Abstract
Background
Integrated group therapy, a new treatment for patients with bipolar disorder and substance use disorder, has previously been found to be efficacious in reducing substance use, but its length (20 sessions) and need for highly trained therapists may limit its adoption in substance use disorder community treatment programs. This paper compares a briefer (12-session) version of integrated group therapy, led by substance use disorder counselors without previous cognitive-behavioral training or bipolar disorder experience, to group drug counseling.
Methods
Sixty-one patients with bipolar disorder and substance dependence, taking mood stabilizers, were randomized to 12 sessions of integrated group therapy (n=31) or group drug counseling (n=30).
Results
Analyses of primary outcomes showed trends favoring integrated group therapy, with greater reduction in substance use during follow-up and a greater decline in risk of mood episodes during treatment. Secondary analyses favored integrated group therapy, with a significantly greater likelihood of achieving total abstinence, a significantly shorter time to the first abstinent month, and a significantly greater likelihood of achieving a “good clinical outcome” (a composite measure encompassing both substance use and mood simultaneously).
Conclusions
A shortened version of integrated group therapy can be delivered successfully by substance use disorder counselors, with better overall outcomes than those achieved with group drug counseling.
Keywords: substance abuse, bipolar disorder, substance dependence, treatment, group therapy, behavioral therapy
1. Introduction
Studies of community and clinical populations have consistently shown a high rate of co-occurrence of substance use disorder (SUD) and bipolar disorder (BD): 26-28% of community-based respondents with BD in the past year also had SUD within the past year (Grant et al., 2004) and 59.4% of BD patients in treatment had a lifetime SUD (Cassidy et al., 2001). Having both disorders is associated with worse outcomes than having either disorder alone, including slower recovery from mood episodes (Keller et al., 1986), poorer medication adherence (Keck et al., 1997), and a greater risk of suicidality (Dalton et al., 2003).
A number of recent studies have shown promising results for psychotherapeutic approaches, in combination with pharmacotherapy, for patients with BD (Colom et al., 2003; Frank et al., 2005; Lam et al., 2003; Miklowitz et al., 2007). These studies have not, however, specifically targeted individuals with co-occurring SUD. Similarly, numerous psychotherapy studies of SUD treatment have not focused on patients with co-occurring BD. Indeed, SUD psychotherapy trials often specifically exclude such individuals (Project MATCH, 1997; Crits-Christoph et al., 1999).
We have developed and tested a new manualized cognitive-behavioral group therapy for patients with BD and substance dependence, entitled integrated group therapy. Integrated group therapy focuses on the relationship between the two disorders, stressing similarities in the thoughts and behaviors typically involved in the recovery from each disorder (Weiss et al., 1999). Two previous studies have demonstrated the promise of integrated group therapy. In our initial open pilot study (Weiss et al., 2000a), patients receiving integrated group therapy had fewer days of drug use and more months of abstinence than a comparison group not receiving this treatment. In a subsequent randomized, controlled trial (Weiss et al., 2007), integrated group therapy was compared to group drug counseling (Daley et al., 2002), a manualized treatment that has been used successfully in previous addiction treatment research (Crits-Christoph et al., 1999); group drug counseling was designed to approximate the treatment typically delivered in SUD community treatment programs. In that study, integrated group therapy patients had fewer days of substance use both during the 20 weeks of treatment and during a 3-month post-treatment follow-up period. Integrated group therapy patients also had a shorter time from treatment initiation to their first full month of abstinence. Patients in both treatment conditions had a similar likelihood of mood episodes during both treatment and follow-up.
Because integrated group therapy has been shown to be efficacious in reducing substance use, we conducted the current study of a more “community-friendly” version of the treatment, to facilitate its adoption in SUD community treatment programs. In its original format, two aspects of integrated group therapy could limit the likelihood of its implementation in the wider SUD treatment community. First, our initial studies required that integrated group therapy be delivered by therapists with psychopathology training, knowledge of both BD and SUD, and experience conducting cognitive-behavioral therapy (CBT). When considering how to modify integrated group therapy to facilitate community implementation, we surveyed nine SUD community treatment programs in New England about their staffing patterns. We found that 85% of the clinicians in these programs were SUD counselors, most of whom had received no formal training in either CBT or BD. Indeed, many SUD clinicians who had a Master’s degree or a Ph.D. also did not have training in CBT, and still others had little experience with BD. A second barrier to community implementation was the length of integrated group therapy in our previous study, i.e., 20 sessions. Research has shown that the length of psychotherapy often does not exceed the number of sessions initially authorized by third-party payers (Liu et al., 1999). A review of agreements between McLean Hospital and its four largest third-party payers revealed that three of the companies initially authorized 12 sessions of psychotherapy, with justification required for more visits. We therefore revised the integrated group therapy manual by (1) reducing the number of sessions from 20 to 12, to increase the likelihood of reimbursement by third-party payers, e.g., managed care companies or state funding agencies; (2) including more basic information on CBT and BD, so that SUD counselors with little experience in these areas could conduct integrated group therapy; and (3) conducting the group in an open (sometimes called “rolling”) format, so that patients could begin at any time and continue for 12 weeks. The open format was initiated for this study (in contrast to our previous studies) because this is typical practice in most SUD community treatment programs (Washton, 2005). The purpose of the current study was to conduct a randomized controlled trial comparing 12 sessions of the revised “community-friendly” version of integrated group therapy to 12 sessions of group drug counseling, both conducted in an open format. In this trial, unlike in our two previous studies, both types of treatment were led by SUD counselors without CBT training or detailed knowledge of BD. We hypothesized that patients receiving integrated group therapy would have better substance use and mood outcomes than patients receiving group drug counseling.
2. Methods
The study protocol was approved by the McLean Hospital Institutional Review Board. Patients with current BD and substance dependence were recruited from McLean Hospital treatment programs, advertisements, fliers, and clinician referrals. Written informed consent was obtained after study procedures were fully explained. Inclusion criteria were (1) current diagnoses of BD and substance dependence other than nicotine, based on the Structured Clinical Interview for DSM-IV (SCID; First et al., 1996); (2) substance use within 60 days prior to intake; (3) a mood stabilizer regimen for ≥2 weeks, prescribed independently by the patient’s own physician; (4) ability to attend group therapy sessions and follow-up research visits at McLean Hospital; and (5) age ≥18. Exclusion criteria were (1) current psychosis, (2) current mania at the intake evaluation, (3) current danger to self or others, (4) current need for medical detoxification, (5) concurrent group treatment, and (6) residential treatment restricting substance use. Individual psychotherapy was permitted. Most patients in our previous studies of integrated group therapy attended individual psychotherapy (Weiss et al., 2007; Weiss et al., 2000b); excluding them would have created an unrepresentative sample.
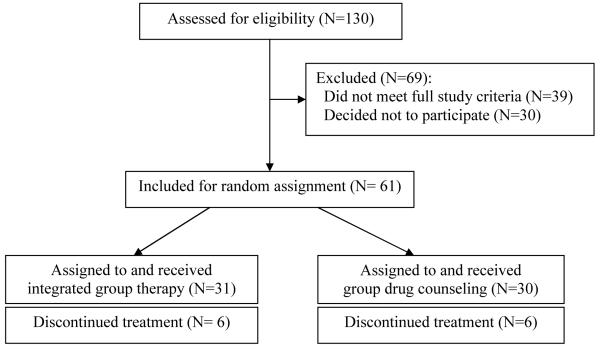
Participants who met study criteria were randomly assigned to integrated group therapy or group drug counseling (see Figure 1). Calculation of statistical power determined that, with a total sample size of N=61, the study had 80% power to detect a standardized effect size ≥0.47, corresponding to a medium effect size, given the longitudinal design and data analytic methodology (see below).
Figure 1.
Study flow chart
2.1. Assessments
Data related to the main outcomes of interest were collected at baseline and monthly for the next six months (3 months of treatment and 3 months of post-treatment follow-up). Psychiatric diagnoses were based on the SCID. SCID modules for mood, psychiatric, and anxiety disorders were administered by a trained Ph.D. or Master’s-level clinician, blinded to treatment condition. Baseline SUD diagnoses were determined using the SCID SUD module, administered by a trained, supervised research assistant.
Further, substance use data were obtained by a trained, supervised research assistant using the fifth edition of the Addiction Severity Index (ASI; McLellan et al., 1992). The ASI is a widely employed, multidimensional assessment of substance-related problems. The Timeline Follow-Back technique (Sobell and Sobell, 1992), which uses a calendar to assist recall, supplemented the drug and alcohol sections of the ASI. Days of substance use during the past month, derived from the ASI, was our primary substance use outcome measure; ASI drug and alcohol composite scores were secondary outcomes. To validate self-reports, urine toxicology screens were obtained at weekly group sessions and at monthly assessments. We previously reported a high degree of validity of substance use self-report data in this population (Weiss et al., 1998).
Mood episodes were assessed using the Longitudinal Interval Follow-Up Evaluation (LIFE; Keller et al., 1987), which combines the Hamilton Depression Rating Scale (Hamilton, 1960), the Young Mania Rating Scale (Young et al., 1978), and the symptom modules for mood and psychotic disorders on the SCID. The Hamilton depression and Young mania scales were administered monthly, and the SCID was completed at baseline and months 3 and 6. At all assessments, calendar methodology was utilized to review and record mood week by week. Our primary mood outcome, assessed weekly, was a binary measure of whether or not criteria were met for a DSM-IV depressive, manic, hypomanic, or mixed mood episode. Secondary mood measures examined depressive episodes and manic episodes (combining manic, hypomanic, and mixed episodes) separately. The LIFE also generates an overall weekly course rating. LIFE ratings of mood episodes were made by a doctoral-level rater, blinded to treatment condition.
An interview, the Treatment Services Review (McLellan et al., 1992), was used to collect data on additional treatment services that subjects might have received throughout the study. Medication adherence was assessed by asking patients each month to report how many days they had taken their various medications as prescribed. This interview was a modification of an instrument we have used previously to examine medication adherence in this population (Weiss et al., 1998).
2.2. Treatment conditions
Integrated group therapy (Weiss et al., 1999) consists of 12 weekly hour-long sessions and employs a cognitive-behavioral model that integrates the treatment of the two disorders by focusing on similarities between recovery and relapse processes in BD and SUD. A fundamental principle of integrated group therapy is that the same types of thoughts and behaviors that facilitate recovery from one disorder will enhance the likelihood of recovery from the other disorder. Conversely, similar types of thoughts and behaviors can be detrimental to recovery from both disorders; for example, parallels are drawn between “addictive thinking” and “depressive thinking.” Most sessions deal with topics explicitly relevant to both disorders (e.g., “Dealing with Depression without Using Alcohol or Drugs” and “Identifying and Fighting Triggers for Mania, Depression, and Substance Use”). The interaction between the two disorders is emphasized, e.g., by focusing on the adverse impact of substance abuse on the course of BD. Each session begins with a “check-in,” during which patients report their substance use, mood, medication adherence, and high-risk situations encountered during the past week; a didactic presentation and discussion of the weekly topic follow.
Group drug counseling (Daley et al., 2002) is an adaptation of the treatment delivered in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study (Crits-Christoph et al., 1999). Group drug counseling, designed to approximate the treatment patients receive in an SUD community treatment program, also consists of 12 weekly hour-long sessions, each focusing on a specific topic. The goals of group drug counseling are to (1) facilitate abstinence, (2) encourage mutual support, and (3) teach new ways to cope with substance-related problems. Sessions begin with a check-in for patients to report their substance use and craving; this is followed by SUD-related topics that do not specifically address mood. Group drug counseling is thus distinguishable from integrated group therapy by its single focus on substance use, rather than the dual focus of integrated group therapy on SUD and BD. Group drug counselors respond to mood or medication problems by discussing them briefly, then referring patients to their prescribing physician. Counselors attend to emergencies, however, until they are satisfactorily resolved.
Counselors
Counselors for both group treatments had Master’s degrees and at least three years of SUD treatment experience, but no previous formal training in CBT. Four counselors, two male and two female, led groups; three led groups for both treatment conditions, and one ran only integrated group therapy sessions. To encourage fidelity to the treatment manuals, all group sessions were recorded, and counselors were supervised weekly by more experienced counselors who had been trained to conduct the treatments by the manual authors (Roger Weiss, M.D., and Dennis Daley, Ph.D., respectively). Further, rating scales were completed by the supervisor after each session to assess adherence to the treatment condition and competence as a counselor. These scales have been found to be psychometrically sound, with good inter-rater reliability and discriminant validity (Weiss et al., 2007). Each counselor achieved mean adherence and competence ratings of 3.0 or greater on a 0-4 scale, which we had designated as an acceptable rating.
2.3. Statistical analysis
Background characteristics of patients were compared by treatment condition, using chi-square tests for categorical variables and independent t-tests for continuous variables. For the primary outcomes, repeated measures modeling methods assessed between-group differences in longitudinal change, during two phases: treatment and follow-up. To relax the assumption of normality for the continuous outcomes, generalized estimating equations (GEE) methods were implemented, using Stata V8.2 for Windows (Stata Version 8.2 for Windows, 2003). Marginal logistic regression models, with estimation via GEE, were used to model the log odds of the binary outcomes over time. We used an intent-to-treat analysis, including data from all randomized participants. To examine the effect of treatment, regression models included the effects of treatment condition, time, and the baseline measure of the outcome. For ease of interpretation, results of these analyses are presented in terms of changes from the baseline month to the last month of treatment and follow-up phases, respectively, and the between-group contrasts of these changes (see Table 2).
Table 2.
Effect of Integrated Group Therapy (IGT) versus Group Drug Counseling (GDC) on change in substance use, mood, and medication adherence over time (N=61)a
| Treatment phase |
Follow-up phase |
|||||
|---|---|---|---|---|---|---|
| Outcomesb | IGT | GDC | Difference | IGT | GDC | Difference |
| Primary | ||||||
| Days of any substance use | -14.3 (1.2) | -11.6 (1.4) | -2.7 (1.8) | -13.2 (1.2) | -10.2 (1.6) | -2.9 (1.8)* |
| Mood episode (% yes) | -1.7 (.4) | -1.1 (.4) | -0.6 (.4)* | -0.8 (.3) | -0.8 (.3) | -0.1(.4) |
| Secondary | ||||||
| Days of use | ||||||
| Any drugs (n=57) | -8.1 (.9) | -7.4 (1.0) | -0.7 (1.3) | -6.9 (1.0) | -5.7 (1.3) | -1.1 (1.4) |
| Any alcohol | -9.9 (1.0) | -9.0 (1.0) | -0.8 (1.3) | -9.2 (1.0) | -8.5 (1.3) | -0.6 (1.5) |
| Alcohol to intoxication | -9.9 (.6) | -9.2 (.5) | -0.8 (.7) | -8.9 (.9) | -7.7 (1.2) | -1.2 (1.2) |
| Addiction Severity Index Composite scores | ||||||
| Drug (n=57) | -0.06 (.01) | -0.05 (.01) | -0.01 (.01) | -0.05 (.01) | -0.05 (.01) | <0.01 (.02) |
| Alcohol | -0.11 (.03) | -0.14 (.03) | 0.03 (.04) | -0.12 (.04) | -0.21 (.03) | 0.10 (.04)** |
| Mood | ||||||
| Depressive episode (% yes) | -1.2 (.4) | -0.5 (.4) | -0.7 (.4)* | -0.6 (.4) | -0.5 (.4) | -0.1 (.5) |
| Manic episode (% yes)c | -2.1 (.6) | -2.1 (.6) | -0.02 (.6) | -0.8 (.5) | -0.8 (.4) | 0.04 (.6) |
| Hamilton depression scores | -5.0 (1.1) | -5.6 (1.2) | 0.6 (1.2) | -4.8 (1.1) | -5.5 (1.2) | 0.7 (1.4) |
| Young mania scores | -3.8 (.9) | -4.1 (1.1) | 0.4 (1.1) | -3.7 (1.0) | -2.5 (-1.2) | -1.2 (1.3) |
| Medication adherence | ||||||
| Rated | 5.5 (4.1) | 2.3 (3.4) | 3.3 (5.0) | 1.9 (4.8) | 3.9 (4.1) | -2.0 (5.7) |
Coefficients are followed by standard errors in parentheses.
Binary outcomes were measured weekly; other outcomes were measured monthly. Binary outcomes are expressed as log odds rather than as percentages (see text for detailed interpretation)
Includes manic, hypomanic, and mixed episodes
% of days taking mood stabilizers as prescribed
p<0.10;
p<0.05
A secondary substance use outcome was abstinence from both drugs and alcohol. Patients were compared by treatment condition on (1) their likelihood of attaining abstinence during treatment, using chi-square tests, and (2) time to first abstinent month, using Cox regression analysis, adjusted for baseline severity. We also examined the number of days using alcohol, the number of days using drugs other than alcohol, SUD severity as measured by ASI Drug and Alcohol Composite scores, weeks ill with depression, weeks ill with mania, Hamilton depression scores, Young mania scores, and medication adherence. For analyses separating drug use from alcohol use, patients (n=4) with no lifetime drug use disorder and no drug use throughout the study were excluded from analyses of drug use outcomes. Using an analogous procedure, no patients were excluded from analyses of alcohol use outcomes. Finally, we created a composite outcome measure similar to that created for other SUD studies (Anton et al., 2006; Cisler and Zweben, 1999); for this dually diagnosed population, patients were rated as having a “good clinical outcome” with respect to both disorders if they abstained from substance use and had no mood episodes during the last month of treatment. The same measure was used for the last month of follow-up.
3. Results
3.1. Baseline characteristics
The sample of 31 integrated group therapy patients and 30 group drug counseling patients was 41.0% female and mostly white (91.8%). Mean age was 38.3 (sd=11.1) years. Half of the sample (49.2%) had completed college, and just under half (45.9%) were currently employed. Most patients (72.1%) were not married. The treatment conditions were similar on these characteristics.
Most patients (78.7%) were diagnosed with bipolar I disorder, 14.8% had bipolar II disorder, and 6.6% had BD, not otherwise specified. Seventy-five percent of patients had ≥1 psychiatric hospitalization, with a mean of 3.8 hospitalizations (range=0-40), and 43% had attempted suicide. Most patients (65.6%) had both drug and alcohol dependence, 26.2% had alcohol dependence only, and 8.2% had drug dependence only. Among the 45 patients with drug use disorders, the most common primary drugs of abuse were cocaine (n=19) and marijuana (n=18), followed by opioids (n=2), benzodiazepines (n=1), hallucinogens (n=1), and more than one drug (n=4). Neither BD nor SUD diagnoses varied by treatment condition. Patients reported a mean of 18.2 (sd=9.2) days of substance use during the baseline month: 10.2 (sd=11.0) days of drug use and 13.1 (sd=9.9) days of alcohol use, with some days using both drugs and alcohol. The mean ASI Drug Composite score at baseline was 0.11 (sd=0.11), and the mean ASI Alcohol Composite score was 0.39 (sd=0.23). Mean mood symptom scores during the baseline week were 12.7 (sd=8.6) for the Hamilton depression scale and 10.0 (sd=11.5) for the Young mania scale. At intake, as well as during the three weeks preceding intake, the median overall weekly course rating on the LIFE was 5 on a 1-6 scale; a score of 5 corresponds to a full DSM-IV mood episode, mild to moderate. There were no between-group differences on baseline substance use or mood symptoms (see Table 1 for baseline values).
Table 1.
Means (standard deviations in parentheses) for outcomes by treatment conditiona at baseline, end of treatment (month 3), and end of follow-up (month 6) (N=61)
| Baseline |
End of treatment |
End of follow-up |
||||
|---|---|---|---|---|---|---|
| Outcomesb | IGT | GDC | IGT | GDC | IGT | GDC |
| Primary | ||||||
| Days of any substance use | 18.6 (9.8) | 17.9 (8.8) | 4.4 (7.2) | 6.5 (7.9) | 5.2 (7.0) | 7.9 (10.7) |
| Mood episode (% yes) | 52 (51) | 57 (50) | 20 (41) | 30 (47) | 27 (45) | 37 (49) |
| Secondary | ||||||
| Days of use | ||||||
| Any drugs (n=57) | 8.3 (10.4) | 12.1 (11.6) | 2.1 (4.2) | 3.0 (7.3) | 2.3 (5.4) | 6.0 (10.3) |
| Any alcohol | 15.3 (10.8) | 10.7 (8.5) | 3.6 (6.5) | 3.8 (5.6) | 4.2 (5.9) | 4.2 (8.0) |
| Alcohol to intoxication | 13.2 (11.3) | 9.9 (7.9) | 1.8 (3.4) | 2.3 (3.6) | 2.8 (5.4) | 3.7 (7.8) |
| Addiction Severity Index Composite scores | ||||||
| Drug (n=57) | .09 (.10) | .14 (.11) | .04 (.06) | .07 (.08) | .06 (.09) | .08 (.09) |
| Alcohol | .36 (.25) | .43 (.22) | .27 (.20) | .25 (.19) | .25 (.22) | .20 (.22) |
| Mood | ||||||
| Depressive episode (% yes) | 35 (49) | 40 (50) | 20 (41) | 23 (43) | 20 (41) | 22 (42) |
| Manic episode (% yes)c | 16 (37) | 17 (38) | 0 (0) | 7 (25) | 7 (25) | 15 (36) |
| Hamilton depression scores | 10.8 (7.6) | 14.7 (9.2) | 8.4 (6.7) | 11.0 (8.0) | 10.1 (8.1) | 9.2 (7.8) |
| Young mania scores | 8.9 (10.4) | 11.2 (12.7) | 5.0 (4.6) | 6.1 (7.6) | 4.3 (4.9) | 8.3 (9.3) |
| Medication adherence | ||||||
| Rated | 86.1 (24.6) | 83.8 (21.4) | 92.3 (19.9) | 87.8 (20.8) | 86.7 (28.4) | 90.0 (22.5) |
Treatment conditions: Integrated Group Therapy (IGT) and Group Drug Counseling (GDC)
Binary outcomes were measured weekly; other outcomes were measured monthly.
Includes manic, hypomanic, and mixed episodes
% of days taking mood stabilizers as prescribed
Pharmacotherapy and other treatment
Valproate (29.5%) and lithium (27.9%) were the most commonly prescribed mood stabilizers at baseline, followed by olanzapine (16.4%); one-third of the patients (34.4%) were taking more than one mood stabilizer. Medication adherence was quite high: mood stabilizers were taken as prescribed on a mean of 85.0% (sd=22.9) of the days in the month before study entry. Most patients (65.6%) received individual psychotherapy, with a mean of 1.8 (sd=2.5) sessions attended during the month prior to study entry. Approximately half (54.1%) attended 12-step self-help groups (mean=6.7, sd=9.7 groups) during the month prior to study entry. No between-group differences were found for these additional forms of treatment.
3.2. Substance use outcomes
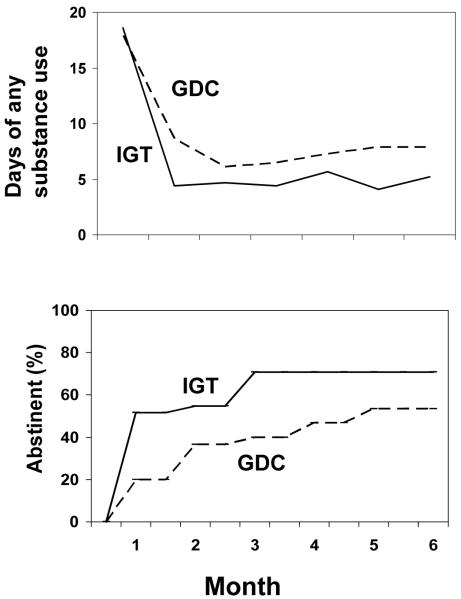
Integrated group therapy patients decreased their days of substance use more than patients in group drug counseling, by an additional 2.7 days from the baseline month to the last month of treatment and by an additional 2.9 days from baseline to the last month of follow-up; this difference was marginally significant (p<0.10) during follow-up (see Table 2). Overall, patients significantly reduced their days of substance use by the last month of treatment (by 14.3 days for integrated group therapy patients, p<0.001; and by 11.6 days for group drug counseling patients, p<0.001) as well as by the last month of follow-up (by 13.2 days for integrated group therapy patients, p<0.001; and 10.2 days for group drug counseling patients, p<0.001). See Table 1 for the mean days of substance use at the end of treatment and the end of follow-up as key data points for reference; for actual declines shown longitudinally over all three months of each phase, see Table 2 and Figure 2, upper panel.
Figure 2.
Treatment condition over time by days of substance use (upper panel) and by time to first abstinent month (lower panel; N=61). IGT = Integrated Group Therapy, GDC = Group Drug Counseling
Integrated group therapy patients were nearly twice as likely to achieve at least one month of abstinence from both drugs and alcohol during treatment (71.0% vs. 40.0%; χ2(1)=5.93, p<0.02), and were nearly three times as likely to be abstinent throughout all three months of treatment (35.5% vs. 13.3%; χ2(1)=4.03, p<0.05). Integrated group therapy patients also had a shorter time from treatment initiation to the first abstinent month (see Figure 2, lower panel), with a hazard ratio of 2.02 (95% confidence interval=1.04-3.90, p<0.04).
When days of drug and alcohol use were separated, no between-group differences were found (see Table 2). Days of drug use decreased significantly: 8.1 days for integrated group therapy patients and 7.4 days for group drug counseling patients from baseline to the last month of treatment, and 6.9 days for integrated group therapy patients and 5.7 days for group drug counseling patients from baseline to the last month of follow-up (all p values<0.001). Similarly, neither days of any alcohol use nor days using alcohol to intoxication (i.e., ≥3 drinks) showed between-group differences in patterns of change. Decreases over time in both measures of alcohol use were significant for each treatment condition (during treatment, by 9.9 and 9.9 days for integrated group therapy and 9.0 and 9.2 days for group drug counseling patients; and during follow-up, 9.2 and 8.9 days for integrated group therapy and 8.5 and 7.7 days for group drug counseling patients; all p values<0.001).
ASI Drug and Alcohol Composite scores showed no between-group differences during treatment; during follow-up, integrated group therapy patients declined less on the ASI Alcohol Composite score than group drug counseling patients (by 0.10 points from the baseline month to the last month of follow-up, p<0.05; see Table 2). Because days of alcohol use did not differ by treatment condition during follow-up, we examined the remaining items that constitute the ASI Alcohol Composite score. At each month of follow-up, results showed that integrated group therapy patients reported significantly more days experiencing “alcohol problems” than group drug counseling patients, despite the similarity in number of days of use in both treatment conditions. Each treatment condition showed significant declines in both ASI Drug and Alcohol Composite scores (0.06-0.14 points lower from baseline to the last month of treatment and 0.05-0.21 points lower from baseline to the last month of follow-up, p values<0.001-0.003).
3.3. Mood outcomes
Mood episodes were assessed as present or absent each week, as described above. Most patients (67.8%) experienced a mood episode at some point during treatment. The between-group difference in risk for mood episodes during treatment was marginally significant: the decline in risk for integrated group therapy patients was 1.8 times greater (1/e-0.6=1.8, p<0.10) than for group drug counseling patients (see Table 2). Overall, mood episode risk declined 82% (1-e-1.7=82% relative decline) for integrated group therapy patients and 67% (1-e-1.1=67% relative decline) for group drug counseling patients by end of treatment (p values<0.001); by end of follow-up, the risk for each treatment condition declined 55% (1-e-0.8=55% relative decline, p values<0.02). The significant decrease in mood episode risk was due to decreased episodes of both depression and mania during treatment.
Examination of the secondary mood outcome of depressive episodes showed that the decline in risk for depression among integrated group therapy patients was two times greater during treatment (odds ratio=1/e-0.7=2.0) than for group drug counseling patients; this difference was marginally significant (p<0.10). During treatment, integrated group therapy patients showed a 70% decline in risk of a depressive episode (1-e-1.2=70%, p<0.001), whereas group drug counseling patients showed only a trend toward a decline in depressive episode risk (e-0.5=39%, p<0.08). There were no significant between-group differences in depressive episodes during follow-up or in manic episodes during treatment or follow-up. Depressive episodes declined during follow-up, by approximately 40-45% for both treatment conditions. Manic episodes showed an 88% decline during treatment (e-2.1=88%, p values<0.001 for each treatment condition), but only a trend toward a lower risk during follow-up (e-0.8=55% lower, p values<0.10 for each treatment condition).
No between-group differences were significant for changes in Hamilton depression and Young mania scores (see Table 2). Each treatment condition showed significant declines in both mood scores during treatment and follow-up (4.8-5.6 points lower for Hamilton depression scores and 2.5-4.1 points lower for Young mania scores, p values<0.001-0.05).
3.4. Medication adherence outcomes
Patients took mood stabilizers as prescribed on a mean of 88.3% (sd=21.9) of days during treatment and a mean of 89.7% (sd=22.1) of days during follow-up, with no significant between-group differences or changes over time (see Tables 1-2).
3.5. Good clinical outcome
Our composite measure of a good clinical outcome for both substance use and mood also favored integrated group therapy at the end of treatment: patients in integrated group therapy were more than twice as likely as patients in group drug counseling to be both abstinent and have no weeks ill with a mood episode in the final month of treatment (45.2% vs. 20.0%; χ2(1)=4.38, p<0.04). The month 6 follow-up also favored integrated group therapy (30.0% vs. 21.4% of patients had good clinical outcomes), but this difference was not significant.
3.6. Additional treatment
Pharmacotherapy
The number of changes in mood stabilizers was examined to consider potential between-group differences in medication management or effectiveness. The number of changes during treatment (mean=0.6, sd=0.8) and during follow-up (mean=0.4, sd=0.7) did not vary by treatment condition.
Psychosocial treatment
Most patients (86.7%; range=2.6-2.9 sessions/month) received individual psychotherapy and just over half (60.0%; range=7.9-8.7 meetings/month) attended 12-step self-help groups during the 3-month treatment; no between-group differences were statistically significant for attendance or for number of sessions attended.
3.7. Quality assurance
Data completion rate
During treatment, data completion was quite high for the primary outcomes of substance use and mood: 100% of data were collected for days of substance use, and mood data were collected for 60/61 patients; we collected follow-up data for 58 of 61 patients (95.1%). For the secondary outcomes, data were collected on 54-60 patients for all six study months. We designated two tiers of data, similar to the National Institute on Drug Abuse Collaborative Cocaine Treatment Study (Crits-Christoph et al., 1999) and our previous randomized controlled trial of integrated group therapy (Weiss et al., 2007). “First-tier” data were collected during face-to-face meetings. “Second-tier” data were collected from telephone interviews and mailed questionnaires if we were unable to collect data in person. We collected exclusively first-tier data from 45 patients (73.8%), and a combination of first- and second-tier data from the rest; this did not vary by treatment condition. The frequency of substance use and mood episodes did not vary by type of data collection.
Self-report validity
We compared urine screens obtained at weekly group sessions to weekly self-reports. Four patients failed once each to report substance use when urine screens were positive, and one patient failed to do so twice. Hence, only 1.2% (6/505) of self-reports showed underreporting of substance use compared to urine data. In these situations, patients were contacted and discrepancies were resolved.
3.8. Group session attendance
The number of group sessions attended did not vary by treatment condition: integrated group therapy patients attended a mean of 74.2% (sd=24.2) of groups, while group drug counseling patients attended a mean of 71.1% (sd=20.5) of group sessions.
4. Discussion
4.1. Summary of findings
In this randomized controlled study, we successfully modified integrated group therapy to be delivered with excellent fidelity by SUD counselors without previous training in cognitive-behavioral therapy or bipolar disorder treatment. The results of this trial support the findings for substance use reported in our previous study examining a longer version of integrated group therapy, conducted by therapists with greater knowledge of both BD and CBT. In that previous trial, we reported between-group differences in (1) days of substance use and (2) time to the first abstinent month, with no difference between groups in mood episodes. In the current study, our primary outcome analyses showed trends toward a greater reduction in days of substance use during follow-up and a greater decrease in risk of mood episodes during treatment for integrated group therapy patients. Some secondary outcomes also favored integrated group therapy patients during treatment, with a significantly greater likelihood of total abstinence, a significantly shorter time to the first abstinent month, and a trend toward a greater decrease in risk of depressive episodes. Finally, patients receiving this “community-friendly” version of integrated group therapy were significantly more likely to achieve a “good clinical outcome” on a composite measure designed to capture both substance use and mood domains simultaneously.
4.2. Issues in outcome measurement for dually diagnosed patients
There is no “gold standard” for a substance use outcome measure in dually diagnosed patients. Assessing the number of days of substance use (or its converse, days abstinent) highlights relative success, but this is an imperfect measure among individuals using different substances at different levels of intensity and risk. Moreover, levels of use that could be non-problematic under most circumstances could be hazardous among those with serious psychiatric illness such as bipolar disorder. It is also unclear what level of improvement in this outcome measure is clinically significant. Alternatively, measuring total abstinence affords a clear indicator of success for substance use, but does not take into account improvement that is less than “perfect.” Examining both of these substance use outcomes, then, provides a more comprehensive assessment, which in this case favors integrated group therapy more on measures of abstinence. Recent research has suggested that abstinence may be very important clinically; Goldstein et al. (2006) found that even moderate use of alcohol may adversely influence the course of bipolar disorder. Our use of a composite measure of a good clinical outcome, i.e., doing well in both substance use and mood domains at the end of treatment, was designed as a clinically relevant measure of treatment success specific to this population. The fact that integrated group therapy produced significantly higher rates of total abstinence and good clinical outcomes than did group drug counseling supports the specific emphasis on the interface between mood and substance use.
4.3. Possible explanations for the study results
The comparatively smaller impact of integrated group therapy on mood could be related to the high degree of medication adherence among both groups throughout the study; this could have created a ceiling effect for one of the potential mechanisms of action of integrated group therapy on mood, i.e., improvement in medication adherence. Alternatively, dually diagnosed patients can achieve some psychiatric benefit from manualized SUD treatment; for example, significant improvement in psychiatric symptoms has been reported in patients with posttraumatic stress disorder and SUD who received manualized SUD relapse prevention treatment (Hien et al., 2004). The non-specific benefits of group drug counseling (e.g., the emphasis on the need to be self-aware, to accept one’s problems, and to lead a healthy lifestyle) may have helped patients deal with their BD as well.
Another reason for the greater differential impact of integrated group therapy on substance use than on mood is the fact that a patient can choose to stop using drugs and alcohol immediately, but cannot make an analogous decision to cease being depressed or manic. Interestingly, visual inspection of the monthly data on days of substance use suggests that the greatest decrease occurred during the first month in treatment (see Figure 2, upper panel). Thus, short-term substantive gains can be achieved in behavioral treatments of SUD, whereas gains from behavioral treatments of BD are usually achieved over a longer period of time. Since our previous study (Weiss et al., 2007) of a 20-week course of integrated group therapy also found that integrated group therapy had a greater impact on SUD than on BD, however, an even longer period of treatment might be needed to produce enduring mood outcomes.
The worse scores for integrated group therapy patients on the ASI Alcohol Composite, despite similar amounts of drinking, may indeed reflect more alcohol problems for integrated group therapy patients compared to group drug counseling patients. Alternatively, the scores may be related to a perception on the part of these patients that continued drinking could worsen the course of their BD; the adverse impact of continued substance use on mood is a central theme of integrated group therapy, and is not emphasized in group drug counseling. Thus, integrated group therapy patients could have been more concerned about potential use even during periods of abstinence or reduced alcohol consumption.
4.4. From efficacy to effectiveness research
This study represents a step from efficacy research to effectiveness research. Efficacy studies examine specific treatments under the strictest and presumably most favorable conditions: they focus on narrowly defined patient populations, with strict inclusion and exclusion criteria and highly trained clinicians. Unfortunately, empirically supported treatment approaches that are efficacious in such studies have been infrequently adopted in SUD community treatment programs (Lamb et al., 1998). Academic centers often study populations that are unrepresentative of treatment-seeking patients in the community, thus limiting the generalizability and the credibility of the treatment to community practitioners. Moreover, such studies often examine complex, expensive treatments delivered by highly trained clinicians which community SUD programs may be unable to implement due to the lack of properly trained personnel or inadequate reimbursement.
In the current trial, we shifted toward effectiveness research by using SUD counselors as study clinicians and shortening the length of treatment to accommodate the realities of limited funding for mental health and SUD treatment. We did not expand the patient population, since even our efficacy study had been relatively inclusive, with few clinical exclusion criteria.
4.5. Limitations
Generalizability is limited by the nature of the study sample: most were white and half were college graduates; this level of education is high compared to a nationally representative sample of people with bipolar disorder (Goldstein et al., 2009). Further, patients were seeking treatment for both disorders and had to be taking a mood stabilizer. The high degree of medication adherence exhibited by participants in both treatment conditions suggests that some of the most difficult and severely disabled patients with these two disorders, who often have poor adherence to treatment, were not represented in this trial. Implementation of integrated group treatment in a clinical setting with a larger sample, perhaps in a public mental health system, and including patients with lower motivation for treatment, would thus be informative.
It is unlikely that other factors, such as medication regimens, individual psychotherapy, or self-help group attendance accounted for the better outcomes in integrated group therapy, since we found no between-group differences in these factors. Conversely, certain aspects of the study design, such as including patients with different substances of abuse and different medication regiments, enabled us to more closely approximate clinical practice and thus shift toward effectiveness research. Increased variability within the relatively small study sample, however, may have reduced power to detect certain between-group differences.
In the analyses of the secondary outcomes, it must be acknowledged that no corrections were made for multiple testing. Although Bonferroni corrections are a potential safeguard against multiple tests of statistical significance, they are overly conservative when the multiple outcomes are expected to be correlated (Miller, 1981). However, we note that with analyses of 14 secondary outcomes, and testing at the alpha=0.05 level, we would expect less than one significant result due to chance. Therefore, the significant results reported for four out of 14 secondary outcomes favoring integrated group therapy cannot be explained as due to chance alone.
4.6. Strengths
Our study had a number of strengths, including a very high rate of data completion (e.g., complete substance use and mood data for all six study months in 95% of the patients). Moreover, since three of the four study clinicians administered both treatment modalities, the effects of individual therapist characteristics are largely controlled for. Furthermore, all group sessions were tape-recorded and monitored for fidelity to the treatment modality. This enabled us to assess for possible contamination of one treatment by the other (e.g., a counselor using IGT techniques in GDC); adherence was high for each counselor.
It is noteworthy that integrated group therapy can be delivered with a high degree of fidelity and competence by SUD counselors without previous CBT experience or knowledge of BD; this finding supports the feasibility of implementing integrated group therapy in real-world SUD community treatment settings. Future research should continue to broaden the scope of integrated group therapy, focusing on more sociodemographically and clinically heterogeneous populations. The results of this study suggest that integrated group therapy is an effective treatment in conjunction with pharmacotherapy for patients with bipolar disorder and substance dependence.
Footnotes
This clinical trial has been registered in a public trials registry at clinicaltrials.gov (identifier is NCT00227838).
Presented in part at the 69th Annual Meeting of The College on Problems of Drug Dependence, June 16-21, 2007, Quebec City, Canada.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anton RF, O’Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM, Gastfriend DR, Hosking JD, Johnson BA, LoCastro LS, Longabaugh R, Mason BJ, Mattson ME, Miller WR, Pettinati HM, Randall CL, Swift R, Weiss RD, Williams LD, Zweben A. Combined pharmacotherapies and behavioral interventions for alcohol dependence. The COMBINE study: a randomized controlled trial. JAMA. 2006;295:2003–2017. doi: 10.1001/jama.295.17.2003. [DOI] [PubMed] [Google Scholar]
- Ball SA, Martino S, Nich C, Frankforter TL, Van Horn D, Crits-Christoph P, Woody GE, Obert JL, Farentinos C, Carroll KM. Site matters: multisite randomized trial of motivational enhancement therapy in community drug abuse clinics. J Consult Clin Psychol. 2007;75:556–567. doi: 10.1037/0022-006X.75.4.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy F, Ahearn EP, Carroll BJ. Substance abuse in bipolar disorder. Bipolar Disord. 2001;3:181–188. [PubMed] [Google Scholar]
- Cisler RA, Zweben A. Development of a composite measure for assessing alcohol treatment outcome: operationalization and validation. Alcohol Clin Exp Res. 1999;23:263–271. [PubMed] [Google Scholar]
- Colom F, Vieta E, Martinez-Aran A, Reinares M, Goikolea JM, Benabarre A, Torrent C, Comes M, Corbella B, Parramon G, Corominas J. A randomized trial on the efficacy of group psychoeducation in the prophylaxis of recurrences in bipolar patients whose disease is in remission. Arch Gen Psychiatry. 2003;60:402–407. doi: 10.1001/archpsyc.60.4.402. [DOI] [PubMed] [Google Scholar]
- Crits-Christoph P, Siqueland L, Blaine J, Frank A, Luborsky L, Onken L, Muenz L, Thase ME, Weiss RD, Gastfriend DR, Woody G, Barber JP, Butler SF, Daley D, Salloum I, Bishop S, Najavits LM, Lis J, Mercer D, Griffin ML, Moras K, Beck AT. Psychosocial treatments for cocaine dependence: results of the National Institute on Drug Abuse Collaborative Cocaine Treatment Study. Arch Gen Psychiatry. 1999;56:493–502. doi: 10.1001/archpsyc.56.6.493. [DOI] [PubMed] [Google Scholar]
- Daley DC, Mercer D, Carpenter G. Group Drug Counseling for Cocaine Dependence: Therapy Manuals for Drug Addition. United States Department of Health and Human Services; 2002. [Google Scholar]
- Dalton EJ, Cate-Carter TD, Mundo E, Parikh SV, Kennedy JL. Suicide risk in bipolar patients: the role of co-morbid substance use disorders. Bipolar Disord. 2003;5:58–61. doi: 10.1034/j.1399-5618.2003.00017.x. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Patient Edition. New York State Psychiatric Institute; 1996. [Google Scholar]
- Frank E, Kupfer DJ, Thase ME, Mallinger AG, Swartz HA, Fagiolini AM, Grochocinski V, Houck P, Scott J, Thompson W, Monk T. Two-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Arch Gen Psychiatry. 2005;62:996–1004. doi: 10.1001/archpsyc.62.9.996. [DOI] [PubMed] [Google Scholar]
- Goldstein BI, Houck PR, Karp JF. Factors associated with pain interference in an epidemiological sample of adults with bipolar I disorder. J Affective Disorders. 2009 doi: 10.1016/j.jad.2009.01.011. doi:10.1016/j.jad.2009.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein BI, Velyvis VP, Parikh SV. The association between moderate alcohol use and illness severity in bipolar disorder: a preliminary report. J Clin Psychiatry. 2006;67:102–106. doi: 10.4088/jcp.v67n0114. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien DA, Cohen LR, Miele GM, Litt LC, Capstick C. Promising treatments for women with comorbid PTSD and substance use disorders. Am J Psychiatry. 2004;161:1426–1432. doi: 10.1176/appi.ajp.161.8.1426. [DOI] [PubMed] [Google Scholar]
- Keck P, McElroy S, Strakowski S, Bourne M, West S. Compliance with maintenance treatment in bipolar disorder. Psychopharmacol Bull. 1997;33:87–91. [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Coryell W, Andreasen NC, Endicott J, Clayton PJ, Klerman GL, Hirschfeld RM. Differential outcome of pure manic, mixed/cycling, and pure depressive episodes in patients with bipolar illness. JAMA. 1986;255:3138–3142. [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC. The Longitudinal Interval Follow-up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Lam DH, Watkins ER, Hayward P, Bright J, Wright K, Kerr N, Parr-Davis G, Sham P. A randomized controlled study of cognitive therapy for relapse prevention for bipolar affective disorder: outcome of the first year. Arch Gen Psychiatry. 2003;60:145–152. doi: 10.1001/archpsyc.60.2.145. [DOI] [PubMed] [Google Scholar]
- Lamb S, Merwyn R, McCarty D, editors. Bridging the Gap Between Practice and Research: Forging Partnerships with Community-Based Drug and Alcohol Treatment. National Academy Press; Washington, DC: 1998. [PubMed] [Google Scholar]
- Liu X, Sturm R, Cuffel BJ. The impact of prior authorization on outpatient utilization in managed behavioral health plans. Med Care Res Rev. 2000;57:182–195. doi: 10.1177/107755870005700203. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Alterman AI, Cacciola J, Metzger D. A new measure of substance abuse treatment: Initial studies of the Treatment Services Review. J Nerv and Ment Dis. 1992;180:101–110. doi: 10.1097/00005053-199202000-00007. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinati H, Argeriou M. The Fifth Edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Otto MW, Frank E, Reilly-Harrington NA, Wisniewski SR, Kogan JN, Nierenberg AA, Calabrese JR, Marangell LB, Gyulai L, Araga M, Gonzalez JM, Shirley ER, Thase ME, Sachs GS. Psychosocial treatments for bipolar depression: a 1-year randomized trial from the Systematic Treatment Enhancement Program. Arch Gen Psychiatry. 2007;64:419–427. doi: 10.1001/archpsyc.64.4.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller RG. Simultaneous statistical inference. 2nd ed. Springer Verlag; New York: 1981. [Google Scholar]
- Project MATCH Research Group Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. J Stud Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- Scott J, Paykel E, Morriss R, Bentall R, Kinderman P, Johnson T, Abbott R, Hayhurst H. Cognitive-behavioural therapy for severe and recurrent bipolar disorders: randomised controlled trial. Br J Psychiatry. 2006;188:313–320. doi: 10.1192/bjp.188.4.313. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Follow-Back: a technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring Alcohol Consumption: Psychosocial and Biochemical Methods. Humana Press; Totowa, NJ: 1992. pp. 41–72. [Google Scholar]
- Stata Version 8.2 for Windows (computer program) Stata Corp.; College Station, TX: 2003. [Google Scholar]
- Washton AM. Group therapy with outpatients. In: Lowinson JH, Ruiz P, Millman RB, Langrod JG, editors. Substance Abuse: A Comprehensive Textbook. 4th Edition Lippincott Williams & Wilkins; 2005. pp. 671–679. [Google Scholar]
- Weiss RD, Greenfield SF, Najavits LM, Soto JA, Wyner D, Tohen M, Griffin ML. Medication compliance among patients with bipolar disorder and substance use disorder. J Clin Psychiatry. 1998;59:172–174. doi: 10.4088/jcp.v59n0405. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Griffin ML, Greenfield SF, Najavits LM, Wyner D, Soto JA, Hennen JA. Group therapy for patients with bipolar disorder and substance dependence: results of a pilot study. J Clin Psychiatry. 2000a;61:361–367. doi: 10.4088/jcp.v61n0507. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Griffin ML, Kolodziej ME, Greenfield SF, Najavits LM, Daley DC, Doreau HR, Hennen JA. A randomized trial of integrated group therapy versus group drug counseling for patients with bipolar disorder and substance dependence. Am J Psychiatry. 2007;164:100–107. doi: 10.1176/ajp.2007.164.1.100. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Kolodziej ME, Najavits LM, Greenfield SF, Fucito LM. Utilization of psychosocial treatments by patients diagnosed with bipolar disorder and substance dependence. Am J Addict. 2000b;9:314–320. doi: 10.1080/105504900750047364. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Najavits LM, Greenfield SF. A relapse prevention group for patients with bipolar and substance use disorders. J Subst Abuse Treat. 1999;16:47–54. doi: 10.1016/s0740-5472(98)00011-7. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Najavits LM, Greenfield SF, Soto JA, Shaw SR, Wyner D. Validity of substance use self-reports in dually diagnosed outpatients. Am J Psychiatry. 1998;155:127–128. doi: 10.1176/ajp.155.1.127. [DOI] [PubMed] [Google Scholar]
- Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–435. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- Zanis DA, McLellan AT, Corse S. Is the Addiction Severity Index a reliable and valid assessment instrument among clients with severe and persistent mental illness and substance abuse disorders? Community Mental Health Journal. 1997;33:213–227. doi: 10.1023/a:1025085310814. [DOI] [PubMed] [Google Scholar]