Abstract
Objective To use structural equation modeling to provide a preliminary examination of the relationship between parental support and conflict regarding physical activity behaviors in preadolescents with type 1 diabetes. Method Parent–child dyads (n = 85, M child age = 10.8) completed physical activity items from the Diabetes Family Behavior Scale, Diabetes Related Conflict Scale, and Self-Care Inventory. Children completed physical activity items from the Center for Disease Control's Youth Risk Behavior Surveillance System, and activity was further measured via 24 hr recall interviews assessing physical activity behavior on a typical day. Results Parental conflict was related to less frequent physical activity, whereas parental support was related to more frequent physical activity. Conclusions In this exploratory study, parental conflict and support for physical activity were related to physical activity in preadolescents with type 1 diabetes. Further research and development of interventions aimed at improving parental support and decreasing conflict around physical activity are warranted.
Keywords: adolescents, family conflict, family support, physical activity, type 1 diabetes
Physical activity is important for the management of type 1 diabetes, as it is associated with better metabolic control, fewer cardiovascular difficulties, and improved quality of life (American Diabetes Association [ADA], 2004). Despite the reported benefits, there is often a decline in physical activity that occurs during adolescence (Duncan, Duncan, Strycker, & Chaumeton, 2007). Thus, it is likely during preadolescence that these changes in physical activity begin to occur, making it an important developmental stage in which to examine the factors that contribute to rates of physical activity.
Increased parental support and involvement with all aspects of care in type 1 diabetes is related to improved adherence and glycemic control (La Greca et al., 1995), and adolescents who report having more supportive families have better metabolic control and self-care behaviors (LaGreca et al., 1995). Further, although parental support for physical activity in youth with type 1 diabetes has not been studied specifically, research in healthy children indicates that such support can improve children's physical activity (Heitzler, Martin, Duke, & Huhman, 2006), and this may also be the case in youth with type 1 diabetes.
With regard to adherence behaviors, the roles of parental support and conflict are not necessarily overlapping; however, both are related to youths’ overall adherence to the diabetes regimen (La Greca & Bearman, 2002). Therefore, examining both parental conflict and support is important for understanding youths’ adherence behaviors. Findings regarding parental roles in physical activity in youths with type 1 diabetes indicate that physical activity is frequently an area of conflict between parents and children, particularly in early and mid-adolescence (Schilling, Knalf, & Grey, 2006). In healthy youths, higher rates of parental support and participation in exercise have been related to increased youth physical activity (Heitzler et al., 2006).
The importance of parent factors in understanding adherence and physical activity in youths with type 1 diabetes is clear, especially in preadolescence when physical activity begins to decline. The current study proposed a model predicting physical activity in preadolescents with type 1 diabetes from parental conflict and support regarding physical activity. Specifically, the model proposed that parental support for physical activity would be related to increased rates of physical activity, whereas parental conflict around physical activity would be related to decreased rates of physical activity.
Method
Participants and Procedure
Participants were 85 preadolescent youths (52% girls; ages 9–11, M = 10.8 years, SD = .75) and their parents (93% mothers; mean age = 41.20, SD = 5.58) involved in a larger randomized controlled treatment study. Youths were fairly representative of the outpatient endocrinology clinics at a large, urban children's hospital and its satellite clinics in the mid-Atlantic (73% Caucasian, 73% of families earning >$75 K per year). Eligibility requirements included the ability to speak and write in English and being free of developmental disabilities, psychotic disorders, or other serious medical conditions. As the focus of the larger study was on preadolescents, females who had reached menarche were also excluded.
Approval for the study was obtained from the Institutional Review Board. Introductory letters were sent to all preadolescents within the ages of 8–11 at participating clinics. Phone contact was made to verify enrollment criteria and determine desire to participate. Overall, 265 families were sent letters describing the study. Of those, 200 were able to be contacted by phone and 130 were eligible to participate. Of the eligible families, 110 consented to participate and 85 completed baseline data. Following study consent, the majority of baseline questionnaires were completed at the child's next clinic visit, with a small percentage conducted over the telephone with a trained research assistant or through the mail. All data for the current study were obtained at the baseline assessment of the larger intervention trial.
Measures
Parental Support and Conflilct
Children and their parents completed the Diabetes Family Behavior Scale (DFBS; McKelvey et al., 1993). The DFBS lists parental behaviors supporting diabetes management and has good psychometric properties demonstrated (McKelvey et al., 1993). For the current study, three single items were utilized from both the parent and child measure assessing parental support and conflict around physical activity. The items assessing support were: “How often does your parent encourage you to participate in sports activities,” and “exercise with you.” The item assessing conflict was: “How often does your parent criticize you for not exercising regularly.” These items are rated from 1 (never) to 5 (at least once a day).
The Diabetes Responsibility and Conflict Scale (DRCS; Rubin, Young-Hyman, & Peyrot, 1989), conflict subscale, assesses the frequency of conflict around specific diabetes-care activities, and has demonstrated good psychometric properties in previous research (Rubin et al., 1989). The responses are rated from 1 (never) to 5 (all the time). For the current study, only one item from the child and parent report (how much parents and children argued about physical activity over the past month), was used.
Physical Activity
Children and their parents completed items from the Self-Care Inventory (SCI; La Greca, Swales, Klemp, & Madigan, 1988) and the 24 hr recall interview (Johnson, Silverstein, Rosenbloom, Carter, & Cunningham, 1986). Children also completed four physical activity items from the Center for Disease Control's (CDC) Youth Risk Behavior Surveillance System (YRBSS; CDC, 2003).
The SCI assesses how well adolescents have followed recommendations for specific diabetes-care behaviors and has been found to have adequate reliability and validity (Greco et al., 1990). Items are ranked from 1 (never do it) to 5 (always do this as recommended without fail). Both parents and children completed this measure. For the current study, the two items assessing exercising regularly and strenuously were used.
Johnson et al.'s (1986) 24 hr recall technique provides data about disease care behaviors by recording regimen behaviors on a typical day. Specifically, parents and children are asked in detail about all their disease care behaviors (eating, exercise, blood glucose checks, and insulin injections) the previous day (after determining the day was typical in terms of disease care behaviors). This measure has demonstrated good psychometric properties (Johnson et al., 1986). For the current study, number of minutes spent exercising on the assessed day was used as an indicator of a typical amount of a child's daily physical activity.
Youth also completed four questions about their physical activity from the CDC's YRBSS (CDC, 2003), which asks about the amount of hard, moderate, and strengthening physical activity over the past 7 days, and on how many sports teams the youth played during the past year. Items were averaged for a mean physical activity score. In the current sample, internal consistency was not strong (Cronbach's α = .59), similar to other research in this area (Mackey & La Greca, 2007). The questions were initially meant to be examined alone in epidemiological research. However, it is possible that the reliability of this measure is low because adolescents are involved with only one or two of the types of physical activity assessed on a regular basis, so including an average across all types of exercise may be important for capturing the full range of activity in which youth engage.
Overview of Data Analytic Procedures
The model assessing the relationship of parental support and conflict regarding physical activity to youths’ physical activity behaviors was analyzed using structural equation modeling in Mplus. The full information maximum likelihood procedure was used to include participants who had data missing, presumed to be missing at random. The data were screened for outliers and for indicators that were nonnormal (i.e., skewness >3, kurtosis >8). There was one outlier in the 24 hr recall measure of exercise that created significant kurtosis in this variable (10.53). When this one data point for that participant was removed, kurtosis for the variable was within normal limits (1.78). All other variables were within normal limits for skewness and kurtosis.
Overall model fit was assessed with a chi-squared analysis, root-mean-square error of approximations (RMSEA; values below .05 indicate good fit; Kline, 2005), comparative fit index (CFI; values above .95 indicate good fit; Kline, 2005), and the standardized root mean square residual (SRMR; values < .10 are acceptable; Kline, 2005). To determine significant paths, critical ratios (CR) were examined (above 1.95 was considered significant at the .05 level).
Results
Rates of Physical Activity
In general, youths in the current sample reported a fairly high amount of physical activity. Both youths and parents reported that the child “usually” gets the amount of recommended regular exercise on the SCI. On the 24 hr recall interview, the average reported minutes of physical activity on the previous day was 64.93.
Model Testing
The measurement model was tested to ensure that each of the observed variables was a sufficient indicator of the hypothesized latent variables. The proposed measurement model fit the data well [χ2 = 58.89 (51), p = .21, CFI = .97, RMSEA = .04, SRMR = .07]. All indicators sufficiently (CR > 1.95) measured the hypothesized latent variables.
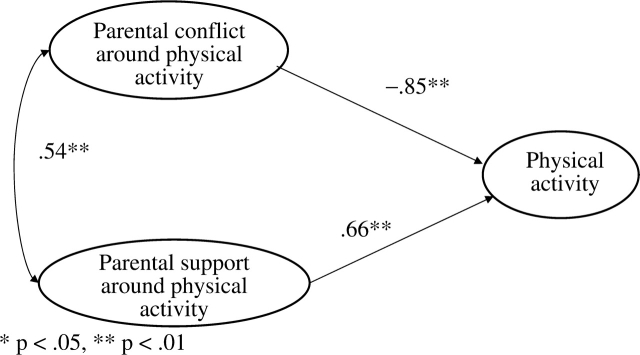
The proposed hybrid model demonstrated good fit [χ2 = 58.89 (51), p = .21, CFI = .97, RMSEA = .04, SRMR = .07]. Overall, this model accounted for 55% of the variance in physical activity (Figure 1). Results suggest that parental support for physical activity is related to more physical activity in youths with type 1 diabetes. Alternatively, parental conflict around physical activity is related to less physical activity.
Figure 1.
Model predicting physical activity.
Discussion
Physical activity is critical to good metabolic control in youths with type 1 diabetes (ADA, 2004). Because physical activity often declines in adolescence (Duncan et al., 2007), it is important to examine factors contributing to physical activity during an earlier, potentially more modifiable time of development, such as preadolescence. Results of the current study suggest that parents play an important role in their children's physical activity, and may be an important target of intervention and prevention programs.
Supporting hypotheses, parental support for and participation in physical activity was related to higher rates of physical activity in youths with type 1 diabetes. This is consistent with previous research finding that the more parents participate in physical activity with their children and model physical activity, the more likely their children are to engage in physical activity (Heitzler et al., 2006). It is also possible that parental participation is related to improved ability to help the child problem solve about when to exercise, decide in which type of exercise to engage, decrease difficulties related to safety exercising outside in an urban area, and encourage the perception of physical activity as “family time.”
Further, more parental conflict around physical activity was related to decreased activity in children with type 1 diabetes. This suggests that nagging and criticism, as well as arguing about physical activity, make a child less likely to engage in this activity.
Although the current study is largely exploratory, the findings have clinical implications that will be important to assess in future research. For example, current intervention programs aimed at improving diabetes care could emphasize family support and aim to reduce family conflict. Parents could be encouraged to participate in physical activity with their children, help their children join sports teams, and find ways to enable children to adhere to the recommendations for physical activity. Additionally, an intervention could promote family physical activity by helping parents design fun family activities that involve physical activity.
Findings also support the idea that parental conflict regarding physical activity should be discouraged. Further, psychoeducation provided upon diagnosis of type 1 diabetes or as part of regular care could include reminding parents that encouragement, rather than conflict, around issues of adherence, particularly physical activity, is important.
There are a few key limitations of the current study that should be noted. As there are no established measures to assess parental support and conflict concerning physical activity, and physical activity itself was assessed using single-item and self-report measures, the current study is largely exploratory in nature, and future research is needed to examine these preliminary findings further. Assessment tools such as accelerometers (shown to be a more objective measure of physical activity; Sallis & Saelens, 2000), or using exercise tolerance as an outcome variable should be employed in future research.
The sample size of the current study is small (less than 100 as suggested by Kline, 2005) and allows for an examination of only basic models. Therefore, future research with larger sample sizes should expand the model to include other important variables, such as knowledge about diabetes management, environmental factors, social–cognitive factors, or parent psychological functioning. Additionally, the current study is cross-sectional in nature. Examination of longitudinal data would enable us to determine a predictive relationship between parental support and conflict and physical activity.
The current study represents an important first step in understanding parental factors promoting physical activity in youths with type 1 diabetes. Clinicians should keep in mind that encouraging parental support of physical activity while reducing conflict in this area may help increase youths’ physical activity to improve metabolic control and general health.
Acknowledgments
The authors would like to acknowledge the help of Jaclyn Shepard, M.A. for her help with the literature review and Lifescan for donating blood glucose meters to families who participated in the study. This research was supported by grants DK062161 from NIDDK (to R.S.) and 5-MO1-RR-020359-04 for Children's National Medical Center's General Clinical Research Center.
Conflicts of interest: None declared.
References
- American Diabetes Association. Physical activity/exercise and diabetes. Diabetes Care. 2004;27:S58–S62. doi: 10.2337/diacare.27.2007.s58. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control. Youth Risk Behavior Surveillance Survey. 2003. [Retrieved September 21, 2007]. from http://www.cdc.gov/HealthyYouth/YRBS/data/2003/yrbs2003codebook.pdf.
- Duncan S, Duncan T, Strycker L, Chaumeton N. A cohort-sequential latent growth model of phsycial activity from ages 12 to 17 years. Annals of Behavioral Medicine. 2007;33(1):80–89. doi: 10.1207/s15324796abm3301_9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greco P, La Greca A, Ireland S, Wick P, Freeman C, Agramonte R, et al. Assessing adherence in IDDM: A comparison of two methods. Diabetes. 1990;40:A165. [Google Scholar]
- Heitzler CD, Martin SL, Duke J, Huhman M. Correlates of physical activity in a national sample of children aged 9-13 years. Preventive Medicine. 2006;42:254–260. doi: 10.1016/j.ypmed.2006.01.010. [DOI] [PubMed] [Google Scholar]
- Johnson SB, Silverstein J, Rosenbloom A, Carter R, Cunningham W. Assessing daily mangement in childhood diabetes. Health Psychology. 1986;5(6):545–564. doi: 10.1037/0278-6133.5.6.545. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling: 2nd. New York, NY: Guilford Press; 2005. [Google Scholar]
- La Greca AM, Auslander WF, Greco P, Spetter D, Fisher EB, Santiago JV. I get by with a little help from my family and friends: Adolescents’ support for diabetes care. Journal of Pediatric Psychology. 1995;20(4):449–476. doi: 10.1093/jpepsy/20.4.449. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Bearman KJ. The Diabetes Social Support Questionnaire-family version: Evaluating adolescents’ diabetes-specific support from family members. Journal of Pediatric Psychology. 2002;27(8):665–676. doi: 10.1093/jpepsy/27.8.665. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Swales T, Klemp S, Madigan S. In Ninth annual sessions of the society of behavioral medicine. Baltimore, MD: Society of Behavioral Medicine; 1988. Self care behaviors among adolescents with diabetes; p. A42. [Google Scholar]
- Mackey E, La Greca A. Adolescents’ eating, exercise, and weight control behaviors: Does peer crowd affiliation play a role? Journal of Pediatric Psychology. 2007;32:13–23. doi: 10.1093/jpepsy/jsl041. [DOI] [PubMed] [Google Scholar]
- McKelvey J, Waller D, North A, Marks J, Schreiner B, Travis L, et al. Reliability and validity of the Diabetes Family Behavior Scale. Diabetes Educator. 1993;19:125–132. doi: 10.1177/014572179301900206. [DOI] [PubMed] [Google Scholar]
- Rubin R, Young-Hyman D, Peyrot M. Parent-child responsibility and conflict in diabetes care. Diabetes. 1989;38:28A. [Google Scholar]
- Sallis JF, Saelens BE. Assessment of physical activity by self-report: Status, limitations, and future directions. Research Quarterly for Exercise and Sport. 2000;71:1–14. doi: 10.1080/02701367.2000.11082780. [DOI] [PubMed] [Google Scholar]
- Schilling LS, Knafl KA, Grey M. Changing patterns of self-management in youth with type 1 diabetes. Journal of Pediatric Nursing. 2006;21(6):412–424. doi: 10.1016/j.pedn.2006.01.034. [DOI] [PubMed] [Google Scholar]