and which should not. Medical end-of-life decision-making is a crucial part of end-of-life care. It should therefore be given continuous attention in health care policy and medical training. Systematic periodic research is crucial for enhancing our understanding of end-of-life care in modern medicine, in which the pursuit of a good quality of dying is nowadays widely recognized as an important goal, in addition to the traditional goals such as curing diseases and prolonging life.
Keywords: Euthanasia, The Netherlands
Introduction
Many people have pronounced opinions about the acceptability of euthanasia and the circumstances in which it should or should not be allowed. Worldwide, the topic sparks debates. Many of these debates are based on personal and moral views, whereas actual facts rooted in empirical research will contribute to a more enlightened debate.
To improve understanding of the Dutch situation regarding euthanasia, this paper provides a concise overview of research that has been performed in this field during the past two decades. Because the legalization of euthanasia in the Netherlands is the result of decades of debates, an overview is provided of the history of the Dutch debate on euthanasia, including the highlighting of some specific aspects of Dutch culture that contributed to the legalization of euthanasia.
Terminology
In the Netherlands, euthanasia has been defined since 1985 as the administration of drugs with the explicit intention to end life at the explicit request of a patient. Physician-assisted suicide is defined as the administration, supply or prescription of drugs with the explicit intention to enable the patient to end his or her life. Euthanasia and physician-assisted suicide are therefore to be distinguished from other medical decisions concerning the end-of-life; such as withdrawing or withholding potentially life-prolonging treatments; intensified measures to alleviate pain or other symptoms while taking into account the possible hastening of death or appreciating that possibility; or actively ending the patient’s life without an explicit request.
Since 2002, in the Netherlands both euthanasia and physician-assisted suicide have been lawful and they are both subject to the same criteria for due care. Therefore, in this paper, when mentioning “euthanasia”, “physician-assisted suicide” is included, unless stated otherwise.
Overview of the History of the Debate
Law on Medical Practice and the Penal Code
In the Netherlands, an important step towards physicians’ professionalism was the enactment of the Law on Medical Practice, in 1865. The law restricted medicine to those physicians who had passed a state exam, made it subject to governmental inspection, and introduced organization and standardization into medical practice. Four years later, in 1869, the Burial Act was enacted, regulating the way physicians should deal with deceased patients. It stated that a burial could only take place after written permission of a municipal registrar. This permission was only given when the attending physician stated on the death certificate that the patient died from a natural cause. In case of an unnatural death, the death should be reported to the national authorities. The enactment of the Penal code in 1881 made it an “offence, punishable by up to 12 years of imprisonment, for a person to cause the death of another person at his or her request”.
Start, Progress and Formalizing of the Euthanasia Debate
The societal debate about euthanasia in the Netherlands was triggered in 1973 by the so-called “Postma case” (Sheldon 2007). A physician helped her dying mother end her own life following repeated and explicit requests for euthanasia. The physician eventually received a short, suspended sentence. While the court upheld that she did commit murder, it offered an opening for regulating euthanasia by acknowledging that a physician does not always have to keep a patient alive against his or her will when faced with pointless suffering. As the first euthanasia test case, it broke social taboos in a country with strong Christian traditions. It also reflected a wave of awareness among many young medical professionals about the limits of medical care and patients’ self determination.
In the 1980s, the debate about euthanasia progressed and formalized. In 1980, the Committee of Attorneys-General took a special interest in physicians’ end-of-life decisions. To achieve uniformity in policy, they decided that every case of euthanasia should be scrutinized and that it should be decided whether or not the attending physician should be prosecuted. In 1982, the Health Council advised that a State Commission should be installed to address the definition of euthanasia as well as the criteria under which it should be allowed. In 1985, the Commission produced its report. The Commission defined euthanasia as “intentionally terminating another person’s life at the person’s request”. This definition has been used ever since. The Commission also drew up a series of criteria for due care to be met in every case of euthanasia. We shall return to those criteria later.
When the State Commission was working on its report, the Supreme Court ruled on the Schoonheim case, in 1984 (Griffiths et al. 1998). It was the first euthanasia case that was judged by the Dutch Supreme Court. Euthanasia was performed on the explicit request of a 95-year-old patient who suffered unbearably of a combination of deteriorating eyesight, hearing and speech, as well as being bedridden and experiencing general deterioration and loss of dignity. The Court concluded that the physician had acted in a situation of “necessity”, that is, the physician was confronted with a conflict of duties: the duty to relieve suffering and the duty not do harm. The physician was acquitted from prosecution.
The Role of the Royal Dutch Medical Association
The Royal Dutch Medical Association also undertook important steps towards formal societal control of euthanasia in the Netherlands in the 1980s. It took an official affirmative position regarding the legalization of euthanasia, and called for the elimination of barriers for physicians who intended to report their life-ending acts. It emphasized that only physicians should be allowed to perform euthanasia and that euthanasia can only take place within a physician-patient relationship. The Royal Dutch Medical Association further tried to improve formal societal control of euthanasia through encouraging physicians to report their cases. It brought out their vision on euthanasia for the first time in 1984, describing how physicians could prudently deal with patient’s request for euthanasia. (Central Board of the Royal Dutch Medical Association 1984) This vision on euthanasia was revised several times. In this way the medical professionals, through their professional organization, influenced the development of the due care criteria.
National Notification and Reporting Procedure for Euthanasia
After the start of the debate on euthanasia, some physicians were willing to report euthanasia cases and thus be held accountable. However, until the mid-1980s only a very small number of cases were reported. In 1990, the Ministry of Justice—together with the Royal Dutch Medical Association—agreed to proclaim a formal and uniform notification procedure, aiming at transparency, accountability, and harmonizing regional prosecution policies. Physicians who had complied with the criteria for due care for euthanasia would not be prosecuted. The notification procedure further aimed at eliminating practices that were perceived as hampering the physicians’ willingness to report. Examples are physicians treated as a murder-suspect, policemen interrogating relatives shortly after a patient died of euthanasia, or doctors who were taken for questioning from their surgeries, in front of patients, but subsequently found to have done nothing wrong.
This notification procedure entailed that the physician performing euthanasia informed the local medical examiner about his or her act through filling in an extensive questionnaire. Subsequently, the medical examiner informed the public prosecutor, who decided whether the physician had adhered to the criteria for due care or should be prosecuted.
As a next step, in 1998, a national reporting procedure was developed through establishing multidisciplinary review committees, consisting of a lawyer, a physician, and an ethicist. These committees judged the reported cases and advised the public prosecutor about whether or not the criteria for due care had been fulfilled. The reporting procedure was endorsed by many physicians, and the review committees only rarely found serious violations of the requirements.
The Euthanasia Act
After two decades of policy interventions, in which the public acceptance of euthanasia had further increased (from nearly 50% in 1966 up to 90% in 1998 (van der Maas et al. 1995)), a shift in the composition of the Dutch governing coalition occurred, and in 2001, the parliament decided that euthanasia should be legalized. On April 1st, 2002, the Euthanasia Act came into effect to regulate the ending of life by a physician at the request of a patient who was suffering unbearably without hope of relief. The criteria for due care, originally formulated by the State Commission, had been further developed, partly through case law (de Haan 2002). They require a physician to assess that:
The patient’s request is voluntary and well-considered;
The patient’s suffering is unbearable and hopeless;
The patient is informed about his situation and prospects;
There are no reasonable alternatives. Further,
Another independent physician should be consulted; and
The termination of life should be performed with due medical care and attention.
The Act officially legalized euthanasia, but in effect it mainly legalized an existing practice. The only major change was that, under the Act, the review committees needed to forward to the public prosecutor only those cases in which the criteria for due care criteria were not met. As such, the Act has diminished legal interference with physicians’ medical end-of-life practices. In the period 2003–2005, the review committees gave the verdict of non-compliance in 15 cases on a total of 5,600 reported cases. The main reason for the verdict of non-compliance was a failure to fulfill the requirement of consultation of a second “independent physician”. None of the involved physicians was eventually prosecuted (Onwuteaka-Philipsen et al. 2007). Most physicians think that the Act has improved their legal certainty and contributes to the care with which euthanasia and physician-assisted suicide are practiced (Onwuteaka-Philipsen et al. 2007).
Elements of Dutch Culture Related to Legalization of Euthanasia
The legalization of euthanasia is often considered to be the result of three changes in society: individualization, diminished taboos concerning death, and an increased recognition that prolonging life is not necessarily the appropriate focus of medical treatment for all patients (Weyers 2006). The fact that these changes occurred in many Western countries but led to legislation in only a few makes clear that some other elements of the Dutch culture and healthcare system played a significant role in the process of legalization of euthanasia.
First of all, the Dutch health care system has several important attributes that shaped a context of safeguards in which the legalization of euthanasia could take place. Social policies in the Netherlands have given broad support for equity in sharing financial burdens (Griffiths et al. 2008). As a result, virtually everyone is covered by health insurance and healthcare is freely accessible and affordable to all. Also, the general structure of the Dutch health care system is unique. The Dutch general practitioner is the pivot of primary care in the Netherlands: end-of-life care is in many instances provided at home; 65% of the people who die of cancer, die at home (Cohen et al. 2008; van der Heide et al. 2007). Almost all inhabitants in the Netherlands have a general practitioner with whom they often have a longstanding and personal relationship (Janssens and ten Have 2001). This might enable a general practitioner to judge whether a patient fulfills the first three, patient-related criteria of due care for euthanasia.
Second, the Netherlands has a history in which candor is highly valued (Kennedy 2002) and the Netherlands on the whole can be considered a climate in which new views and ideas are generally welcomed and openly discussed, as was the case for euthanasia. Further, in political culture, there is a general conviction that it is better to guide social developments than to try to stop them (Griffiths et al. 1998).
Research on End-of-Life Decision-Making
Background
A unique feature of the process of legalizing euthanasia in the Netherlands was the position of systematic empirical research. In 1990, along with the establishment of the notification procedure, the government decided that further legislation of euthanasia should await the findings of a commission appointed to conduct research on the frequency and characteristics of euthanasia, physician-assisted suicide and other medical end-of-life decisions in the Netherlands. This commission, known as the Remmelink Commission, appointed a research-group supervised by Professor Paul van der Maas. Since that first nationwide study, similar studies have been conducted every 5 years to study the frequency and characteristics of end-of-life decisions, as well as the proportion of reported cases of euthanasia. To enhance the cooperation of physicians, the information that was collected from physicians could not be claimed from the researchers by the public prosecutor in case of legal prosecution.
Methodology
Death Certificate Study
Nationwide frequencies and characteristics of end-of-life decisions were studied through death certificates studies in 1990 (van der Maas et al. 1992), 1995 (van der Maas et al. 1996), 2001 (Onwuteaka-Philipsen et al. 2003) and 2005 (van der Heide et al. 2007). Stratified samples of deaths cases were drawn from the central death registry of Statistics Netherlands, where all deaths in the Netherlands are reported. All physicians attending a death case—unless the cause of death precluded an end-of-life decision (such as a car accident resulting in instant death)—received a written questionnaire, accompanied by a recommendation letter of the Chief Inspector for Health care and the president of the Royal Dutch medical Association. The anonymity of physicians and patients was guaranteed. These measurements resulted in high response rates: 76% in 1990, 77% in 1995, 74% in 2001 and 78% in 2005.
Classification of End-of-Life Decisions
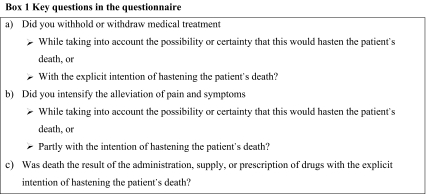
The questionnaire focused on the characteristics of end-of-life decisions that preceded the patient’s death. Such decisions can be characterized by several aspects: the acts of the physician (e.g. administering drugs or forgoing treatments), the intention of the physician (death can be explicitly intended, partly intended, or only taken into account), the involvement of the patient (actively involved in the decision-making process or not), and the life-shortening effect. The key questions for every death are shown in Box 1. When at least one of the questions (a) were answered with yes, the case was classified as a non-treatment decision. When at least one of the questions (b) was answered with yes, the case was classified as the alleviation of symptoms with a possible life-shortening effect. When question (c) was answered with yes, the case was classified as euthanasia when the drug was administered by the physician at the explicit request of the patient, and as physician-assisted suicide when the patient had taken the drug him- or herself. In the remaining cases where question (c) was answered with yes, but without explicit patient request, the case was classified as ending of life without an explicit request. For cases in which more than one question had been answered affirmatively, the decision with the most explicit intention prevailed over other decisions, whereas in cases of similar intentions question (c) prevailed over (b) and (b) over (a). A prominent aspect of the key questions is that words such as “euthanasia” and “physician-assisted suicide” are not used in the questionnaire, mainly because they may have different connotations and may lead to different interpretations by many physicians. In each study, the key questions were followed by questions about the decision-making process, the type of drugs that had been used, and the degree to which death had been hastened, according to the physician. Numbers of reported cases of euthanasia of physician-assisted suicide were obtained from the Public Prosecutors (1995, 1990) or the regional review committees (2001, 2005).
Main Findings from the Death Certificate Studies
In 1990, 1.7% of all deaths were preceded by euthanasia, as compared with 2.4% in 1995 and 2.6% in 2001 (see Table 1). This trend reversed in 2005, when 1.7% of all deaths were the result of euthanasia (approximately 2,300 cases). The number of euthanasia requests also decreased in this period: from 9700 in 2001 to 8400 in 2005. Despite recommendations from the Royal Dutch Medical Association that physician-assisted suicide should be preferred over euthanasia, physician-assisted suicide had a much lower frequency than euthanasia in each study; in 2005 this occurred in 0.1% of all deaths (approximately 100 cases annually). Possible explanations for the frequent choice of euthanasia over physician-assisted suicide are that physicians want to control the act of ending life and to have medical assistance available in case of unforeseen difficulties, which are more likely to occur when patients take the drugs orally themselves (Groenewoud et al. 2000). Euthanasia is also often preferred when patients are physically too weak to take the drugs themselves. An important factor in explaining the decline in the frequency of euthanasia and physician-assisted suicide in the period 2000–2005 may be an increased use of other options to relieve the patient’s suffering, such as continuous deep sedation, which was for the first time included in the 2001 study and has increased from 5.6% of all deaths in 2001 to 8.2% in 2005 (Rietjens et al. 2008). Table 1 further shows that the frequency of ending of life without an explicit patient request decreased from 0.8% of all deaths in 1990 to 0.4% in 2005 (approximately 550 cases annually). Further analyses of the cases of ending of life without an explicit request show that these concern nearly always patients who are very close to death, are incompetent but with whom the hastening of death has been discussed earlier in the disease trajectory and/or with their relatives, and for whom opioids were used to end life (Rietjens et al. 2007).
Table 1.
Frequency of euthanasia and other end-of-life practices in the Netherlands, in 1990, 1995, 2001 and 2005
| 1990 | 1995 | 2001 | 2005 | |
|---|---|---|---|---|
| Number of studied cases | 5197 | 5146 | 5617 | 9965 |
| Number of questionnaires | 4900 | 4604 | 5189 | 5342 |
| % | % | % | % | |
| Euthanasia | 1.7 | 2.4 | 2.6 | 1.7 |
| Assisted suicide | 0.2 | 0.2 | 0.2 | 0.1 |
| Ending of life without explicit patient request | 0.8 | 0.7 | 0.7 | 0.4 |
| Intensified alleviation of symptoms | 19 | 19 | 20 | 25 |
| Forgoing of life-prolonging treatment | 18 | 20 | 20 | 16 |
Forgoing of potentially life prolonging treatments (either withholding or withdrawing) and intensified alleviation of symptoms occurred much more often than active ending of life. In all of the studied years, the frequency of forgoing of life-prolonging treatments was rather stable, between 16–20% of all deaths. The percentage of the use of intensified alleviation of symptoms increased from 19% of all deaths in 1990 up to 25% in 2005.
Table 2 shows that the reporting rates of cases of euthanasia and physician-assisted suicide have increased since the first study in 1990. It can be estimated that in 1990, 18% of all euthanasia and physician-assisted suicide cases were reported, at that time to the Public Prosecutor. This percentage increased to 41% in 1995 (Public Prosecutor), 54% in 2001 (review committees) and 80% in 2005, after the introduction of the Act (review committees).
Table 2.
Reported cases of euthanasia and assisted suicide in 1990, 1995, 2001 and 2005
| 1990 | 1995 | 2001 | 2005 | |
|---|---|---|---|---|
| Total estimated number of euthanasia and assisted suicide | 2700 | 3600 | 3800 | 2425 |
| Reported number of number of euthanasia and assisted suicide | 486 | 1466 | 2054 | 1933 |
| Reporting rate | 18% | 41% | 54% | 80% |
In the 2005 study, it could be established that the major reason for not reporting was that the physician did not regard the course of action as euthanasia or physician-assisted suicide and therefore did not see the necessity to legally report the case (Onwuteaka-Philipsen et al. 2007). This was strongly related to the kind of drugs used. In cases where physicians used drugs that are advised by the Royal Dutch Association for the advancement of Pharmacy, that is, a barbiturate followed by a muscle-relaxant for euthanasia or barbiturates for physician-assisted suicide, the percentage of reporting in 2005 was 99%. In cases where other drugs were used to end a patient’s life with the explicit intention to end life at the patient’s request, which are mostly opioids, the reporting rate was 2%.
Table 3 shows the frequency of euthanasia and physician-assisted suicide in different patient subgroups in 2001 and 2005. The rates in 1990 and 1995 were comparable to those of 2001. The highest rates of the use of euthanasia were found in cancer patients: in 2005, 5.1% of all deaths of cancer patients were preceded by euthanasia or physician-assisted suicide. This explains partly the higher frequency of euthanasia and physician-assisted suicide among younger patients. Furthermore, compared to clinical specialists and nursing home physicians, general practitioners performed euthanasia or physician-assisted suicide in a higher proportion of deaths. This can be explained by the fact that euthanasia is usually performed in the context of a longstanding patient-physician relationship, which is typical for the type of contact that general practitioners have with their patients.
Table 3.
Euthanasia and physician-assisted suicide in different patient groups in 2001 and 2005
| Total | 2001 | 2005 |
|---|---|---|
| % | % | |
| 2.8 | 1.8 | |
| Age (years) | ||
| 0–64 | 5.0 | 3.5 |
| 65–79 | 3.3 | 2.1 |
| 80 or over | 1.4 | 0.8 |
| Sex | ||
| Male | 3.1 | 2.0 |
| Female | 2.5 | 1.5 |
| Cause of death | ||
| Cancer | 7.4 | 5.1 |
| Cardiovascular disease | 0.4 | 0.3 |
| Other/unknown | 1.2 | 0.4 |
| Type of physician | ||
| General practitioner | 5.8 | 3.7 |
| Clinical specialist | 1.8 | 0.5 |
| Nursing home physician | 0.4 | 0.2 |
Euthanasia and physician-assisted suicide were by definition always discussed with the patient (Table 4). In the large majority of cases, the physician also discussed the use of euthanasia or physician-assisted suicide with the patient’s family and with one or more colleagues. This indicates that euthanasia is usually performed in an open atmosphere. The rates from 1990 and 1995 were comparable. In most of the cases of euthanasia or physician-assisted suicide, life was ended with drugs that are recommended by guidelines, that is, muscle relaxants and/or barbiturates. Opioids were used in 27% of the cases in 1995, 22% of the cases in 2001, and 16% of the cases in 2005 (no comparable data available from 1990). Thus, there seems to be a tendency to use the recommended drugs when performing euthanasia or physician-assisted suicide, which is probably due to increased knowledge of physicians of how to perform euthanasia.
Table 4.
Discussion and use of drugs for euthanasia and physician-assisted suicide in 2001 and 2005
| 2001 | 2005 | |
|---|---|---|
| % | % | |
| Discussiona | ||
| Discussion with or previous wish of patient | 100 | 100 |
| Discussion with relative(s) | 96 | 75 |
| Discussion with other physician(s) | 91 | 88 |
| Drugsb | ||
| Neuromuscular relaxants | 63 | 65 |
| Barbiturates | 11 | 8 |
| Opioids | 22 | 16 |
| Benzodiazepines | 0 | 7 |
| Other drugs | 1 | 0 |
| Unknown | 4 | 3 |
aMore than one answer possible
bNeuromuscular relaxants, in any combination; barbiturates, possibly in combination with other drugs except neuromuscular relaxants; opioids, possibly in combination with other drugs except neuromuscular relaxants and barbiturates; benzodiazepines, possibly in combination with other drugs except neuromuscular relaxants, barbiturates and opioids; other drugs, any other combination of drugs
The Netherlands in a European Perspective
The death certificate study of 2001 was simultaneously and with the same questionnaire performed in five other European countries: Belgium (Flanders), Denmark, Italy (four areas), Sweden and Switzerland (German-speaking part) (van der Heide et al. 2003). These countries have a rather comparable epidemiology of diseases and quality of health care. They differ, however, in the legal regulations regarding euthanasia and physician-assisted suicide. Both practices are prohibited in Sweden, Denmark and Italy. In Switzerland, physician-assisted suicide is allowed if it is done without any self-interest, for physicians and other citizens, while euthanasia is forbidden. Interestingly, until recently in Switzerland, physicians could not provide physician-assisted suicide because being paid for their services could be seen as self-interest. Euthanasia was also prohibited in Belgium at the time of the study, but a new law that allowed euthanasia under comparable circumstances as in the Netherlands had already been discussed in the Parliament (Adams and Nys 2003). This was the first time that end-of-life decisions were studied in these countries, except for Belgium where in 1997 a similar study had been performed (Deliens et al. 2000).
Table 5 shows the main results of the study. The response percentages were satisfactory: 59% for Belgium, 62% for Denmark, 44% for Italy, 75% for the Netherlands, 61% for Sweden, and 67% for Switzerland. In all countries, physicians reported to have used drugs with the explicit intention to hasten the death of a patient (euthanasia, physician-assisted suicide, or ending of life without an explicit patient request). These proportions differed between countries, from 1% of all deaths or less in Denmark, Italy and Sweden, to 1.9% in Belgium and 3.4% in the Netherlands. Ending of life without a patient request occurred more often than euthanasia and physician-assisted suicide in all countries apart from the Netherlands.
Table 5.
Frequency of euthanasia and other end-of-life decisions in the Netherlands, Belgium, Denmark, Italy, Sweden, and Switzerland in 2001
| NL | BE | DK | IT | SW | CH | |
|---|---|---|---|---|---|---|
| % | % | % | % | % | % | |
| Euthanasia | 2.6 | 0.3 | 0.1 | 0.0 | – | 0.3 |
| Assisted suicide | 0.2 | 0.01 | 0.1 | 0.0 | – | 0.4 |
| Ending of life without explicit patient request | 0.7 | 1.5 | 0.7 | 0.1 | 0.2 | 0.4 |
| Intensified alleviation of symptoms | 20 | 22 | 26 | 19 | 21 | 22 |
| Forgoing of life-prolonging treatment | 20 | 15 | 14 | 4 | 14 | 28 |
The proportion of non-treatment decisions also differed substantially between countries: between 4% in Italy up to 28% of all deaths in Switzerland. Alleviation of pain and symptoms while taking into account or appreciating hastening of death as a possible side-effect happened more frequently and in comparable rates in all countries: between 19% (Italy) and 26% (Denmark) of all deaths.
These rates show that end-of-life decision-making with a possible or certain life-shortening effect is practiced everywhere in the studied West-European countries. End-of-life decisions that are mainly a medical response to the suffering of patients, such as alleviation of pain and symptoms, are performed in rather similar frequencies. However, the frequency of end-of-life decisions that are to a large extent determined by cultural factors—such as euthanasia, physician-assisted suicide and non-treatment decisions—varies much more between the countries.
Another striking finding of this study was that in countries where patients and relatives are more often involved in the decision-making at the end of life, the frequency of end-of-life decisions was higher, for example in the Netherlands. Many terminally ill patients who are facing death are offered interventions that may prolong their lives but at the same time may diminish their quality of life, such as cardiopulmonary resuscitation, mechanical ventilation or nasal-gastric feeding tubes. Discussion between patient, relatives and professional caregivers about whether or not to use such interventions may result in the recognition that quality of life is sometimes to be preferred over prolonging life at all costs.
What Have We Learnt?
A first important lesson that can be drawn from the past two decades of research on euthanasia in the Netherlands is that it is feasible to study physicians’ practices of end-of-life decision-making. While initially we thought that the high response rates of the Dutch studies could probably be explained by the Dutch tradition of openness about the subject, our European study showed that quite large proportions of physicians in other countries were also willing to share their experiences.
Second, our research shows that end-of-life decision-making is a significant aspect of end-of-life care. In approximately 4 out of every 10 patients, death is preceded by a decision that possibly or certainly hastened their dying process. This points to the growing awareness that high quality end-of-life care is not always aimed at prolonging the patient’s life at all costs. Rather, it is also aimed at improving the quality of life of patients through the prevention and relief of their symptoms, sometimes to the extent that far-reaching decisions such as euthanasia are requested by the patient.
Third, public control and transparency of the practice of euthanasia is to a large extent possible, at least in the Netherlands. The review and notification procedure has increasingly been accepted by physicians, which shows their trust in the system. While in 1990, 18% of the cases of euthanasia were reported, this percentage has increased up to 80% in 2005.
A last important lesson that can be learnt is that the legalization of euthanasia in the Netherlands did not result in a slippery slope for medical end-of-life practices. Besides religious or principal-based arguments, the slippery slope argument is the mainstay of opponents of the legalization of euthanasia. Briefly, the argument states that: if we allow A (the use euthanasia at the request of terminally ill patients), B (abuse of euthanasia, that is, ending the life of vulnerable patient groups without their consent) will necessarily or very likely follow. B is morally not acceptable; therefore, we must not allow A (Griffiths et al. 1998; van der Burg 1992). Our studies show no evidence of a slippery slope. The frequency of ending of life without explicit patient request did not increase over the studied years. Also, there is no evidence for a higher frequency of euthanasia among the elderly, people with low educational status, the poor, the physically disabled or chronically ill, minors, people with psychiatric illnesses including depression, or racial or ethnic minorities, compared with background populations (Battin et al. 2007).
Remaining Questions
Interpreting the Criteria for Due Care: The Case of “Unbearable Suffering”
Some of the criteria for due care for euthanasia are formulated as open general concepts, because they have to be interpreted taking into account the specific circumstances of every new case. The best example of such an open concept is the condition that the patient should suffer unbearably. In the Chabot-case (1994), the Court decided that suffering that has a non-somatic origin (such as a severe and refractory depression) can also be a justification for euthanasia; in the Brongersma-case (2002) this was further specified in the sense that suffering should originate from a medically classifiable disease, either somatic or psychiatric (Griffiths et al. 2008). Yet, the question remains what exactly the boundaries of “unbearable suffering” are. Euthanasia is most often performed in cases of severe suffering due to physical disease and symptoms and severe function loss, for patients with a limited life expectancy (Onwuteaka-Philipsen et al. 2007; van Delden and Battin 2008). In such cases there is usually little discussion about whether or not the suffering was unbearable. However, it appears that in “boundary cases”, such as suffering in the case of early dementia or existential suffering, there is more variance between physicians’ and patients’ perception of whether such suffering could be considered unbearable (Rietjens et al. 2005).
A previous study showed that a quarter of physicians who receive euthanasia requests find it problematic to assess the criteria of due care (Buiting et al. 2008). Problems are mostly related to the assessment of whether the patient suffered unbearably. To assess unbearability, physicians have to know how their patients experience the suffering, and there is no specific instrument to do so. What can be objectively determined is the underlying disease and the accompanying symptoms and loss of function. However, the question of whether and when symptoms lead to unbearable suffering ultimately depends on the experience of the person who is suffering, and hence is an individual matter depending on the patient’s personality, physical and mental perseverance, history and perceptions of the future (Cassel 1982). Hence, what is still bearable for one person may be unbearable for another. Some claim this makes the unbearability of suffering something a physician can hardly assess and which should mainly be left to the judgment of the patient (Beijk 1998; Buiting et al. 2008). Yet, the review committees argue that suffering should be at least partly open to objectification (Regional Euthanasia Review Committees 2007). Consequently, it is likely that physicians may have different opinions about which suffering can count as a legitimate ground for euthanasia. They may also have a different judgment than their patients, which is illustrated by the fact that a frequently mentioned reason for rejecting a patient’s euthanasia request is that the physician did not consider the patient’s suffering to be unbearable (Jansen-van der Weide et al. 2005).
On the one hand, different opinions about when suffering becomes unbearable could be interpreted as problematic. From the perspective of a patient, it may partly be a matter of chance whether a request for euthanasia will be granted. However, it is likely that this problem mainly exists in boundary cases, which are a minority of the euthanasia cases in the Netherlands (Onwuteaka-Philipsen et al. 2007). On the other hand, performing euthanasia is not part of “normal medical practice” and a physician is not obliged to perform euthanasia when a patient requests this (although he should refer the patient to another physician) and a patient has no “right to euthanasia”. From this point of view, difficulties with interpreting whether suffering is unbearable and potential differences between physicians (and patients) are to be expected and are consistent with the legal system of euthanasia in the Netherlands
Thus, although assessing when suffering becomes unbearable is highly personal and ultimately depends on the experience of the person who is suffering, fostering societal and professional discussion and case law can further stimulate the exploration of the legal and moral boundaries of unbearable suffering in the context of the euthanasia law.
Palliative Sedation: An Alternative for Euthanasia?
When patients who are nearing death have symptoms that cannot be relieved with conventional medical care, another option to relieve the patients’ suffering is to render them deeply asleep, to make them unaware of suffering. This practice is often referred to as “palliative sedation”. Medical indications for continuous deep sedation are present when one or more untreatable or refractory symptoms are causing the patient unbearable suffering (Verkerk et al. 2007; de Graeff and Dean 2007). In practice, pain, dyspnea and/or delirium are the refractory symptoms that lead most frequently to the use of continuous deep sedation (de Graeff and Dean 2007). A second precondition for the use of continuous deep sedation is the expectation that death will ensue in the reasonably near future—that is, within one to two weeks (Verkerk et al. 2007; de Graeff and Dean 2007) In these situations, a physician may decide to commence continuous deep sedation and in principle to continue it until death. In this situation, it is assumed that continuous deep sedation will not include the artificial administration of food or fluids because this will only prolong the patient’s suffering. If the patient’s life expectancy exceeds one to two weeks at the time that sedation is started, continuous deep sedation will affect the time of death, which is hastened by dehydration. Studies in the Netherlands show that the estimated life shortening effect of continuous deep sedation is limited in most cases (Rietjens et al. 2008, 2004).
As already described, the use of continuous deep sedation in the Netherlands was for the first time studied in 2001 and has increased from 5.6% of all deaths in 2001 to 8.2% in 2005 (Rietjens et al. 2008). Frequencies in other European countries are between 3–8% of all deaths in 2001 (Miccinesi et al. 2006). An important reason for the increased use of continuous deep sedation in the Netherlands is probably the increased attention to its use: guidelines have been published and continuous deep sedation received increasing societal and media attention. Another possible reason for the increased use of continuous deep sedation is that it may have increasingly been used as a relevant alternative to euthanasia (Rietjens et al. 2008). In the period 2000–2005, the use of euthanasia decreased from 2.6% to 1.7%. The increase of continuous deep sedation took place mostly in the subgroups in which euthanasia is most common: patients attended by general practitioners and those with cancer. Also, in 9% of the cases, continuous deep sedation was preceded by an ungranted euthanasia request. This suggests that continuous deep sedation may in some instances be a relevant alternative to euthanasia.
This raises the question whether continuous deep sedation may take away the need for euthanasia. The answer points to the similarities and differences between euthanasia and continuous deep sedation. The starting point of both practices is similar: a patient who suffers severely from a fatal disease. Yet, there are marked differences (Rietjens et al. 2006a). Continuous deep sedation is most often used in the last week of life to relieve unbearable physical suffering. Euthanasia is in the majority of patients applied somewhat earlier in the disease process to relieve unbearable suffering that is often rooted in a perceived loss of dignity and independency, and pointless suffering. Further, it is known that patients have varying perceptions about what constitutes a “good death”. Some consider control over the moment and time of dying of utmost importance, whereas others prefer to die in a deep sleep (Rietjens et al. 2006b; Steinhauser et al. 2000a, b). As such, euthanasia and continuous deep sedation are both relevant options to relieve unbearable suffering at the end of life. Nevertheless, the substitution of a part of euthanasia by continuous deep sedation shows that the situations in which physicians consider their use and physicians’ reasons for their use are not fully defined yet, and are still developing. More research and debate is needed to monitor both practices, and to investigate how they can contribute to an optimal quality of dying.
Can the Dutch Euthanasia Law be Used as a Model by Other Countries?
At the moment, euthanasia or physician-assisted suicide are legally allowed in the Netherlands, Belgium (Adams and Nys 2003; Deliens and Bernheim 2003), Switzerland (Hurst and Mauron 2003), and in the US states of Oregon (Chin et al. 1999) and Washington (Dyer 2008). In 1995, the world’s first euthanasia legislation, the Rights of the Terminally Ill Act, was passed in the Northern Territory of Australia, but the legislation was overturned in 1997 by Australia’s Federal Parliament. Currently, discussions about the legalization of euthanasia or assisted dying are also occurring in other countries, such as the UK (Dyer 2006), France (Peretti-Watel et al. 2003), Columbia (Moyano and Sambrano 2008) and Australia (Syme 2008). Debates about legalization often relate to concerns about whether a model of the Netherlands (or Belgium, Switzerland or Oregon) is “exportable” to other countries. There is no straightforward answer to this question.
As described earlier, the Netherlands has several unique features that have contributed to the legalization of euthanasia, probably the most important one being several decades of debate about euthanasia rooted in society. The Dutch health care system has several attributes that shaped a context of safeguards in which the legalization of euthanasia could take place, such as the fact that virtually everyone is covered by health insurance. Further, healthcare, including home care in case of chronic or terminal disease, is freely accessible and affordable to all. This gives no ground for the sometimes heard fear that euthanasia can be (mis)used in case of high costs of medical care. Also, the general structure of the Dutch health care system is quite unique, with the Dutch general practitioner as a core of primary care. Euthanasia is in the large majority of cases performed by general practitioners, who often know the patient for a long time, which might enable the physician to judge whether the patient fulfills the first three, patient-related, criteria of due care. These factors suggest that exporting the Dutch legalization process to other countries is not straightforward.
On the other hand, studies suggest that everywhere in the world, patients request for their life to be ended, also in countries where euthanasia or physician-assisted suicide are not legalized (Meier et al. 1998; van der Heide et al. 2003). Furthermore, our European study showed that euthanasia, physician-assisted suicide or life ending without an explicit patient request are part of medical practice in every studied country (van der Heide et al. 2003). If a society wants to control and improve life-ending practices, insight into the frequency and the characteristics of such practices is a first requirement. Our studies show that conducting research on end-of-life decision-making can greatly improve such insight. To improve life-ending practices, it can be argued that some degree of legalization may be a first prerequisite (Griffiths et al. 2008). Of course, the specific situation of each country should be taken into account when considering the conditions under which legalization can be discussed (van Delden and Battin 2008).
In Conclusion
Two decades of research on euthanasia in the Netherlands have resulted in clear insights into the frequency and characteristics of euthanasia and other medical end-of-life decisions in the Netherlands. These empirical studies have contributed to the quality of the public debate, and to the regulating and public control of euthanasia and physician-assisted suicide. No slippery slope seems to have resulted. Physicians seem to adhere to the criteria for due care in the large majority of cases. Further, it has been shown that the majority of physicians think that the euthanasia Act has improved their legal certainty and contributes to the carefulness of life-terminating acts. In 2005, 80% of euthanasia cases were reported to the review committees. Thus, the transparency envisaged by the Act still does not extend to all cases. Almost all unreported cases involve the use of opioids, and are not considered to be euthanasia by physicians. More education and debate is needed to disentangle in these situations which acts should be regarded as euthanasia and which should not.
Medical end-of-life decision-making is a crucial part of end-of-life care. It should therefore be given continuous attention in health care policy and medical training. Systematic periodic research is crucial for enhancing our understanding of end-of-life care in modern medicine, in which the pursuit of a good quality of dying is nowadays widely recognized as an important goal, in addition to the traditional goals such as curing diseases and prolonging life.
Acknowledgments
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- Adams, M. and H. Nys. 2003. Comparative reflections on the Belgian Euthanasia Act 2002. Medical Law Revision 11(3): 353–376. [DOI] [PubMed]
- Battin, M.P., A. van der Heide, L. Ganzini, G. van der Wal, and B.D. Onwuteaka-Philipsen. 2007. Legal physician-assisted dying in Oregon and the Netherlands: Evidence concerning the impact on patients in “vulnerable” groups. Journal of Medical Ethics 33(10): 591–597. [DOI] [PMC free article] [PubMed]
- Beijk, M.M. 1998. Unbearable suffering. What is it, what causes it, and who defines it. (In Dutch: Ondraaglijk lijden. Wat is het, waar wordt het door veroorzaakt en door wie wordt het bepaald). Medisch Contact 53: 825–827.
- Buiting, H.M., J.K. Gevers, J.A. Rietjens, B.D. Onwuteaka-Philipsen, P.J. van der Maas, A. van der Heide, and J.J. van Delden. 2008. Dutch criteria of due care for physician-assisted dying in medical practice: A physician perspective. Journal of Medical Ethics 34(9): e12. [DOI] [PubMed]
- Cassel, E.J. 1982. The nature of suffering and the goals of medicine. New England Journal of Medicine 306(11): 639–645. [DOI] [PubMed]
- Central Board of the Royal Dutch Medical Association. 1984. Vision on euthanasia. Medisch Contact 39: 990–997. [in Dutch].
- Chin, A.E., K. Hedberg, G.K. Higginson, and D.W. Fleming. 1999. Legalized physician-assisted suicide in Oregon—the first year’s experience. N Engl J Med 340(7): 577–583. [DOI] [PubMed]
- Cohen, J., J. Bilsen, J. Addington-Hall, R. Lofmark, G. Miccinesi, S. Kaasa, B. Onwuteaka-Philipsen, and L. Deliens. 2008. Population-based study of dying in hospital in six European countries. Palliative Medicine 22(6): 702–710. [DOI] [PubMed]
- de Graeff, A. and M. Dean. 2007. Palliative sedation therapy in the last weeks of life: A literature review and recommendations for standards. Journal of Palliative Medicine 10: 67–85. [DOI] [PubMed]
- de Haan, J. 2002. The new Dutch law on euthanasia. Medical Law Review 10(1): 57–75. [DOI] [PubMed]
- Deliens, L. and J. Bernheim. 2003. Palliative care and euthanasia in countries with a law on euthanasia. Palliative Medicine 17(5): 393–394. [DOI] [PubMed]
- Deliens, L., F. Mortier, J. Bilsen, M. Cosyns, R. Vander Stichele, J. Vanoverloop, and K. Ingels. 2000. End-of-life decisions in medical practice in Flanders, Belgium: A nationwide survey. Lancet 356(9244): 1806–1811. [DOI] [PubMed]
- Dyer, C. 2006. UK House of Lords rejects physician assisted suicide. British Medical Journal 332(7551): 1169. [DOI] [PMC free article] [PubMed]
- Dyer, C. 2008. Washington follows Oregon to legalise physician assisted suicide. British Medical Journal 337: a2480. [DOI] [PubMed]
- Griffiths, J., A. Bood, and H. Weyers. 1998. Euthanasia and law in the Netherlands. Amsterdam: Amsterdam University Press.
- Griffiths, J., H. Weyers, and M. Adams. 2008. Euthansia and law in Europe. Portland: Hart.
- Groenewoud, J.H., A. van der Heide, B.D. Onwuteaka-Philipsen, D.L. Willems, P.J. van der Maas, and G. van der Wal. 2000. Clinical problems with the performance of euthanasia and physician-assisted suicide in The Netherlands. New England Journal of Medicine 342(8): 551–556. [DOI] [PubMed]
- Hurst, S.A. and A. Mauron. 2003. Assisted suicide and euthanasia in Switzerland: Allowing a role for non-physicians. British Medical Journal 326(7383): 271–273. [DOI] [PMC free article] [PubMed]
- Jansen-van der Weide, M.C., B.D. Onwuteaka-Philipsen, and G. van der Wal. 2005. Granted, undecided, withdrawn, and refused requests for euthanasia and physician-assisted suicide. Archives of Internal Medicine 165(15): 1698–704. [DOI] [PubMed]
- Janssens, R.J. and H.A. ten Have. 2001. The concept of palliative care in The Netherlands. Palliative Medicine 15(6): 481–486. [DOI] [PubMed]
- Kennedy, J. 2002. A well-considered death [In Dutch: een weloverwogen dood]. Amsterdam: Prometheus Groep.
- Meier, D.E., C.A. Emmons, S. Wallenstein, T. Quill, R.S. Morrison, and C.K. Cassel. 1998. A national survey of physician-assisted suicide and euthanasia in the United States. New England Journal of Medicine 338(17): 1193–1201. [DOI] [PubMed]
- Miccinesi, G., J.A. Rietjens, L. Deliens, E. Paci, G. Bosshard, T. Nilstun, M. Norup, and G. van der Wal. 2006. Continuous deep sedation: Physicians’ experiences in six European countries. Journal of Pain and Symptom Management 31(2): 122–129. [DOI] [PubMed]
- Moyano, J., and S. Sambrano. 2008. Ten years later, Columbia is still confused about euthanasia. British Medical Journal: http://www.bmj.com/cgi/eletters/314/7098/1849/h#187734.
- Onwuteaka-Philipsen, B.D., A. van der Heide, D. Koper, I. Keij-Deerenberg, J.A. Rietjens, M.L. Rurup, A.M. Vrakking, J.J. Georges, M.T. Muller, G. van der Wal, and P.J. van der Maas. 2003. Euthanasia and other end-of-life decisions in the Netherlands in 1990, 1995, and 2001. Lancet 362(9381): 395–399. [DOI] [PubMed]
- Onwuteaka-Philipsen, B.D., J.K.M. Gevers, A. van der Heide, J.J. van Delden, H. Pasman, J.A. Rietjens, M.L. Rurup, H.M. Buiting, H. Hanssen-de Wolf, A. Janssen, and P.J. van der Maas. 2007. Evaluatie van de Wet toetsing levensbeëindiging op verzoek en hulp bij zelfdoding: Praktijk, melding en toetsing. Den Haag: ZonMW.
- Peretti-Watel, P., M.K. Bendiane, A. Galinier, R. Favre, J.M. Lapiana, H. Pegliasco, and J.P. Moatti. 2003. French physicians’ attitudes toward legalisation of euthanasia and the ambiguous relationship between euthanasia and palliative care. Journal of Palliative Care 19(4): 271–277. [PubMed]
- Regional Euthanasia Review Committees. 2007. Regional euthanasia review committees: 2007 annual report. http://www.euthanasiecommissie.nl/en/ (accessed June 12, 2009.)
- Rietjens, J.A., J. Bilsen, S. Fischer, A. Van Der Heide, P.J. Van Der Maas, G. Miccinessi, M. Norup, B.D. Onwuteaka-Philipsen, A.M. Vrakking, and G. Van Der Wal. 2007. Using drugs to end life without an explicit request of the patient. Death Studies 31(3): 205–221. [DOI] [PubMed]
- Rietjens, J.A., J.J. van Delden, A. van der Heide, A.M. Vrakking, B.D. Onwuteaka-Philipsen, P.J. van der Maas, and G. van der Wal. 2006a. Terminal sedation and euthanasia: a comparison of clinical practices. Archives of Internal Medicine 166(7): 749–753. [DOI] [PubMed]
- Rietjens, J.A., A. van der Heide, B.D. Onwuteaka-Philipsen, P.J. van der Maas, and G. van der Wal. 2006b. Preferences of the Dutch general public for a good death and associations with attitudes towards end-of-life decision-making. Palliative Medicine 20(7): 685–692. [DOI] [PubMed]
- Rietjens, J.A., A. van der Heide, B.D. Onwuteaka-Philipsen, P.J. van der Maas, and G. van der Wal. 2005. A comparison of attitudes towards end-of-life decisions: Survey among the Dutch general public and physicians. Social Science and Medicine 61(8): 1723–1732. [DOI] [PubMed]
- Rietjens, J.A., A. van der Heide, A.M. Vrakking, B.D. Onwuteaka-Philipsen, P.J. van der Maas, and G. van der Wal. 2004. Physician reports of terminal sedation without hydration or nutrition for patients nearing death in the Netherlands. Annals of Internal Medicine 141(3): 178–185. [DOI] [PubMed]
- Rietjens, J., J. van Delden, B. Onwuteaka-Philipsen, H. Buiting, P. van der Maas, and A. van der Heide. 2008. Continuous deep sedation for patients nearing death in the Netherlands: Descriptive study. British Medical Journal 336(7648): 810–813. [DOI] [PMC free article] [PubMed]
- Sheldon, T. 2007. Obituary: Andries Postma. British Medical Journal 334: 320. [DOI]
- Steinhauser, K.E., N.A. Christakis, E.C. Clipp, M. McNeilly, L. McIntyre, and J.A. Tulsky. 2000a. Factors considered important at the end of life by patients, family, physicians, and other care providers. Journal of the American Medical Association 284(19): 2476–2482. [DOI] [PubMed]
- Steinhauser, K.E., E.C. Clipp, M. McNeilly, N.A. Christakis, L.M. McIntyre, and J.A. Tulsky. 2000b. In search of a good death: Observations of patients, families, and providers. Annals of Internal Medicine 132(10): 825–832. [DOI] [PubMed]
- Syme, R. 2008. A good death: an argument for voluntary euthanasia. Melbourne: Melbourne University Press.
- van Delden, J.J.M. and M.P. Battin. 2008. Euthanasia: Not just for rich countries. In Global bioethics, ed. R. Green and A. Donovan. Oxford: Oxford University Press.
- van der Burg, W. 1992. The slippery-slope argument. Journal of Clinical Ethics 3(4): 256–268. [PubMed]
- van der Heide, A., L. Deliens, K. Faisst, T. Nilstun, M. Norup, E. Paci, G. van der Wal, and P.J. van der Maas. 2003. End-of-life decision-making in six European countries: Descriptive study. Lancet 362(9381): 345–350. [DOI] [PubMed]
- van der Heide, A., B.D. Onwuteaka-Philipsen, M.L. Rurup, H.M. Buiting, J.J. van Delden, J.E. Hanssen-de Wolf, A.G. Janssen, H.R. Pasman, J.A. Rietjens, C.J. Prins, I.M. Deerenberg, J.K. Gevers, P.J. van der Maas, and G. van der Wal. 2007. End-of-life practices in the Netherlands under the Euthanasia Act. New England Journal of Medicine 356(19): 1957–1965. [DOI] [PubMed]
- van der Maas, P.J., L. Pijnenborg, and J.J. van Delden. 1995. Changes in Dutch opinions on active euthanasia, 1966 through 1991. Journal of the American Medical Association 273(18): 1411–1414. [DOI] [PubMed]
- van der Maas, P.J., J.J. van Delden, and L. Pijnenborg. 1992. Euthanasia and other medical decisions concerning the end of life. An investigation performed upon request of the Commission of Inquiry into the Medical Practice concerning Euthanasia. Health Policy 21(1-2): vi-x, 1–262. [PubMed]
- van der Maas, P.J., G. van der Wal, I. Haverkate, C.L. de Graaff, J.G. Kester, B.D. Onwuteaka-Philipsen, A. van der Heide, J.M. Bosma, and D.L. Willems. 1996. Euthanasia, physician-assisted suicide, and other medical practices involving the end of life in the Netherlands, 1990–1995. New England Journal of Medicine 335(22): 1699–1705. [DOI] [PubMed]
- Verkerk, M., E. van Wijlick, J. Legemaate, and A. de Graeff. 2007. A national guideline for palliative sedation in the Netherlands. Journal of Pain and Symptom Management. [DOI] [PubMed]
- Weyers, H. 2006. Explaining the emergence of euthanasia law in the Netherlands: How the sociology of law can help the sociology of bioethics. Sociology of Health and Illness 28(6): 802–816. [DOI] [PubMed]


