Abstract
Background
The high comorbidity between depressive and anxiety disorders, especially among females, has called into question the independence of these two symptom groups. It is possible that childhood anxiety typically precedes depression in girls. Comparing of the predictive utility of symptoms of anxiety with the predictive utility of symptoms of depression from early childhood to early adolescence is needed to test this hypothesis.
Methods
Data from a population-based sample of 2,451 girls were used to examine age-related changes and year-to-year stability within and across symptoms of major depression, separation anxiety, and generalized/social anxiety by maternal report from ages 6 to 12. In addition, the predictive utility of symptoms of major depression, separation anxiety, and generalized/social anxiety at ages 7–10 years of age to depressive disorders at ages 11–13 was tested.
Results
Symptoms of separation anxiety demonstrated a linear decrease, depression symptoms a linear increase and symptoms of generalized/social anxiety an increase from 6–8, a plateau 8–10, followed by a decrease from 10–12 years. Year-to-year changes in symptoms of major depression were best predicted by depressive symptoms in the previous year, although a small amount of additional variance was accounted for by separation anxiety symptoms in early childhood and generalized/social anxiety symptoms in mid to later childhood. Age 8 was the earliest age from which depressive disorders in early adolescence could be predicted from symptoms of depression and generalized social anxiety.
Conclusions
Homotypic continuity of depression and anxiety symptoms from early childhood to early adolescence is more common in girls than heterotypic continuity. Some additional information about year-to-year changes in depression symptoms and later depressive disorder is gained by assessing anxiety symptoms. Depressive symptoms themselves, however, appear to be the strongest and most reliable predictor of later depression.
Keywords: Females, depression, anxiety, prediction
The comorbidity of anxiety and depressive disorders is one of the most consistently reported patterns of comorbidity among children and adolescents (Angold, Costello, & Erkanli, 1999). The high rate of comorbidity is observed in clinical (Karlsson et al., 2006) and community samples (Costello et al., 2003). In the Great Smoky Mountain Study, a longitudinal community study of 9–13-year-olds, the odds of co-occurring anxiety given a depressive disorder or vice versa was close to 30.0, and the two disorders were more likely to co-occur with each other than with attention-deficit hyperactivity disorder, the disruptive behavior disorders, or substance use disorders (Costello et al., 2003).
What do these data mean for the nature of the association between anxiety and depression? Some researchers have argued that the two disorders should be considered a single diagnostic entity. Using the Child Behavior Checklist (CBCL) to assess symptoms of anxiety and depression, Wadsworth and colleagues (2001) reported that a latent class analysis of the items in both a clinical and non-clinical sample revealed that anxiety and depression are part of the same continuum of problems. Stark et al. (1993) reported that 9–12-year-old children who had been diagnosed with depression, anxiety, or combined depression and anxiety did not differ from each other on their responses to self-report measures of anxiety, hopelessness, and self-esteem, and therefore proposed that anxiety and depression essentially form a higher-order factor that can be referred to as negative affectivity. These types of studies have led to the proposal that treating childhood anxiety disorders will prevent depression in adolescence (Flannery-Shroeder, 2006).
Others acknowledge that the overlap suggests some shared etiologic factors, but assert that there is still sufficient data in support of separate constructs (Crowley & Emerson, 1996; Kovacs & Devlin, 1998; Murphy, Marelich, & Hoffman, 2000; Muris, Schmidt, Merckelbach, & Schouten, 2001). In their review, Kovacs and Devlin (1998) presented several arguments favoring the independence of anxiety and depression. First, data from both epidemiologic and clinical studies demonstrate that homotypic continuity of depressive and anxiety disorders is more common than heterotypic continuity. Second, although comorbidity is high, there are many studies in which the majority of depressed children and adolescents do not report a co-occurring anxiety disorder. Third, the course of depressive and anxiety disorders does not appear to be significantly influenced by comorbidity.
Research on the developmental ontogeny of depression and anxiety is critical to this debate and could potentially resolve it. If depressive disorders are nearly always preceded by anxiety, then it is possible that the two symptom groups may be better thought of as a syndrome that begins with anxiety and emerges as depression or comorbid depression and anxiety. In order to demonstrate that childhood anxiety is a stepping-stone to later depression, one would need to contrast the predictive utility of anxiety with the predictive utility of depression. Results from prospective studies on the prediction of depression from anxiety are fairly equivocal. In the Children in the Community Study, a continuous measure of fears at age 13, but not a diagnosis of major depression, predicted major depression at 16 (Pine, Cohen, & Brook, 2001). A continuous measure of depression symptoms, however, was not included in the model. Thus, anxiety and depression were confounded with type of assessment: continuous versus categorical. In the Christchurch Health and Development Study, level of ‘anxious and withdrawn’ behaviors at age 8 predicted risk for major depression in late adolescence and early adulthood (Goodwin et al., 2004). Among the 10 items measuring anxiety and withdrawal were ‘crying easily or often,’ ‘often appearing miserable, unhappy or distressed,’ and ‘being overly serious or sad.’ Thus, it is possible that depressive disorders in adolescence and adulthood were preceded by endorsement of these items in childhood rather than anxiety items.
The Dunedin Study is one of the few studies within which the relative predictive utility of anxiety versus depression to later disorders was tested (Moffitt et al., 2007). The results demonstrated that anxiety and major depression had a reciprocal relation such that one preceded the onset of the other relatively equally from ages 11 to 32 years (Moffitt et al., 2007). Similar findings of reciprocal relations between anxiety and depression were reported in the Great Smoky Mountain Study, in which testing of heterotypic and homotypic patterns of stability in anxiety and depression was carried out using a much narrower age range from 9–16 (Costello et al., 2003). Because the data in both studies were collapsed across age, and anxiety disorders were combined into one group, the authors were unable to test whether the nature of the association between anxiety and depression is different depending on the age of assessment (e.g., childhood versus adolescence) and the type of anxiety disorder being assessed. In addition, Moffit and colleagues (2007) called for modeling correlational structures at the symptom level to determine whether their findings were influenced substantially by the requirement of meeting criteria for a disorder. Costello and colleagues (2003) pointed to the need to refine the study of comorbidity of anxiety and depression by studying specific anxiety disorders given that continuity and age of onset of the different anxiety disorders vary, and will therefore affect the developmental association with depression.
These issues and unanswered questions are especially relevant for females, for whom the rate of major depressive disorder (MDD), anxiety disorders, and their co-occurrence is high and more common than that observed in males (Costello et al., 2003; Joiner et al., 1999). In the context of greater interest in preventative interventions for mood disorders, particularly for females, establishing the early developmental inter- or independence of these two symptom groups is important and is required to determine whether the call to treat anxiety disorders to prevent depression has sufficient empirical support.
In the present study we use a population-based sample of girls for whom symptoms of depression, separation anxiety, and generalized/social anxiety were assessed by maternal report repeatedly from early childhood through early adolescence to answer the following questions:
What are the age-related changes in symptoms and disorders of generalized/social anxiety, separation anxiety, and depression in girls from childhood to adolescence;
Are there reciprocal associations between anxiety and depressive symptoms and disorders in childhood and early adolescence, and does the nature of the association vary as a function of the type of anxiety (i.e., separation anxiety versus generalized/social anxiety) and age;
Are symptoms of childhood separation anxiety disorder or generalized/social anxiety better predictors of depressive disorders than childhood depressive symptoms, and at what age are such symptoms predictive of depressive disorders?
Methods
Participants
In the Pittsburgh Girls Study (PGS), a stratified, random household sampling, with over-sampling of households in low-income neighborhoods, was used to identify girls who were between the ages of 5 and 8 years. Neighborhoods in which at least 25% of the families were living at or below the poverty level were fully enumerated (i.e., all homes were contacted to determine if the household contained an eligible girl), and a random selection of 50% of the households in all other neighborhoods were enumerated during 1998 and 1999. The enumeration identified 3,118 separate households in which an eligible girl resided. From these households, families who moved out of state and families in which the girl would be age ineligible by the start of the study were excluded. When two age-eligible girls were enumerated in a single household, one girl was randomly selected for participation. Of the 2,992 eligible families 2,875 (96%) were successfully re-contacted to determine their willingness to participate in the longitudinal study. Of those families, 85% agreed to participate, resulting in a total sample size of 2,451. The University of Pittsburgh Institutional Review Board approved all study procedures. Written informed consent was obtained from the primary caregiver and verbal assent from the child.
Approximately half of the girls were African American (52%), 41% were European American, and the remaining girls were described as multiracial or representing another race. Approximately a third of families reported receiving public assistance such as food stamps, Medicaid, or TANF (temporary aid to needy families) from the Department of Public Welfare.
Measures
Symptoms of major depressive disorder (DEP) were measured using the Childhood Symptom Inventory (CSI-4; Gadow & Sprafkin, 1994) based on caregiver report. The nine items measuring DSM-IV symptoms of depression that were endorsed as ‘a lot’, ‘all the time’ or ‘yes’ were summed to generate symptoms counts. Estimates of minor and major depressive disorders were generated using DSM-IV criteria for symptom thresholds.
Symptoms of separation anxiety disorder (SAD) and generalized/social anxiety (GSA) were measured by caregiver report using the Screen for Child Anxiety and Related Emotional Disorders (SCARED; Birmaher et al., 1997). On the separation anxiety factor, one question about the child being afraid of being alone in the house was scored as not applicable by 20% of the caregivers. Thus, this item was not included in the total score for the separation anxiety factor, resulting in a negligible change in the alpha coefficient (from .68 to .65). We estimated symptoms of separation anxiety disorder and generalized/social anxiety by counting endorsement of items at the level of ‘often,’ such as ‘often worries that something bad will happen to caregiver.’
The SCARED measures generalized anxiety in a way that is independent of depression. According to DSM-IV, five of the six additional symptoms of generalized anxiety disorder (GAD), in addition to worrying, are symptoms of depression (e.g., fatigue, difficulty concentrating). In contrast, the generalized anxiety factor as measured by the SCARED includes 9 items assessing worry about competence, like-ability, past acts, and the future. We thus refer to scores on this factor as generalized/social anxiety (GSA).
Data analysis
The PGS uses an accelerated longitudinal design, with relatively equal numbers of girls at ages 5, 6, 7, and 8 years being enrolled in the study at wave 1, followed by annual assessments. For most of the analyses in the present study we included ages for which at least half of the sample contributed data, resulting in a developmental span from ages 6 to 12 years. The total number of participants contributing data to each assessment is listed in Table 1. All analyses were conducted with weighted data to correct for the over-sampling of the low-income neighborhoods in order to generate prevalence rates that are representative of the population in the City of Pittsburgh. Given the large sample size, significant differences are reported for p values that are less than .01.
Table 1.
Number of participants at each age point by cohort and descriptive statistics
| Age | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|
| N | 1166 | 1746 | 2336 | 2315 | 2296 | 1736 | 1143 |
| 5 years | 554 | 548 | 550 | 545 | 538 | ||
| 6 years | 612 | 606 | 598 | 595 | 586 | 588 | |
| 7 years | 592 | 591 | 581 | 578 | 569 | 568 | |
| 8 years | 597 | 594 | 594 | 579 | 575 | ||
| DEP Mean (SD) | .47 (.89) | .46 (.84) | .50 (.88) | .51 (.90) | .56 (.95) | .64 (1.01) | .68 (1.12) |
| SAD Mean (SD) | .85 (1.12) | .75 (1.04) | .65 (1.03) | .50 (0.91) | .45 (.89) | .32 (.74) | .25 (.66) |
| GSA Mean (SD) | .55 (1.08) | .61 (1.22) | .65 (1.22) | .60 (1.18) | .63 (1.25) | .60 (1.14) | .48 (1.11) |
Note: DEP = depression symptoms; SAD = separation anxiety symptoms; GSA = generalized/social anxiety symptoms.
Analyses were conducted in three steps. First, to examine the overall developmental change across middle childhood and early adolescence, we estimated separate latent growth curve models (LGCM) for DEP, SAD, GSA symptoms using structural equation modeling (SEM). Each unconditional model, which included only the repeated measures, was fit followed by the conditional model, in which covariates (i.e., race, receipt of public assistance) were introduced. In the unconditional model, the mean and variance of the latent growth factors (i.e., intercept and slope) were estimated, and in the conditional model, the association between the covariates and the intercept and slope of the growth curve were tested. Model fit was evaluated using the root mean square error of approximation (RMSEA), and the comparative fit index (CFI), using the recommended cutoffs of ≤.06 for RMSEA (Hu & Bentler, 1999), and ≥.90 for CFI (Kline, 1998).
Second, we examined the time-specific relations between DEP and SAD and GSA symptoms, using autoregressive and cross-lagged structural models. These models allowed us to address whether anxiety symptoms precede depressive symptoms (or vice versa) and the timing of the effects. The cross-lagged associations were estimated while accounting for the autoregressive relations between later and earlier symptoms within each repeated measure. In these models we also compared the magnitude of the stability of the autoregressive with that for the cross-lagged paths. All analyses were carried out using Mplus 4.1 (Muthén & Muthén, 2007). All models in steps 1 and 2 were specified using maximum likelihood estimation with robust standard errors (MLR).
Third, we tested the predictive utility of DEP, SAD, and GSA symptoms at ages 6–10 years to depressive disorders at ages 11–13 years, to determine the earliest age at which the three symptoms groups are predictive of later depressive disorders.
Results
Age-related changes in symptoms and of generalized social anxiety, separation anxiety, and depression
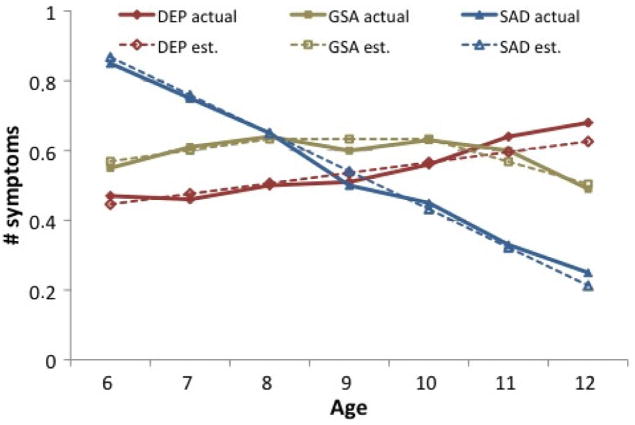
Age-related trends in maternal report of SAD, GSA and DEP symptoms from ages 6–12 are shown in Figure 1 and means and standard deviations at each age are presented in Table 1. For each of the repeated measures (i.e., SAD, GSA, and DEP symptoms) unconditional and conditional growth models were estimated separately.
Figure 1.
Age-related changes in symptoms of major depression (DEP), 1 separation anxiety (SAD), and generalized/social anxiety (GSA)
A linear model was the best fitting model for DEP symptoms (χ2 = 50.68, df = 32, p < .05; CFI = .99; RMSEA = .02). As shown in Figure 1, DEP symptoms increased across the 7-year period. There was significant individual variance around the intercept (σ2 = .30, p < .001) and the slope (σ2 = .01, p < .001). Race and receipt of public assistance were associated with the intercept but not the growth of depression symptoms; African American girls had higher levels of depressive symptoms than European American girls (β = .15, p < .001) and girls living in families receiving public assistance had more depressive symptoms than girls whose families did not receive public assistance (β = .15, p < .001).
A linear model also had the best fit for SAD symptoms (χ2 = 45.85, df = 22, p < .05; CFI = .98; RMSEA = .02). On average the level of SAD symptoms declined over time. There was significant individual variance around the intercept (σ2 = .85, p < .001) and the slope (σ2 = .02, p < .001). Race and receipt of public assistance were not associated with the intercept or slope of SAD symptoms.
The growth in GSA symptoms showed a nonlinear pattern. A piecewise growth model was estimated with a linear increase between ages 6 and 8 (slope1 = .03, SE = .01 p < .05), no change between ages 8 and 10, and a linear decrease between ages 10 and 12 (slope2 = −.06, SE = .02, p < .001). Variance around the intercept was significant (σ2 = .89, p < .001), as was the variance for slope1 (σ2 = .12, p < .001) and slope2 (σ2 = .14, p < .001). The model provided a good fit with the data (χ2 = 77.61, df = 18, p < .001; CFI = .96; RMSEA = .04). Race and receipt of public assistance were not associated with the intercept or the slope of GSA symptoms.
Reciprocal associations between anxiety and depressive symptoms
To examine the time-specific effect of anxiety symptoms (SAD and GSA) on DEP symptoms and of DEP symptoms on anxiety symptoms, two bivariate autoregressive and cross-lagged path models were fitted and several nested models were tested. In the preliminary analyses racial differences were tested by fitting the models by racial groups and no differences were found. The final analyses were conducted using the whole sample. Fit indices of these models are summarized in Table 2. The baseline model consisted of only autoregressive relations within each repeated measures. In all these models, errors of different constructs (e.g., SAD and DEP) measured at the same point in time were correlated, and errors of the same construct measured at non-adjacent time-points were correlated. The Satorra–Bentler scaled difference chi-square tests were used to compare the nested models (Satorra & Bentler, 2001), because chi-square values generated with MLR as the estimator cannot be used for chi-square difference tests directly (Muthén & Muthén, 2007).
Table 2.
Fit indices of autoregressive and cross-lagged models and model comparisons
| Model | X2 | df | CFI | RMSEA | Model comparison | ΔX2 (df = 6) |
|---|---|---|---|---|---|---|
| DEP and SAD model | ||||||
| 1. Autoregressive | 376.31*** | 48 | .90 | .06 | ||
| 2. Autoregressive + SAD → DEP cross-lagged paths | 344.56*** | 42 | .91 | .06 | 2 vs. 1 | 32.10*** |
| 3. Autoregressive + DEP → SAD cross-lagged paths | 359.38*** | 42 | .90 | .06 | 3 vs. 1 | 17.25** |
| 4. Full model | 329.07*** | 36 | .91 | .06 | 4 vs. 2 | 15.81* |
| 4 vs. 3 | 30.75*** | |||||
| DEP and GSA model | ||||||
| 1. Autoregressive | 388.01*** | 48 | .90 | .06 | ||
| 2. Autoregressive + GSA → DEP cross-lagged paths | 360.28*** | 42 | .91 | .06 | 2 vs. 1 | 26.48*** |
| 3. Autoregressive + DEP → GSA cross-lagged paths | 372.68*** | 42 | .90 | .06 | 3 vs. 1 | 14.50* |
| 4. Full model | 345.29*** | 36 | .91 | .06 | 4 vs. 2 | 13.25* |
| 4 vs. 3 | 25.31*** | |||||
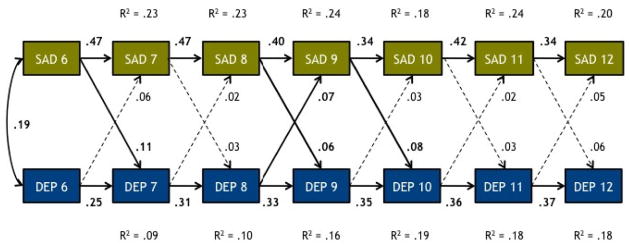
For SAD and DEP symptoms, the fit of the baseline model was only marginally adequate, suggesting that additional relations needed to be included. In the second model, all cross-lagged paths from time t SAD symptoms to time t+1 DEP symptoms were added, and this resulted in a significant improvement in the model fit. In the third model, all cross-lagged paths from prior DEP symptoms to the next assessment of SAD symptoms were added, which further improved the model fit (Table 2). The final model for SAD and DEP symptoms is presented in Figure 2. SAD symptoms were moderately stable (βs = .34–.47, ps < .001) from ages 6–12 years. Autoregressive paths for DEP symptoms ranged from .25 (age 6) to .37 (age 12), p values all < .001. Three of the six paths from SAD to subsequent DEP symptoms were significant at p < .01 with higher levels of SAD symptoms at ages 6, 8, and 9 predicting DEP symptoms at ages 7, 9, and 10, respectively. Only one of the cross-lagged paths from DEP symptoms to SAD symptoms (DEP at age 8 to SAD at age 9) was statistically significant.1 Finally, to test whether DEP symptoms were more strongly associated with previous DEP symptoms than with previous SAD symptoms, the autoregressive path and the cross-lagged path between the same time points were set equal, and the model was re-estimated. With equality constraints the model fit significantly worsened, ΔX2 (6) = 224.29, p < .001, which indicated that compared with SAD symptoms, DEP symptoms were more strongly predictive of later DEP symptoms.
Figure 2.
Autoregressive cross-lagged model of symptoms of major depression (DEP) and separation anxiety (SAD). Note: All paths represented by solid lines are siginificant at the P >.01 level.
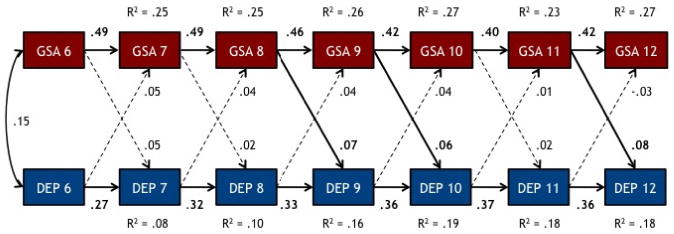
Similarly, the best fitting model for DEP and GSA symptoms included all the cross-lagged paths (see Table 2). The path coefficients for the final model are shown in Figure 3. Girls’ GSA symptoms were moderately stable over time (βs = .40–.49, p values all < .001). Three out of the six cross-lagged paths from GSA to DEP were significant. None of the paths from DEP symptoms to subsequent GSA symptoms was significant at p < .01. Adding the cross-lagged paths significantly improved the model fit from the baseline models, although the overall fit for the final model did not substantially change.
Figure 3.
Autoregressive cross-lagged model of symptoms of major depression (DEP) and generalized/social anxiety (GSA). Note: All paths represented by solid lines are siginificant at the P >.01 level.
The autoregressive path coefficients of DEP and cross-lagged path coefficients between GSA and DEP were compared by imposing the equality constraints as described above. The significant worsening of the model fit, ΔX2 (6) = 293.07, p < .001, suggested that the association between previous and later DEP symptoms were stronger than associations between previous GAS and later DEP symptoms.
Predictive validity of depression and anxiety symptoms to depressive disorders
Logistic regressions were computed to test whether and at what age symptoms of DEP, SAD, and GSA predicted depressive disorders. For these analyses symptoms at age 6 were not included because half of the girls who contributed data to age 6 symptoms did not have data at ages 11–13 and the other half contributed data for age 11 symptoms, but not at ages 12–13. Four percent of girls met DSM-IV criteria (APA, 1994) for a major or minor depression between the ages of 11 and 13 by maternal report. Four separate logistic regressions were computed with symptoms of DEP, SAD, and GSA at ages 7, 8, 9, and 10, respectively, entered simultaneously as the independent measures.
At ages 8, 9, and 10, DEP symptoms were significantly predictive of later depressive disorders, with each increase of 1 symptom resulting in a 1.5–1.8 fold increase in the odds of early adolescent major/minor depressive disorders (all p values ≤.001, and all lower limits of confidence intervals > 1.00). At ages 7, 8, and 10 GSA symptoms were predictive of later depressive disorders, with each increase of 1 symptom resulting in a 1.4-fold increase in the odds of early adolescent major/minor depressive disorders (all p values ≤.01, and all lower limits of confidence intervals > 1.00). Finally, only at age 9 were SAD symptoms associated with future diagnosis of major/minor depression, with each one unit increase in SAD symptoms resulting in an increase of 1.4 in the odds of a meeting criteria for a depressive disorder in early adolescence (95% CI = 1.08–1.77).
Discussion
In an effort to generate data that can inform preventative interventions for mood disorders in females, the present study aimed to establish the early developmental inter- and/or independence of anxiety and depressive symptoms in a population-based sample of girls, with the specific goal of addressing the hypotheses that anxiety often precedes depression and that treating anxiety disorders is one method of preventing later depressive disorders.
Regarding age-related changes, symptoms of separation anxiety disorder demonstrated a linear decrease from childhood to early adolescence, symptoms of major depression a linear increase, and symptoms of generalized/social anxiety showed an increase in early childhood, followed by a period of stability, and then a decrease during early adolescence. The pattern of age-related changes suggests that by combining or lumping anxiety disorders together may lead to obscuring important information on the developmental unfolding of the association between anxiety and depression.
Within each symptom group there was a moderate level of stability across age as demonstrated in the path analyses. Fitting models to account for the year-to-year change in depression and DEP, SAD, and GSA symptoms required both the auto-regressive paths and the cross-lagged paths. SAD symptoms that appeared earlier in childhood (i.e., 6, 8 and 9 years of age) were significantly associated with levels of DEP symptoms in the following year, even after controlling for earlier depression. The magnitude of the effect, however, was relatively small, with path coefficients ranging from .06 to .11.
The age at which GSA symptoms were prospectively associated with depressive symptoms was slightly later. The magnitude of effect was similar, with path coefficients from GSA to DEP symptoms ranging from .06 to .08. Interestingly, DEP symptoms had almost no effect on year-to-year changes in SAD and GSA symptoms. One can conclude from these data that among non-referred girls, symptoms of depression and anxiety are moderately stable and do not exert much influence on changes on one another over time. The level of depression in any subsequent year is best predicted by depression symptoms in the previous year, even in early childhood. Thus, there was not support for conceptualizing anxiety and depression symptoms as a unitary construct.
In the prediction of maternal report of minor or major depressive disorders in early adolescence, depressive symptoms reliably predicted risk for disorders beginning at age 8. Change in the level of symptoms of separation anxiety in childhood conferred risk for later depressive disorders only at one of the four ages (9 years), and change in the level of generalized/social anxiety at ages 7, 8 and 10 conferred risk for later depressive disorders. With each increase in number of symptoms of GSA during childhood there was a 40% increase in the risk of meeting criteria for a depressive disorder during early adolescence. For each increase in number of symptoms of MDD during childhood there was a 50–80% increase in the risk of meeting criteria for a depressive disorder during early adolescence. Thus, in contrast to the prediction of changes in symptom level, prediction of depressive disorders is further aided by information on the level of generalized/social anxiety symptoms.
The examination of the predictive utility of symptoms versus disorders is particularly relevant for prevention efforts. Results from a number of studies demonstrate that anxiety disorders are predictive of depressive disorders (e.g., Bittner et al., 2007; Moffitt et al., 2007) (although it is possible that adding depressive symptoms to those models may reduce the strength of the prospective association between anxiety and depressive disorders). Determining the predictive utility of changes in symptom levels, however, is important for identifying the age at which the benefit of prevention clearly outweighs the risk. Our results suggest that symptoms of depression in early childhood are relatively stable and that for each change in the number of depressive symptoms there is approximately a 50–80% increase in the risk of meeting criteria for a depressive disorder in early adolescence.
The fact that separation anxiety symptoms essentially lacked predictive utility to depressive symptoms or disorders, whereas generalized/social anxiety was predictive of later depressive disorders supports recent findings from the Great Smoky Mountain Study (Bittner et al., 2007). In that study, the predictive utility of all anxiety disorders during childhood to adolescent psychopathology was tested, including DSM-III-R overanxious disorder (OAD). DSM-IV SAD and GAD were not associated with adolescent depression, but OAD was. These authors called for reconsidering the decision made in DSM-IV to delete the diagnosis of OAD from the childhood disorders. Although we did not have separate measures of OAD and GAD, our generalized/social anxiety construct more closely resembles the nosology of OAD than of GAD, and our results support the contention that a disorder containing symptoms of general social anxiety, as opposed to physiological symptoms, is a meaningful and developmentally appropriate childhood disorder. Although symptom overlap among disorders is present throughout the DSM-IV noslogy, the overlap between GAD and MDD is particularly problematic. It is highly likely that a depressive-anxious subtype can be meaningfully distinguished from other depressive subtypes. Refining phenotypes by parsing them into subtypes will be critical for identifying the genetic and environmental liabilities for disorders. It will be virtually impossible to accomplish this when the symptoms defining disorders are more similar than different.
Three limitations need to be acknowledged when interpreting the results from this study. First, we relied solely on caregiver report of symptoms. Avoiding the confounding of informant with age is a conundrum for those who aim to test hypotheses across developmental periods. Reliable self-report measures of anxiety and depression prior to the age of 9 that can be used with a large sample are virtually non-existent. Consequently our methods do not include self-reports of symptoms until the age of 9. Combining data from informants, especially for depression, may also not be optimal given the low correspondence between caregiver and child report and the possibility that each informant is reporting a different phenotype in terms of onset, duration, and impairment (Braaten et al., 2001). For these reasons we used caregiver only, which may result in an under-estimate of depressive disorders during early adolescence.
Second, we did not use a single diagnostic interview to generate symptoms. Thus, our data are not quite comparable to studies that used DSM-III-R or DSM-IV based-interviews to measure anxiety and depression symptoms. Although our measure of depressive symptoms was consistent with DSM-IV and allowed us to generate estimates of disorders, our measure of anxiety symptoms did not afford the opportunity to generate estimates of DSM-IV anxiety disorders. On the other hand, our goal was to compare the predictive utility of anxiety and depressive symptoms to changes in depressive symptoms and later disorders to add to the existing literature on disorders, and we accomplished that goal with our psychometrically sound measures of symptoms.
Third, studies of the prediction of depressive disorders typically extend to late adolescence. Our endpoint, in contrast, was early adolescence. Ultimately, it will be important to test whether the results of the present study are unchanged by including data from later developmental periods. We have also highlighted, however, the importance of extending the age of assessment in studies of prediction of depression to early childhood, given that symptoms of depression in childhood appear to be predictive of later disorder and impairment (Keenan et al., in press).
In summary, symptoms of separation and generalized/social anxiety appear to exert little to no effect on developmental changes in girls’ levels of symptoms of depression from early childhood to early adolescence. Increases in symptoms of generalized social anxiety during childhood were associated with increased risk of depressive disorders in early adolescence. These results support the conceptualization of anxiety and depression as separate but related constructs. In addition, depression appears to be a more reliable predictor of later depression than anxiety. Although there may be a subgroup of children for whom anxiety is a stepping-stone to depression, it does not appear to be a common pathway.
Key points
The high level of comorbidity between depressive and anxiety disorders, especially among females, has called into question the independence of these two symptom groups.
Determining whether childhood anxiety typically precedes the onset of depression in girls is critical for the successful prevention of depressive disorders.
This is among the first studies in which hypotheses about the nature of the association between clinically relevant symptoms of anxiety and depression from childhood versus adolescence are tested.
Results demonstrate that homotypic continuity of depression and anxiety symptoms from early childhood to early adolescence is more common in girls than heterotypic continuity.
Depressive symptoms themselves, as opposed to symptoms of separation or generalized/social anxiety, appear to be the strongest and most reliable predictor of later depression.
Abbreviations
- DEP
symptoms of major depressive disorder
- MDD
major depressive disorder
- SAD
symptoms of separation anxiety disorder
- GSA
symptoms of generalized/social anxiety
- GAD
generalized anxiety disorder
- OAD
overanxious disorder
Footnotes
Conflict of interest statement: No conflicts declared.
In Figure 2 we note that path coefficients of apparent similar magnitudes were not all statistically significant. To provide further insights on how to interpret the significance of coefficients with similar magnitudes, we compared the sizes of these paths coefficients by 1) constraining all 6 cross-lagged paths of the same direction to be equal and 2) constraining each pair of the reciprocal cross-lagged paths to be equal, and comparing the model fit between constrained versus non-constrained models. The small and nonsignificant chi-square difference scores indicated that the magnitudes of these coefficients are comparable despite the different levels of statistical significance.
Supporting Information
Additional Supporting Information may be found in the online version of this article:
Table 3 (Correlations of MDD and SAD symptoms between ages 6 and 12) and Table 4 (Correlations of DEP and GSA symptoms between ages 6 and 12). (Word files)
Please note: Wiley-Blackwell are not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Angold A, Costello JE, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, et al. The Screen for Child Anxiety Related Emotional Disorders: Scale construction and psychometric characteristics. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Bittner A, Egger HL, Erkanli A, Costello JE, Foley DL, Angold A. What do childhood anxiety disorders predict? Journal of Child Psychology and Psychiatry. 2007;48:1174–1183. doi: 10.1111/j.1469-7610.2007.01812.x. [DOI] [PubMed] [Google Scholar]
- Braaten EB, Biederman J, DiMauro A, Mick E, Monuteaux MC, Muehl K, Faraone SV. Methodological complexities in the diagnosis of major depression in youth: An analysis of mother and youth self-reports. Journal of Child and Adolescent Psychopharmacology. 2001;11:395–407. doi: 10.1089/104454601317261573. [DOI] [PubMed] [Google Scholar]
- Costello E, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Crowley SL, Emerson EN. Discriminant validity of self-reported anxiety and depression in children: Negative affectivity or independent constructs. Journal of Clinical Child Psychology. 1996;25:139–146. [Google Scholar]
- Flannery-Schroeder EC. Reducing anxiety to prevent depression. American Journal of Preventive Medicine. 2006;31:S136–S142. doi: 10.1016/j.amepre.2006.07.006. [DOI] [PubMed] [Google Scholar]
- Gadow KD, Sprafkin J. Child Symptom Inventory. Stony Brook, NY: State University of New York at Stony Brook; 1994. [Google Scholar]
- Goodwin RD, Fergusson DM, Horwood LJ. Early anxious/withdrawn behaviours predict later internalising disorders. Journal of Child Psychology and Psychiatry. 2004;45:874–883. doi: 10.1111/j.1469-7610.2004.00279.x. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Joiner TE, Blalock JA, Wagner KD. Preliminary examination of sex differences in depressive symptoms among adolescent psychiatric inpatients: The role of anxious symptoms and generalized negative affect. Journal of Clinical Child Psychology. 1999;28:211–219. doi: 10.1207/s15374424jccp2802_8. [DOI] [PubMed] [Google Scholar]
- Karlsson L, Pelkonen M, Ruuttu T, Kiviruusu O, Heila H, Holi M, Kettunen K, Tuisku V, Tuulio-Henriksson A, Torronen J, Marttunen M. Current comorbidity among consecutive adolescent psychiatric outpatients with DSM-IV mood disorders. European Child and Adolescent Psychiatry. 2006;15:220–231. doi: 10.1007/s00787-006-0526-7. [DOI] [PubMed] [Google Scholar]
- Keenan K, Hipwell AE, Feng X, Hinze AE, Babinski DE, Henneberger A, Rischall M. Subthreshold symptoms of depression in girls are stable and predictive of depressive disorders. Journal of the American Academy of Child and Adolescent Psychiatry. doi: 10.1097/CHI.0b013e3181886eab. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York: Guilford; 1998. [Google Scholar]
- Kovacs M, Devlin B. Internalizing disorders in childhood. Journal of Child Psychology and Psychiatry. 1998;39:47–63. [PubMed] [Google Scholar]
- Moffitt TE, Harrington H, Caspi A, Kim-Cohen J, Goldberg D, Gregory AM, Poulton R. Depression and generalized anxiety disorder: Cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years. Archives of General Psychiatry. 2007;64:651–660. doi: 10.1001/archpsyc.64.6.651. [DOI] [PubMed] [Google Scholar]
- Muris P, Schmidt H, Merckelbach H, Schouten E. Anxiety sensitivity in adolescents: Factor structure and relationships to trait and symptoms of anxiety disorders and depression. Behaviour Research and Therapy. 2001;39:89–100. doi: 10.1016/s0005-7967(99)00179-5. [DOI] [PubMed] [Google Scholar]
- Murphy DA, Marelich WD, Hoffman D. Assessment of anxiety and depression in young children: Support for two separate constructs. Journal of Clinical Child Psychology. 2000;29:383–391. doi: 10.1207/S15374424JCCP2903_9. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 4. Los Angeles, CA: Muthén & Muthén; 2007. [Google Scholar]
- Pine DS, Cohen P, Brook J. Adolescent fears as predictors of depression. Biological Psychiatry. 2001;50:721–724. doi: 10.1016/s0006-3223(01)01238-0. [DOI] [PubMed] [Google Scholar]
- Satorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66:507–514. doi: 10.1007/s11336-009-9135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stark KD, Kaslow NJ, Laurent J. The assessment of depression in children: Are we assessing depression or the broad-band construct of negative affectivity. Journal of Emotional and Behavioral Disorders. 1993;1:149–154. [Google Scholar]
- Wadsworth ME, Hudziak JJ, Heath AC, Achenbach TM. Latent class analysis of Child Behavior Checklist anxiety/depression in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:106–114. doi: 10.1097/00004583-200101000-00023. [DOI] [PubMed] [Google Scholar]