Abstract
Purpose
Milk thistle or its purified extract, silymarin (Silybum marianum), is widely used in treating acute or chronic hepatitis. Although silymarin is hepatoprotective in animal experiments and some human hepatotoxic exposures, its efficacy in ameliorating the symptoms of acute clinical hepatitis remains inconclusive. In this study, our purpose was to determine whether silymarin improves symptoms, signs and laboratory test results in patients with acute clinical hepatitis, regardless of etiology.
Methods
This is a randomized, placebo-controlled trial in which participants, treating physicians and data management staff were blinded to treatment group. The study was conducted at two fever hospitals in Tanta and Banha, Egypt where patients with symptoms compatible with acute clinical hepatitis and serum alanine aminotransferase (ALT) levels > 2.5 times the upper limit of normal were enrolled. The intervention consisted of three times daily ingestion of either a standard recommended dose of 140 mg of silymarin (Legalon®, MADAUS GmbH, Cologne, Germany), or a vitamin placebo for four weeks with an additional four-week follow-up. The primary outcomes were symptoms and signs of acute hepatitis and results of liver function tests on days 2, 4 and 7 and weeks 2, 4, and 8. Side-effects and adverse events were ascertained by self-report.
Results
From July 2003 through October 2005, 105 eligible patients were enrolled after providing informed consent. No adverse events were noted and both silymarin and placebo were well tolerated. Patients randomized to the silymarin group had quicker resolution of symptoms related to biliary retention: dark urine (p=0.013), jaundice (p=0.02) and scleral icterus (p=0.043). There was a reduction in indirect bilirubin among those assigned to silymarin (p=0.012), but other variables including direct bilirubin, ALT and aspartate aminotransferase (AST) were not significantly reduced.
Conclusions
Patients receiving silymarin had earlier improvement in subjective and clinical markers of biliary excretion. Despite a modest sample size and multiple etiologies for acute clinical hepatitis, our results suggest that standard recommended doses of silymarin are safe and may be potentially effective in improving symptoms of acute clinical hepatitis despite lack of a detectable effect on biomarkers of the underlying hepatocellular inflammatory process.
Keywords: hepatitis, milk thistle, silymarin, randomized controlled trial, Egypt
INTRODUCTION
Acute hepatitis is a clinical syndrome with a presentation that can range from mild flu-like symptoms to severe fulminant hepatitis and is characterized by a triad of impaired biliary excretion, hepatocellular liver damage and systemic effects of liver inflammation. Acute viral hepatitis (AVH) is the commonest cause of acute hepatitis and infection with hepatitis viruses ranges from 20–40% in developed countries and 80–100% in developing countries.(Corwin et al., 1996, Meky et al., 2006, Shepard et al., 2005)
No significant advances in managing acute symptomatic viral hepatitis have been developed since 1955 (Chalmers et al., 1955) where it was concluded that the best therapy was rest and a high-protein diet. Given that symptoms can last from a few weeks to several months, an effective intervention would permit early recovery and fewer days of work lost. In the absence of allopathic medications, homeopathic remedies such as milk thistle or its purified extract, silymarin, are used extensively.(Jacobs et al., 2002, Luper, 1998, Luper, 1999)
The botanical name for milk thistle is Silybum marianum. It is also referred to as holy thistle, Marian thistle, Mary thistle, Our Lady’s thistle, St. Mary thistle, wild artichoke, Mariendistel (German), and Chardon-Marie (French). The seeds of milk thistle are the medicinal parts of the plant. The primary active constituent of milk thistle is silymarin, which is composed of four isomers: silybin, isosilybin, silychristin, and silydianin. In turn, silybin and isosilybin are both mixtures of two diastereomers, silybins A and B and isosilybins A and B, respectively. (Lee and Liu, 2003, Saller et al., 2001) Special formulations of silybin have been developed to enhance the bioavailability of the herbal product; these forms are sold under the names Legalon®, silipide, and Siliphos. Because of milk thistle’s lipophilic nature, it is usually administered in capsule or tablet form rather than as an herbal tea.
Milk Thistle is widely used in Europe, United States, Egypt, and elsewhere for “liver support”.(Luper, 1998, Luper, 1999, Mulrow et al., 2000, Saller et al., 2001) The German Commission E endorses its use as a supportive treatment for chronic inflammatory liver conditions and cirrhosis. Milk thistle/silymarin is thought to work via: (1) preventing entry of various toxins, e.g., alcohol, carbon tetracholoride and heavy metals, into hepatocytes; (2) stimulating protein synthesis with hepatocyte regeneration; (3) acting as a free-radical scavenger and antioxidant; and (4) modulating the immune response.(Boigk et al., 1997, Deak et al., 1990, Muriel and Mourelle, 1990, Pietrangelo et al., 1995) The hepatoprotective action of silymarin in fatal fulminant hepatic failure following Amanita phalloides mushroom poisoning is documented in experimental animals and humans even when given after exposure.(Hruby et al., 1983, Vogel et al., 1984) Inconclusive results have been reported in a few randomized controlled trials (RCT), mostly on alcoholic liver disease, chronic hepatitis B (HBV) or hepatitis C (HCV) infections.(Ball and Kowdley, 2005, Jacobs et al., 2002, Mayer et al., 2005, Rambaldi et al., 2005, Strickland et al., 2005, Tanamly et al., 2004)
Since the therapeutic endpoint for acute hepatitis occurs in days or a few weeks as opposed to years in chronic hepatitis, we speculated that it would be an excellent model to evaluate safety and efficacy of silymarin.
MATERIALS AND METHODS
Design Overview
We used a double blind, randomized, placebo-controlled trial to compare the effect of a standard recommended dose of silymarin with a placebo. This study was conducted in compliance with the principles of the Declaration of Helsinki and approved by the Institutional Review Boards at both the University of Maryland Baltimore and the Egyptian Ministry of Health & Population. All study participants provided informed consent.
Setting and Participants
Symptomatic patients, thirteen years or older, were enrolled from Tanta and Banha Fever Hospitals in the Nile Delta where the incidence of acute viral hepatitis is high.(Meky et al., 2006) Eligibility criteria included an alanine aminotransferase (ALT) level more than 2.5 times the upper limit of normal (> 100 IU/L), with jaundice and/or scleral icterus and three or more of the following symptoms: dark-colored urine; light-colored stools; fever; nausea; vomiting; anorexia; aversion to smoking; pruritus; right upper abdominal discomfort, pain or feeling of pressure; and pruritic red hives of less than four weeks. Exclusion criteria included being pregnant or breastfeeding; having advanced liver disease, another severe illness, or having taken a known hepatotoxic drug.
Randomization and Interventions
At baseline, a detailed history was recorded, each subject was examined, and a blood sample drawn. Liver biopsies were not performed in this study. Subjects were randomized to receive silymarin or vitamin placebo capsules thrice daily for four weeks and then a follow-up visit at eight weeks. The capsules were similar in appearance to conceal content. A central coordinator in Cairo not involved in patient enrollment, product distribution, or data collection, kept the code for group allocation. Patients were stratified by site and randomized using pre-assigned numbers provided in pre-sealed envelopes.
Outcomes and Follow-up
Primary outcomes were normalization of bilirubin and hepatic enzymes within eight weeks, defined as: ALT ≤ 40 IU/L, aspartate aminotransferase (AST) ≤ 42 IU/L, total bilirubin ≤ 1.0 mg/dl and direct bilirubin ≤ 0.3 mg/dl. Standardized data collection forms were used as described previously (Strickland et al., 2005, Tanamly et al., 2004) to record demographic data, symptoms, clinical history, physical exams, adverse events and laboratory test results at baseline and on days 2, 4 and 7 in the hospital, and in the outpatient clinic at weeks 2, 4, and 8.
Serum samples were tested for ALT, AST, and direct and total bilirubin using standard methods. Hepatitis A IgM antibodies (anti-HAV IgM) were tested with HAVAB-M kits; hepatitis B core antigen IgM antibodies (anti-HBc IgM) with COREM kits; and hepatitis C antibodies (anti-HCV) with Ortho HCV 3.0 enzyme immunoassay (EIA) test system (Ortho Diagnostic System, Raritan, NJ). Hepatitis E IgM and IgG antibodies (anti-HEV IgM and anti-HEV IgG) were evaluated by an in-house National Institutes of Health EIA using a truncated (55-KD) recombinant HEV capsid protein antigen expressed from baculovirus in SF-9 insect cells.(Tsarev et al., 1993) Samples from patients negative for hepatitis A-E viruses were tested for cytomegalovirus (CMV) IgM antibodies with CMV-IgM IMX kits (Abbott Laboratories, Abbott Park, IL) and for Epstein-Barr virus IgM antibodies (anti-EBV IgM) with ETI-EBV-M reverse P001605 kits (DiaSorin, Saluggia, Italy). Tests for HBV surface antigen (HBsAg) were conducted with the Auszyme monoclonal third-generation EIA. HCV-RNA was extracted using the QIAamp Viral RNA extraction kit (Qiagen, Santa Clara, CA), and testing for HCV RNA was performed using a direct nested reverse transcriptase-polymerase chain reaction (RT-PCR), as described elsewhere.(Abdel-Hamid et al., 1997) HEV-RNA was sought in the eluted RNA by nested RT-PCR with primers from the genome ORF2 region.(Wang et al., 1999)
Subjects were considered to have HAV-, HBV- or HEV- AVH, if they had anti-HAV IgM; anti-HBc IgM with/without HBsAg; or anti-HEV IgM and/or HEV-RNA in their serum samples, respectively. Subjects were considered acute incident HCV if they were initially HCV-RNA positive and anti-HCV negative and subsequently became positive for anti-HCV. Subjects with both anti-HCV and HCV RNA and no other viral etiology were considered chronic HCV infection with manifestations of acute hepatitis. Those with HBsAg in the absence of anti-HBc IgM, were considered chronic HBV infection with manifestations of acute hepatitis. AVH due to CMV or EBV was diagnosed if anti-CMV IgM or anti-EBV IgM antibodies were positive, respectively. Subjects not meeting the criteria for infection with hepatitis A-E viruses, EBV or CMV were considered acute hepatitis with no known viral etiology.
Active Compound, Placebo and Dosage
Silymarin was provided in bulk by Madaus GmbH (Cologne, Germany) with the same quality and purity (using 2,4-dinitrophenylhydrazine method [DNPH]) as in their commercial product, Legalon® (Wagner et al. 1974). A low-dose multivitamin and mineral compound marketed in Egypt was used as a placebo. Both silymarin and placebo were placed in identical capsules by the Chemical Industries Development Pharmaceutical Co. (CID; Cairo, Egypt), which markets Legalon® in Egypt. Each capsule of silymarin contained 140 mg silymarin as active ingredient. The placebo was mixed with inactive diluent so that three capsules contained no more multivitamin than the recommended daily allowance. The Egyptian National Organization for Drug Control and Research (NODCAR) assisted in quality control.
Statistical Analysis
All analyses used the intention-to-treat paradigm. Generalized estimating equations (GEE) with a binomial working model were fit to compare trajectories of symptoms and signs between the two groups. The models were refit controlling for baseline factors: age, gender, dark urine, AST, ALT, indirect bilirubin, direct bilirubin, scleral icterus, and type of hepatitis (acute, chronic, undiagnosed source). Additional analyses using GEE with a normal working model were performed comparing treatment and placebo group with respect to changes in mean number of symptoms representing the three pathophysiologic processes: impaired biliary excretion, i.e., dark urine, jaundice, scleral icterus, clay-colored stool, and elevated direct bilirubin; hepatocellular liver damage, i.e., abdominal pain and swelling; enlarged or tender liver; and elevated ALT, AST, and indirect bilirubin; and systemic effects of liver inflammation, i.e., fever, fatigue, malaise, anorexia, nausea, and vomiting.
For each outcome, a chi-square test was used to compare trajectories between groups. An analysis of covariance (ANCOVA) model was fit for each GEE and for interactions. When binary symptoms were sparse (< 5 individuals), time (days from baseline) was fit using natural cubic splines. GEE was used instead of survival analysis because symptom status can fluctuate over time. The ANCOVA models implicitly adjust for baseline imbalances of the analysis outcome, and GEE yields unbiased estimates even if outcomes are not normally distributed. Lastly, a sensitivity analysis using weighted estimating equations (WEE) was performed to assess the impact of missing data.(Robins et al., Mar., 1995) Side effects were compared by median-unbiased estimated rate ratios of complaints and 95% confidence interval (CI). All data were entered into a Microsoft Access (Redmond, WA) database (Arabic version 2000), and the statistical analysis was done using R statistical software (version 2.2). Duplicate data entry helped ensure quality control.
RESULTS
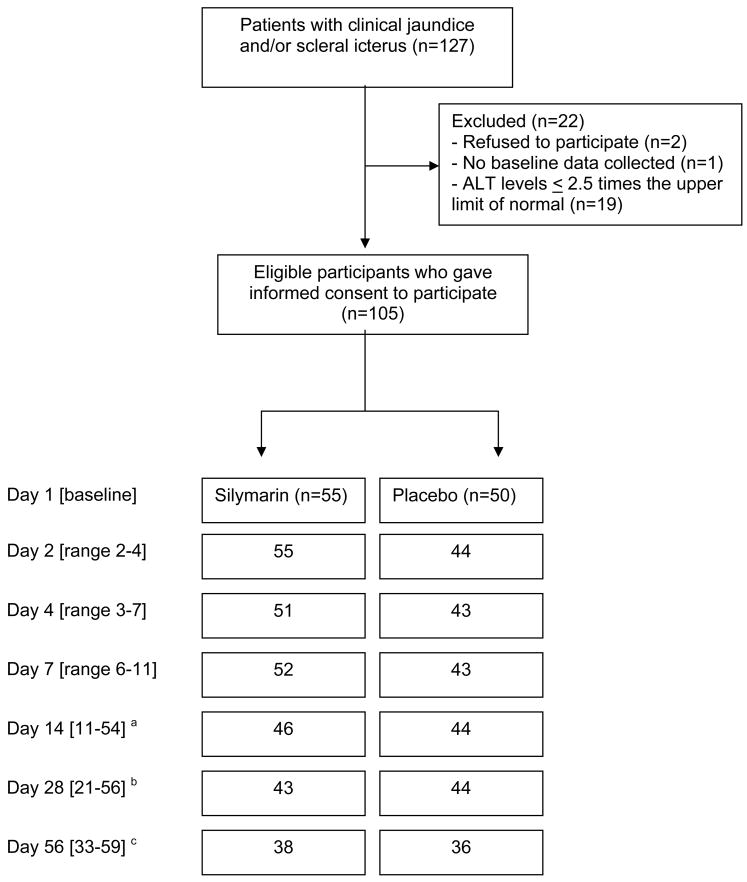
From July 2003 through October 2005, 105 subjects met our inclusion criteria and provided informed consent to be enrolled (Fig. 1). Their mean age was 29.8 (standard deviation (SD) ± 12.0) years and 81.9% were males. Fifty-five and 50 participants were randomly assigned to receive silymarin or vitamin placebo, respectively (Table 1). There were sixteen (15.2%) acute HAV patients; 35 (33.3%) acute HBV; three acute incident HCV; three acute HEV; two acute EBV; and one acute CMV. In addition, one patient had chronic HBV with acute manifestations and 18 (17.1%) had chronic HCV infection with acute manifestations, 14 of whom had ALT levels > 200 IU/L; while 26 (24.8%) had no detectable viral etiology.
Figure 1. Study Flow Chart.
a If a patient with 54 days at follow-up is excluded, the range is 11-21 days.
b If a patient with 56 days at follow-up is excluded, the range is 21-28 days.
c If a patient with 33 days at follow-up is excluded, the range is 42-69 days.
Table 1.
Baseline characteristics of treatment groups.
| Characteristic | Silymarin n=55 | Placebo n=50 |
|---|---|---|
| Mean age, years (SD) | 31 (12) | 29 (12) |
| Male gender, count (%) | 42 (76) | 44 (88) |
| Viral etiology of AVH, count (%) | ||
| Acute HAV | 9 (16) | 7 (14) |
| Acute HBV | 17 (31) | 18 (36) |
| Acute incident HCV | 2 (4) | 1 (2) |
| Acute HEV | 1 (2) | 2 (4) |
| Acute EBV | 1 (2) | 1 (2) |
| Acute CMV | 1 (2) | 0 (0) |
| Acute hepatitis in chronic HCV | 6 (11) | 12 (24) |
| Acute hepatitis in chronic HBV | 0 (0) | 1 (2) |
| No detectable viral cause | 18 (33) | 8 (16) |
| Symptoms and signs, count (%) | ||
| Scleral Icterus | 54 (98) | 44 (88) |
| Jaundice | 40 (73) | 31 (62) |
| Dark Urine | 50 (90) | 38 (76) |
| Malaise | 46 (84) | 38 (76) |
| Weight Loss | 12 (22) | 5 (10) |
| Fatigue | 48 (87) | 39 (78) |
| Clay-colored stools | 23 (42) | 16 (32) |
| Anorexia | 44 (80) | 36 (72) |
| Diarrhea | 8 (15) | 8 (16) |
| Fever | 14 (25) | 16 (32) |
| Nausea | 32 (58) | 32 (64) |
| Vomiting | 18 (36) | 21 (38) |
| Abdominal pain | 36 (65) | 28 (56) |
| Laboratory values, median (IQR) | ||
| Total bilirubin, mg/dl | 7.0 (3.5, 13.8) | 4.0 (2.1, 9.1) |
| Direct bilirubin, mg/dl | 4.3 (1.9, 8.8) | 2.4 (0.9, 5.3) |
| ALT, IU/L | 319 (224, 925) | 484 (255, 753) |
| AST, IU/L | 268 (134, 478) | 214 (120, 394) |
All binary data presented as count (%), age presented as mean (SD), all laboratory test (continuous) values presented as median (interquartile range, IQR).
HAV, hepatitis A virus; HBV, hepatitis B virus; HCV, hepatitis C virus; HEV, hepatitis E virus; EBV, Epstein-Barr virus; CMV, cytomegalovirus; ALT, Alanine Aminotransferase; AST, Aspartate Aminotransferase; SD, standard deviation.
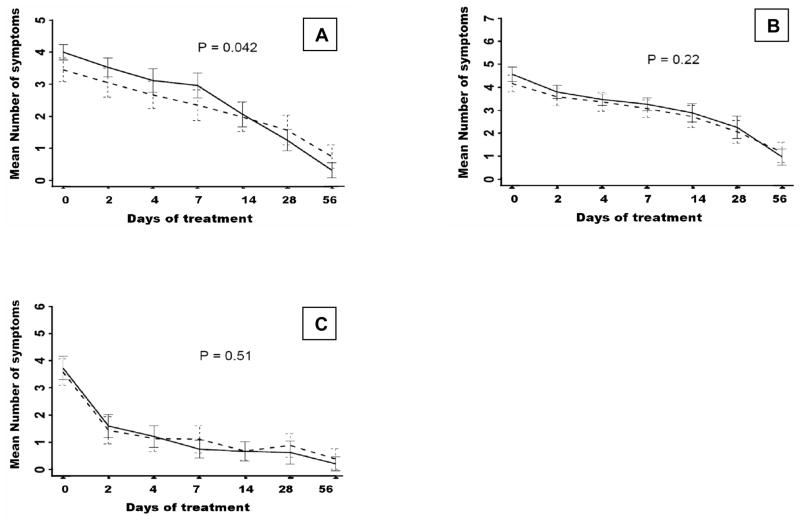
Among those assigned to silymarin there was a significantly faster resolution of the mean number of markers of impaired biliary excretion compared to the placebo group (p=0.042; Fig. 2 A), with significant subjective indicators including dark urine (p=0.013), jaundice (p=0.02), and scleral icterus (p=0.043), while other indicators were not significant (Table 2). Among indicators of hepatocellular damage, there was no difference in trajectories of the mean number of markers between the two groups (p=0.22; Fig. 2 B), except for indirect bilirubin at day 56 (p=0.012), while declines in mean levels of ALT and AST did not differ between the groups. Overall changes in the mean number of symptoms of systemic effects of liver inflammation did not differ between the two groups (p=0.51; Fig. 2 C), although subjective indicators showed that those assigned to silymarin had faster resolution in fatigue (p=0.06), malaise (p=0.045), and anorexia (p=0.061) at eight weeks post-randomization.
Figure 2.
Mean number of symptoms, signs and laboratory values (with 95% confidence intervals) for pathophysiological grouping by (A) impaired biliary excretion; (B) hepatocellular damage; and (C) systemic effects of liver inflammation, comparing silymarin (solid line) and placebo (dashed line) at each visit (see text for which variables were included in the pathophysiological groupings).
Table 2.
Number and percentage (%) of patients with indicators of impaired biliary excretion, hepatocellular damage and systemic effects of liver inflammation at each visit, and mean (SD) of laboratory values at each visit.
| Symptom, Sign or Test Result | Visit Number | |||||||
|---|---|---|---|---|---|---|---|---|
| Impaired biliary excretion | Baseline | 1 | 2 | 3 | 4 | 5 | 6 | P-value |
| Dark urine*, count (%) | 0.013 | |||||||
| Silymarin | 50(91) | 34(62) | 30(59) | 27(52) | 6(13) | 3(7) | 1(3) | |
| Placebo | 38(76) | 24(57) | 14(33) | 13(30) | 6(14) | 8(18) | 4(11) | |
| Jaundice*, count (%) | 0.020 | |||||||
| Silymarin | 40(73) | 40(73) | 30(59) | 33(64) | 19(42) | 7(16) | 2(5) | |
| Placebo | 31(62) | 23(54) | 21(49) | 19(44) | 18(41) | 15(34) | 4(11) | |
| Scleral icterus, count (%) | 0.043 | |||||||
| Silymarin | 54(98) | 53(96) | 44(86) | 43(83) | 31(69) | 17(40) | 5(13) | |
| Placebo | 44(88) | 39(91) | 37(86) | 33(77) | 25(57) | 23(52) | 12(33) | |
| Clay-colored stool*, count (%) | 0.69 | |||||||
| Silymarin | 23(42) | 15(27) | 8(16) | 7(14) | 2(4.4) | 1(2.3) | 0(0) | |
| Placebo | 16(32) | 10(23) | 7(16) | 5(12) | 5(11) | 2(4.5) | 0(0) | |
| Direct bilirubin >0.3 mg/dl*, count (%) | 0.18 | |||||||
| Silymarin | 53(96) | 52(94) | 47(92) | 45(88) | 35(78) | 26(60) | 4(10) | |
| Control | 44(90) | 35(81) | 33(79) | 31(72) | 33(75) | 21(48) | 6(17) | |
|
| ||||||||
|
Hepatocellular damage | ||||||||
| Abdominal pain*, count (%) | 0.34 | |||||||
| Silymarin | 36(65) | 14(25) | 7(14) | 9(17) | 8(18) | 8(19) | 3(8) | |
| Placebo | 28(56) | 10(23) | 9(21) | 7(16) | 10(23) | 8(18) | 3(8) | |
| Abdominal swelling*, count (%) | 0.10 | |||||||
| Silymarin | 17(31) | 7(13) | 4(7.8) | 2(3.8) | 3(7) | 5(12) | 4(10) | |
| Placebo | 11(22) | 6(14) | 3(7.0) | 3(7.0) | 4(9) | 5(11) | 0(0) | |
| Enlarged liver*, count (%) | 0.17 | |||||||
| Silymarin | 19(34) | 19(36) | 18(37) | 16(31) | 12(27) | 7(16) | 3(8) | |
| Placebo | 11(22) | 10(23) | 10(24) | 9(21) | 8(18) | 7(15) | 7(19) | |
| Tender liver*, count (%) | 0.65 | |||||||
| Silymarin | 10(19) | 6(11) | 4(8) | 5(10) | 7(16) | 4(9) | 1(3) | |
| Placebo | 12(24) | 10(26) | 10(24) | 7(16) | 6(14) | 4(9) | 2(6) | |
| ALT > 40 IU/L*, count (%) | 0.56 | |||||||
| Silymarin | 55(100) | 55(100) | 51(100) | 51(100) | 37(82) | 27(63) | 6(16) | |
| Placebo | 49(100) | 43(100) | 42(100) | 41(95) | 37(84) | 24(54) | 10(28) | |
| AST > 42 IU/L*, count (%) | 0.42 | |||||||
| Silymarin | 54(98) | 53(96) | 47(92) | 42(82) | 29(64) | 20(46) | 6(16) | |
| Placebo | 48(98) | 38(88) | 36(86) | 35(81) | 27(61) | 20(45) | 8(22) | |
| Indirect bilirubin> 0.7 mg/dl*, count (%) | 0.012 | |||||||
| Silymarin | 55(100) | 51(93) | 44(86) | 43(84) | 33(73) | 25(58) | 14(37) | |
| Placebo | 42(86) | 35(81) | 32(76) | 29(67) | 27(61) | 23(52) | 12(34) | |
|
| ||||||||
|
Systemic effects of liver inflammation | ||||||||
| Fever*, count (%) | 0.33 | |||||||
| Silymarin | 14(25) | 3(5) | 4(8) | 3(6) | 2(4) | 1(2) | 2(5) | |
| Placebo | 16(32) | 2(5) | 1(2) | 2(5) | 1(2) | 3(7) | 0(0) | |
| Fatigue*, count (%) | 0.060 | |||||||
| Silymarin | 48(87) | 27(49) | 21(41) | 14(27) | 11(24) | 6(14) | 2(5) | |
| Placebo | 39(78) | 19(44) | 15(35) | 15(35) | 11(25) | 11(25) | 4(11) | |
| Malaise*, count (%) | 0.045 | |||||||
| Silymarin | 46(84) | 28(51) | 19(37) | 13(25) | 10(22) | 4 (9) | 1(3) | |
| Placebo | 38(76) | 18(42) | 14(33) | 16(37) | 10(23) | 9 (20) | 4(11) | |
| Anorexia*, count (%) | 0.061 | |||||||
| Silymarin | 44(80) | 19(34) | 14(27) | 4(8) | 4(9) | 7 (16) | 1(3) | |
| Placebo | 36(72) | 14(33) | 9(21) | 6(14) | 5(11) | 8 (18) | 3(8) | |
| Nausea*, count (%) | 0.65 | |||||||
| Silymarin | 32(58) | 18(10) | 4(8) | 5(10) | 2(4) | 6 (14) | 2(5) | |
| Placebo | 32(64) | 9(21) | 8(19) | 6(14) | 3(7) | 5 (11) | 2(6) | |
| Vomiting*, count (%) | 0.68 | |||||||
| Silymarin | 21(38) | 1(2) | 0(0) | 0(0) | 1(2) | 3 (7) | 0(0) | |
| Placebo | 18(36) | 0(0) | 2(5) | 3(7) | 0(0) | 3 (7) | 1(3) | |
P-values estimated using generalized estimating equations based on a model of group, time from baseline, and their interaction with a binomial working model and robust standard errors.
Time fit using natural cubic spline terms of continuous days from baseline due to < 5 participants with or without symptom in at least one group during at least one visit. Otherwise, time fit using indicators for each visit. ALT, Alanine Aminotransferase; AST, Aspartate Aminotransferase; SD, standard deviation
Missing data did not differ between GEE and WEE analyses, and of the possible seven patient contacts, the average attendance was 6.1 (SD = 1.5) [silymarin group = 6.2 (1.4), placebo = 6.1 (1.6)]. Although attendance was less (74 of 105) for the 8-week follow-up, 88% of the total possible visits were attended. No serious adverse events were recorded and side-effects were similar in frequency and uncommon in either group (Table 3). Diarrhea, previously reported as a side-effect of silymarin therapy, was rare, and not more frequent in the silymarin group.
Table 3.
The side-effect rate ratios (silymarin compared to placebo) with 95% confidence intervals.
| Rate Ratio | (95% CI) | Silymarin Complaints/person-visits | Placebo Complaints/person-visits | P-value | |
|---|---|---|---|---|---|
| Abdominal Pain | 1.01 | (0.50, 2.05) | 17/261 | 15/232 | 0.99 |
| Diarrhea | 1.48 | (0.66, 3.57) | 15/263 | 9/236 | 0.35 |
| Nausea | 0.89 | (0.27, 2.91) | 6/260 | 6/231 | 0.84 |
| Vomiting | 0.55 | (0.10, 2.32) | 3/260 | 5/232 | 0.41 |
| Constipation | 0.37 | (0.05, 1.8) | 2/260 | 5/231 | 0.23 |
| Increased fatigue | 0.39 | (0.08, 1.45) | 3/260 | 7/231 | 0.16 |
| Insomnia | 1.30 | (0.20, 11.2) | 3/260 | 2/231 | 0.78 |
| Skin Rash | NA* | -- | 0/260 | 0/231 | NA* |
No participants reported skin rash during follow-up
Methods: rate ratios calculated by median-unbiased estimation and confidence intervals calculated using exact methods.
CI, confidence interval; NA, not applicable
DISCUSSION
This RCT compared the safety and effect of a standard dose of silymarin three times daily to a placebo in patients with acute hepatitis. No adverse events or side-effects were detected thereby supporting silymarin’s safety and tolerability. The study was not designed to evaluate the effect of silymarin on individual viral causes of acute hepatitis, thus making our findings generalizable to other clinically diagnosed cases of acute clinical hepatitis.
Although reports from Europe in the late-1970s suggested that silymarin was beneficial to patients with acute clinical hepatitis, they were not subsequently replicated.(Bode et al., 1977, Magliulo et al., 1978, Patera, 1978) Since then, studies focused on chronic viral infections or alcoholic hepatitis showed inconsistent results.(Deak et al., 1990, Strickland et al., 2005, Tanamly et al., 2004) Although silymarin is known to have non-specific hepatoprotective effects, yet most studies on chronic hepatitis focused on specific outcomes that are known to be unaffected by silymarin, e.g., viral clearance, liver cirrhosis, and liver-related mortality. This culminated in the conclusion of recent meta-analyses of the literature (almost exclusively studies on chronic hepatitis) that there is insufficient evidence to support or refute the use of silymarin in treatment of chronic viral hepatitis.(Jacobs et al., 2002, Mayer et al., 2005, Rambaldi et al., 2005)
However, a recent publication by Ferenci et al. demonstrated that high doses of intravenous silibinin had a potent antiviral effect in chronically infected HCV patients (Ferenci et al. 2008). Furthermore, patients treated with high doses of silymarin (or its most active component, silybin) shortly after ingesting the deadly toadstool, Amanita phalloides, survive; and multiple studies of silymarin in experimental animal models show it has a broad spectrum of hepatoprotective and antioxidant effects, protecting them against injury from several toxins, including Amanita phalloides, carbon tetrachloride, ethanol, and galactosamine, even when given after exposure.(Vogel et al., 1984)
Our definition for acute clinical hepatitis was the presence of an ALT level > 2.5 times normal and compatible clinical symptoms and signs of less than one month duration in the absence of a history of toxic exposures. Sixty (57.1%) of our patients were diagnosed with AVH. Another 19 (18.1%) were diagnosed as “flare-ups” of chronic viral infections, with all but one of these having chronic HCV. We previously reported that “flare-ups” of chronic HCV are a very common cause of a milder form of acute hepatitis in Egypt.(Meky et al., 2006) Also, since testing for anti-HCV IgM is an inadequate indicator of acute HCV infection, some of our patients having both anti-HCV and HCV-RNA could have been acute incident cases that presented to the hospital after developing detectable anti-HCV.
The trend for greater improvement in symptoms and signs related to biliary retention in subjects receiving silymarin is biologically plausible given that silymarin is known to act by membrane stabilization, and neutralization and scavenging of free radicals, thereby possibly protecting neighboring healthy hepatocytes from lysozymes and free radicals released by damaged cells. This would reduce inflammation thereby relieving mechanical compression of bile canaliculi and allowing better excretion of bile and bile salts. Our modest sample size and multiple etiologies for acute hepatitis may have attenuated a true finding.
Other than indirect bilirubin (p=0.012), many of the significant improvements in this clinical trial were either clinical (dark urine, jaundice and scleral icterus) or subjectively reported (fatigue, malaise and anorexia). These “soft” findings are not unique to our study. A recent report by Seeff et al examining reported self-use and potential effects of silymarin was conducted in the Hepatitis C Antiviral Long-Term Treatment Against Cirrhosis (HALT-C) Trial on its 1,145 study participants. Silymarin use was self-motivated and uncontrolled and constituted 72% of 60 herbals used at enrollment. There was no significant improvement in ALT. After adjusting for covariates of age, race, education, alcohol consumption, exercise, body mass index, and smoking, silymarin users were found to have significantly fewer liver-related symptoms such as fatigue (p=0.01), nausea (p=0.02), liver pain (p=0.02), anorexia (p=0.01), muscle and joint pain (p=0.003), and they had higher quality of life scores (all p<0.03).(Seeff et al., 2008)
Many patients in Egypt and elsewhere are empirically given silymarin for symptomatic management of acute hepatitis, particularly AVH.(Strickland, 2006) Although our study showed that the standard 420 mg daily dose of silymarin is safe and well-tolerated by patients with acute clinical hepatitis, it showed a trend towards improvement that was mostly subjective and clinical without a corresponding decline in biomarkers of inflammation. The dose of silymarin currently recommended is a fraction of that given in successful experimental animal studies,(Vogel et al., 1984) and this report and others show the standard 420 mg dose per day of silymarin to be safe and well tolerated. The fact that effects of silymarin were noted mainly on subjective symptoms suggests that there may be a potential beneficial effect of silymarin that is not being captured by traditional laboratory biomarkers, and future studies should incorporate novel biomarkers that can correlate with reported symptoms improvement. Alternatively, larger studies and higher doses of silymarin in both acute and chronic hepatitis may be warranted to detect measurable differences in traditional biomarkers of viral hepatitis such as liver enzymes and viral loads.
Acknowledgments
Manuscript preparation. The funding agencies and Madaus GmbH, either directly or through a third party, had no role in the study design, gathering, preparation, or analyzing the data, or in the writing of the manuscript.
We thank the staff of Tanta and Banha Fever Hospitals, including Drs. El-Menshawy, Khalaf, Farouk, Rabea, and the Data Management Team and Viral Hepatitis Research Laboratory at the National Hepatology & Tropical Medicine Research Institute. We also thank Meaghan E. Donovan, MS, doctoral student at the University of Maryland School of Pharmacy for her help in data management. Financial Support for this project was provided in part by the Wellcome Trust-Burroughs Wellcome Fund grants 059113/z/99/a and 059113/z/99/z; and the NIH International Collaborations in Infectious Disease Research (U01AI058372). The silymarin and placebo capsules were donated by Madaus GmbH.
Footnotes
ClinicalTrials.gov Identifier: NCT00412763
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abdel-Hamid M, Edelman DC, Highsmith WE, Constantine NT. Optimization, assessment, and proposed use of a direct nested reverse transcription-polymerase chain reaction protocol for the detection of hepatitis C virus. J Hum Virol. 1997;1:58–65. [PubMed] [Google Scholar]
- Ball KR, Kowdley KV. A review of Silybum marianum (milk thistle) as a treatment for alcoholic liver disease. J Clin Gastroenterol. 2005;39:520–528. doi: 10.1097/01.mcg.0000165668.79530.a0. [DOI] [PubMed] [Google Scholar]
- Bode JC, Schmidt U, Durr HK. Silymarin for the treatment of acute viral hepatitis? Report of a controlled trial (author’s transl) Med Klin. 1977;72:513–518. [PubMed] [Google Scholar]
- Boigk G, Stroedter L, Herbst H, Waldschmidt J, Riecken EO, Schuppan D. Silymarin retards collagen accumulation in early and advanced biliary fibrosis secondary to complete bile duct obliteration in rats. Hepatology. 1997;26:643–649. doi: 10.1002/hep.510260316. [DOI] [PubMed] [Google Scholar]
- Chalmers TC, Eckhardt RD, Reynolds WE, Cigarroa JG, Jr, Deane N, Reifenstein RW, Smith CW, Davidson CS. The treatment of acute infectious hepatitis. Controlled studies of the effects of diet, rest, and physical reconditioning on the acute course of the disease and on the incidence of relapses and residual abnormalities. J Clin Invest. 1955;34:1163–1235. doi: 10.1172/JCI103164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corwin AL, Dai TC, Duc DD, Suu PI, Van NT, Ha LD, Janick M, Kanti L, Sie A, Soderquist R, Graham R, Wignall SF, Hyams KC. Acute viral hepatitis in Hanoi, Viet Nam. Trans R Soc Trop Med Hyg. 1996;90:647–648. doi: 10.1016/s0035-9203(96)90418-6. [DOI] [PubMed] [Google Scholar]
- Deak G, Muzes G, Lang I, Niederland V, Nekam K, Gonzalez-Cabello R, Gergely P, Feher J. Immunomodulator effect of silymarin therapy in chronic alcoholic liver diseases. Orv Hetil. 1990;131:1291–1292. 1295–1296. [PubMed] [Google Scholar]
- Ferenci P, Scherzer TM, Kerschner H, Rutter K, Beinhardt S, Hofer H, Schöniger-Hekele M, Holzmann H, Steindl-Munda P. Silibinin is a potent antiviral agent in patients with chronic hepatitis C not responding to pegylated interferon/ribavirin therapy. Gastroenterology. 2008 Nov;135(5):1561–7. doi: 10.1053/j.gastro.2008.07.072. Epub 2008 Aug 3. [DOI] [PubMed] [Google Scholar]
- Hruby K, Csomos G, Fuhrmann M, Thaler H. Chemotherapy of Amanita phalloides poisoning with intravenous silibinin. Hum Toxicol. 1983;2:183–195. doi: 10.1177/096032718300200203. [DOI] [PubMed] [Google Scholar]
- Jacobs BP, Dennehy C, Ramirez G, Sapp J, Lawrence VA. Milk thistle for the treatment of liver disease: a systematic review and meta-analysis. Am J Med. 2002;113:506–515. doi: 10.1016/s0002-9343(02)01244-5. [DOI] [PubMed] [Google Scholar]
- Lee DY, Liu Y. Molecular structure and stereochemistry of silybin A, silybin B, isosilybin A, and isosilybin B, Isolated from Silybum marianum (milk thistle) J Nat Prod. 2003;66:1171–1174. doi: 10.1021/np030163b. [DOI] [PubMed] [Google Scholar]
- Luper S. A review of plants used in the treatment of liver disease: part 1. Altern Med Rev. 1998;3:410–421. [PubMed] [Google Scholar]
- Luper S. A review of plants used in the treatment of liver disease: part two. Altern Med Rev. 1999;4:178–188. [PubMed] [Google Scholar]
- Magliulo E, Gagliardi B, Fiori GP. Results of a double blind study on the effect of silymarin in the treatment of acute viral hepatitis, carried out at two medical centres (author’s transl) Med Klin. 1978;73:1060–1065. [PubMed] [Google Scholar]
- Mayer KE, Myers RP, Lee SS. Silymarin treatment of viral hepatitis: a systematic review. J Viral Hepat. 2005;12:559–567. doi: 10.1111/j.1365-2893.2005.00636.x. [DOI] [PubMed] [Google Scholar]
- Meky FA, Stoszek SK, Abdel-Hamid M, Selim S, Abdel-Wahab A, Mikhail N, El-Kafrawy S, El-Daly M, Abdel-Aziz F, Sharaf S, Mohamed MK, Engle RE, Emerson SU, Purcell RH, Fix AD, Strickland GT. Active surveillance for acute viral hepatitis in rural villages in the Nile Delta. Clin Infect Dis. 2006;42:628–633. doi: 10.1086/500133. [DOI] [PubMed] [Google Scholar]
- Mulrow C, Lawrence V, Jacobs B, Dennehy C, Sapp J, Ramirez G, Aguilar C, Montgomery K, Morbidoni L, Arterburn JM, Chiquette E, Harris M, Mullins D, Vickers A, Flora K. Milk thistle: effects on liver disease and cirrhosis and clinical adverse effects. Evid Rep Technol Assess (Summ) 2000:1–3. [PMC free article] [PubMed] [Google Scholar]
- Muriel P, Mourelle M. Prevention by silymarin of membrane alterations in acute CCl4 liver damage. J Appl Toxicol. 1990;10:275–279. doi: 10.1002/jat.2550100408. [DOI] [PubMed] [Google Scholar]
- Patera L. Silymarin in the treatment of acute viral hepatitis. Cesk Gastroenterol Vyz. 1978;32:533–534. [PubMed] [Google Scholar]
- Pietrangelo A, Borella F, Casalgrandi G, Montosi G, Ceccarelli D, Gallesi D, Giovannini F, Gasparetto A, Masini A. Antioxidant activity of silybin in vivo during long-term iron overload in rats. Gastroenterology. 1995;109:1941–1949. doi: 10.1016/0016-5085(95)90762-9. [DOI] [PubMed] [Google Scholar]
- Rambaldi A, Jacobs BP, Iaquinto G, Gluud C. Milk thistle for alcoholic and/or hepatitis B or C liver diseases--a systematic cochrane hepato-biliary group review with meta-analyses of randomized clinical trials. Am J Gastroenterol. 2005;100:2583–2591. doi: 10.1111/j.1572-0241.2005.00262.x. [DOI] [PubMed] [Google Scholar]
- Robins J, Rotnitzky A, Zhao L. Analysis of Semiparametric Regression Models for Repeated Outcomes in the Presence of Missing Data. Journal of the American Statistical Association. 1995 Mar;90:106–121. [Google Scholar]
- Saller R, Meier R, Brignoli R. The use of silymarin in the treatment of liver diseases. Drugs. 2001;61:2035–2063. doi: 10.2165/00003495-200161140-00003. [DOI] [PubMed] [Google Scholar]
- Seeff LB, Curto TM, Szabo G, Everson GT, Bonkovsky HL, Dienstag JL, Shiffman ML, Lindsay KL, Lok AS, Di Bisceglie AM, Lee WM, Ghany MG. Herbal product use by persons enrolled in the hepatitis C Antiviral Long-Term Treatment Against Cirrhosis (HALT-C) Trial. Hepatology. 2008;47:605–612. doi: 10.1002/hep.22044. [DOI] [PubMed] [Google Scholar]
- Shepard CW, Finelli L, Alter MJ. Global epidemiology of hepatitis C virus infection. Lancet Infect Dis. 2005;5:558–567. doi: 10.1016/S1473-3099(05)70216-4. [DOI] [PubMed] [Google Scholar]
- Strickland GT. Liver disease in Egypt: hepatitis C superseded schistosomiasis as a result of iatrogenic and biological factors. Hepatology. 2006;43:915–922. doi: 10.1002/hep.21173. [DOI] [PubMed] [Google Scholar]
- Strickland GT, Tanamly MD, Tadros F, Labeeb S, Makld H, Nessim D, Mikhail N, Magder LS, Afdhal NH, Medhat A, Abdel-Hamid M. Two-year results of a randomised double-blinded trial evaluating silymarin for chronic hepatitis C. Dig Liver Dis. 2005;37:542–543. doi: 10.1016/j.dld.2005.03.001. [DOI] [PubMed] [Google Scholar]
- Tanamly MD, Tadros F, Labeeb S, Makld H, Shehata M, Mikhail N, Abdel-Hamid M, Abu-Baki L, Medhat A, Magder LS, Afdhal NH, Strickland GT. Randomised double-blinded trial evaluating silymarin for chronic hepatitis C in an Egyptian village: study description and 12-month results. Dig Liver Dis. 2004;36:752–759. doi: 10.1016/j.dld.2004.06.015. [DOI] [PubMed] [Google Scholar]
- Tsarev SA, Tsareva TS, Emerson SU, Kapikian AZ, Ticehurst J, London W, Purcell RH. ELISA for antibody to hepatitis E virus (HEV) based on complete open-reading frame-2 protein expressed in insect cells: identification of HEV infection in primates. J Infect Dis. 1993;168:369–378. doi: 10.1093/infdis/168.2.369. [DOI] [PubMed] [Google Scholar]
- Vogel G, Tuchweber B, Trost W, Mengs U. Protection by silibinin against Amanita phalloides intoxication in beagles. Toxicol Appl Pharmacol. 1984;73:355–362. doi: 10.1016/0041-008x(84)90087-5. [DOI] [PubMed] [Google Scholar]
- Wagner H, Diesel P, Seitz M. Arzneim-forsch. 1974;24:466–471. [PubMed] [Google Scholar]
- Wang Y, Ling R, Erker JC, Zhang H, Li H, Desai S, Mushahwar IK, Harrison TJ. A divergent genotype of hepatitis E virus in Chinese patients with acute hepatitis. J Gen Virol. 1999;80(Pt 1):169–177. doi: 10.1099/0022-1317-80-1-169. [DOI] [PubMed] [Google Scholar]