Abstract
There is currently no treatment for the inherited motor neuron disease, spinal muscular atrophy (SMA). Severe SMA causes lower motor neuron loss, impaired myofiber development, profound muscle weakness and early mortality. Myostatin is a transforming growth factor-β family member that inhibits muscle growth. Loss or blockade of myostatin signaling increases muscle mass and improves muscle strength in mouse models of primary muscle disease and in the motor neuron disease, amyotrophic lateral sclerosis. In this study, we evaluated the effects of blocking myostatin signaling in severe SMA mice (hSMN2/delta7SMN/mSmn−/−) by two independent strategies: (i) transgenic overexpression of the myostatin inhibitor follistatin and (ii) post-natal administration of a soluble activin receptor IIB (ActRIIB-Fc). SMA mice overexpressing follistatin showed little increase in muscle mass and no improvement in motor function or survival. SMA mice treated with ActRIIB-Fc showed minimal improvement in motor function, and no extension of survival compared with vehicle-treated mice. Together these results suggest that inhibition of myostatin may not be a promising therapeutic strategy in severe forms of SMA.
INTRODUCTION
The motor neuron disease, spinal muscular atrophy (SMA), is a leading inherited cause of infant mortality. SMA is caused by mutation or deletion of the survival motor neuron 1 (SMN1) gene and deficiency of the SMN protein leading to loss of lower motor neurons (1,2). SMA is characterized by profound muscle weakness involving truncal and proximal, more than distal, limb muscles (3,4). Studies of muscle pathology in severe SMA patients and mice have shown widespread, small myofibers expressing an immature pattern of contractile protein genes (5–9). It has been debated whether this pathology results solely from denervation or whether SMN protein deficiency causes contributing intrinsic defects of muscle (10–14). It is unknown whether therapeutic interventions targeted to muscle could be effective for the treatment of SMA patients.
Myostatin belongs to the transforming growth factor (TGF)-β superfamily and negatively regulates skeletal muscle mass (15). Genetic deletion or natural loss-of-function mutations of myostatin in multiple species including mice, cattle, sheep, dogs and humans cause a marked increase in skeletal muscle mass due to hypertrophy and/or hyperplasia (15–20). Myostatin is produced primarily by skeletal muscle and circulates in the bloodstream as an inactive complex with its own propeptide and other endogenous inhibitors (reviewed in 21). Upon activation, the myostatin C-terminal dimer binds to the activin receptor type IIB (ActRIIB) on skeletal muscle and initiates an intracellular signaling cascade that results in translocation of a Smad complex to the nucleus and transcriptional activation of target genes such as myogenic regulatory factors (21,22).
Several endogenous inhibitors of myostatin have been identified including follistatin, FLRG and GASP-1 (23–25). Follistatin is a secreted glycoprotein that regulates the activity of a number of TGF-β family members and potently inhibits myostatin (23). Genetic deletion of follistatin is associated with muscle hypotrophy (26), while transgenic overexpression of follistatin in mouse muscle results in increased muscle mass (23). The quadrupling of muscle mass seen in transgenic mice overexpressing follistatin on the myostatin null background (27) indicates that follistatin stimulates muscle growth by additional mechanisms independent of myostatin inhibition.
Multiple synthetic myostatin inhibitors have been recently generated in efforts to capitalize on the therapeutic potential of stimulating muscle growth for human disease. These synthetic inhibitors have primarily included neutralizing antibodies to myostatin (24,28), modifications of the myostatin propeptide (29,30) and soluble ActRIIB (31), all of which increase post-natal muscle growth in mice. Soluble ActRIIB has shown the most remarkable effects on muscling with up to 60% increases in muscle mass within 2 weeks (31). Similar to the effects of follistatin, the stimulation of muscle growth by soluble ActRIIB is not secondary to myostatin inhibition alone as additional increases in muscle mass are obtained when treating myostatin null animals (31). Indeed, ActRIIB-Fc was found to bind with high affinity to GDF-11 and activin in addition to myostatin (32).
Multiple studies with mouse models of human disease suggest that inhibition of myostatin may be a promising therapy for both primary and secondary muscle diseases. Loss or blockade of myostatin signaling by genetic deletion (33), neutralizing monoclonal antibody (34) or inhibitory myostatin propeptide (29,30) ameliorates the disease features in the Duchenne and Becker muscular dystrophy mdx mouse model lacking dystrophin. Myostatin inhibition also improves some disease features of limb-girdle muscular dystrophy mouse models due to loss of calpain (35), gamma-sarcoglycan (36), delta-sarcoglycan (37) and caveolin-3 (38), but does not rescue mice with alpha-sarcoglycan (35) or laminin deficiency (39). Importantly, the first clinical trial of a neutralizing antibody to myostatin, MYO-029, in adult muscular dystrophies showed good tolerability further supporting the promise of this therapeutic strategy for humans (40).
Myostatin inhibition has also been investigated in denervating diseases in which muscle atrophy is presumed to be secondary to loss or dysfunction of motor nerve terminals. In SOD1G93A mice, a model of the adult motor neuron disease amyotrophic lateral sclerosis (ALS), administration of myostatin neutralizing antibodies (41), gene transfer of follistatin to muscle (42), myostatin knock-out and treatment with a soluble ActRIIB (32) improves muscle mass and motor function during the disease course, but does not prolong survival. Myostatin inhibition was also recently evaluated in an animal model of SMA. SMAΔ7 mice (hSMN2/delta7SMN/mSmn−/−), which express a reduced level of SMN protein and show early, severe motor weakness dying at 2 weeks of life (6), were treated with recombinant follistatin protein delivered by intraperitoneal injection. One of the three doses of recombinant follistatin tested was reported to increase survival and motor function of SMAΔ7 mice (43).
In order to further evaluate the therapeutic potential of myostatin inhibition in SMA, we evaluated the effects of blocking myostatin signaling in SMAΔ7 mice by transgenic overexpression of follistatin and post-natally by administration of a soluble activin IIB receptor (ActRIIB-Fc).
RESULTS
Altered expression of myostatin and follistatin in SMAΔ7 mice
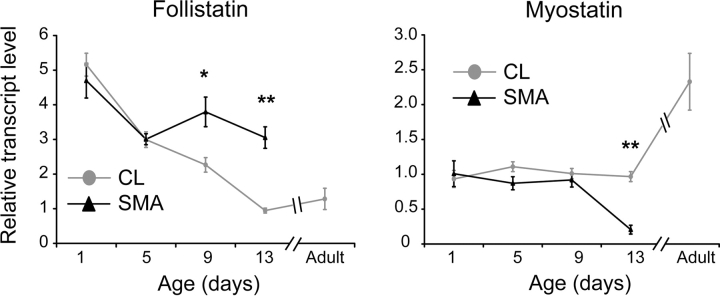
We examined the gene expression of follistatin and myostatin in hind-limb muscles of SMAΔ7 mice compared with control littermate (CL) mice at different ages by quantitative reverse transcription–PCR (qRT–PCR) (Fig. 1). In CLs, follistatin gene expression progressively decreased during the early post-natal developmental period, whereas myostatin gene expression was stable in the neonatal period and increased late in development. This data is in agreement with results showing an overall decrease of follistatin and an increase in myostatin protein expression in rats during the first several weeks of development (44). In SMA mice, there was no significance difference in gene expression at post-natal day 1 (P1) or P5 compared with CLs; however, follistatin was increased in SMA mice by 1.7-fold at P9 and 3.2-fold at P13, whereas myostatin was decreased in SMA mice by 4.7-fold at P13 (Fig. 1). These abnormalities may represent a compensatory response to muscle hypotrophy; a histological finding that we have previously shown is evident by P9 in these SMA mice (9). Consistent with this, follistatin and myostatin gene expression levels in muscle from P13 SMAΔ7 mice treated with trichostatin A (TSA), which increases myofiber size in SMAΔ7 mice (45,46), were more similar to normal neonatal muscle. The relative follistatin gene expression level was 1.68 ± 0.27 in TSA-treated P13 SMAΔ7 mice (a 1.6-fold increase compared with P13 CLs, P = 0.04) and the relative myostatin gene expression level was 1.38 ± 0.26 (not significantly different compared with P13 CLs, P = 0.20).
Figure 1.
SMA disease progression is associated with increased follistatin gene expression and decreased myostatin gene expression. Follistatin and myostatin transcripts were measured in all hind-limb muscles at different ages in SMA and CL mice and values were normalized for each transcript to the P13 CL value. Adult mice were approximately 6 weeks old [*P < 0.05, **P < 0.001, n = 5 mice per group except for P1 SMA (n = 3), P5 SMA (n = 3) and P9 CLs (n = 4)].
Overexpression of follistatin in muscle does not improve disease features of SMAΔ7 mice
Given that SMAΔ7 mice show myofiber hypotrophy, we postulated that early pre- and post-natal overexpression of follistatin might increase muscle mass and improve survival. Follistatin transgenic mice that express follistatin in skeletal muscle under control of the muscle-specific myosin light chain promoter, which is active starting at approximately embryonic day 9.5, have previously been shown to have a 3-fold increase in muscle mass compared with CLs in adulthood (23). Mice expressing the human follistatin transgene on the Y chromosome were bred to SMA (hSMN2+/+/SMNΔ7+/+/mSMN+/−) mice (see Materials and Methods). Subsequent intercrossing yielded the following experimental groups: female CLs (hSMN2+/+/SMNΔ7+/+/mSMN+/+ or +/−, Fst−), male CLs (hSMN2+/+/SMNΔ7+/+/mSMN+/+ or +/−, Fst+), female SMA (hSMN2+/+/SMNΔ7+/+/mSMN−/−, Fst−) or male SMA (hSMN2+/+/SMN Δ7+/+/mSMN−/−, Fst+) mice. Although this genetic strategy meant mice of the same genotype could not be gender-matched with control animals obtained from the same litters, gender has not previously been shown to significantly influence survival, weight or motor function in SMAΔ7 mice in our own experience (unpublished data) or in that of Butchbach et al. (47). Twenty-two of the resulting 194 offspring analyzed (11%) died at P1 or P2 and were not included in the survival analysis. Genotyping of available P1 and P2 carcasses showed the approximate expected ratios of SMA and CL mice. Of those mice surviving past P2, 19% were SMA indicating that there was not excessive pre-natal death of SMA mice.
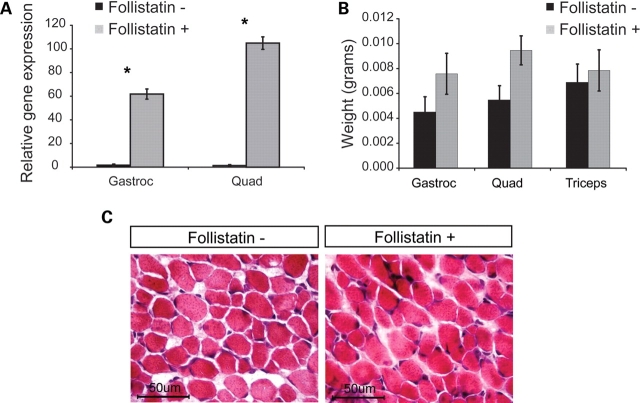
In order to verify transgenic overexpression of follistatin in these mice, we measured human follistatin transcript levels by qRT–PCR in the gastrocnemius and quadriceps muscles of P10 SMA and CL mice. Follistatin-positive mice overexpressed follistatin by approximately 40-fold in gastrocnemius muscles and 80-fold in quadriceps muscles compared with follistatin-negative mice (Fig. 2A). Increased follistatin gene expression in SMA mice resulted in a mild increase in skeletal muscle formation analyzed at P10. Muscle mass was increased by as much as 74% in the gastrocnemius, quadriceps and triceps muscles (Fig. 2B), but due to mouse variability this did not reach statistical significance. No difference in average myofiber diameter was observed (Fig. 2C). No change was seen in the mass of inguinal and scapular fat pads between follistatin-positive and -negative SMA mice (data not shown).
Figure 2.
Overexpression of follistatin does not substantially increase muscle mass in SMAΔ7 mice. (A) The extent of follistatin transgene expression was determined by qRT–PCR in P10 quadriceps and gastrocnemius muscles from follistatin-negative and -positive mice [*P < 0.005, n = 3 per group (2 CL and 1 SMA)]. (B) Weights of gastrocnemius (gastroc), quadriceps (quad) and triceps muscles in P10 follistatin-negative and -positive SMA mice. Only the quadriceps showed a significant trend of increased muscle weight in follistatin-positive SMA mice (P = 0.065). (C) Hematoxylin and eosin (H&E) stained cross sections of quadriceps muscle from a P10 SMA mouse (left) and a P10 follistatin-positive SMA mouse.
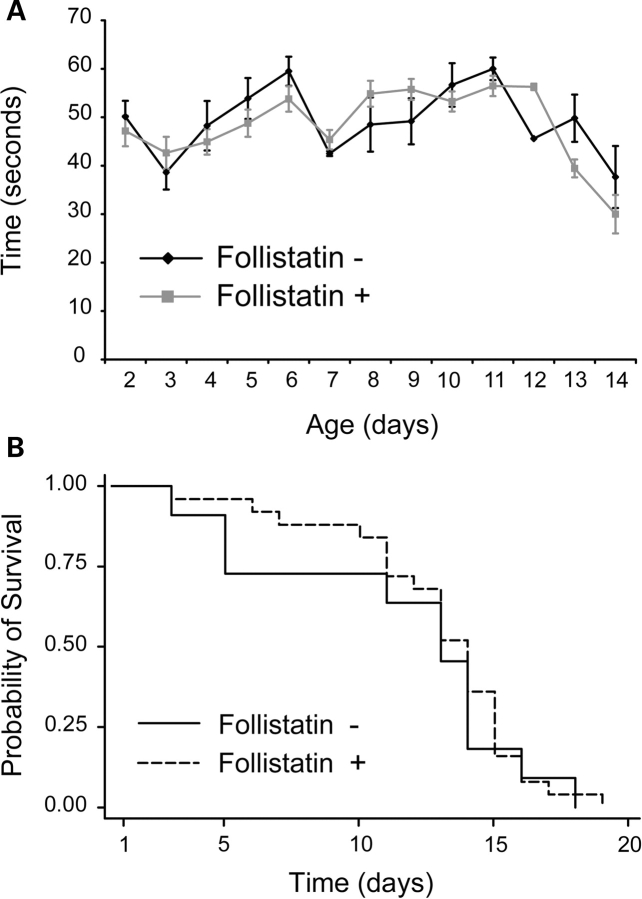
In order to examine whether follistatin overexpression in muscle improved motor function in SMA mice, we measured righting time. SMA mice overexpressing follistatin showed neither an improvement in total righting time (Fig. 3A), nor an improvement in the fraction of mice able to achieve any ability to right during the two trials [a measure recently used by Rose et al. (43)] (data not shown). In a hind-limb suspension test, SMA mice overexpressing follistatin showed no improvement in any of the three scoring parameters: average position score, total number of pulls and latency to fall (Supplementary Material, Fig. S1). Finally, the survival of SMA mice was unaffected by follistatin overexpression (Fig. 3B, Log rank P = 0.6).
Figure 3.
Overexpression of follistatin does not improve disease features of severe SMA mice. (A) Average total righting time in follistatin-negative (n = 8) and follistatin-positive SMA mice (n = 17). (B) Kaplan–Meier survival curves comparing follistatin-negative and follistatin-positive SMA mice. Median survival in follistatin-negative SMA mice was 13 and median survival in follistatin-positive mice was 14 (Log rank P = 0.6, n = 11 follistatin-negative, 25 follistatin-positive SMA mice).
ActRIIB-Fc treatment does not rescue SMAΔ7 mice
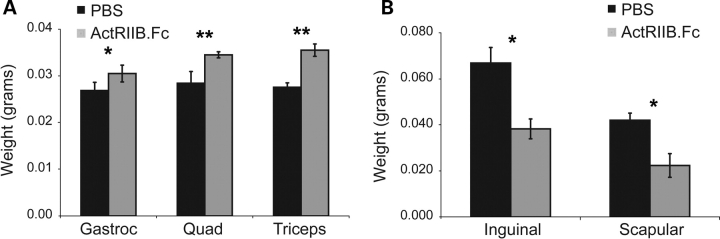
Previous studies have shown that preparations of soluble ActRIIB have dramatic and rapid effects on normal adult skeletal muscle (31) and improve muscle function in the SOD model of ALS (32). In order to evaluate the efficacy of this treatment in normal neonatal mice, we treated CL mice with a dose of 10 mg/kg every 3 days starting at P2 for 2 weeks. This dose was selected, because it has shown efficacy in a previous study in adult animals (32). Average total mouse weight at P15 was equivalent between vehicle and ActRIIB-Fc-treated mice (8.61 ± 0.17 and 8.82 ± 0.58 g, respectively). We compared muscle weights in ActRIIB-Fc and vehicle-treated mice at P15 and found an increased muscle weight of 20% in the gastrocnemius muscle (P = 0.048), 31% in the quadriceps muscle (P = 0.002) and 27% in the triceps muscle (P = 0.001) (Fig. 4). Fat pad weight showed a decrease in ActRIIB-Fc-treated animals of 39% in inguinal white fat pads (P = 0.014) and 46% in scapular white fat pads (P = 0.012) (Fig. 4A). There was no difference in the scapular brown fat weights between drug and vehicle-treated mice (data not shown).
Figure 4.
ActRIIB-Fc increases muscle mass and decreases fat mass in neonatal mice. CLs were treated with ActRIIB-Fc for 2 weeks. Muscle (left) and fat (right) weights from CL mice treated with vehicle (n = 6) or ActRIIB-Fc (n = 5) (*P < 0.05, **P < 0.005).
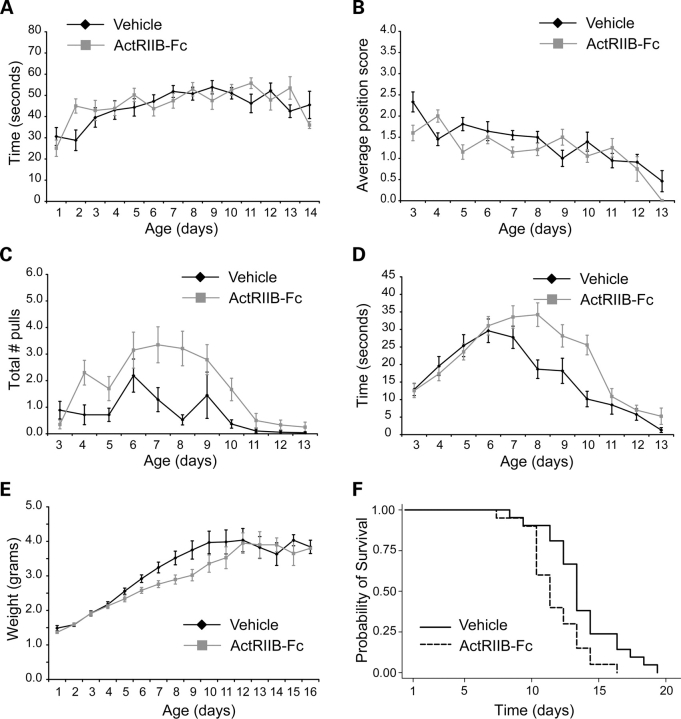
To determine if ActRIIB-Fc could ameliorate disease features of SMAΔ7 mice, we treated SMA mice with 10 mg/kg or vehicle starting at P2. Righting time and position score on the hind-limb suspension test showed no improvement in treated mice (Fig. 5A and B), but the total number of pulls and the total latency to fall time were increased in mice treated with ActRIIB-Fc compared with vehicle-treated mice (Fig. 5C and D). This may indicate that ActRIIB-Fc treatment resulted in modest increase in hind-limb strength between P7 and P10, however, ActRIIB-Fc-treated mice also showed a mild reduction in total body weight during this time period, which could account, at least in part, for the change in motor function (Fig. 5E). Survival was mildly decreased in ActRIIB-Fc compared with vehicle-treated mice (ActRIIB-Fc median = 11 and vehicle median = 13, Log rank P = 0.008) (Fig. 5F). In order to explore whether either a higher or lower dose of ActRIIB-Fc might be more efficacious in SMA mice, we treated additional cohorts with doses of 5 and 60 mg/kg. A similar decrease in survival was seen in mice treated with these two other doses compared with vehicle-treated mice (Supplementary Material, Fig. S2).
Figure 5.
ActRIIB-Fc does not extend survival of SMA mice. (A) Average total righting time, (B) average position score, (C) total number of pulls, (D) total latency to fall time on the hind-limb suspension test, (E) weights and (F) Kaplan–Meier survival curves of vehicle-treated (n = 21) and ActRIIB-Fc-treated SMA mice (n = 20) (Log rank P = 0.008).
DISCUSSION
We have examined the therapeutic potential of myostatin inhibition for SMA in a severe mouse model using two independent strategies, both of which have been previously demonstrated to effectively increase muscle mass in normal and diseased animals. In contrast to a recent study reporting an increase in survival and motor function in SMAΔ7 mice with injection of recombinant follistatin protein (43), we observed no extension of survival of SMAΔ7 mice overexpressing follistatin in muscle and a decrease of survival of SMAΔ7 mice treated with ActRIIB-Fc. Myostatin negatively regulates muscle growth by inhibiting the proliferation and differentiation of muscle progenitor cells and by inhibiting protein synthesis (reviewed in 21). In the absence of myostatin, muscle regenerates more robustly (48,49). We postulated that myostatin inhibition might be particularly effective in SMA because arrested myofiber growth, whether due to early denervation or intrinsic defects of SMN-deficient muscle (10–13), is likely to be a significant cause of muscle weakness in SMA patients. Pathological studies of human type I SMA muscle show very small, rounded muscle fibers, which are similar in appearance to developing myotubes (5). In SMAΔ7 mice, myofibers are small and immature before there is overt denervation (9). These observations suggest that SMA myofibers are impaired in their normal maturation and strategies that activate muscle growth could potentially increase myofiber size, muscle mass and strength.
SMAΔ7 mice showed minimal improvement in motor function and no improvement in survival when myostatin was inhibited by two different strategies in our study. This was surprising given the observations that inhibition of myostatin, including by ActRIIB-Fc, improved muscle function in the motor neuron SODG93A mouse model (32). One explanation for the difference in response between the mouse models may be the developmental age at which these diseases present. Myofiber size normally increases very rapidly during the neonatal period with the diameter of the myofiber influencing its contractile strength (50). During this period, we demonstrated that in normal mice, follistatin gene expression is high and myostatin expression is low relative to adults. Inhibition of the myostatin pathway in the neonatal period may have less effect on muscle mass than in the adult animal. Support for this hypothesis includes our observation that neonatal myostatin null mice (P10) have increased muscle weights of 45% (myostatin null = 0.015 ± 0.002 g versus WT = 0.010 ± 0.002 g, P = 0.06) in the gastrocnemius muscle and 76% (myostatin null = 0.022 ± 0.002 g versus WT = 0.013 ± 0.001 g, P = 0.0002) in the quadriceps muscle; whereas adult myostatin knock-out mice demonstrate increases of greater than 200% in these muscles (15). Furthermore, ActRIIB-Fc treatment of P10 control mice resulted in an increase of muscle weights of only 20–31% at 2 weeks, whereas increases of 35–49% in 2 weeks are seen in normal adult mice with a different preparation of soluble ActRIIB (31). These studies may suggest that neonatal mice have less capacity for muscle growth in response to myostatin inhibition compared with adult mice. In SMA mice, this is likely further exacerbated by an increase in follistatin and a decrease of myostatin gene expression that occurs in the late stages of the SMAΔ7 disease course (Fig. 1).
Myostatin blockade has been reported to be ineffective in the dyW/dyW mouse, a mouse model of congenital muscular dystrophy due to merosin deficiency (MDC1A) (39). In this very severe form of muscular dystrophy, dyW/dyW mice typically die at 3–6 weeks of age. Myostatin knock-out in dyW/dyW mice resulted in a further reduction of survival. Although muscle mass was increased in these mice, fat mass was substantially reduced exacerbating a baseline reduction of fat in these animals (39). Myostatin is expressed in adipose tissue and it has been previously reported that adult myostatin null mice are lean with an estimated 70% reduction in total fat stores (51). Adequate fat stores are particularly crucial in the neonatal period as brown fat is crucial for thermoregulation in neonates (52,53). In our study, follistatin overexpression restricted to muscle did not alter fat weights, but systemic treatment with ActRIIB-Fc did cause a substantial decrease in white fat pad weights. Given that white fat stores are already reduced by 2–6-fold and brown fat stores are reduced by 2-fold in P10 SMA mice compared with CLs (personal observation), we postulate that the further reduction of fat induced by ActRIIB treatment resulted in increased mortality similar to the experience in dyW/dyW mice. The effects of myostatin blockade on adipogenesis need to be carefully considered in severe SMA patients who are often malnourished (54).
Like myostatin blockade, histone deacetylase (HDAC) inhibitors have shown efficacy in muscular dystrophy animals models (55). This effect is thought to be mediated by induction of follistatin gene expression in muscle with resulting myostatin blockade, activation of satellite cells and myofiber regeneration (56). We have previously shown that the HDAC inhibitor, TSA, can substantially extend survival and improve motor function of severe SMA mice (45,46). The results of the current study provide evidence that the beneficial effects of TSA in SMA mice are likely independent of follistatin induction in muscle.
Here, we demonstrate that myostatin blockade is not beneficial in a severe mouse model of SMA. The inhibitory effects on adipogenesis may outweigh the minimal increases of muscle mass that are achievable with myostatin blockade in the neonatal period. It is possible that the lack of benefit is specific to mice, which have distinct fat stores compared with humans, or to this particular, severe model of SMA. Further investigations in other animal models may be needed to support development of myostatin inhibitors for therapeutic clinical trials in SMA patients.
MATERIALS AND METHODS
Animals
All experiments were carried out in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals and were approved by the Institutional Animal Care and Use Committee at the Johns Hopkins University. Breeder pairs for SMAΔ7 mice on the FVB background (Stock number 005025; FVB.Cg-Tg(SMN2*delta7)4299Ahmb Tg(SMN2)89Ahmb Smn1tm1Msd/J) were purchased from Jackson Laboratories. These mice were genotyped by PCR of tail DNA as previously reported (45) and CLs were defined as those that were heterozygous or wild-type at the mSmn allele.
Follistatin transgenic mice on a C57BL/6 background were a kind gift of Lee (23). Follistatin transgenic mice were crossed with SMAΔ7 mice from the Jackson Laboratory (mSMN+/−/hSMN2+/+/SMN Δ7+/+). Progeny from this cross was subsequently intercrossed to achieve a strain that was homozygous for both Tg(SMN2*delta7)4299Ahmb and Tg(SMN2)89Ahmb transgenes, heterozygous for the Smn1tm1Msd allele and hemizygous for the Y-linked follistatin transgene. These mice were then sent to the Jackson Laboratory to establish an ongoing breeding colony where sperm from males (hSMN2+/+/SMN Δ7+/+/mSMN+/−, Fst+) were used in an in vitro fertilization with stock 005025 (hSMN2+/+/SMN Δ7+/+/mSMN−/− or +/−) as the oocyte donor mice. Specific pathogen free mice were derived and breeders maintained as female (hSMN2+/+/SMN Δ7+/+/mSMN+/−) X male (hSMN2+/+/SMN Δ7+/+/mSMN+/−, Fst+) to establish the experimental groups described. Confirmatory genotyping of the transgenic follistatin allele on tail DNA was done using real-time PCR and human follistatin primers purchased from Applied Biosystems (ABI).
Drug treatment and behavior
ActRIIB-Fc was a gift of Acceleron Pharma, Inc. Drug was injected into the intraperitoneal cavity at doses of 5, 10 or 60 mg/kg every 3 days starting on the second day of life. Vehicle consisted of PBS alone. We have previously shown that nutritional support substantially increases the efficacy of TSA treatment in SMA mice (45,46). Given this experience, in order to optimize treatment effects, we provided SMAΔ7 mice that received ActRIIB-Fc at 5 and 10 mg/kg with nutritional support as previously described (46). This consisted of a 4:1 mix of Esbilac and infant formula (Enfamil, Lipil, low iron) that was delivered per os ad libitum two times daily using a polypropylene feeding tube (Instech Solomon, Plymouth Meeting, PA, USA). In addition, all CLs were culled within 3 days of birth in these litters to minimize competition amongst the litter. The vehicle-treated mice included 11 mice that received nutritional support and were in culled litters, three mice that received nutritional support but were not in culled litters, and seven mice that did not receive nutritional support nor were in culled litters. There was no difference in survival in these groups and they were therefore combined into a single vehicle-treated group.
Daily weights were measured starting from the day of birth (P1). The sum of two trials of righting time was determined starting on P1 by placing mice on their back and recording the time to flip to their front with a maximum righting time of 30 s per trial. The hind-limb suspension test was performed by suspending the mouse from the hind-limbs on the edge of a 50 ml conical between P2 and P12 as previously described by El-Khodor et al. (57). Average position score, total number of pulls and total latency to fall time (maximum 30 s) during two trials were determined.
Histological analysis of muscle
Quadriceps, gastrocnemius and triceps muscles were dissected, weighed, embedded in OCT and flash frozen in liquid nitrogen. Multiple 12 µm sections were taken 100 µm apart from the mid-belly of each muscle and stained with hematoxylin and eosin (H&E). Muscle fiber diameters were quantified by an investigator blinded to the animal's treatment group using a Microcolor RGB-MS-C camera, OpenLab software and a Zeiss Axiophot microscope. Fiber diameter was defined as the longest aspect of the shortest axis. At least 300 individual myofiber diameters were measured from each animal.
qRT–PCR
RNA was isolated from all leg muscles using TRIzol reagent and converted to cDNA as previously described (45). Primers to amplify human follistatin, mouse follistatin, mouse myostatin and 18S RNA were purchased from ABI. Reactions were run in triplicate using the ABI Prism 7900 Sequence Detector System as previously described (45).
Statistical analysis
Survival data were analyzed using STATA v10 software package and Log rank analysis of Kaplan–Meier curves. Behavioral, pathological and biochemical data were analyzed using Excel and Statistica software packages, and statistical significance was determined using either Student's t-tests or two-way analysis of variance.
SUPPLEMENTARY MATERIAL
Supplementary Material is available at HMG online.
FUNDING
The generation of transgenic follistatin SMA mice at Jackson Laboratories was funded by the Spinal Muscular Atrophy Foundation. C.J.S. was supported by a Howard Hughes Medical Institute Physician Scientist Award and NINDS Career Transition Award (K22-NS0048199-01).
ACKNOWLEDGEMENTS
We would like to thank Dr S.-J. Lee of the Johns Hopkins School of Medicine for providing the follistatin transgenic mice and Dr Jasbir Seehra of Accleron Pharmaceuticals, Inc. for providing ActRIIB-Fc.
Conflict of Interest statement. None declared.
REFERENCES
- 1.Lefebvre S., Burglen L., Reboullet S., Clermont O., Burlet P., Viollet L., Benichou B., Cruaud C., Millasseau P., Zeviani M., et al. Identification and characterization of a spinal muscular atrophy-determining gene. Cell. 1995;80:155–165. doi: 10.1016/0092-8674(95)90460-3. [DOI] [PubMed] [Google Scholar]
- 2.Lefebvre S., Burlet P., Liu Q., Bertrandy S., Clermont O., Munnich A., Dreyfuss G., Melki J. Correlation between severity and SMN protein level in spinal muscular atrophy. Nat. Genet. 1997;16:265–269. doi: 10.1038/ng0797-265. [DOI] [PubMed] [Google Scholar]
- 3.Dubowitz V. Muscle Disorders in Childhood. 2nd edn. Philadelphia: WB Saunders; 1995. [Google Scholar]
- 4.Crawford T.O. Spinal muscular atrophies. In: Jones H., Vivo D.D., Darras B., editors. Neuromuscular Disorders of Infancy, Childhood and Adolescence: a Clinician's Approach. Philadephia: Butterworth Heinemann; 2003. pp. 145–166. [Google Scholar]
- 5.Fidzianska A., Goebel H.H., Warlo I. Acute infantile spinal muscular atrophy. Muscle apoptosis as a proposed pathogenetic mechanism. Brain. 1990;113:433–445. doi: 10.1093/brain/113.2.433. [DOI] [PubMed] [Google Scholar]
- 6.Le T.T., Pham L.T., Butchbach M.E., Zhang H.L., Monani U.R., Coovert D.D., Gavrilina T.O., Xing L., Bassell G.J., Burghes A.H. SMNDelta7, the major product of the centromeric survival motor neuron (SMN2) gene, extends survival in mice with spinal muscular atrophy and associates with full-length SMN. Hum. Mol. Genet. 2005;14:845–857. doi: 10.1093/hmg/ddi078. [DOI] [PubMed] [Google Scholar]
- 7.Biondi O., Grondard C., Lécole S., Deforges S., Pariset C., Lopes P., Cifuentes-Diaz C., Li H., della Gaspera B., Chanoine C., Charbonnier F. Exercise-induced activation of NMDA receptor promotes motor unit development and survival in a type 2 spinal muscular atrophy model mouse. J. Neurosci. 2008;28:953–962. doi: 10.1523/JNEUROSCI.3237-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stevens L., Bastide B., Maurage C.A., Dupont E., Montel V., Cieniewski-Bernard C., Cuisset J.M., Vallee L., Mounier Y. Childhood spinal muscular atrophy induces alterations in contractile and regulatory protein isoform expressions. Neuropathol. Appl. Neurobiol. 2008;34:659–670. doi: 10.1111/j.1365-2990.2008.00950.x. [DOI] [PubMed] [Google Scholar]
- 9.Kong L., Wang X., Choe D.W., Polley M., Burnett B.G., Bosch-Marce M., Griffin J.W., Rich M.M., Sumner C.J. Impaired synaptic vesicle release and immaturity of neuromuscular junctions in spinal muscular atrophy mice. J. Neurosci. 2009;29:842–851. doi: 10.1523/JNEUROSCI.4434-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Braun S., Croizat B., Lagrange M.C., Warter J.M., Poindron P. Constitutive muscular abnormalities in culture in spinal muscular atrophy. Lancet. 1995;345:694–695. doi: 10.1016/s0140-6736(95)90869-2. [DOI] [PubMed] [Google Scholar]
- 11.Nicole S., Desforges B., Millet G., Lesbordes J., Cifuentes-Diaz C., Vertes D., Cao M.L., De Backer F., Languille L., Roblot N., et al. Intact satellite cells lead to remarkable protection against Smn gene defect in differentiated skeletal muscle. J. Cell Biol. 2003;161:571–582. doi: 10.1083/jcb.200210117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shafey D., Cote P.D., Kothary R. Hypomorphic Smn knockdown C2C12 myoblasts reveal intrinsic defects in myoblast fusion and myotube morphology. Exp. Cell Res. 2005;311:49–61. doi: 10.1016/j.yexcr.2005.08.019. [DOI] [PubMed] [Google Scholar]
- 13.Rajendra T.K., Gonsalvez G.B., Walker M.P., Shpargel K.B., Salz H.K., Matera A.G. A Drosophila melanogaster model of spinal muscular atrophy reveals a function for SMN in striated muscle. J. Cell Biol. 2007;176:831–841. doi: 10.1083/jcb.200610053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gavrilina T.O., McGovern V.L., Workman E., Crawford T.O., Gogliotti R.G., DiDonato C.J., Monani U.R., Morris G.E., Burghes A.H. Neuronal SMN expression corrects spinal muscular atrophy in severe SMA mice while muscle-specific SMN expression has no phenotypic effect. Hum. Mol. Genet. 2008;17:1063–1075. doi: 10.1093/hmg/ddm379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McPherron A.C., Lawler A.M., Lee S.J. Regulation of skeletal muscle mass in mice by a new TGF-beta superfamily member. Nature. 1997;387:83–90. doi: 10.1038/387083a0. [DOI] [PubMed] [Google Scholar]
- 16.McPherron A.C., Lee S.J. Double muscling in cattle due to mutations in the myostatin gene. Proc. Natl Acad. Sci. USA. 1997;94:12457–12461. doi: 10.1073/pnas.94.23.12457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grobet L., Martin L.J., Poncelet D., Pirottin D., Brouwers B., Riquet J., Schoeberlein A., Dunner S., Menissier F., Massabanda J., et al. A deletion in the bovine myostatin gene causes the double-muscled phenotype in cattle. Nat. Genet. 1997;17:71–74. doi: 10.1038/ng0997-71. [DOI] [PubMed] [Google Scholar]
- 18.Schuelke M., Wagner K.R., Stolz L.E., Hubner C., Riebel T., Komen W., Braun T., Tobin J.F., Lee S.J. Myostatin mutation associated with gross muscle hypertrophy in a child. N. Engl. J. Med. 2004;350:2682–2688. doi: 10.1056/NEJMoa040933. [DOI] [PubMed] [Google Scholar]
- 19.Clop A., Marcq F., Takeda H., Pirottin D., Tordoir X., Bibe B., Bouix J., Caiment F., Elsen J.M., Eychenne F., et al. A mutation creating a potential illegitimate microRNA target site in the myostatin gene affects muscularity in sheep. Nat. Genet. 2006;38:813–818. doi: 10.1038/ng1810. [DOI] [PubMed] [Google Scholar]
- 20.Mosher D.S., Quignon P., Bustamante C.D., Sutter N.B., Mellersh C.S., Parker H.G., Ostrander E.A. A mutation in the myostatin gene increases muscle mass and enhances racing performance in heterozygote dogs. PLoS Genet. 2007;3:e79. doi: 10.1371/journal.pgen.0030079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee S.J. Regulation of muscle mass by myostatin. Annu. Rev. Cell Dev. Biol. 2004;20:61–86. doi: 10.1146/annurev.cellbio.20.012103.135836. [DOI] [PubMed] [Google Scholar]
- 22.Hennebry A., Berry C., Siriett V., O'Callaghan P., Chau L., Watson T., Sharma M., Kambadur R. Myostatin regulates fiber-type composition of skeletal muscle by regulating MEF2 and MyoD gene expression. Am. J. Physiol. Cell Physiol. 2009;296:C525–C534. doi: 10.1152/ajpcell.00259.2007. [DOI] [PubMed] [Google Scholar]
- 23.Lee S.J., McPherron A.C. Regulation of myostatin activity and muscle growth. Proc. Natl Acad. Sci. USA. 2001;98:9306–9311. doi: 10.1073/pnas.151270098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hill J.J., Davies M.V., Pearson A.A., Wang J.H., Hewick R.M., Wolfman N.M., Qiu Y. The myostatin propeptide and the follistatin-related gene are inhibitory binding proteins of myostatin in normal serum. J. Biol. Chem. 2002;277:40735–40741. doi: 10.1074/jbc.M206379200. [DOI] [PubMed] [Google Scholar]
- 25.Hill J.J., Qiu Y., Hewick R.M., Wolfman N.M. Regulation of myostatin in vivo by growth and differentiation factor-associated serum protein-1: a novel protein with protease inhibitor and follistatin domains. Mol. Endocrinol. 2003;17:1144–1154. doi: 10.1210/me.2002-0366. [DOI] [PubMed] [Google Scholar]
- 26.Matzuk M.M., Lu N., Vogel H., Sellheyer K., Roop D.R., Bradley A. Multiple defects and perinatal death in mice deficient in follistatin. Nature. 1995;374:360–363. doi: 10.1038/374360a0. [DOI] [PubMed] [Google Scholar]
- 27.Lee S.J. Quadrupling muscle mass in mice by targeting TGF-beta signaling pathways. PLoS One. 2007;2:e789. doi: 10.1371/journal.pone.0000789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Whittemore L.A., Song K., Li X., Aghajanian J., Davies M., Girgenrath S., Hill J.J., Jalenak M., Kelley P., Knight A., et al. Inhibition of myostatin in adult mice increases skeletal muscle mass and strength. Biochem. Biophys. Res. Commun. 2003;300:965–971. doi: 10.1016/s0006-291x(02)02953-4. [DOI] [PubMed] [Google Scholar]
- 29.Bogdanovich S., Perkins K.J., Krag T.O., Whittemore L.A., Khurana T.S. Myostatin propeptide-mediated amelioration of dystrophic pathophysiology. FASEB. J. 2005;19:543–549. doi: 10.1096/fj.04-2796com. [DOI] [PubMed] [Google Scholar]
- 30.Qiao C., Li J., Jiang J., Zhu X., Wang B., Li J., Xiao X. Myostatin propeptide gene delivery by adeno-associated virus serotype 8 vectors enhances muscle growth and ameliorates dystrophic phenotypes in mdx mice. Hum. Gene Ther. 2008;19:241–254. doi: 10.1089/hum.2007.159. [DOI] [PubMed] [Google Scholar]
- 31.Lee S.J., Reed L.A., Davies M.V., Girgenrath S., Goad M.E., Tomkinson K.N., Wright J.F., Barker C., Ehrmantraut G., Holmstrom J., et al. Regulation of muscle growth by multiple ligands signaling through activin type II receptors. Proc. Natl Acad. Sci. USA. 2005;102:18117–18122. doi: 10.1073/pnas.0505996102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Morrison B.M., Lachey J.L., Warsing L.C., Ting B.L., Pullen A.E., Underwood K.W., Kumar R., Sako D., Grinberg A., Wong V., et al. A soluble activin IIB receptor improves function in a mouse model of amyotrophic lateral sclerosis. Exp. Neurol. 2009;217:258–268. doi: 10.1016/j.expneurol.2009.02.017. [DOI] [PubMed] [Google Scholar]
- 33.Wagner K.R., McPherron A.C., Winik N., Lee S.J. Loss of myostatin attenuates severity of muscular dystrophy in mdx mice. Ann. Neurol. 2002;52:832–836. doi: 10.1002/ana.10385. [DOI] [PubMed] [Google Scholar]
- 34.Bogdanovich S., Krag T.O., Barton E.R., Morris L.D., Whittemore L.A., Ahima R.S., Khurana T.S. Functional improvement of dystrophic muscle by myostatin blockade. Nature. 2002;420:418–421. doi: 10.1038/nature01154. [DOI] [PubMed] [Google Scholar]
- 35.Bartoli M., Poupiot J., Vulin A., Fougerousse F., Arandel L., Daniele N., Roudaut C., Noulet F., Garcia L., Danos O., et al. AAV-mediated delivery of a mutated myostatin propeptide ameliorates calpain 3 but not alpha-sarcoglycan deficiency. Gene Ther. 2007;14:733–740. doi: 10.1038/sj.gt.3302928. [DOI] [PubMed] [Google Scholar]
- 36.Bogdanovich S., McNally E.M., Khurana T.S. Myostatin blockade improves function but not histopathology in a murine model of limb-girdle muscular dystrophy 2C. Muscle Nerve. 2008;37:308–316. doi: 10.1002/mus.20920. [DOI] [PubMed] [Google Scholar]
- 37.Parsons S.A., Millay D.P., Sargent M.A., McNally E.M., Molkentin J.D. Age-dependent effect of myostatin blockade on disease severity in a murine model of limb-girdle muscular dystrophy. Am. J. Pathol. 2006;168:1975–1985. doi: 10.2353/ajpath.2006.051316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ohsawa Y., Hagiwara H., Nakatani M., Yasue A., Moriyama K., Murakami T., Tsuchida K., Noji S., Sunada Y. Muscular atrophy of caveolin-3-deficient mice is rescued by myostatin inhibition. J. Clin. Invest. 2006;116:2924–2934. doi: 10.1172/JCI28520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li Z.F., Shelton G.D., Engvall E. Elimination of myostatin does not combat muscular dystrophy in dy mice but increases postnatal lethality. Am. J. Pathol. 2005;166:491–497. doi: 10.1016/S0002-9440(10)62271-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wagner K.R., Fleckenstein J.L., Amato A.A., Barohn R.J., Bushby K., Escolar D.M., Flanigan K.M., Pestronk A., Tawil R., Wolfe G.I., et al. A phase I/II trial of MYO-029 in adult subjects with muscular dystrophy. Ann. Neurol. 2008;63:561–571. doi: 10.1002/ana.21338. [DOI] [PubMed] [Google Scholar]
- 41.Holzbaur E.L., Howland D.S., Weber N., Wallace K., She Y., Kwak S., Tchistiakova L.A., Murphy E., Hinson J., Karim R., et al. Myostatin inhibition slows muscle atrophy in rodent models of amyotrophic lateral sclerosis. Neurobiol. Dis. 2006;23:697–707. doi: 10.1016/j.nbd.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 42.Miller T.M., Kim S.H., Yamanaka K., Hester M., Umapathi P., Arnson H., Rizo L., Mendell J.R., Gage F.H., Cleveland D.W., et al. Gene transfer demonstrates that muscle is not a primary target for non-cell-autonomous toxicity in familial amyotrophic lateral sclerosis. Proc. Natl Acad. Sci. USA. 2006;103:19546–19551. doi: 10.1073/pnas.0609411103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rose F.F., Jr, Mattis V.B., Rindt H., Lorson C.L. Delivery of recombinant follistatin lessens disease severity in a mouse model of spinal muscular atrophy. Hum. Mol. Genet. 2009;18:997–1005. doi: 10.1093/hmg/ddn426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Suryawan A., Frank J.W., Nguyen H.V., Davis T.A. Expression of the TGF-beta family of ligands is developmentally regulated in skeletal muscle of neonatal rats. Pediatr. Res. 2006;59:175–179. doi: 10.1203/01.pdr.0000196718.47935.6e. [DOI] [PubMed] [Google Scholar]
- 45.Avila A.M., Burnett B.G., Taye A.A., Gabanella F., Knight M.A., Hartenstein P., Cizman Z., Di Prospero N.A., Pellizzoni L., Fischbeck K.H., et al. Trichostatin A increases SMN expression and survival in a mouse model of spinal muscular atrophy. J. Clin. Invest. 2007;117:659–671. doi: 10.1172/JCI29562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Narver H.L., Kong L., Burnett B.G., Choe D.W., Bosch-Marce M., Taye A.A., Eckhaus M.A., Sumner C.J. Sustained improvement of spinal muscular atrophy mice treated with trichostatin a plus nutrition. Ann. Neurol. 2008;64:465–470. doi: 10.1002/ana.21449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Butchbach M.E., Edwards J.D., Burghes A.H. Abnormal motor phenotype in the SMNDelta7 mouse model of spinal muscular atrophy. Neurobiol. Dis. 2007;27:207–219. doi: 10.1016/j.nbd.2007.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McCroskery S., Thomas M., Maxwell L., Sharma M., Kambadur R. Myostatin negatively regulates satellite cell activation and self-renewal. J. Cell Biol. 2003;162:1135–1147. doi: 10.1083/jcb.200207056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wagner K.R., Liu X., Chang X., Allen R.E. Muscle regeneration in the prolonged absence of myostatin. Proc. Natl Acad. Sci. USA. 2005;102:2519–2524. doi: 10.1073/pnas.0408729102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lieber R.L. Skeletal Muscle Structure and Function. Baltimore: Williams and Wilkens; 1992. [Google Scholar]
- 51.McPherron A.C., Lee S.J. Suppression of body fat accumulation in myostatin-deficient mice. J. Clin. Invest. 2002;109:595–601. doi: 10.1172/JCI13562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lean M.E. Brown adipose tissue in humans. Proc. Nutr. Soc. 1989;48:243–256. doi: 10.1079/pns19890036. [DOI] [PubMed] [Google Scholar]
- 53.Gesta S., Tseng Y.H., Kahn C.R. Developmental origin of fat: tracking obesity to its source. Cell. 2007;131:242–256. doi: 10.1016/j.cell.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 54.Wang C.H., Finkel R.S., Bertini E.S., Schroth M., Simonds A., Wong B., Aloysius A., Morrison L., Main M., Crawford T.O., et al. Consensus statement for standard of care in spinal muscular atrophy. J. Child Neurol. 2007;22:1027–1049. doi: 10.1177/0883073807305788. [DOI] [PubMed] [Google Scholar]
- 55.Minetti G.C., Colussi C., Adami R., Serra C., Mozzetta C., Parente V., Fortuni S., Straino S., Sampaolesi M., Di Padova M., et al. Functional and morphological recovery of dystrophic muscles in mice treated with deacetylase inhibitors. Nat. Med. 2006;12:1147–1150. doi: 10.1038/nm1479. [DOI] [PubMed] [Google Scholar]
- 56.Iezzi S., Di Padova M., Serra C., Caretti G., Simone C., Maklan E., Minetti G., Zhao P., Hoffman E.P., Puri P.L., et al. Deacetylase inhibitors increase muscle cell size by promoting myoblast recruitment and fusion through induction of follistatin. Dev. Cell. 2004;6:673–684. doi: 10.1016/s1534-5807(04)00107-8. [DOI] [PubMed] [Google Scholar]
- 57.El-Khodor B.F., Edgar N., Chen A., Winberg M.L., Joyce C., Brunner D., Suárez-Fariñas M., Heyes M.P. Identification of a battery of tests for drug candidate evaluation in the SMNDelta7 neonate model of spinal muscular atrophy. Exp. Neurol. 2008;212(1):29–43. doi: 10.1016/j.expneurol.2008.02.025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.