Abstract
The identification and evaluation of medically impaired drivers is an important safety issue. Medical fitness to drive is applicable to all ages but is particularly salient for older adults. Voluntary procedures, whereby various professionals and family members may report medical fitness concerns to State driver license bureaus, are common in the United States. This paper examines traffic crashes of drivers reported during 2001–2005 under the State of Missouri’s voluntary reporting law (House Bill HB-1536) and the resulting licensing outcomes.
Missouri’s law is non-specific as to age, but the mean age of reported drivers was 80. Reports were submitted by police officers (30%), license office staff (27%), physicians (20%), family members (16%), and others (7%). The most common medical condition was dementia/cognitive (45%). Crash history for reported drivers was higher than that of controls, dating back to 1993, reaching a peak in 2001 when the crash involvement of reported drivers was 9.3% vs. 2.2% for controls—a fourfold difference. The crash involvement of reported drivers decreased rapidly after, indicating the impact of HB-1536 reporting with subsequent license revocation and to a lesser degree, mortality. Of the 4,100 reported individuals, 144 (3.5%) retained a driver’s license after the process.
Keywords: fitness to drive, aging, voluntary reporting, older driver, crash history, driver licensing, medical impairment, safety
1. Introduction
There are 35+ million people over age 65 years in the United States (U.S.) with almost 5 million over age 85 (US Census Bureau, 2005). Twenty-one percent of the U.S. population will be over age 65 by the year 2050, representing over 86 million older adults (US Census Bureau, 2005). A major increase in the number of older drivers is expected based on current demographics (Dobbs, 2008; Retchin and Anapolle, 1993) and these drivers will retain their licenses longer than past generations (Hakamies-Blomqvist, 1994). Older drivers will also travel greater distances and take more trips than the current cohort (Rosenbloom, 2000).
Older drivers may have more favorable driving behavior profiles when compared to other age groups. For instance, they are less likely to travel in poor weather, drive on busy roadways or during rush hour, and they limit their driving at night (Ball et al., 1998). Older drivers are less likely to drive while intoxicated and are more likely to obey speed limits (Lyman et al., 2002; Langford and Koppel, 2006). Studies show that many older adults make decisions to restrict their on-road exposure in response to perceived changes in health and function (Langford and Koppel, 2006; Ball et al., 1998). Still, other studies suggest that self-regulation is not always consistent in this group (e.g., Browning and Simms, 2007; Baldock et al., 2006; Stalvey and Owsley, 2003), and self-regulation “is clearly not a sufficient process alone to ensure safe driving among the elderly” (Fildes, 2008, p. 389).
As a group, older adults are at greater risk for health conditions that may impair driving ability (Darzins and Hull, 1999) and increase crash risk, especially after age 70 (Carr, 2000). In Alabama, McGwin and Brown (1999) found that 8.4% of the crashes of older adults had an associated medical illness as determined by a police officer, when compared to younger drivers (1.4%). In a study of fixed deficits that included vision and cognition, Hakamies-Blomqvist (1993) noted that 50% of fatal crashes involving an older driver had a medical factor that played a contributing role in comparison to just 10% for younger drivers. Research indicates that some drivers with a dementing illness continue to drive (Odenheimer, 1993). A study using a brief cognitive screen during driver license renewal found that as many as 6% of persons 65–69 years old and almost 20% of those 80+ years had health-related impairments (Stutts et al., 1998).
A range of health conditions have been linked with crashes, licensing, and performance-based outcomes, including: neurological disorders (e.g., Alzheimer’s disease, stroke, epilepsy), vision disorders (e.g., cataracts, glaucoma, macular degeneration), and joint/movement-related disorders, such as rheumatoid arthritis (Dobbs, 2005; Charlton et al., 2004). Chronic medical illnesses often progress in severity and may impair the ability to drive for a substantial minority of elders, resulting in increased crash risk if undetected or insufficiently addressed by health professionals.
The “medically fit” driver has sufficient vision, alertness, cognition, joint range of motion, and motor skills, to manage the operational, tactical, and strategic demands of driving (Michon, 1985; Anstey et al., 2005; Wang and Carr, 2004). Health conditions that detract meaningfully from these key abilities may increase crash risk, and thus require focused evaluation and intervention (Odenheimer, 2006; Dobbs and Carr, 2005). Not all drivers age in the same way, however, and a major challenge is how to separate the subgroup of “medically-at-risk” older drivers from the total population (see discussions in Dobbs, 2008; Molnar and Eby, 2008).
The concept of medical fitness to drive (MFD) is applicable to all age groups and it is particularly salient for older adults. Most U.S. states utilize voluntary procedures to address MFD concerns, whereby various professionals and/or family members may report concerns to State Driver’s License Bureaus (DLB) (Morrisey and Grabowski, 2005).
When a report is made, a DLB may require medical evaluation and/or driving-related testing (written, vision, and/or on-road) to inform the license eligibility decision. Should a physician identify an MFD-related concern, the physician can report the driver to a DLB for evaluation and possible license revocation. A few U.S. states, such as Maryland, utilize detailed, age-specific evaluation protocols (Staplin et al., 2003), whereas others, such as Missouri, evaluate older drivers using standard driving tests applied at any age. A handful of U.S. states, including California, Delaware, New Jersey, Oregon, and Pennsylvania, mandate that certain MFD-related health conditions (e.g., Alzheimer’s disease, epilepsy) must be reported to the DLB for evaluation at the time of diagnosis (Wang et al., 2003).
Although much is known about medical conditions and driving, the translation of this knowledge to driver licensing and individual driver safety needs more attention. A DLB requires reliable and valid processes for evaluating driving competency (Christie, 2000). A report from the Organization of Economic Cooperation and Development expressed support for a more focused, consistent approach to older driver evaluation and licensing (OECD, 2001). The OECD report argued that crash risk is largely a function of medical illnesses and associated functional deficits, many of which are more prevalent with aging. Thus, OECD recommended that future efforts for evaluating older driver safety should target medically impaired drivers and not older adults in general (OECD, 2001).
One promising approach is to incorporate research on MFD into driver licensing procedures. In this way, drivers with medical conditions can be identified, and their problems can be addressed through education, use of adaptive equipment, license restrictions, and/or license revocation when appropriate. In order to target drivers with medical impairments there must also be a policy or law that allows for DLB referrals from health professionals, law enforcement, and family members.
Little systemic information is known about how drivers are reported to DLBs under voluntary reporting mechanisms, the drivers’ characteristics and health status, and—most importantly—what happens in terms of driver licensing and protection of public safety.
This paper is drawn from a project that evaluated the functional impact of the State of Missouri’s voluntary reporting law (House Bill HB-1536), passed in 1999, for drivers considered as potentially unfit to drive due to medical impairment (Meuser et al., 2008). HB-1536 provides a voluntary, legal process whereby concerned family members, police officers, physicians, and others can report a driver for evaluation and/or possible license revocation. The reporter’s identity is confidential, and HB-1536 provides civil immunity protection from prosecution for breach of confidentiality. HB-1536 is non-specific with regard to age, and includes a Medical Advisory Board to review complex cases. This board is composed of three licensed physicians appointed by the Director of Revenue. The law is administered through the DLB of the Missouri Department of Revenue. On-road testing of reported drivers is conducted through the Driver Examination Division of the Missouri State Highway Patrol (MSHP) utilizing a standardized operational test applied to all drivers.
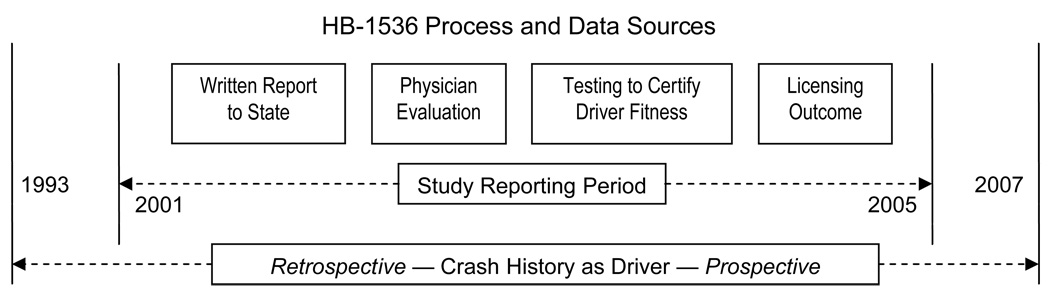
The HB-1536 process is depicted in Figure 1 along with boundary years for the crash investigation described in this paper.
Fig. 1.
Crash study time period and medical fitness reporting and evaluation process.
This effort to evaluate the efficacy of HB-1536 is an outgrowth of an educational initiative to train physicians and other healthcare professionals about MFD assessment and reporting procedures (Meuser et al., 2006). An important goal was to change behavior, such that health professionals would incorporate evaluation of MFD into regular patient care activities.
This research addresses a number of questions concerning reported individuals: Who initiates reports, what are the prevalent medical conditions noted, what is the crash history of reported drivers and how does it compare to controls, what are the licensing outcomes from the process?
2. Data Collection
Reports under HB-1536 are maintained and stored at the Department of Revenue (DOR), Jefferson City, Missouri. Most data for this project were retrieved from archival sources: microfilm images (reports received 2004 and before) and scanned images (reports from 2005+).
Figure 1 depicts the HB-1536 reporting process and the primary data sources: report of a MFD concern, physician’s medical evaluation, on-road testing, licensing outcome, and crash history. HB-1536 was implemented in 1999, but with few reports in the first two years. From January 2001 through December 2005, 5,362 drivers were reported to DOR as potentially medically unfit to drive. The majority, 4,987 (93%), were age 50 and older at the time of report, and 4,134 (83%) were age 70 and older. This research focuses on those 50 and older, and material from 4,100 cases (87% of all cases) were reviewed. Some cases were omitted due to time constraints for data collection. First, a pilot set of 389 cases was used to develop and test coding schemes, reliability and stability of hand data entry, etc. (Meuser et al., 2008).
Approximately 15,000 pages were reviewed. The average time to build a case packet and hand enter data was 20 minutes; thus, the 4,100 case sample required 1,350 person hours. Codes were assigned to each individual for confidential tracking and data analysis. Only coded, de-identified data were taken off-site for analysis. A detailed description of the data collection effort is given by Meuser et al. (2008).
The DOR assisted in developing a control sample of non-reported drivers. The DOR extracted gender and birth year for licensed drivers born during selected weeks resulting in a large pool of non-reported drivers. Cross-classifications of birth year and gender were tabulated. The year-gender combination with the fewest individuals in the control group was 2.8 times larger than the same combination in the reported sample. A uniform random distribution was used to sample from the control pool to yield a 2.8:1 control sample that has the same birth year and gender distribution as the reported drivers, resulting in a control sample of 11,615 unreported drivers, born 1900–1955.
Police and highway patrol officers in Missouri complete reports for crashes involving death, injury, or property damage in excess of $500. The reports include crash, driver, road, and environmental characteristics. Data were obtained for reported drivers and controls for crashes from January 1993 through the first quarter of 2007. In some instances, complete years, 1993–2006, were used for analysis. Older adults are at risk for chronic-progressive medical conditions, and this timeframe was chosen to allow retrospective review of crash history during the years leading up to HB-1536 reporting, and also to quantify the impact on public safety post license revocation.
3. Data Description
When a driver is reported under HB-1536, the DOR initiates a “Department Action” (DA) against the driver’s license within one to two weeks. A notification letter is mailed and a DA date is assigned. The majority of reported drivers (92%) had one DA during 2001–2005. To standardize the analyses, the first DA date (DA1) served as the de facto report date.
Basic demographic, driver licensing, and crash data are summarized in Table 1. Means were evaluated with t-tests. Frequency differences were evaluated with nonparametric tests (e.g., χ2). Due to the large sample size, findings are considered statistically significant when at the p < 0.001 level, indicated by * in the tables.
Table 1.
Characteristics of reported and control samples
| Reported (R) 2001–2005 |
Control (C) 2.8:1 Match to Reported Cases on Gender & Birth Year |
||
|---|---|---|---|
| n = 4,100 (2,553 living 12/06) |
n = 11,615 (7,770 living 12/06) |
||
| Median Birth Year | 1922 | ||
| (Mean Age at DA 1 for Reported Drivers) | 80 (9.3) | ||
| Male Gender | 55.1% | ||
| Living Driver (as of ~12/06 – ~3/07) |
62.4% | 66.9% | |
| R=C* | |||
| Last License Class = F (non-commercial) |
95.6% | 93.3% | |
| Urban Location | 68% | Unavailable | |
| Any (1+) Listed Traffic Convictions | 8.7% | Unavailable | |
| Required to Take Driving Skills Test | 26% | NA | |
| Participated in Driving Skills Test | 14% 562 or 57% of those required |
NA | |
| Retained Valid Driver License Subsequent to HB-1536 Reporting (2001–2005) | 3.5% | NA | |
| Valid Driver License (of living drivers in 12/06 only) |
2.4% | 67% | |
|
Any Crash as Driver (1993–2007) |
48.7% | 27% | |
| R>C* | |||
| Multiple (2+) Crashes as Driver (1993–2007) | 20.7% | 7.3% | |
| R>C* | |||
| Crash as Driver—Before Reporting Period (1993–1999) | 27.3% | 18.2% | |
| R>C * | |||
| Crash as Driver—Proximate to Reporting Period (2000–2007) | 33.5% | 12.4% | |
| R>C* | |||
| Crash as Driver—Recent before report (0–6 months before Department Action 1) | 31% | NA | |
Statistically significantly different at the p < 0.001 level. R=C indicates reported not statistically significantly different from controls. R>C indicates reported statistically significantly greater than controls.
NA indicates Not Applicable.
Reported drivers were of advanced age, with a mean age of 80 years (Range 50–105, Standard Deviation = 9), and disproportionately male (55%). Birth years ranged from 1896–1955, with a median birth year of 1922. Just one reported individual was born before 1900. Mortality was high, such that 38% were listed as deceased in December 2006. Mortality in the control sample was lower at 33%.
The majority (95%) possessed standard Class F (e.g., passenger car, pick-up truck, sport-utility vehicle), non-commercial driver licenses. Few (8.7%) had prior convictions for traffic violations. Two thirds (68%) lived in urban areas when last licensed to drive. The crash data results in Table 1 show that crash involvement for controls is close to half of those for reported drivers. Crash results are discussed separately in a later section.
Gender differences in traffic safety have previously been noted (e.g., Ulfarsson and Mannering, 2004). Table 2 shows gender differences for reported and control drivers. Mortality was greater in males, who also had more convictions and were more likely to have been involved in a crash when driving. Living males were more likely to retain a valid license to drive.
Table 2.
Gender differences in reported and control samples
| Reported (R) 2001–2005 |
Control (C) 2.8:1 Match to Reported Cases on Gender & Birth Year |
||||
|---|---|---|---|---|---|
| n = 4,100 (2,553 living 12/06) |
n = 11,615 (7,770 living 12/06) |
||||
| Male | Female | Male | Female | ||
| Median Birth Year (Mean Age at DA 1) |
1922 80 (SD = 9.5) |
1922 80 (9) |
1922 | 1922 | |
| Age Difference NS | |||||
| Living Driver (as of ~12/06 – ~3/07) |
55% | 71.5% | 61.7% | 73% | |
| R,C – F>M* | |||||
| Urban Location | 66.7% | 69.5% | Unavailable | Unavailable | |
| R – F>M* | |||||
| Any (1+) Listed Traffic Convictions | 11.5% | 5.3% | Unavailable | Unavailable | |
| R - M>F* | |||||
| Valid Driver License (of living drivers in 12/06 only) |
3% | 1.8% | 69% | 66% | |
|
Any Crash as Driver (1993–2007) |
52.8% | 43.6% | 30% | 23.4% | |
| R,C – M>F* | |||||
| Multiple (2+) Crashes as Driver (1993–007) | 23.7% | 16.9% | 8.9% | 5.5% | |
| R,C – M>F* | |||||
| Crash as Driver—Before Reporting Period Driver (1993–1999) | 30.1% | 23.8% | 20.6% | 15.2% | |
| R,C – M>F* | |||||
| Crash as Driver—Proximate to Reporting Period (2000–2007) | 36.3% | 30.1% | 13.8% | 10.8% | |
| R,C – M>F* | |||||
| Crash as Driver—Recent Before Report (0–6 months before Department Action 1) | 32% | 30% | NA | NA | |
| NS | |||||
Statistically significantly different at the p < 0.001 level; NS not statistically significantly different. R,C indicates both reported and controls. F>M (M>F) indicates females (males) are statistically significantly greater than males (females). NA indicates Not Applicable.
We tabulated medical condition categories that were identified across all report sources (i.e., the condition can have been reported by a physician, police officer, family member, etc.). The mean number of health conditions for reported drivers was 1.6 (Range 0–8, Standard Deviation = 1.4). The prevalent medical conditions were: dementia/cognitive (45%), vision (31%), musculoskeletal/neuromuscular (28%), disorders of consciousness (16%), cardiac/cardiovascular (12%), brain insult/tumor/stroke (10%), psychiatric (8%), and alcohol/drug abuse (3%). Future research will investigate medical conditions in detail.
4. Medical Impairment Reporting Results
HB-1536 was developed, in part, to encourage identification and reporting of medically-at-risk drivers by physicians and other health professionals. During 2001–2005, more than half of all reports were submitted together by police officers (30%) and license office staff (27%). Most police-initiated reports (87%) were made pursuant to a crash, dangerous action, and/or traffic violation involving the reported driver. Reports from license office staff, in contrast, focused on observations of cognitive and physical function, and included concerns about balance/ambulation (33%), confusion (15%), and appearance of frailty (15%).
Physicians (20%) and family members (16%) were the sources for most other reports. While concerns about driving were noted by these sources, their primary concerns were related to medical impairments (e.g., specific medical diagnosis, observed confusion).
To retain a valid license, reported drivers must in most cases submit a physician’s evaluation within 30 days (60 days if driver requests an extension). Depending on physician recommendation, the reported driver may at this point be allowed to keep the license, be subject to immediate license revocation, license restriction, or be required to participate in written and/or on-road testing through the MSHP. Test results are sent to DOR for a final determination on license status.
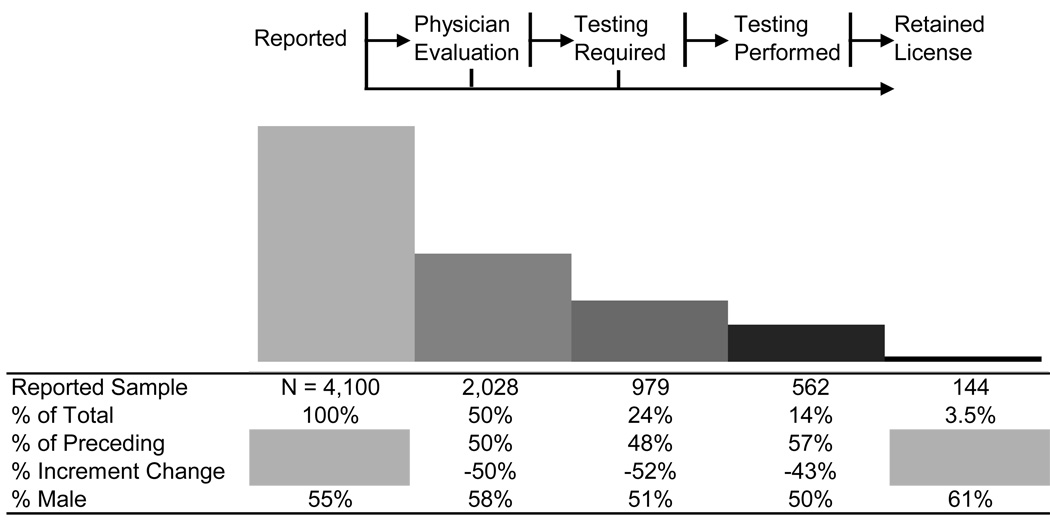
Figure 2 summarizes what occurred at each step in the HB-1536 process in 2001–2005, starting with the sample of 4,100 reported drivers and ending with the 144 (3.5%) who retained a valid license in the end.
Fig. 2.
Overview of medical impairment reporting results in Missouri, 2001–2005.
About half of the sample of reported drivers failed to arrange and submit the required physician evaluation and were subject to immediate license revocation. Possible reasons for this early attrition include failure of memory for the initiation of a response (i.e., forgetting that the notice ever came), pressure from family members to cease driving, self-awareness of an impairment, and trepidation (or even intimidation) concerning the impending evaluation process. Apart from crash information, driving history data were not available for either reported or control drivers. It cannot be seen how many continued to drive without a license, or ceased driving of their own accord before HB-1536 action. With so many dropping out, it cannot be concluded that all reported drivers were unfit. Although beyond the scope of this paper, an investigation of differences in crash characteristics between those that complete the HB-1536 process vs. those dropping out is important to pursue in further studies.
Based in part on physician recommendation for 2,028 individuals participating in the physician evaluation and diagnosis of medical impairment, DOR revoked the licenses of about half of those that turned in a physician evaluation. The others (979) were directed to participate in driver license testing through the MSHP to certify fitness to drive. Many individuals chose or were forced by circumstances of life and function to drop out at this stage. Missouri physicians recommended on-road testing alone in 38% of the cases they reviewed, testing with license restriction in 6% of cases, and license restriction alone in 5% of cases. There are a number of potential reasons for this emphasis on testing over restriction. On the physician form, the section on license restriction is perhaps overlooked at the end of the form. Also, physicians lack education and training concerning the evaluation of fitness-to-drive and restricted licensure. Physicians that noticed the section might not have felt competent to complete it and the section lacks specific instruction. Many patients may lack sufficient insight (e.g., dementia) or may be too medically compromised to comply with restrictions if given. Further studies are needed to evaluate the utility and feasibility of license restriction, whether it would be helpful in groups with a high prevalence of dementia and other co-morbid conditions, and how physicians can be trained and otherwise encouraged to consider such options.
Just 14% (562) of those originally reported participated in driver license testing (combination of written and on road testing). These individuals were allowed up to three attempts to pass either written or on-road (a total of six theoretical maximum testing sessions for drivers that fail the written twice and pass on the third attempt, then have three attempts at the on-road test) with the following results:
Examination session 1 (n = 562) — 14 (2.5%) passing,
Examination session 2 (n = 417) — 6 (1%) passing,
Examination session 3 (n = 324) — 4 (<1%) passing,
Examination session 4 (n = 49) — 0 passing,
Examination session 5 (n = 21) — 0 passing.
Only 3.5% (144) retained a valid license subsequent to the HB-1536 process. This is more than those passing the driver license testing since a few reported drivers were directly approved by DOR at the initial report, a few were approved by DOR subsequent to the physician evaluation. However, the end result is that nearly all drivers reported under HB-1536 from 2001–2005 moved into driving retirement.
Given the advanced age of this sample, current demographics reveal that older aged females outnumber males ~60% to 40% in Missouri, yet the sample was 55% male. Males are more likely to be licensed drivers (FHWA, 2006), however, and are reported to travel greater distances than females (Bergdahl, 2005). Additionally, males tend to have more chronic medical conditions (e.g., cardiac, pulmonary) than females when matched for similar ages (Wray and Blaum, 2001).
When tracing the proportion of males across the process (Figure 2), males were more likely to have a physician evaluation submitted, but they were less likely to have an opportunity of on-road testing. Males had a higher reported mean number of health conditions (1.7 vs. 1.4). In the end, however, males were more likely to pass and retain a valid license to drive.
Advancing illness and death were likely contributing factors in why so many dropped out at each step; 38% were deceased when mortality data were obtained in December 2006, almost a year after the reporting period. Of the 144 individuals who retained a valid license subsequent to HB-1536 reporting, 75 were still living at this time.
5. Traffic Crash Histories
Crash histories were tabulated for all reported drivers. About 28% (1,150) had one crash from 1993–2007. One in five (19%) had 2–4 crashes; a handful (2%) had 5–11 crashes. Looking at Table 1 for comparisons between reported drivers and controls, about half (48.7%) of the reported sample had a crash history (at least one crash as driver) during 1993–2007 compared with 27% of the controls. About 21% of reported drivers had two or more crashes in that time period, compared to 7% of controls. When exploring the first half of the time period (1993–1999), 27% of reported drivers had at least one crash compared to 18% of controls. In the more recent years, 2000–2007, 33% of reported drivers had at least one crash compared to 12% of controls. The share of reported drivers in crashes increased proximate to the reporting period, while it decreased for controls. Some of the reported drivers were reported at least in part due to a crash or crashes; about 31% of them experienced a crash as a driver within 6 months before DA1 (i.e., report date). A recent crash or on-road incident was a precipitating factor in most police-initiated reports, and this may explain part of the difference in crash involvement between groups. While this might account for the differences in the reporting year, it cannot account for differences going back several years.
When considering gender (Table 2), males were more likely to have had a crash as a driver than females. Among those with a positive crash history, males had a mean number of crashes of 1.83 vs. 1.61 for females (p < .001, t-test). A greater percentage of males were involved in crashes every year in the observation period, and this pattern was also true for controls.
Crashes did not differ in overall severity between reported and control drivers. We compared crashes closest in time to the DA1 date in reported drivers to most recent crashes in controls. High severity crashes were those involving a fatality or a major disabling injury per police designation. All others were considered of low severity. Six percent of reported driver crashes were of high severity vs. 5% in control drivers. This difference was not statistically significant. Two-vehicle incidents were prominent and statistically similar in both groups: 78% reported drivers vs. 82% controls. For both groups, the same proportion of crashes (32%) occurred at intersections.
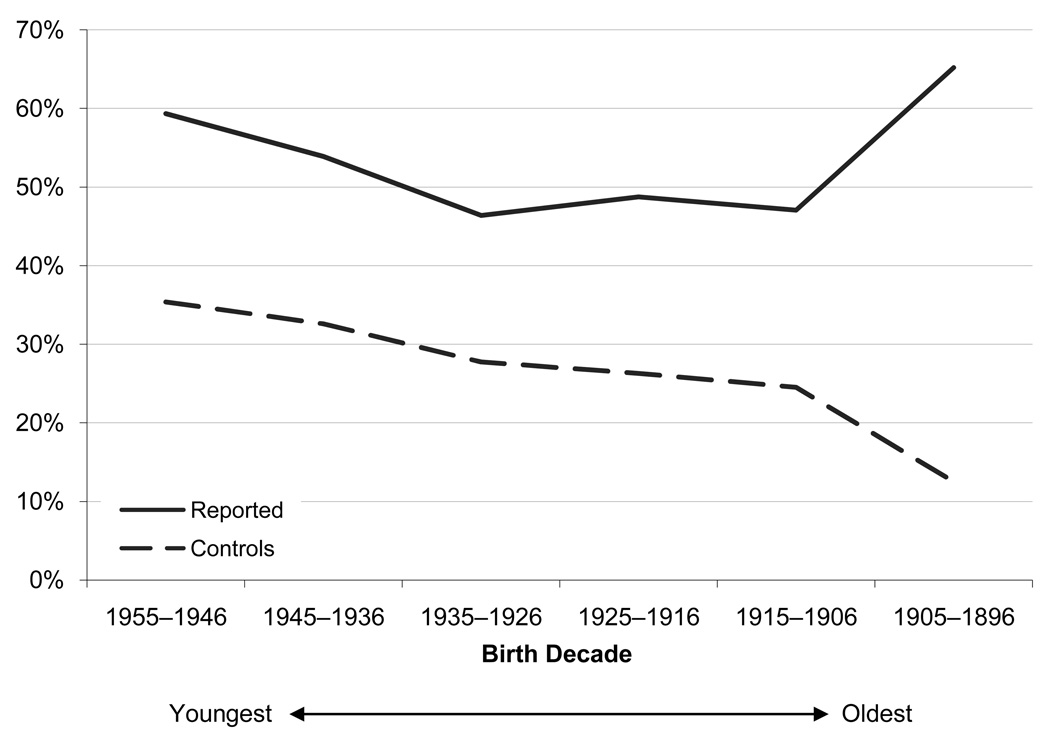
Figure 3 shows involvement in at least one crash by birth year decade. Crash history in reported drivers was double (or more) that of controls. A U-shaped curve is shown in Figure 3, such that there was a greater history of crashes among younger (~50–60) and older (85+) age groups, but just in the reported driver sample. History of crashes tails off in Figure 3 as age increases in controls.
Fig. 3.
Percentage in crashes by birth year range (1993–2006).
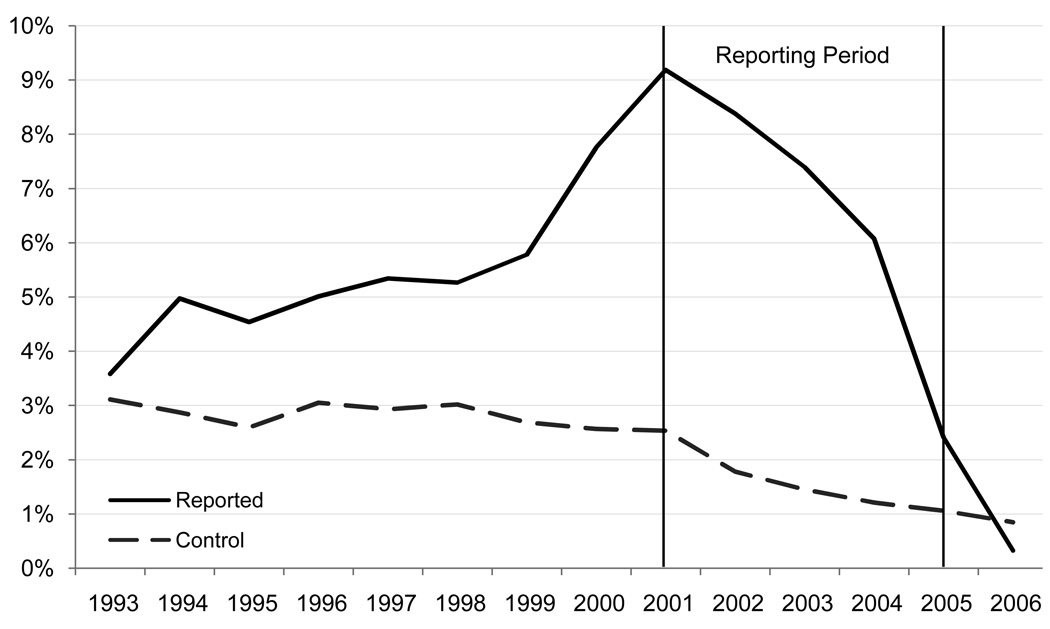
Figure 4 shows the percentage of drivers involved in at least one crash for the years 1993–2007. This started at 4% in 1993 for reported drivers and increased to 9.3% in 2001 when reporting began vs. just 2.2% of control drivers—a fourfold difference. It is important to note that crash involvement is comparable between groups in the years 1993–2000. However, in 2001 the effect of reporting begins. The percentage of reported drivers in crashes dropped steadily after 2001, presumably due to driving retirement as licenses were revoked and the impact of mortality. The share of control drivers in crashes starts at a 3%, holds relatively steady until 1998 and then gradually declines, likely due to driving retirement or reduction and mortality.
Fig. 4.
Percentage in crashes by year (1993–2006).
6. Conclusions
Identifying medically impaired drivers who are at risk for a motor vehicle crash is an important traffic safety concern. This paper describes an investigation into the State of Missouri’s HB-1536 voluntary reporting law during 2001–2005. The law is non-specific as to age, but the evidence shows that reported drivers were generally elderly, frail, and medically compromised. Dementia/cognitive impairment was most common, identified in 45% of cases.
Input from police officers accounted for the largest share of reports (30%). The high rate of reporting by police officers, while important, indicates there is potential to shift the proportional burden to other stakeholders. Police officers file reports when a crash, violation, or abnormal driving behavior has occurred, indicating that public safety may already be compromised. Procedural and educational initiatives to enhance reporting by physicians, other health/service professionals, and family members could have a positive impact on public safety. Early recognition of medical impairment “red flags”, along with the knowledge and motivation to intervene with respect to driving, could mean that more drivers are reported when less medically compromised and before crashing becomes a major factor.
The crash histories spanning 1993–2007 show a much larger percentage of the reported drivers in crashes (48.7%) than the controls (27%). When studying crashes on a year-by-year basis, crash involvement of reported drivers is elevated going back to 1993, eight years before the reporting period. There are a number of possible explanations for this long-term difference in crash history. The data suggest that reported drivers were medically impaired and could have differed from controls in this regard for years prior to the reporting period. It is possible that reported drivers had higher exposure (e.g., distance driven per year) but we believe it unlikely. This is because the mortality difference between these groups suggests greater fragility on the part of reported drivers, which makes it less believable that they consistently drove significantly more than the control sample.
The number of controls that crashed each year dropped over time, presumably due to driving reduction, driving retirement, driving behavior change, and mortality. The percentage of reported individuals in crashes peaked in 2001 (when reporting for this group began) at 9.3% vs. only 2.2% for controls—a fourfold difference. The percentage of reported individuals in crashes fell steeply after that, due mainly to the HB-1536 process. Few crashes occurred in the reported group in 2006 after the reporting period. Crash data indicate that, once reported, medically impaired individuals generally ceased to be active drivers, and public safety was thereby enhanced.
Of the reported drivers, 96.5% retired from driving at some step in the process and only the most determined and/or functional were able to pass physician evaluation, written and/or on-road testing to retain a valid license to drive. HB-1536 was an effective tool for driver de-licensing in 2001–2005, operating as a package of steps and interventions to encourage driving retirement in older individuals with medical impairment. However, it is possible that a portion of this sample was not at an increased risk and stopped driving prematurely. It is possible that some reported drivers found the HB-1536 process intimidating, starting with a formal letter requiring physician evaluation in 30 days. Half dropped out at this first hurdle. The final hurdle—written and/or on-road testing—was similarly challenging for the drivers, with most failing. Such failures may have resulted from one or more factors, including compromised health (physical and/or cognitive), performance anxiety, and ageist bias on the part of the driver examiner. Another potential concern is the one-size-fits-all approach to testing used in Missouri and in other states. Might more have passed if an age-adjusted, functional approach to testing was followed?
More studies are needed to determine how on-road tests might be tailored to different populations and the on-road tests’ value for predicting future at-fault crashes. Meanwhile, functional based testing holds promise for more cost-effective measures in assessing driving outcomes (Staplin, et al 2003).
Self-regulation and license restriction are other important areas for education and intervention research. Whereas data from this study have bearing on these topics, the focus was limited to the reporting, testing, and primary licensing decisions. One outcome of this work, however, is a renewed commitment on the part of the Missouri DLB to review its procedures and enhance submission forms used by physicians and others in support of more comprehensive case review and decision-making. The option for restricted licensure—in lieu of license revocation—is a topic for consideration and revision.
Acknowledgments
This project was funded in part by the AAA Foundation for Traffic Safety, with additional support from the Washington University Alzheimer’s Disease Research Center (NIA P50-AG05681) and the Washington University Friedman Center for Aging (NIA Grant K07AG21164).
The authors extend their gratitude to the Missouri Department of Revenue (especially Trish Vincent, Norma Hensiek, Brad Brester, Julie Allen, Roger Doerhoff, Carisa Bunting, Laura Scott, Gina Wisch, Lynn Armour, Charlotte Braun, John Sappington) and the Missouri State Highway Patrol (especially Ronald Beck, William Nelson, Rhonda Czarnecki, Gary Moore, Cynthia Anders, Arie Hoard, Reita Cyrus, Gerry Estes) for their support of this project.
We extend special thanks to Scott Osberg, PhD, AAA Foundation for Traffic Safety; John C. Morris, MD, Director of the Washington University Alzheimer’s Disease Research Center; Mike Right, AAA Auto Club of Missouri; Carol Rodriguez, Alzheimer’s Association, St. Louis; Leanna Depue, PhD, Division of Highway Safety, Missouri Department of Transportation; Sheldon Suroff, Concerned Americans for Responsible Driving.
We thank the excellent researchers that contributed: Marla Berg-Weger, PhD, Saint Louis University; Patricia Niewoehner, OTR/L, CDRS, St. Louis VA Medical Center; Joon-Ki Kim, DSc, Korea Research Institute for Human Settlements; Peggy Barco, MS, OTR/L, Washington University in St. Louis; Katherine MacLean, MSW, Alzheimer’s Association, St. Louis. We thank our student assistants: Thomas J. Epplin-Zapf, Jessica Lester, Jami Croston, Jamin Barber, Donna Keller, Emily Kissel, Mathew Minn, Mimi Hillburg.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Thomas M. Meuser, Email: meusert@umsl.edu.
David B. Carr, Email: dcarr@im.wustl.edu.
Gudmundur F. Ulfarsson, Email: gfu@hi.is.
References
- Anstey K, Wood J, Lord S, Walker J. Cognitive, sensory, and physical factors enabling driving safety in older adults. Clinical Psychology Review. 2005;25:45–65. doi: 10.1016/j.cpr.2004.07.008. [DOI] [PubMed] [Google Scholar]
- Baldock MR, Mathias JL, McLean AJ, Berndt A. Self-regulation of driving and its relationship to driving ability among older adults. Accident Analysis and Prevention. 2006;8(5):1038–1045. doi: 10.1016/j.aap.2006.04.016. [DOI] [PubMed] [Google Scholar]
- Ball K, Owsley C, Stalvey B, Roenker DL, Sloane ME, Graves M. Driving avoidance and functional impairment in older drivers. Accident Analysis and Prevention. 1998;30:313–322. doi: 10.1016/s0001-4575(97)00102-4. [DOI] [PubMed] [Google Scholar]
- Bergdahl J. Sex differences in attitudes toward driving: a survey. Social Science Journal. 2005;42:595–601. [Google Scholar]
- Browning C, Sims J. Ageing without driving: Keeping older people connected. In: Currie G, Stanley J, Stanley J, editors. “No Way to Go: Transportation and Social Disadvantage in Australian Communities”. Victoria, Australia: Monash University Press; 2007. [Google Scholar]
- Carr DB. The older adult driver. American Family Physician. 2000;61(1):141–148. [PubMed] [Google Scholar]
- Charlton JL, Koppel S, O'Hare M, Andrea D, Smith G, Khodr B, et al. Influence of Chronic Illness on Crash Involvement of Motor Vehicle Drivers. Report 213. Victoria, Australia: Monash University Accident Research Centre; 2004. [Google Scholar]
- Christie R. Driver Licensing Requirements and Performance Standards Including Driver and Rider Training. Melbourne, Australia: National Road Transport Commission; 2000. [Google Scholar]
- Darzins P, Hull M. Older road users: issues for general practitioners. Australian Family Physician. 1999;28(7):663–667. [PubMed] [Google Scholar]
- Dobbs BM. Medical Conditions and Driving: Current Knowledge. Final Report, Association for the Advancement of Automotive Medicine, DTNH22-94-G-05297. Washington, District of Columbia: National Highway Traffic Safety Administration; 2005. [Google Scholar]
- Dobbs BM. Aging baby boomers: A blessing or challenge for driver licensing authorities. Traffic Injury Prevention. 2008;9:379–386. doi: 10.1080/15389580802045823. [DOI] [PubMed] [Google Scholar]
- Dobbs BM, Carr D. Screening and assessment of medically at-risk drivers. Public Policy & Aging Report. 2005;15(2):6–12. [Google Scholar]
- Federal Highway Administration. [Accessed June 24, 2008];Highway Statistics 2006. 2008 www.fhwa.dot.gov/policy/ohim/hs06/driver_licensing.htm/.
- Fildes BN. Future directions for older driver research. Traffic Injury Prevention. 2008;9:387–393. doi: 10.1080/15389580802272435. [DOI] [PubMed] [Google Scholar]
- Hakamies-Blomqvist L. Fatal accidents of older drivers. Accident Analysis and Prevention. 1993;25:19–27. doi: 10.1016/0001-4575(93)90093-c. [DOI] [PubMed] [Google Scholar]
- Hakamies-Blomqvist L. Aging and fatal accidents in male and female drivers. Journal of Gerontology Social Sciences. 1994;49:S286–S290. [PubMed] [Google Scholar]
- Langford J, Koppel S. Epidemiology of older driver crashes – Identifying older driver risk factors and exposure patterns. Transportation Research Part F. 2006;9:309–321. [Google Scholar]
- Lyman S, Ferguson SA, Braver ER, Williams AF. Older driver involvement in police reported crashes and fatal crashes: trends and predictions. Injury Prevention. 2002;8:116–120. doi: 10.1136/ip.8.2.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGwin G, Jr, Brown DB. Characteristics of traffic crashes among young, middle-aged, and older drivers. Accident Analysis and Prevention. 1999;31(3):181–198. doi: 10.1016/s0001-4575(98)00061-x. [DOI] [PubMed] [Google Scholar]
- Meuser TM, Carr DB, Berg-Weger M, Niewoehner P, Morris JC. Driving and dementia in older adults: implementation and evaluation of a continuing education project. The Gerontologist. 2006;46(5):680–687. doi: 10.1093/geront/46.5.680. [DOI] [PubMed] [Google Scholar]
- Meuser TM, Carr DB, Ulfarsson GF, Berg-Weger M, Niewoehner P, Kim J-K, Epplin-Zapf TJ, Barco P, MacLean K, Osberg S. Medical Fitness to Drive and a State Voluntary Reporting Law. Washington, DC: AAA Foundation for Traffic Safety; 2008. [Accessed October 22, 2008]. www.aaafoundation.org/pdf/MedicalFitnesstoDriveReport.pdf/ [Google Scholar]
- Michon JA. A critical review of the driver behavior models. What do we know, what should we do? In: Evans L, Schwing R, editors. “Human Behavior and Traffic Safety”. New York: Plenum Press; 1985. pp. 485–524. [Google Scholar]
- Molnar LJ, Eby D. Proceedings of the North American License Policies Workshop. Washington, DC: AAA Foundation for Traffic Safety; 2008. [Accessed September 3, 2008]. www.aaafoundation.org/pdf/LPWorkshopProceedings.pdf/ [Google Scholar]
- Morrisey MA, Grabowski DC. State motor vehicle laws and older drivers. Health Economics. 2005;14(4):407–419. doi: 10.1002/hec.955. [DOI] [PubMed] [Google Scholar]
- Odenheimer GL. Dementia and the older driver. Clinics in Geriatric Medicine. 1993;9:349–364. [PubMed] [Google Scholar]
- Odenheimer GL. Driver safety in older adults. The physician's role in assessing driving skills of older patients. Geriatrics. 2006;61(10):14–21. [PubMed] [Google Scholar]
- OECD. Ageing and Transport. Mobility Needs and Safety Issues. Paris, France: OECD Publications; 2001. [Google Scholar]
- Retchin SM, Anapolle J. An overview of the older driver. Clinical Geriatric Medicine. 1993;9:279–296. [PubMed] [Google Scholar]
- Rosenbloom S. OECD: Transport and Ageing of the Population. Paris, France: OECD; 2000. Report by the chairperson. [Google Scholar]
- Stalvey BT, Owsley C. The development and efficacy of a theory-based educational curriculum to promote self-regulation among high-risk older drivers. Health Promotion and Practice. 2003;4(2):109–119. doi: 10.1177/1524839902250757. [DOI] [PubMed] [Google Scholar]
- Staplin L, Lococo KH, Gish KW, Decina LE. Model Driver Screening and Evaluation Program & Maryland Pilot Older Driver Study. DOT HS 809581. Washington, District of Columbia: National Highway Traffic Safety Administration; 2003. [Google Scholar]
- Stutts JC, Stewart JR, Martell CM. Cognitive test performance and crash risk in older driver population. Accident Analysis and Prevention. 1998;30(3):337–346. doi: 10.1016/s0001-4575(97)00108-5. [DOI] [PubMed] [Google Scholar]
- U. S. Census Bureau. [Accessed October 17, 2007];Facts for Features. 2005 http://www.census.gov/Press-Release/www/releases/archives/facts_for_features_special_editions/004210.html/
- Ulfarsson GF, Mannering FL. Difference in male and female injury severities in sport-utility vehicle, minivan, pickup and passenger car accidents. Accident Analysis and Prevention. 2004;36(2):135–147. doi: 10.1016/s0001-4575(02)00135-5. [DOI] [PubMed] [Google Scholar]
- Wang CC, Kosinski CJ, Schwartzberg JG, Shanklin AV. Physician’s Guide to Assessing and Counseling Older Drivers. Washington, District of Columbia: National Highway Traffic Safety Administration; 2003. [Google Scholar]
- Wang C, Carr D. Older driver safety: a report from the older drivers project. Journal of the American Geriatrics Society. 2004;52:143–149. doi: 10.1111/j.1532-5415.2004.52025.x. [DOI] [PubMed] [Google Scholar]
- Wray LA, Blaum CS. Explaining the role of sex on disability: a population-based study. Gerontologist. 2001;41:499–510. doi: 10.1093/geront/41.4.499. [DOI] [PubMed] [Google Scholar]