Abstract
Objectives
To examine whether sex-based differences in mortality after percutaneous coronary interventions (PCIs) have changed in the past 25 years.
Background
Women with coronary artery disease have a higher risk of adverse outcomes after PCIs than do men. Recent temporal trends in short-term and long-term mortality in women after PCIs are unknown.
Methods
We performed a retrospective cohort study of 18,885 consecutive, unique patients who underwent PCIs between 1979 and 1995 (Early group, n=7,904, 28% women) and between 1996 and 2004 (Recent group, n=10,981, 31% women). Thirty-day and long-term mortality were compared by sex.
Results
Compared with men, women undergoing PCIs were older and more likely to have diabetes mellitus, hypertension, or hypercholesterolemia. Overall, PCI was successful in 89% of women and 90% of men. In the Recent group, 30-day mortality was significantly reduced compared with the Early group in women (2.9% vs 4.4%, P=.002) and men (2.2% vs 2.8%, P=.04). However, long-term survival was similar between Early and Recent groups among both men and women. After adjustment for risk factors, there was no difference between men and women from 1994 onward for either 30-day or long-term outcomes.
Conclusions
Thirty-day mortality after PCI in men and women has decreased in the past 25 years. After accounting for baseline risks, no differences in short-term or long-term mortality were observed between men and women.
Keywords: angina, angioplasty, coronary disease, follow-up studies, women
Introduction
Heart disease is the leading cause of death in women—approximately 400,000 deaths annually. In the United States, around 30% of the approximately 1 million annual percutaneous coronary intervention (PCI) procedures are performed in women. It is important, therefore, to carefully documentthe outcomes of women undergoing this procedure (1).
Women undergoing PCI are known to have a higher incidence of adverse outcomes than men (2–4). However, the results of risk-adjusted analyses of short-term and long-term outcomes after PCI are discordant with earlier studies demonstrating an adverse prognosis in women (2,3); more recent data indicate narrowing of the sex gap (5,6). Prior studies have shown that women undergo PCI later in the course of disease, have more comorbid conditions, and have more technically challenging coronary anatomy (7–9).
Most studies reporting on the sex-based differences in outcomes after PCI date from the early to mid 1990s. Coronary interventional practice since 1995 has been revolutionized with stents, combination oral antiplatelet therapy, glycoprotein IIb/IIIa inhibitors, and, even more recently, drug-eluting stents. To address the hypothesis that the sex gap in outcomes after PCI has narrowed, we performed an analysis of the Mayo Clinic PCI registry data 1) to characterize the current (1996–2004) practice and outcomes of PCI in women, 2) to compare current to past (1979–1995) practice, and 3) to compare the experience of women and men.
Methods
Patient Population
Since 1979, data from patients undergoing PCI at Mayo Clinic have been recorded in a prospective registry. For the present study, we considered 19,238 consecutive, unique patients undergoing PCI at Mayo Clinic Rochester. We considered the first PCI performed at Mayo Clinic for each patient; thus, patients with prior PCI performed elsewhere were included, and repeat procedures performed at Mayo Clinic were excluded. A total of 353 patients did not allow research use of their medical records and were excluded as required by State of Minnesota statute. The resulting cohort of 18,885 patients was divided into 2 groups for analysis: those treated in 1979 through 1995 (“Early” group; 7,904 patients, 28% women) and those treated in 1996 through 2004 (“Recent” group; 10,981 patients, 31% women). The cutoff point of 1996 was chosen because substantial changes in the treatment of and pharmacotherapy for coronary artery disease—eg, routine use of dual oral antiplatelet therapy and stents—occurred around that time period. The Mayo Clinic Institutional Review Board approved the study.
The medical records of all patients were reviewed to determine postprocedural outcomes. Procedural success was defined as decrease in the diameter of stenosis to less than 50%, without death, Q-wave myocardial infarction, or coronary artery bypass grafting surgery. All in-hospital deaths during the index hospital stay were attributed to the procedure. Additional data were recorded regarding noncardiac comorbid conditions such as cerebrovascular disease, peripheral vascular disease, malignancy, renal disease, diabetes mellitus, and hypertension.
Follow-Up
Follow-up information for all patients dismissed from the hospital was obtained by an experienced data technician by telephone 6 and 12 months after the initial procedure and annually thereafter. Information regarding vital status was sought. In the event of death, a patient’s next of kin reported the patient’s health status preceding the event, and the death certificate was requested. Mayo Clinic records were reviewed for all patients who were followed up at this institution, and verification of events occurring at other hospitals was obtained from the attending physicians. Routine review and editing of out-of-range data were performed to ensure quality of data received after dismissal from the hospital.
Statistical Analysis
Continuous data were summarized as mean±SD; discrete data were summarized as frequencies and group percentages. Linear and logistic regression models were used to test whether sex differences varied between the Early and Recent groups (ie, test for interaction). Comparisons between men and women within era or between eras within sex are not reported; most of these comparisons were significant because of the large sample size. P values less than .05 were considered significant.
The 2 end points of interest were 30-day and long-term mortality rates. Although patients were scheduled for 6-month and yearly telephone contact, some patients were not contacted after discharge; thus, neither 30-day nor long-term follow-up data were available. Therefore, 30-day and long-term mortality rates were analyzed with Kaplan-Meier estimates and Cox proportional hazards models. The formal analyses were based on long-term mortality; all hazard ratios, effects estimates, and P values are based on these outcomes. The 1-year estimates are provided for descriptive purposes. For actual event rates, we reported 1-year rates for the absolute risks (eg, Kaplan-Meier estimate) versus relative risks (eg, hazard ratio).
Multivariate Cox regression models were used to estimate partial hazard ratios. Because data regarding some important risk factors (preprocedural shock, peripheral vascular disease, renal disease, history of cerebrovascular accident/transient ischemic attack, American College of Cardiology/American Heart Association [ACC/AHA] lesion classification, bifurcated lesion, tumor/lymphoma/leukemia, and metastatic cancer) were not recorded in the database until late 1993, the multivariate analysis was restricted to 1994 onward. All but 2 covariates had less than 6% missing data. History of high cholesterol was missing in 11% of patients and ACC/AHA lesion type was missing in 9%. Multiple imputation was used to impute replacement values in 5 imputation data sets; models were then estimated for each data set. Missing data were imputed using the aregImpute function in the Hmisc library for S-Plus (Insightful Corp, Seattle, Washington). The SAS 9.1 procedure PROC MIANALYZE (SAS Institute, Cary, North Carolina) was used to combine each imputation’s parameter estimates (10,11).
Because the outcomes trends over time are unlikely to be strictly linear, we used restricted cubic splines to model curvilinear associations between procedure date and the outcome of interest, as well as other continuous covariates. In general, splines are piecewise equations tied together at locations called knots. Splines are similar to polynomial equations but are able to fit a more diverse set of relationships. We used 5 knots for the splines for procedure date and included an interaction between sex and date. Thus, 9 parameters were estimated to describe the post-PCI mortality trends over time for men and women.
Results
The baseline clinical characteristics for the study population are shown in Table 1. In both time periods, women were older and had more severe symptoms of coronary heart disease, more heart failure, and more frequent presentation with acute coronary syndromes (unstable angina, Canadian Cardiovascular Society Angina class III and IV) than men. Women also had a higher prevalence of comorbid conditions including diabetes mellitus and hypertension but were less likely to have had prior surgical or percutaneous coronary revascularization procedures. Table 2 summarizes the angiographic characteristics and highlights the number of patients discharged on evidence-based medications. Increased use of evidence-based medications for secondary prevention was noted in the Recent group. The mean medication score (based on the number of evidence-based medications, such as antiplatelet therapy, β-blockers, angiotensin-converting enzyme inhibitors, and lipid-lowering agents, the patient is receiving at dismissal) was higher in the Recent group and comparable in men and women (12). The use of stents and glycoprotein IIb/IIIa receptor inhibitors also was similar. Despite the greater severity of symptoms of angina, women had lower prevalence of multivessel disease, thrombus, and ACC/AHA type C lesions, and fewer women than men had left ventricular ejection fractions less than 40%.
Table 1.
Baseline Characteristics of the Early and Recent Groups*
| Early group (1979–1995) |
Recent group (1996–2004) |
||||
|---|---|---|---|---|---|
| Variable | Women (n=2,203) | Men (n=5,701) | Women (n=3,365) | Men (n=7,616) | Interaction P value† |
| Mean±SD age, y | 67.3±11.1 | 62.4±11.2 | 69.4±12.0 | 64.7±11.8 | .48 |
| MI, day of PCI or ≤24 h | 280 (13) | 821 (14) | 625 (19) | 1,380 (18) | .07 |
| MI, 1–7 days before PCI | 395 (18) | 838 (15) | 571 (17) | 1,156 (15) | .23 |
| Preprocedural shock | 55 (5) | 77 (3) | 170 (5) | 301 (4) | .10 |
| (n=1,022)‡ | (n=2,539)‡ | ||||
| Unstable angina | 1,633 (74) | 3,898 (68) | 1,977 (59) | 4,250 (56) | .02 |
| CCS Class III or IV | 1,581 (72) | 3,483 (61) | 1,800 (53) | 3,611 (47) | <.001 |
| Diabetes mellitus | 514 (23) | 846 (15) | 935 (28) | 1,634 (22) | .007 |
| Hypertension | 1,316 (60) | 2,512 (44) | 2,453 (73) | 4,571 (60) | .46 |
| Mean±SD body mass index | 27.7±5.6 | 28.0±4.3 | 29.3±6.4 | 29.4±5.1 | .18 |
| History of cholesterol ≥240, mg/dL | 978 (54) | 1,931 (41) | 2,312 (77) | 4,824 (71) | |
| (n=1,801)‡ | (n=4,737)‡ | (n=3,018)‡ | (n=6,829)‡ | .002 | |
| CHF on presentation | 224 (10) | 349 (6) | 444 (13) | 686 (9) | .27 |
| History of CHF | 330 (15) | 537 (9) | 572 (17) | 940 (12) | .16 |
| Current smoker | 422 (19) | 1,281 (23) | 589 (18) | 1,489 (20) | .34 |
| Prior MI | 1,200 (54) | 3,228 (57) | 1,747 (52) | 3,950 (52) | .23 |
| Prior PTCA | 60 (3) | 146 (3) | 338 (10) | 968 (13) | .06 |
| Prior CABG | 274 (12) | 1,058 (19) | 448 (13) | 1,570 (21) | .57 |
| Peripheral vascular disease | 65 (12) | 160 (12) | |||
| (n=541)‡ | (n=1,329)‡ | 355 (11) | 762 (10) | .67 | |
| CVA/TIA | 58 (11) | 116 (9) | 409 (12) | 765 (10) | .99 |
| (n=543)‡ | (n=1,332)‡ | ||||
| Moderate/severe renal disease | 23 (4) | 54 (4) | |||
| (n=544)‡ | (n=1,336)‡ | 123 (4) | 273 (4) | .93 | |
CABG, coronary artery bypass grafting surgery; CCS, Canadian Cardiovascular Society; CHF, congestive heart failure; CVA/TIA, cerebrovascular accident/transient ischemic attack; MI, myocardial infarction; PCI, percutaneous coronary intervention; PTCA, percutaneous transluminal coronary angioplasty.
Values are no. of patients (%) unless otherwise stated.
Tests for a change in the difference between men and women from the Early to the Recent group.
Number with data available.
Table 2.
Medications, Procedural Data, and Lesion Characteristics*
| Early group (1979–1995) |
Recent group (1996–2004) |
||||
|---|---|---|---|---|---|
| Variable | Women (n=2,203) | Men (n=5,701) | Women (n=3,365) | Men (n=7,616) | Interaction P value† |
| Medications at discharge | |||||
| Antiplatelet therapy | 1,767 (83) | 4,724 (85) | 3,102 (99) | 7,207 (99) | .34 |
| (n=2,125) | (n=5,569) | (n=3,130) | (n=7,252) | ||
| β-Blockers | 993 (45) | 2,655 (47) | 2,525 (75) | 5,666 (74) | .19 |
| Lipid-lowering drugs | 250 (11) | 613 (11) | 2,203 (65) | 5,136 (67) | .11 |
| ACE inhibitors | 237 (11) | 469 (8) | 1,507 (45) | 3,200 (42) | .045 |
| Medication score 3 or 4 | 240 (11) | 566 (10) | 2,174 (65) | 4,968 (65) | .16 |
| Glycoprotein IIb/IIIa antagonists | 4 (0.2) | 13 (0.2) | 1,642 (49) | 4,069 (53) | .94 |
| Stent use | 186 (8) | 555 (10) | 2,908 (86) | 6,673 (88) | .64 |
| Multivessel disease | 1,067 (48) | 2,815 (49) | 1,546 (46) | 3,758 (49) | .09 |
| ACC/AHA type C lesions | 279 (29) | 838 (35) | 1,270 (42) | 3,130 (45) | .22 |
| (n=961) | (n=2,394) | (n=3,056) | (n=6,885) | ||
| Maximum device size used, mm | 3.1±0.9 | 3.2±0.9 | 3.3±0.6 | 3.4±0.7 | .51 |
| Mean±SD percentage stenosis | |||||
| Preprocedure | 90.2±8.1 | 89.9±8.7 | 87.1±9.7 | 87.8±9.4 | .002 |
| Postprocedure | 32.5±21.4 | 32.7±21.0 | 8.6±17.6 | 8.8±18.0 | .98 |
| Lesion characteristics | |||||
| Calcified | 590 (28) | 1,389 (26) | 1,222 (40) | 2,702 (39) | .29 |
| (n=2,083) | (n=5,351) | (n=3,026) | (n=6,864) | ||
| Bifurcation | 58 (11) | 141 (11) | 406 (13) | 923 (13) | .91 |
| (n=530) | (n=1,301) | (n=3,185) | (n=7,177) | ||
| Thrombus | 789 (40) | 2,120 (41) | 984 (31) | 2,471 (35) | .22 |
| (n=1,993) | (n=5,122) | (n=3,164) | (n=7,131) | ||
| Ostial | 163 (17) | 383 (16) | 512 (21) | 1,206 (21) | .50 |
| (n=981) | (n=2,430) | (n=2,458) | (n=5,712) | ||
| EF ≤40% | 111 (5) | 335 (6) | 335 (10) | 870 (11) | .95 |
ACC/AHA, American College of Cardiology/American Heart Association; ACE, angiotensin-converting
enzyme; EF, ejection fraction.
Values are no. of patients (%) unless otherwise stated.
Tests for a change in the difference between men and women from the Early to the Recent group.
Table 3 shows the procedural success rate and in-hospital, 30-day, and 1-year outcomes. Procedural success was high and similar for the 2 sexes (women, 89%; men, 90%), with improvements noted in the recent time period. A total of 522 deaths occurred in the first 30 days, starting from the date of PCI. The 30-day mortality for women and men (4.4% and 2.8%, respectively) in the Early group was significantly higher than that of women and men in the Recent group (2.9% and 2.2%; P<.001). In addition, 30-day mortality in the Recent group was significantly decreased compared with the Early group in women (P=.002) and men (P=.04).
Table 3.
Procedural Success and Outcomes After PCI*
| Early group (1979–1995) |
Recent group (1996–2004) |
||||
|---|---|---|---|---|---|
| Variable | Women (n=2,203) | Men (n=5,701) | Women (n=3,365) | Men (n=7,616) | Interaction P value† |
| Procedural success | 1,821 (82.7) | 4,806 (84.3) | 3,142 (93.4) | 7,153 (93.9) | .80 |
| In-hospital events | |||||
| Death | 89 (4.0) | 145 (2.5) | 83 (2.5) | 139 (1.8) | .38 |
| Q-wave MI | 23 (1.0) | 67 (1.2) | 48 (1.4) | 87 (1.1) | .44 |
| Stroke | 5 (0.2) | 3 (0.1) | 30 (0.9) | 35 (0.5) | .29 |
| Emergent CABG | 69 (3.1) | 172 (3.0) | 28 (0.8) | 60 (0.8) | .95 |
| 30-Day events‡ | |||||
| Death | 97 (4) | 160 (3) | 96 (3) | 169 (2) | .25 |
| Any MI | 16 (1) | 32 (1) | 14 (0) | 34 (0) | .43 |
| 1-Year events‡ | |||||
| Death | 88 (4) | 194 (4) | 120 (4) | 256 (4) | .49 |
| Any MI | 106 (5) | 226 (4) | 109 (3) | 236 (3) | .31 |
| Repeat revascularization | 361 (17) | 1,015 (19) | 352 (11) | 767 (11) | .20 |
CABG, coronary artery bypass grafting surgery; MI, myocardial infarction; PCI, percutaneous coronary intervention.
Values are no. of patients (%).
Tests for a change in the difference between men and women from the Early to the Recent group.
Percentages are based on the event rates from the Kaplan-Meier estimator.
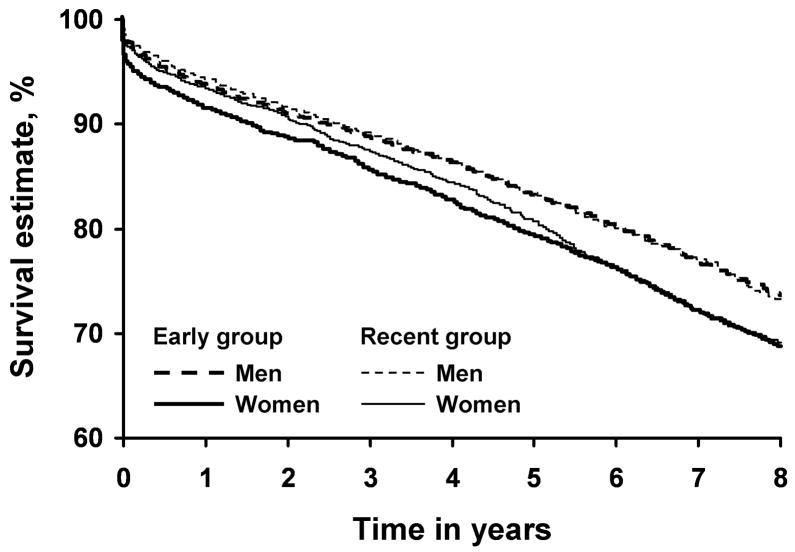
Unadjusted Survival
Follow-up was available through September 2005, with annual follow-up complete in 92% of patients. Median duration of follow-up was 13.2 years (interquartile range, 11.0–17.0 years) for the Early group and 4.1 years (interquartile range, 2.0–6.2 years) for the Recent group. There were 4,791 deaths during the long-term follow-up period (after a median of 7.0 years), 658 of which occurred in the first year after PCI. Figure 1 shows the overall estimated survival rates for women and men. Women had slightly lower survival than men, and for both sexes, especially men, survival was similar between the 2 time periods. The probability of survival at 5 years was 79% and 81% in women versus 83% and 83% in men, in the Early and Recent groups, respectively.
Fig. 1.
Kaplan-Meier curves estimating overall survival. Estimated survival is shown in men and women stratified by time period: Early group (1979–1995) and Recent group (1996–2004).
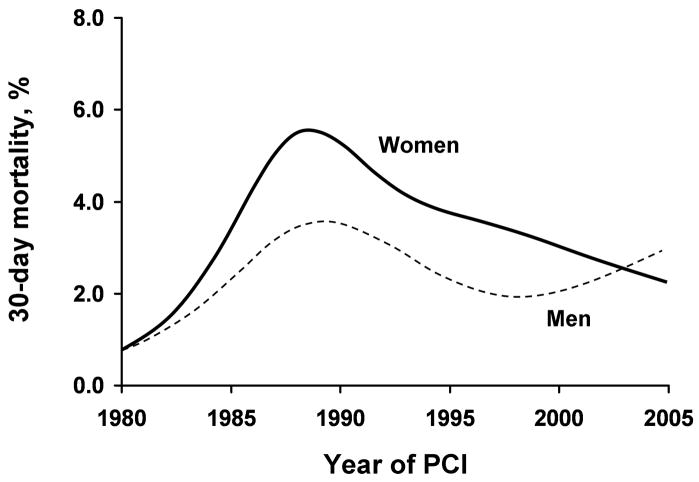
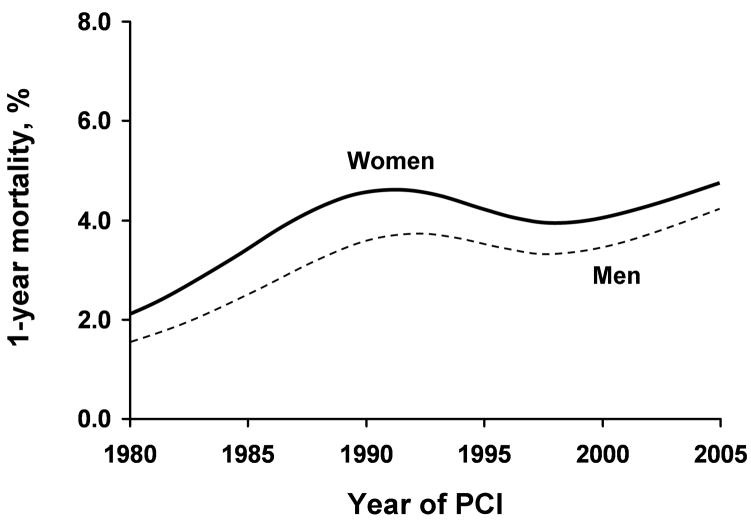
Temporal Trends for 30-Day and Long-Term Mortality
We further analyzed whether differences in 30-day and long-term mortality rates have significantly changed over time and whether the sex differential has varied over time. To avoid overfitting, we estimated 35 parameters for the 30-day model and 40 parameters for the long-term model. Analyses of long-term mortality started from day 31. For long-term mortality, we excluded patients who had less than 30 days of follow-up due to death (n=522) or censoring (n=249) (total n=771; 4%). Figures 2 and 3 show unadjusted estimates for 30-day and 1-year mortality rates based on the year of PCI. Women had significantly higher event rates at 30 days (P<.001) and over long-term follow-up (P<.001). Tests for interaction were nonsignificant (P=.23, 30 days; and P=.49, long term), indicating that the difference in men’s and women’s mortality rates was similar over time.
Fig. 2.
Unadjusted 30-day mortality rates. Mortality is shown in men and women by year of percutaneous coronary intervention (PCI).
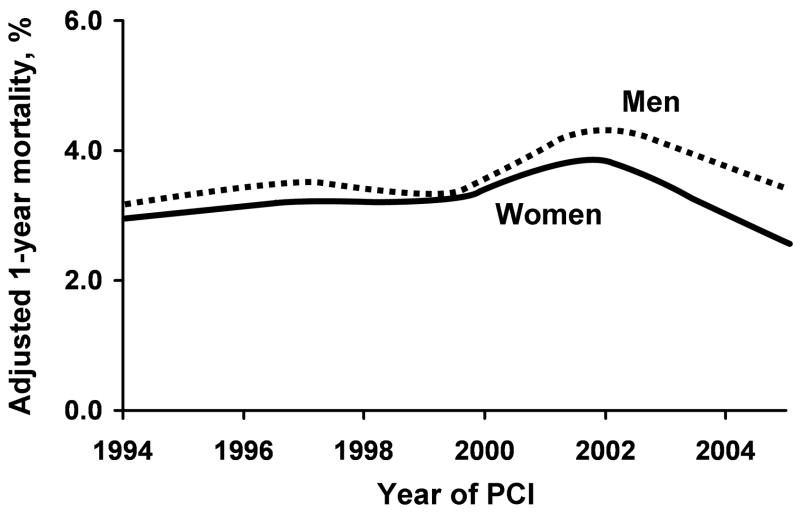
Fig. 3.
Unadjusted 1-year mortality rates. Mortality is shown in men and women by year of percutaneous coronary intervention (PCI).
To discern whether better application of drug treatment influenced improvement in mortality in women, we tested predismissal percentage utilization of 6 medications (β-blockers, aspirin, lipid-lowering agents, calcium-channel blockers, angiotensin-converting enzyme inhibitors, and diuretics) and its interaction with sex to influence long-term mortality. The results indicated that medication use was not more effective in women (data not shown).
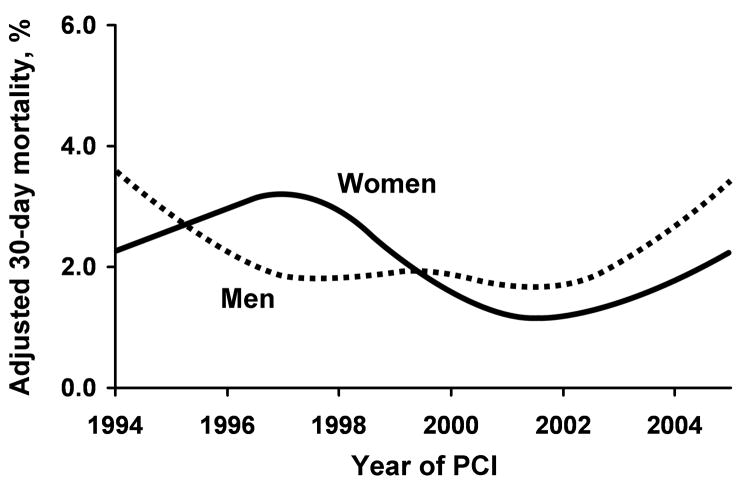
After adjusting for risk factors, the mortality rates were not significantly different between men and women at 30 days (Fig. 4; P=.10) and over long-term follow-up (Fig. 5; P=.42). Test for interaction was nonsignificant at 30 days and long term (P=.06 and P=.84, respectively). The estimates from the multiple regression models and the risk factors used for adjustment are shown in Table 4.
Fig. 4.
Adjusted 30-day mortality rates. Mortality is shown in men and women by year of percutaneous coronary intervention (PCI) after adjustment for factors listed in Table 4.
Fig. 5.
Adjusted 1-year mortality rates. Mortality is shown in men and women by year of percutaneous coronary intervention (PCI) after adjustment for factors listed in Table 4.
Table 4.
Multivariate Predictors of 30-Day and Long-Term Outcome*
| 30-day outcome |
Long-term outcome |
|||
|---|---|---|---|---|
| Variable | HR (95% CI) | P value | HR (95% CI) | P value |
| Time and sex† | 9 df | .007 | 9 df | .02 |
| Sex effect | 5 df | .10 | 5 df | .42 |
| Interaction‡ | 4 df | .06 | 4 df | .84 |
| Nonlinearity§ | 6 df | .01 | 6 df | .17 |
| Age | 3 df spline | <.001 | 3 df spline | <.001 |
| Emergency PCI | 2.36 (1.64–3.39) | <.001 | 1.15 (0.99–1.33) | .06 |
| Elective PCI | 0.65 (0.43–0.98) | .04 | 0.91 (0.84–1.00) | .053 |
| Pre-PCI shock | 5.03 (3.81–6.63) | <.001 | ||
| MI | ||||
| 0–6 h | 1.59 (1.05–2.40) | .03 | ||
| 6–23 h | 1.32 (0.85–2.06) | .22 | ||
| <24 h | 0.99 (0.84–1.17) | .88 | ||
| 1–7 d | 1.64 (1.17–2.31) | .004 | 1.05 (0.94–1.18) | .36 |
| >7 d | 1.26 (0.95–1.66) | .10 | 1.21 (1.08–1.36) | .001 |
| CHF on presentation | 1.75 (1.34–2.29) | <.001 | ||
| History of CHF | 2.31 (2.11–2.53) | <.001 | ||
| Hyperlipidemia | 0.74 (0.67–0.82) | <.001 | ||
| Body mass index | 2 df spline | .29 | 2 df spline | <.001 |
| Renal disease | 2.18 (1.55–3.07) | <.001 | 2.28 (1.96–2.65) | <.001 |
| Current smoking | 1.31 (1.15–1.48) | <.001 | ||
| History of smoking | 1.10 (0.85–1.41) | .47 | 1.23 (1.12–1.34) | <.001 |
| History of CVA/TIA | 1.36 (1.23–1.51) | <.001 | ||
| Diabetes mellitus | 1.19 (0.91–1.54) | .20 | 1.68 (1.54–1.83) | <.001 |
| Hypertension | 1.11 (0.84–1.45) | .47 | 1.09 (0.99–1.19) | .08 |
| B2/C lesion | 1.15 (1.01–1.31) | .03 | ||
| Type C lesion | 1.49 (1.07–2.08) | .02 | 1.10 (1.01–1.21) | .04 |
| Two VD (70%) | 1.24 (0.92–1.66) | .16 | 1.18 (1.08–1.29) | <.001 |
| Three VD (70%) | 1.95 (1.42–2.68) | <.001 | 1.26 (1.14–1.40) | <.001 |
| Prior CABG | 1.02 (0.76–1.39) | .88 | 1.55 (1.41–1.70) | <.001 |
| Previous PCI | 1.31 (0.90–1.91) | .16 | 1.02 (0.90–1.16) | .72 |
| PVD | 1.65 (1.24–2.19) | <.001 | 1.50 (1.35–1.66) | <.001 |
| PCI on a severe bend | 1.08 (0.93–1.26) | .32 | ||
| Thrombus in any lesion | 0.89 (0.81–0.98) | .02 | ||
| Metastatic cancer | 3.15 (2.39–4.14) | <.001 | ||
| Tumor/leukemia/lymphoma | 1.41 (1.28–1.57) | <.001 | ||
| Tumor/metastatic cancer | 1.08 (0.80–1.45) | .63 | ||
CABG, coronary artery bypass grafting surgery; CHF, congestive heart failure; CI, confidence interval; CVA/TIA, cerebrovascular accident/transient ischemic attack; HR, hazard ratio; MI, myocardial infarction; PCI, percutaneous coronary intervention; PVD, peripheral vascular disease; VD, vessel disease.
Splines were fitted to allow for nonlinear relationships between continuous variables and the HR. Splines are piecewise equations tied together at locations called knots. Splines are similar to polynomial equations but are able to fit a more diverse set of relationships. For further information, see the Statistical Analysis section.
Four parameters were estimated to model the trends over time in women, 4 parameters were estimated to model the trends over time in men, and 1 parameter was estimated to allow for a different intercept between men and women. The interaction between time and sex is tested by comparing the full model to a model with only a single time trend for both men and women.
Tests the null hypothesis that the difference in outcomes between men and women has been the same over time.
Tests the null hypothesis that the trend over time is strictly linear.
Complete Case Analysis
We also analyzed the outcomes based only on the patients without any missing data. Complete data were available for only 9,392 of 12,798 subjects for the 30-day mortality model. For long-term mortality, only 7,598 of 12,324 observations had complete data. The analysis of 30-day mortality in this subset indicates no significant difference between men and women (P=.18) and no significant interaction in time trends (P=.11) between men and women. The estimated probabilities from this model are similar to those from the imputed data model, although they show a slightly decreased mortality risk over time. The long-term mortality analysis of the subset shows no significant difference between men and women (P=.43), with results similar to the multiple imputation analysis.
Discussion
Over the past 25 years, the outcomes of PCI in women have improved, as is the case in men. Nonetheless, risk profile and absolute adverse event rates in women are higher than in men, and this has not changed over time, as shown in this and prior studies from our institution (13,14). After adjustment for risk factors, the 30-day and long-term mortality rates are similar in men and women. Additionally, the time trends in the past 25 years fail to show any sex-related disparity in the improved outcomes after PCI that have been noted over time.
Earlier studies evaluating sex differences in outcomes of PCI showed disparate results but in general reported higher complication rates in women (2,3). The earlier National Heart, Lung, and Blood Institute PCI registry indicated female sex to be independently predictive of in-hospital mortality (2). The adverse outcomes in women were attributed largely to older age, lower body surface area, smaller size of coronary arteries, higher risk profile, and more prevalent comorbid conditions. More recent studies, however, more consistently show improvement in rates of in-hospital complications after PCI in women which matched the rates in men. Jacobs et al (5) concluded, from National Heart, Lung, and Blood Institute data from 1993 to 1994, that sex differences decreased and women had significantly improved outcomes after PCI. The improvement for women has been reported not only in elective PCI but also in acute coronary syndrome, including acute myocardial infarction and shock (15,16). Malenka et al (17) made similar observations, reporting no sex differences in the outcomes from 1994 to 1999 in 33,666 consecutive hospital admissions for PCI in northern New England. Although most studies compiled in the AHA statement (6) indicate that more recent data do not support sex-based differences in the in-hospital outcome after PCI, the early hazard carried by women undergoing coronary stenting was noted in a recent study (18). We believe that the reasons for temporal improvement noted in both sexes are most likely multifactorial. The possible determinants of mortality reduction over time include newer technologies, improved operator experience, and better education and adherence to evidence-based medications by the patients.
Few reports have examined long-term sex-based differences related to PCI. Similar to our observations, the recent National Heart, Lung, and Blood Institute registry study noted higher unadjusted 1-year mortality in women than men (6.5% vs 4.3%; P=.02). However, after adjustment for other variables, sex was not a predictor of death or death and/or myocardial infarction. The present analysis is unique in that it spans 25 years and provides not only temporal trends in outcome between the sexes but also a long framework to analyze any sex differences over time. The present analysis shows significant improvement over time in outcome after PCI in both sexes and is consonant with recent observations from other centers in noting no differences in the outcome between the sexes after adjustment for other variables (16). The higher in-hospital mortality noted in women is likely multifactorial and may be largely due to increased risk profile (advanced age at PCI, more frequent presentation with acute coronary syndrome, and higher prevalence of comorbid conditions), because the sex differences for in-hospital complications narrowed or disappeared after adjustment for these and other significant risk factors predicting outcome.
The long-term predictors associated with lower mortality included hyperlipidemia and presence of thrombus. We have shown previously that hyperlipidemia was associated with decreased in-hospital mortality and increased postprocedural cardiac biomarker levels (19). The decreases in adverse outcomes were limited to patients taking statin drugs at the time of PCI. However, the 1-year survival in successful PCI was similar. Other studies have shown improved survival for patients receiving statin therapy after PCI (20,21). Most studies support angiographic thrombus as a predictor of in-hospital mortality but not of long-term mortality. In the 2 studies from our group regarding thrombus, mortality at 6 months to 1 year was similar in groups with and without thrombus (22,23). Thrombus, however, was associated with higher rates of in-hospital and 6-month myocardial infarction. The survival advantage in patients with thrombus is intriguing, and the reasons for it are, at best, speculative. We measured only mortality and not other end points such as myocardial infarction associated with thrombus. Favorable selection of survivors of PCI could be another reason for lower mortality in this subgroup.
Our study showed high and similar rates of evidence-based medications (given at the time of discharge) in both sexes in the Recent group—66% discharged with a medication score of 3 or 4. Such high medication scores were associated with lower rates of death or myocardial infarction on follow-up after PCI in a recent study from our institution (12). We also noted similar utilization of stents and glycoprotein IIb/IIIa receptor inhibitors in both sexes in the Recent group. The results from our study at a tertiary-care, high-volume center are incongruent with most available trials and multicenter quality improvement registries reporting underutilization of evidence-based medications, coronary angiography, and revascularization procedures in women (24–26). Such disparities highlight underutilization of evidence-based therapies in women in the real world versus the results obtained at a single-center, tertiary-care, referral hospital. We did not examine the utilization rates of invasive procedures in our dataset or adherence to evidence-based medications by the patients who did not undergo coronary angioplasty. Clearly, after coronary revascularization was performed, the early and long-term outcomes in both sexes were similar, underscoring the need to increase awareness among patients and physicians that outcome after PCI will likely be similar in men and women. Efforts should be taken to streamline, implement, and improve adherence to evidence-based medications and increase and optimize the utilization of invasive procedures in appropriate high-risk patients regardless of sex (14,26–28).
Limitations
This study is a retrospective analysis from a single, large-volume, tertiary-care center, which limits its generalizability. For some variables, the percentage of missing data was high, especially for earlier time periods, which restricted our ability to adjust for risk factors for PCI before 1994. We used multiple imputation to allow analysis of all observations from 1994 onward, while accounting for the uncertainty of unmeasured variables. We did not report other major adverse cardiovascular outcomes, including myocardial infarction, because the definitions of outcomes have changed over time. We could not elaborate on the physician and patient factors influencing the decision to perform coronary angiography and PCI. Even as we limited our analysis to short-term and long-term mortality, it is plausible that different methods of follow-up for patients treated at or outside our institution could have led to some misclassification bias.
Conclusions
The results of the present study indicate that after PCI, 30-day and long-term mortality in both sexes has decreased in the past 25 years. The higher short-term and long-term mortality in women are related more to underlying risk factors and comorbid conditions. After adjustment for such factors, survival is comparable in both sexes.
Acknowledgments
Editing, proofreading, and reference verification were provided by the Section of Scientific Publications, Mayo Clinic.
Abbreviations
- ACC
American College of Cardiology
- AHA
American Heart Association
- CI
confidence interval
- PCI
percutaneous coronary intervention
References
- 1.American Heart Association. Heart disease and stroke statistics—2005 update. Dallas (TX): American Heart Association; 2005. [Google Scholar]
- 2.Cowley MJ, Mullin SM, Kelsey SF, Kent KM, Gruentzig AR, Detre KM, et al. Sex differences in early and long-term results of coronary angioplasty in the NHLBI PTCA Registry. Circulation. 1985;71:90–7. doi: 10.1161/01.cir.71.1.90. [DOI] [PubMed] [Google Scholar]
- 3.Kelsey SF, James M, Holubkov AL, Holubkov R, Cowley MJ, Detre KM. Results of percutaneous transluminal coronary angioplasty in women: 1985–1986 National Heart, Lung, and Blood Institute’s Coronary Angioplasty Registry. Circulation. 1993;87:720–7. doi: 10.1161/01.cir.87.3.720. [DOI] [PubMed] [Google Scholar]
- 4.Maynard C, Every NR, Martin JS, Kudenchuk PJ, Weaver WD. Association of gender and survival in patients with acute myocardial infarction. Arch Intern Med. 1997;157:1379–84. [PubMed] [Google Scholar]
- 5.Jacobs AK, Johnston JM, Haviland A, Brooks MM, Kelsey SF, Holmes DR, Jr, et al. Improved outcomes for women undergoing contemporary percutaneous coronary intervention: a report from the National Heart, Lung, and Blood Institute Dynamic registry. J Am Coll Cardiol. 2002;39:1608–14. doi: 10.1016/s0735-1097(02)01835-1. [DOI] [PubMed] [Google Scholar]
- 6.Lansky AJ, Hochman JS, Ward PA, Mintz GS, Fabunmi R, Berger PB, et al. American College of Cardiology Foundation, American Heart Association. Percutaneous coronary intervention and adjunctive pharmacotherapy in women: a statement for healthcare professionals from the American Heart Association. Circulation. 2005 Feb 22;111:940–53. doi: 10.1161/01.CIR.0000155337.50423.C9. Epub 2005 Feb 1. [DOI] [PubMed] [Google Scholar]
- 7.Gardner TJ, Horneffer PJ, Gott VL, Watkins L, Jr, Baumgartner WA, Borkon AM, et al. Coronary artery bypass grafting in women: a ten-year perspective. Ann Surg. 1985;201:780–4. doi: 10.1097/00000658-198506000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Steingart RM, Packer M, Hamm P, Coglianese ME, Gersh B, Geltman EM, et al. Survival and Ventricular Enlargement Investigators. Sex differences in the management of coronary artery disease. N Engl J Med. 1991;325:226–30. doi: 10.1056/NEJM199107253250402. [DOI] [PubMed] [Google Scholar]
- 9.Maynard C, Litwin PE, Martin JS, Weaver WD. Gender differences in the treatment and outcome of acute myocardial infarction: results from the Myocardial Infarction Triage and Intervention Registry. Arch Intern Med. 1992;152:972–6. [PubMed] [Google Scholar]
- 10.Rubin DB. Multiple imputation for nonresponse in surveys. New York: Wiley; 1987. [Google Scholar]
- 11.Schafer JL. Multiple imputation: a primer. Stat Methods Med Res. 1999;8:3–15. doi: 10.1177/096228029900800102. [DOI] [PubMed] [Google Scholar]
- 12.Jaber WA, Lennon RJ, Mathew V, Holmes DR, Jr, Lerman A, Rihal CS. Application of evidence-based medical therapy is associated with improved outcomes after percutaneous coronary intervention and is a valid quality indicator. J Am Coll Cardiol. 2005 Oct 18;(46):1473–8. doi: 10.1016/j.jacc.2005.06.070. Epub 2005 Sep 23. [DOI] [PubMed] [Google Scholar]
- 13.Bell MR, Holmes DR, Jr, Berger PB, Garratt KN, Bailey KR, Gersh BJ. The changing in-hospital mortality of women undergoing percutaneous transluminal coronary angioplasty. JAMA. 1993;269:2091–5. [PubMed] [Google Scholar]
- 14.Bell MR, Grill DE, Garratt KN, Berger PB, Gersh BJ, Holmes DR., Jr Long-term outcome of women compared with men after successful coronary angioplasty. Circulation. 1995;91:2876–81. doi: 10.1161/01.cir.91.12.2876. [DOI] [PubMed] [Google Scholar]
- 15.Azar RR, Waters DD, McKay RG, Giri S, Hirst JA, Mitchell JF, et al. Short- and medium-term outcome differences in women and men after primary percutaneous transluminal mechanical revascularization for acute myocardial infarction. Am J Cardiol. 2000;85:675–9. doi: 10.1016/s0002-9149(99)00839-5. [DOI] [PubMed] [Google Scholar]
- 16.Wong SC, Sleeper LA, Monrad ES, Menegus MA, Palazzo A, Dzavik V, et al. SHOCK Investigators. Absence of gender differences in clinical outcomes in patients with cardiogenic shock complicating acute myocardial infarction: a report from the SHOCK Trial Registry. J Am Coll Cardiol. 2001;38:1395–401. doi: 10.1016/s0735-1097(01)01581-9. [DOI] [PubMed] [Google Scholar]
- 17.Malenka DJ, Wennberg DE, Quinton HA, O’Rourke DJ, McGrath PD, Shubrooks SJ, et al. Northern New England Cardiovascular Disease Study Group. Gender-related changes in the practice and outcomes of percutaneous coronary interventions in Northern New England from 1994 to 1999. J Am Coll Cardiol. 2002;40:2092–101. doi: 10.1016/s0735-1097(02)02605-0. [DOI] [PubMed] [Google Scholar]
- 18.Mehilli J, Kastrati A, Dirschinger J, Bollwein H, Neumann FJ, Schomig A. Differences in prognostic factors and outcomes between women and men undergoing coronary artery stenting. JAMA. 2000;284:1799–805. doi: 10.1001/jama.284.14.1799. [DOI] [PubMed] [Google Scholar]
- 19.Singh M, Lennon RJ, Roger VL, Rihal CS, Halligan S, Lerman A, et al. Relation of preprocedural statin therapy to in-hospital procedural complications following percutaneous coronary interventions in patients with hyperlipidemia. Am J Cardiol. 2006 Aug 1;(98):325–30. doi: 10.1016/j.amjcard.2006.02.036. Epub 2006 Jun 12. [DOI] [PubMed] [Google Scholar]
- 20.Lee PC, Kini AS, Ahsan C, Fisher E, Sharma SK. Anemia is an independent predictor of mortality after percutaneous coronary intervention. J Am Coll Cardiol. 2004;44:541–6. doi: 10.1016/j.jacc.2004.04.047. [DOI] [PubMed] [Google Scholar]
- 21.Serruys PW, de Feyter P, Macaya C, Kokott N, Puel J, Vrolix M, et al. Lescol Intervention Prevention Study (LIPS) Investigators. Fluvastatin for prevention of cardiac events following successful first percutaneous coronary intervention: a randomized controlled trial. JAMA. 2002;287:3215–22. doi: 10.1001/jama.287.24.3215. [DOI] [PubMed] [Google Scholar]
- 22.Singh M, Berger PB, Ting HH, Rihal CS, Wilson SH, Lennon RJ, et al. Influence of coronary thrombus on outcome of percutaneous coronary angioplasty in the current era (the Mayo Clinic experience) Am J Cardiol. 2001;88:1091–6. doi: 10.1016/s0002-9149(01)02040-9. [DOI] [PubMed] [Google Scholar]
- 23.Singh M, Reeder GS, Ohman EM, Mathew V, Hillegass WB, Anderson RD, et al. Does the presence of thrombus seen on a coronary angiogram affect the outcome after percutaneous coronary angioplasty? An Angiographic Trials Pool data experience. J Am Coll Cardiol. 2001;38:624–30. doi: 10.1016/s0735-1097(01)01445-0. [DOI] [PubMed] [Google Scholar]
- 24.Anand SS, Xie CC, Mehta S, Franzosi MG, Joyner C, Chrolavicius S, et al. CURE Investigators. Differences in the management and prognosis of women and men who suffer from acute coronary syndromes. J Am Coll Cardiol. 2005 Nov 15;(46):1845–51. doi: 10.1016/j.jacc.2005.05.091. Epub 2005 Oct 24. [DOI] [PubMed] [Google Scholar]
- 25.Blomkalns AL, Chen AY, Hochman JS, Peterson ED, Trynosky K, Diercks DB, et al. CRUSADE Investigators. Gender disparities in the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes: large-scale observations from the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines) National Quality Improvement Initiative. J Am Coll Cardiol. 2005;45:832–7. doi: 10.1016/j.jacc.2004.11.055. [DOI] [PubMed] [Google Scholar]
- 26.Hollenbeak CS, Weisman CS, Rossi M, Ettinger SM. Gender disparities in percutaneous coronary interventions for acute myocardial infarction in Pennsylvania. Med Care. 2006;44:24–30. doi: 10.1097/01.mlr.0000188915.66942.69. [DOI] [PubMed] [Google Scholar]
- 27.Guru V, Fremes SE, Austin PC, Blackstone EH, Tu JV. Gender differences in outcomes after hospital discharge from coronary artery bypass grafting. Circulation. 2006;113:507–16. doi: 10.1161/CIRCULATIONAHA.105.576652. [DOI] [PubMed] [Google Scholar]
- 28.Mehilli J, Ndrepepa G, Kastrati A, Nekolla SG, Markwardt C, Bollwein H, et al. Gender and myocardial salvage after reperfusion treatment in acute myocardial infarction. J Am Coll Cardiol. 2005;45:828–31. doi: 10.1016/j.jacc.2004.11.054. [DOI] [PubMed] [Google Scholar]